Key Points
Question
To what extent do Tourette syndrome and chronic tic disorders reduce the chances that affected persons will fulfill their educational potential?
Findings
In this Swedish cohort study that included more than 2 million individuals, including 3590 diagnosed with Tourette syndrome or chronic tic disorders in specialist care, patients were significantly more likely to fail all subjects in compulsory school and less likely to attain each level of education from primary school to university. This was not fully explained by psychiatric comorbidities or familial confounders.
Meaning
Help-seeking individuals with Tourette syndrome or chronic tic disorders diagnosed in specialist care can experience substantial academic underachievement across the lifespan.
This Swedish national register-based study investigates the association of Tourette syndrome and chronic tic disorders with objectively measured educational outcomes, adjusting for psychiatric comorbidities and factors shared between siblings.
Abstract
Importance
The influence of Tourette syndrome and chronic tic disorders on academic performance has not been objectively quantified.
Objective
To investigate the association of Tourette syndrome and chronic tic disorders with objectively measured educational outcomes, adjusting for measured covariates and unmeasured factors shared between siblings and taking common psychiatric comorbidities into account.
Design, Setting, and Participants
A population-based birth cohort consisting of all individuals born in Sweden from 1976 to 1998 was followed up until December 2013. Individuals with organic brain disorders, mental retardation, and 2 foreign-born parents were excluded. We further identified families with at least 2 singleton full siblings and families with siblings discordant for Tourette syndrome or chronic tic disorders.
Exposures
Previously validated International Classification of Diseases diagnoses of Tourette syndrome or chronic tic disorders in the Swedish National Patient Register.
Main Outcomes and Measures
Eligibility to access upper secondary school after compulsory education, finishing upper secondary school, starting a university degree, and finishing a university degree.
Results
Of the 2 115 554 individuals in the cohort, 3590 had registered a diagnosis of Tourette syndrome or a chronic tic disorder in specialist care (of whom 2822 [78.6%] were male; median [interquartile] age at first diagnosis, 14.0 [11-18] years). Of 726 198 families with at least 2 singleton full siblings, 2697 included siblings discordant for these disorders. Compared with unexposed individuals, people with Tourette syndrome or chronic tic disorders were significantly less likely to pass all core and additional courses at the end of compulsory school (odds ratios ranging from 0.23 [95% CI, 0.20-0.26] for the handcraft textile/wood course to 0.36 [95% CI, 0.31-0.41] for the English language course) and to access a vocational program (adjusted OR [aOR], 0.31; 95% CI, 0.28-0.34) or academic program (aOR, 0.43; 95% CI, 0.39-0.47) in upper secondary education. Individuals with the disorders were also less likely to finish upper secondary education (aOR, 0.35; 95% CI, 0.32-0.37), start a university degree (aOR, 0.41; 95% CI, 0.37-0.46), and finish a university degree (aOR, 0.39; 95% CI, 0.32-0.48). The results were only marginally attenuated in the fully adjusted sibling comparison models. Exclusion of patients with neuropsychiatric comorbidities, particularly attention-deficit/hyperactivity disorder and pervasive developmental disorders, resulted in attenuated estimates, but patients with Tourette syndrome or chronic tic disorders were still significantly impaired across all outcomes.
Conclusions and Relevance
Help-seeking individuals with Tourette syndrome or chronic tic disorders seen in specialist settings experience substantial academic underachievement across all educational levels, spanning from compulsory school to university, even after accounting for multiple confounding factors and psychiatric comorbidities.
Introduction
Tourette syndrome (TS) and chronic tic disorders (CTD) are childhood-onset neurodevelopmental conditions characterized by multiple motor and/or vocal tics persisting for more than 1 year.1 The estimated prevalence of TS and CTD ranges between 0.15% to 1% of the population, with larger prevalence reported in nontreatment-seeking populations and when impairment is not required for diagnosis.2,3,4,5 Most individuals have comorbid conditions, including neuropsychiatric disorders, which are often more impairing than the tics themselves.6,7
Tourette syndrome or CTD, especially when tics are severe and presenting with psychiatric comorbidities, considerably impair a person’s general functioning and quality of life.8 An area that has received relatively little attention is academic performance in individuals with TS/CTD. Children with tic disorders experience a range of school difficulties, some of which are directly associated with the symptoms themselves (eg, the time and energy spent on performing or trying to suppress motor tics may interfere with the learning process).9 Individuals with TS/CTD also experience psychosocial stressors (eg, teasing or bullying at school),10 which might further interfere with their education. Furthermore, TS/CTD have been associated with neuropsychological deficits, such as executive, memory, and fine motor dysfunctions,9,11 which might have a direct outcome on learning and school performance. There is some evidence from cross-sectional studies that children and adolescents with TS/CTD are at increased risk for experiencing academic difficulties and/or dropping out of school prematurely compared with the general population.12,13,14,15,16,17 However, previous studies have been beset by various limitations, including the reliance on generally small samples from highly specialist clinics,12,13,14 use of cross-sectional designs,13,14,15 lack of control groups,12,13,15 use of self-reports or parent reports rather than objective measures of educational outcomes,13,14,15,16,17 and insufficient control of potential confounders.15,16,17 Furthermore, previous studies have been limited to the educational outcomes in childhood and adolescence and thus the influence of TS/CTD on later stages of education (eg, university) is unknown. Since most individuals with TS/CTD experience a gradual decline in tic severity as they enter their adult life,18 it is plausible that some patients may compensate for their initial difficulties and complete their education, but this has not been explored.
This population-based study aimed to investigate the association of TS/CTD with educational attainment across the person’s lifespan from compulsory school through university, taking into account a number of measured covariates, such as parental age and parity. In addition, we used a sibling control design to control for unmeasured familial confounders shared by full siblings (such as genetic factors, parental psychopathology, or socioeconomic status). To evaluate to what extent the observed associations are explained by comorbid neuropsychiatric conditions, we performed sensitivity analyses in subgroups in which all individuals with comorbid conditions were excluded. We hypothesized that TS/CTD would be associated with academic underachievement across all educational levels, that this would be particularly apparent in the early stages of education (when symptoms are most severe), and that comorbid neuropsychiatric conditions would further contribute to the observed academic impairments.
Methods
Ethical approval was obtained from the regional ethical review board in Stockholm. The requirement for informed consent was waived because the study was register based and the included individuals deidentified.
Study Population and Design
We linked the following Swedish national population-based registers through the individuals’ unique personal identification numbers (recoded for anonymity)19: (1) the National School Register, that holds information on individual school performance from all municipal and independent schools starting from December, 31, 198820; (2) the Longitudinal Integration Database for Health Insurance and Labor Studies (that has the acronym LISA in Swedish), which annually integrates data on the labor market, education, and social sectors from all individuals living in Sweden21; (3) the Swedish National Patient Register (NPR), which covers inpatient hospital admissions since 1969 and outpatient care since 2001 using codes from International Classification of Diseases (ICD), Eighth Revision (ICD-8), Ninth Revision (ICD-9), and Tenth Revision (ICD-10)22; (4) the Multi-Generation Register, which connects every person born in Sweden from 1932 onwards ever registered as living in Sweden after 1961 to their parents and enables to obtain family pedigree for each subject23; (5) the Migration Register, providing information about migration in and out of Sweden24; and (6) the Cause of Death Register, with information on dates and causes of all deaths since 1961.25
The initial study cohort consisted of 2 328 201 individuals (1 195 489 males; 51.3%) who were born in Sweden between January 1, 1976, and December 31, 1998, and who had information available up to December 31, 2013. As described elsewhere,26 individuals diagnosed with organic brain disorders (ICD-9 code 310 and ICD-10 codes F00-F09) and/or mental retardation (ICD-8 codes 310-315, ICD-9 codes 317-319, and ICD-10 codes F70-F79) were excluded from the cohort (n = 23 115). Additionally, individuals with 2 parents born outside Sweden or missing data on the origin of the parents were also excluded (n = 192 426).27 The final study cohort consisted of 2 115 554 individuals (1 085 445 males; 51.0%). For the sibling-comparison analyses, we identified a subsample of 726 198 families with at least 2 singleton full siblings (ie, siblings of either sex sharing the same biological mother and father) during the same period.
Exposure
We used a previously validated algorithm to define the individuals who received a diagnosis of TS or CTD.28 Those considered as exposed were (1) all individuals with at least 1 diagnosis of a tic disorder in ICD-8 (code 306.2) or ICD-9 (code 307C); (2) all individuals with at least 1 diagnosis in ICD-10 of CTD (code F95.1) or TS (code F95.2), unless they received a final diagnosis of transient tic disorder (code F95.0) within the same year as the initial diagnosis; (3) all individuals with other tic disorders (code F95.8) or unspecified tic disorders (code F95.9) who also received at least 1 additional tic disorder diagnosis (codes F95.1, F95.2, F95.8, or F95.9), unless they received a final diagnosis of transient tic disorder (code F95.0) within the same year as the initial diagnosis. This approach resulted in nearly perfect interrater reliability and highly valid diagnoses, with a positive predictive value of 0.89 for the ICD-8, 0.86 in the ICD-9, and 0.97 in the ICD-10.28
Compulsory Education Outcomes
The National School Register contains information on each student’s eligibility to access upper secondary education after completion of compulsory education at age 15 or 16 years in Sweden. Because of different admission requirements before 1998 and after 2010, information from the National School Register was retrieved for a subcohort of individuals with data between these years (n = 1 234 042). Eligibility to access upper secondary education (dichotomized as eligible vs not eligible) is based on the school grades in the final year of compulsory school. The admission requirements vary depending on the student’s choice for a vocational program or an academic program. Students aiming to enter a vocational program were required to pass the 3 core courses (Swedish, English, and mathematics), and students aiming to enter an academic program (preparatory for higher education, such as a university degree) were required to pass the 3 core courses and at least 9 additional courses. The National School Register also includes information on the individual school courses, which were coded as binary variables (passed vs not passed).
Educational Outcomes After Compulsory Education
Data on binary educational outcomes (achieved vs not achieved) for the full cohort (n = 2 115 554) were retrieved from the LISA database.21 Finishing upper secondary school, starting a university degree, and finishing a university degree were the selected outcomes.
Statistical Methods
Individuals with a diagnosis of TS/CTD were considered exposed and those without these disorders were considered unexposed. Logistic regression models were fit to compare exposed and unexposed individuals on all binary outcomes (ie, passing specific courses, eligibility to progress to secondary education, and achievement of subsequent educational levels). Results were expressed as odds ratios (ORs) with 95% CIs. First, crude associations with TS/CTD were modeled separately for each outcome. Subsequently, models were adjusted for sex, year of birth, maternal age, paternal age, and parity.
As per the methods of previous studies,26,29 a fixed-effects model was implemented in the subsample of clusters of all full siblings of individuals with TS/CTD using conditional logistic regression models, where each family was considered a stratum. By design, these models control for shared familial confounders30 and, in particular, for genetic factors and unmeasured shared confounders, such as socioeconomic status or stable parental factors, that make siblings similar. Furthermore, we adjusted for all measured confounders listed here, which typically vary between siblings.
Sensitivity analyses were performed in subgroups in which all individuals with lifetime comorbid conditions were excluded. These conditions were organized in 10 groups according to the most relevant comorbidities in individuals with TS/CTD: (1) obsessive-compulsive disorder; (2) attention-deficit/hyperactivity disorder (ADHD); (3) pervasive developmental disorders; (4) conduct disorders; (5) learning disabilities; (6) schizophrenia, schizotypal, and delusional disorders; (7) phobic, anxiety, and stress reaction or adjustment disorders; (8) affective disorders; (9) substance use disorders; and (10) other disorders (including dissociative, somatoform, other neurotic disorders, and eating disorders) (eTable 1 in the Supplement). All disorders were defined as at least 1 registered diagnosis in the NPR. These models also adjusted for sex, year of birth, maternal age, paternal age, and parity.
Additionally, analyses for postcompulsory educational outcomes were repeated on subgroups of individuals to ensure that all included individuals had had the time necessary to complete every level of education (cohorts born between 1976 and 1992 for upper secondary school, between 1976 and 1990 for starting a university degree, and between 1976 and 1988 for finishing a university degree, respectively). Because prior to 2001 only inpatients were included in the NPR (resulting in potential bias), analyses were repeated using a more recent subcohort of individuals born between 1994 and 1998 to ensure full coverage of specialized outpatient care.28
All analyses were conducted using SAS, version 9.4 (SAS Institute Inc). All P values less than .05 were considered significant.
Results
Descriptive Statistics
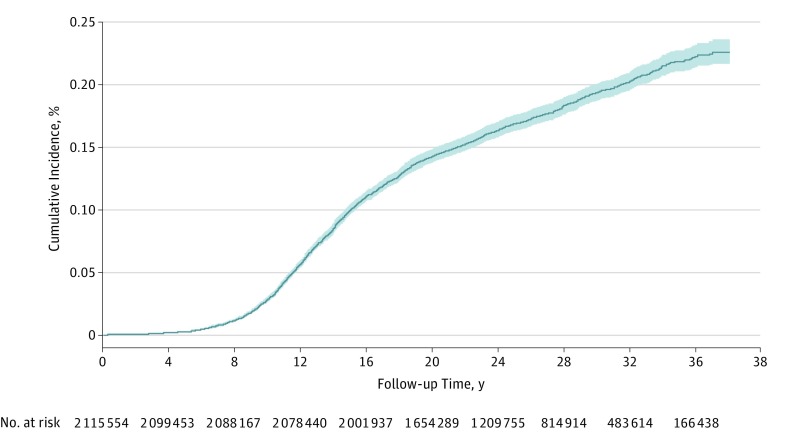
Descriptive characteristics of the study cohort are presented in Table 1. Of the 2 115 554 individuals included, 3590 received a diagnosis of TS/CTD, resulting in a Kaplan-Meier estimated cumulative incidence of 0.22% (95% CI, 0.21%-0.23%) by age 37 years (Figure). The median (interquartile) age at first diagnosis was 14 (11-18) years. As expected, those with a diagnosis of TS/CTD were more frequently diagnosed with psychiatric disorders compared with those without TS/CTD (76.8% vs 23.2%, respectively). Of the 726 198 families with at least 2 singleton children, 2697 included full siblings discordant for TS/CTD.
Table 1. Distribution of Study Variables Among Study Cohort Members Born in Sweden Between 1976 and 1998, Stratified by Presence of Tourette Syndrome/Chronic Tic Disorder.
| Characteristic | Individuals, No. (%) | |
|---|---|---|
| With TS/CTD (n = 3590)a | Without TS/CTD (n = 2 111 964) | |
| Male | 2822 (78.6) | 1 082 623 (51.3) |
| Age of mothers at birth of index person, mean (SD), yb | 27.6 (5.3) | 28.0 (5.0) |
| Age of fathers at birth of index person, mean (SD), yb | 30.5 (6.3) | 30.7 (5.8) |
| Missing | 30 (0.8) | 14 021 (0.7) |
| Parityb | ||
| 1 | 1897 (52.8) | 1 116 790 (52.9) |
| 2 | 1131 (31.5) | 704 737 (33.4) |
| 3 | 406 (11.3) | 226 065 (10.7) |
| ≥4 | 156 (4.4) | 64 372 (3.1) |
| Comorbidity | ||
| Any psychiatric disorder | 2757 (76.8) | 833 (23.2) |
| Obsessive-compulsive disorderb | 719 (20.0) | 14 401 (0.7) |
| Attention-deficit/ hyperactivity disorderb | 1873 (52.2) | 53 986 (2.6) |
| Pervasive developmental disorderb | 1014 (28.3) | 21 752 (1.0) |
| Conduct disorderb | 263 (7.3) | 5285 (0.3) |
| Learning disabilitiesb | 151 (4.2) | 5265 (0.3) |
| Schizophrenia, schizotypal, delusional disordersb | 159 (4.4) | 13 034 (0.6) |
| Phobic, anxiety, and reaction to stress/adjustment disordersb | 856 (23.8) | 107 550 (5.1) |
| Affective disordersb | 882 (24.6) | 115 263 (5.5) |
| Substance use disordersb | 453 (12.6) | 90 111 (4.3) |
| Other disordersb,c | 469 (13.1) | 81 521 (3.9) |
Kaplan-Meier estimate of expected cumulative incidence at age 37 years: 0.22% (Figure).
Statistically significant between-group difference (P < .001) determined with a χ2 test or a 2-tailed t test of independent samples.
Includes dissociative, somatoform, other neurotic, and eating disorders.
Figure. Expected Cumulative Incidence of Tourette Syndrome/Chronic Tic Disorder in the Study Cohort.
Compulsory Education
Individuals with TS/CTD were significantly less likely to be eligible to access a vocational or an academic program in upper secondary school, compared with the general population; 74.9% were eligible for vocational program in the exposed group compared with 91.3% in the unexposed group (OR, 0.31 [95% CI, 0.28–0.34]), and 56.3% were eligible for an academic program in the exposed group compared with 77.0% in the unexposed group (OR, 0.43 [95% CI, 0.39–0.47]). The results were marginally attenuated in the sibling comparison models (OR for vocational program, 0.40 [95% CI, 0.31–0.51]; OR for academic program, 0.47 [95% CI, 0.38–0.58]) (Table 2).
Table 2. Odds Ratios for Educational Attainment Among Individuals With Tourette Syndrome/Chronic Tic Disorders Compared With Unaffected Individuals From the General Population and Full Siblings of Affected Individuals.
| Educational Attainment Level | Individuals, No. (%) | Odds Ratio (95% CI) | |||
|---|---|---|---|---|---|
| With TS/CTD | Without TS/CTD | Unadjusted Model | Adjusteda,b | Full Sibling Comparisona,b | |
| Compulsory education, No. | 2019 | 1 232 023 | |||
| Eligible for vocational program | 1512 (74.9) | 1 124 909 (91.3) | 0.28 (0.26-0.31) | 0.31 (0.28-0.34) | 0.40 (0.31-0.51) |
| Eligible for academic program | 1136 (56.3) | 948 735 (77.0) | 0.38 (0.35-0.42) | 0.43 (0.39-0.47) | 0.47 (0.38-0.58) |
| Postcompulsory education, No. | 3590 | 2 111 964 | |||
| Finishing upper secondary school | 1181 (32.9) | 1 402 807 (66.4) | 0.25 (0.23-0.27) | 0.35 (0.32-0.37) | 0.46 (0.40-0.53) |
| Starting a university degree | 336 (9.4) | 608 648 (28.8) | 0.26 (0.23-0.29) | 0.41 (0.37-0.46) | 0.45 (0.37-0.56) |
| Finishing a university degree | 112 (3.1) | 294 474 (13.9) | 0.20 (0.17-0.24) | 0.39 (0.32-0.48) | 0.64 (0.46-0.90) |
Abbreviation: TS/CTD, Tourette syndrome/chronic tic disorders.
Adjusted by sex, year of birth, maternal age, paternal age, and parity.
All findings in these columns are statistically significant.
Analyses of the specific subjects revealed that individuals with a diagnosis of TS/CTD were significantly less likely to pass all subjects in the last year of compulsory education (ORs in the fully adjusted models ranging from 0.23 [95% CI, 0.20-0.26] for a course in handcraft textile/wood to 0.36 [95% CI, 0.31-0.41] for English language). For example, individuals with TS/CTD had 68%, 64%, and 65% lower odds of passing each of the core courses (Swedish language: OR, 0.32 [95% CI, 0.28-0.37]; English language: OR, 0.36 [95% CI, 0.31-0.41]; mathematics: OR, 0.35 [95% CI, 0.31-0.39]; Table 3). The results of the sibling comparison analyses yielded estimates with smaller magnitude (ORs ranging from 0.33 to 0.57; Swedish language: OR, 0.47 [95% CI, 0.34-0.65]; English language: OR, 0.45 [95% CI, 0.33-0.61]; mathematics: OR, 0.45 [95% CI, 0.34-0.60]; Table 3).
Table 3. Odds Ratios for Passing Courses on Graduation From Compulsory Education Among Individuals With Tourette Syndrome/Chronic Tic Disorders Compared With Unaffected Individuals From the General Population and Full Siblingsa.
| Courses | Individuals, No. (%) | OR (95% CI) | |||
|---|---|---|---|---|---|
| With TS/CTD (n = 2019) | Without TS/CTD (n = 1 232 023) | Unadjusted Modelb | Adjustedb,c | Full Sibling Comparisonb,c | |
| Core courses | |||||
| Swedish language | 1684 (87.3) | 1 173 856 (96.2) | 0.28 (0.24-0.31) | 0.32 (0.28-0.37) | 0.47 (0.34-0.65) |
| English language | 1673 (86.4) | 1 163 500 (95.2) | 0.32 (0.28-0.37) | 0.36 (0.31-0.41) | 0.45 (0.33-0.61) |
| Mathematics | 1627 (84.0) | 1 151 391 (94.2) | 0.33 (0.29-0.37) | 0.35 (0.31-0.39) | 0.45 (0.34-0.60) |
| Additional courses | |||||
| Arts | 1651 (85.3) | 1 173 851 (96.0) | 0.24 (0.21-0.27) | 0.28 (0.24-0.31) | 0.51 (0.37-0.69) |
| Biology | 1159 (76.6) | 935 941 (92.5) | 0.27 (0.24-0.30) | 0.29 (0.26-0.33) | 0.41 (0.30-0.57) |
| Chemistry | 1069 (70.7) | 917 035 (90.6) | 0.25 (0.22-0.28) | 0.27 (0.24-0.30) | 0.37 (0.27-0.50) |
| Geography | 1026 (80.5) | 787 191 (93.4) | 0.29 (0.25-0.34) | 0.33 (0.28-0.38) | 0.57 (0.39-0.84) |
| Handcraft textile/ wood | 1658 (85.7) | 1 180 095 (96.6) | 0.21 (0.19-0.24) | 0.23 (0.20-0.26) | 0.29 (0.21-0.40) |
| History | 1034 (81.2) | 785 721 (93.2) | 0.31 (0.27-0.36) | 0.33 (0.29-0.38) | 0.47 (0.31-0.70) |
| Home and consumer studies | 1473 (84.6) | 934 845 (95.8) | 0.24 (0.21-0.28) | 0.26 (0.23-0.30) | 0.44 (0.31-0.61) |
| Knowledge of society | 1023 (80.3) | 788 011 (93.5) | 0.28 (0.25-0.33) | 0.31 (0.27-0.36) | 0.48 (0.33-0.71) |
| Music | 1590 (82.2) | 1 165 243 (95.3) | 0.23 (0.20-0.25) | 0.25 (0.22-0.28) | 0.33 (0.25-0.45) |
| Physics | 1093 (72.2) | 922 202 (91.1) | 0.25 (0.23-0.28) | 0.26 (0.24-0.30) | 0.36 (0.26-0.49) |
| Religion | 1004 (78.8) | 787 373 (93.4) | 0.26 (0.23-0.30) | 0.29 (0.26-0.34) | 0.41 (0.27-0.62) |
| Sports and health | 1537 (79.4) | 1 137 550 (93.1) | 0.29 (0.26-0.32) | 0.27 (0.24-0.30) | 0.47 (0.36-0.60) |
| Technology | 1545 (79.8) | 1 157 210 (94.7) | 0.22 (0.20-0.25) | 0.23 (0.20-0.25) | 0.37 (0.28-0.48) |
Abbreviations: OR, odds ratio; TS/CTD, Tourette syndrome/chronic tic disorders.
Data from the subcohort of individuals graduating compulsory school between 1998 and 2010.
Adjusted by sex, year of birth, maternal age, paternal age, and parity.
All findings in these columns are statistically significant.
Educational Attainment After Compulsory School
Compared with the rest of the population, individuals with TS/CTD were significantly less likely to achieve each of the assessed educational levels during the study period. Specifically, in the adjusted models, people with TS/CTD had 65% lower odds of completing upper secondary school (OR, 0.35 [95% CI, 0.32-0.37]), 59% lower odds of starting a university degree (OR, 0.41 [95% CI, 0.37-0.46]), and 61% lower odds of finishing a university degree (OR, 0.39 [95% CI, 0.32-0.48]) (Table 2). The results remained fairly similar in the sibling comparison model, although the estimates were less precise (with broader CIs).
Association With Psychiatric Comorbidity
When individuals with different groups of comorbidities were excluded from the analyses, the results were largely unchanged, except for ADHD and pervasive developmental disorders. Exclusion of these individuals resulted in attenuated estimates but did not account for the entire association (Table 4). Notably, these comorbidities were also the most frequent in the TS/CTD cohort, with more than half of these individuals being also diagnosed with ADHD (1873 of 3590 [52.2%]) and almost one-third being diagnosed with pervasive developmental disorders (1014 of 3590 [28.3%]) (Table 1).
Table 4. Adjusted Odds Ratios for Educational Attainment Among Individuals With Tourette Syndrome/Chronic Tic Disorders Compared With Unaffected Individuals From the General Population, Excluding Comorbidities.
| Educational Outcome | Excluding, OR (95% CI)a,b | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Whole Cohort (Adjusted Model) | OCD | ADHD | PDD | Conduct Disorders | Learning Disabilities | Psychotic Disorders | Anxiety Disorders | Affective Disorders | Substance Use Disorders | Other Psychiatric Disordersa,c | |
| Compulsory education | |||||||||||
| Eligible for vocational program | 0.31 (0.28- 0.34) |
0.31 (0.27- 0.35) |
0.43 (0.36- 0.50) |
0.37 (0.33- 0.43) |
0.32 (0.29- 0.36) |
0.32 (0.28- 0.35) |
0.32 (0.29- 0.35) |
0.34 (0.30- 0.39) |
0.30 (0.27- 0.34) |
0.31 (0.27- 0.34) |
0.32 (0.29- 0.36) |
| Eligible for academic program | 0.43 (0.39- 0.47) |
0.42 (0.38- 0.47) |
0.57 (0.50- 0.65) |
0.48 (0.43- 0.53) |
0.44 (0.40- 0.49) |
0.44 (0.40- 0.48) |
0.43 (0.40- 0.48) |
0.46 (0.41- 0.51) |
0.43 (0.39- 0.48) |
0.45 (0.41- 0.50) |
0.43 (0.39- 0.47) |
| Post-compulsory education | |||||||||||
| Finishing upper secondary school | 0.35 (0.32- 0.37) |
0.35 (0.32- 0.38) |
0.48 (0.44- 0.54) |
0.42 (0.38- 0.45) |
0.36 (0.33- 0.38) |
0.35 (0.32- 0.38) |
0.37 (0.34- 0.39) |
0.41 (0.38- 0.45) |
0.38 (0.35- 0.41) |
0.38 (0.35- 0.42) |
0.38 (0.35- 0.41) |
| Starting a university degree | 0.41 (0.37- 0.46) |
0.40 (0.35- 0.46) |
0.60 (0.52- 0.69) |
0.43 (0.38- 0.50) |
0.43 (0.38- 0.48) |
0.42 (0.37- 0.48) |
0.43 (0.38- 0.48) |
0.45 (0.39- 0.52) |
0.42 (0.36- 0.48) |
0.46 (0.40- 0.52) |
0.44 (0.39- 0.50) |
| Finishing a university degree | 0.39 (0.32- 0.48) |
0.40 (0.32- 0.50) |
0.56 (0.45- 0.70) |
0.48 (0.39- 0.60) |
0.40 (0.32- 0.49) |
0.40 (0.32- 0.49) |
0.42 (0.34- 0.51) |
0.48 (0.38- 0.61) |
0.43 (0.34- 0.55) |
0.43 (0.35- 0.53) |
0.43 (0.35- 0.53) |
Abbreviations: ADHD, attention-deficit/hyperactivity disorder; OCD, obsessive-compulsive disorder; OR, odds ratio; PDD, pervasive developmental disorders.
Adjusted by sex, year of birth, maternal age, paternal age, and parity.
All findings in the Table are statistically significant.
Includes dissociative, somatoform, other neurotic, and eating disorders.
Sensitivity Analyses
A similar pattern of results was obtained in the sensitivity analyses, in which all individuals in the subcohorts had had the time to complete postcompulsory educational levels (eTable 2 in the Supplement). Similar outcomes were found when we selected a younger subcohort of individuals born between 1994 and 1998 (eTable 3 in the Supplement).
Discussion
To our knowledge, this is the first study examining the influence of TS/CTD diagnosed in specialist settings on prospective, objectively measured educational outcomes at a nationwide level. Patients were more likely to fail all subjects in compulsory school, less likely to be eligible for and to complete secondary school, and less likely to complete all post-secondary educational levels. Individuals with organic brain disorders, mental retardation, and 2 parents born outside Sweden were not included in the cohort. Exclusion of individuals with ADHD and pervasive developmental disorders attenuated but did not substantially alter the estimates, whereas the exclusion of the other relevant lifetime comorbidities did not alter the magnitude of the results. Thus, TS/CTD are associated with substantial educational impairment in their own right.
Our results showed that TS/CTD was associated with substantial educational impairment across all education levels, including beyond primary school. Affected individuals had 65% lower odds of completing secondary education, 59% lower odds of entering a university program, and 61% lower odds of completing a university degree. This is striking, considering that TS/CTD is mostly known as a childhood disorder and that a substantial number of individuals experience a decline of symptoms as they age. Approximately 20% of TS/CTD cases continue to experience clinically impairing tics as adults.18,31,32 These findings suggest that the effect of the disorder on the individual’s educational potential is long-lasting and that it may be difficult for these individuals to find alternative routes to reengage with the education system (such as the locally funded adult education system known as komvux in Sweden), even if their symptoms somewhat improve with age. This contrasts with obsessive-compulsive disorder, where educational impairments are most pronounced early during the course of the disorder and somewhat improve later in life.26
The findings from the sibling analyses suggest that the results are likely to primarily reflect impairments directly associated with TS/CTD or factors that are highly correlated with the tic disorders. However, the magnitude of the associations was somewhat attenuated in these sibling models. There are several possible explanations for these findings. One possibility is that there are genetic and/or environmental risk factors that may partially explain both the disorder and the educational performance. For example, because both TS/CTD and educational attainment are known to be genetically influenced,33,34 it may be that pleiotropic genetic effects are at play. Another possible interpretation is that, while siblings of affected individuals did not have a diagnosis of TS/CTD, they may have had undiagnosed tic disorders or other neuropsychiatric disorders that are known to impair education.26 This is plausible, given the known shared causal mechanisms between neuropsychiatric disorders in general35,36 and TS/CTD, obsessive-compulsive disorder, and ADHD in particular.37
Our results highlight the need to detect and correctly treat TS/CTD at an early stage to increase the chances that affected individuals fulfill their educational potential, particularly when symptoms are severe or comorbid with other neuropsychiatric problems. Person-centered educational plans aimed at reducing school underachievement in children with complex TS/CTD are warranted, such as establishing a private space where the child can release the tics, providing extra time to complete school tasks, or providing separate locations to take exams. Furthermore, education of teachers and peers about TS/CTD is important because the disorder is still stigmatizing10 and TS/CTD patients are more prone to experience violence and isolation from their peers.10 The hypothesis that receipt of evidence-based treatment for TS/CTD (ie, behavior therapy, selective α2A receptor agonists, or antipsychotics) is associated with improved educational outcomes makes intuitive sense and should be evaluated in future research. Because of the nature of our cohort, composed of treatment-seeking individuals who required and received specialist care, our results may not necessarily generalize to individuals with mild tics who are not impaired. It is likely that many individuals with mild tics are quite successful in life both academically and otherwise.38,39
Strengths
A major strength of the study is the use of a large nationally representative cohort with data collected from records kept by government agencies or other organizations, which ensured minimal risk of selection, recall, and report biases. The long follow-up period enabled the examination of educational outcomes, spanning from childhood (compulsory school) to adulthood (up to finishing university). Finally, the use of sibling comparison models allowed us to strictly control for unmeasured confounders, such as genetic and environmental factors shared by siblings.
Limitations
Several limitations of the study need to be considered. The register only includes specialist care visits and not patients seen in general practitioner clinics. Similarly, the NPR does not include patients diagnosed by professionals other than physicians working in specialist care. These limitations also apply to the identification of the comorbid psychiatric conditions. Thus, while the patients included in our cohort resemble other patients recruited from specialist tic disorder clinics around the world, it is possible that our results do not generalize to less complex patient samples. Prior to 2001, the NPR only included inpatient admissions, which could have biased the results toward the most severe end of the tic disorder spectrum. However, sensitivity analyses limiting the cohort to younger individuals born between 1994 and 1998 (to ensure full coverage of outpatient care) resulted in similar estimates. Interpretation of the sibling comparison analyses requires consideration of some limitations associated with such designs, such as lower statistical power than population-based estimates.40 An additional limitation is that the NPR does not include measures of symptom severity, which may have a clear effect on the eventual educational attainment of an individual. Presumably, individuals with mild tics are much less likely to have impaired educational outcomes. Finally, we were not able to investigate other interesting outcomes, such as absenteeism from school, which would have added valuable information on the influence of TS/CTD on education.
Conclusions
Treatment-seeking individuals with TS/CTD seen in specialist settings experience substantial academic underachievement across all educational levels, spanning from compulsory school to university, even after accounting for multiple confounding factors and psychiatric comorbidities.
eTable 1. ICD codes used in the study.
eTable 2. Sensitivity analyses (1).
eTable 3. Sensitivity analyses (2).
References
- 1.American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders. 5th ed Washington, DC: American Psychiatric Association; 2013. [Google Scholar]
- 2.Scahill L, Specht M, Page C. The prevalence of tic disorders and clinical characteristics in children. J Obsessive Compuls Relat Disord. 2014;3(4):394-400. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Knight T, Steeves T, Day L, Lowerison M, Jette N, Pringsheim T. Prevalence of tic disorders: a systematic review and meta-analysis. Pediatr Neurol. 2012;47(2):77-90. [DOI] [PubMed] [Google Scholar]
- 4.Scharf JM, Miller LL, Gauvin CA, Alabiso J, Mathews CA, Ben-Shlomo Y. Population prevalence of Tourette syndrome: a systematic review and meta-analysis. Mov Disord. 2015;30(2):221-228. [DOI] [PubMed] [Google Scholar]
- 5.Kadesjö B, Gillberg C. Tourette’s disorder: epidemiology and comorbidity in primary school children. J Am Acad Child Adolesc Psychiatry. 2000;39(5):548-555. [DOI] [PubMed] [Google Scholar]
- 6.Lebowitz ER, Motlagh MG, Katsovich L, et al. ; Tourette Syndrome Study Group . Tourette syndrome in youth with and without obsessive compulsive disorder and attention deficit hyperactivity disorder. Eur Child Adolesc Psychiatry. 2012;21(8):451-457. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Martino D, Ganos C, Pringsheim TM. Tourette syndrome and chronic tic disorders: the clinical spectrum beyond tics. Int Rev Neurobiol. 2017;134:1461-1490. [DOI] [PubMed] [Google Scholar]
- 8.Eapen V, Cavanna AE, Robertson MM. Comorbidities, social impact, and quality of life in Tourette Syndrome. Front Psychiatry. 2016;7:97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Morand-Beaulieu S, Leclerc JB, Valois P, Lavoie ME, O’Connor KP, Gauthier B. A review of the neuropsychological dimensions of Tourette Syndrome. Brain Sci. 2017;7(8):E106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Malli MA, Forrester-Jones R, Murphy G. Stigma in youth with Tourette’s syndrome: a systematic review and synthesis. Eur Child Adolesc Psychiatry. 2016;25(2):127-139. [DOI] [PubMed] [Google Scholar]
- 11.Como PG. Neuropsychological function in Tourette syndrome. Adv Neurol. 2001;85:103-111. [PubMed] [Google Scholar]
- 12.Packer LE. Tic-related school problems: impact on functioning, accommodations, and interventions. Behav Modif. 2005;29(6):876-899. [DOI] [PubMed] [Google Scholar]
- 13.Eysturoy AN, Skov L, Debes NM. Genetic predisposition increases the tic severity, rate of comorbidities, and psychosocial and educational difficulties in children with Tourette syndrome. J Child Neurol. 2015;30(3):320-325. [DOI] [PubMed] [Google Scholar]
- 14.Shady GA, Fulton WA, Champion LM. Tourette syndrome and educational problems in Canada. Neurosci Biobehav Rev. 1988;12(3-4):263-265. [DOI] [PubMed] [Google Scholar]
- 15.Wadman R, Glazebrook C, Beer C, Jackson GM. Difficulties experienced by young people with Tourette syndrome in secondary school: a mixed methods description of self, parent and staff perspectives. BMC Psychiatry. 2016;16:14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Chalita PJ, Palacios L, Cortes JF, Landeros-Weisenberger A, Panza KE, Bloch MH. Relationship of dropout and psychopathology in a high school sample in Mexico. Front Psychiatry. 2012;3:20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Wei MH. The social adjustment, academic performance, and creativity of Taiwanese children with Tourette’s syndrome. Psychol Rep. 2011;108(3):791-798. [DOI] [PubMed] [Google Scholar]
- 18.Leckman JF, Zhang H, Vitale A, et al. . Course of tic severity in Tourette syndrome: the first two decades. Pediatrics. 1998;102(1, pt 1):14-19. [DOI] [PubMed] [Google Scholar]
- 19.Ludvigsson JF, Otterblad-Olausson P, Pettersson BU, Ekbom A. The Swedish personal identity number: possibilities and pitfalls in healthcare and medical research. Eur J Epidemiol. 2009;24(11):659-667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.The Swedish National Agency for Education National School Register 2017. https://www.skolverket.se. Published 2017. Accessed December 20, 2017.
- 21.Statistics Sweden Longitudinell Integrationsdatabas för Sjukförsäkrings- och Arbetmsmarknadsstudier (LISA) http://www.scb.se/sv_/Vara-tjanster/Bestalla-mikrodata/Vilka-mikrodata-finns/Longitudinell-integrationsdatabas-for-sjukforsakrings–och-arbetsmarknadsstudier-LISA/. Accessed December 20, 2017.
- 22.Ludvigsson JF, Andersson E, Ekbom A, et al. . External review and validation of the Swedish national inpatient register. BMC Public Health. 2011;11:450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Ekbom A. The Swedish Multi-generation Register. Methods Mol Biol. 2011;675:215-220. [DOI] [PubMed] [Google Scholar]
- 24.Ludvigsson JF, Almqvist C, Bonamy AK, et al. . Registers of the Swedish total population and their use in medical research. Eur J Epidemiol. 2016;31(2):125-136. [DOI] [PubMed] [Google Scholar]
- 25.Socialstyrelsen. Cause of death: 2013. http://www.socialstyrelsen.se/statistics/statisticaldatabase/help/causeofdeath. Published 2014. Accessed December 20, 2017.
- 26.Pérez-Vigil A, Fernández de la Cruz L, Brander G, et al. . Association of obsessive-compulsive disorder with objective indicators of educational attainment: a nationwide register-based sibling control study. JAMA Psychiatry. 2018;75(1):47-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Niederkrotenthaler T, Tinghög P, Alexanderson K, et al. . Future risk of labour market marginalization in young suicide attempters—a population-based prospective cohort study. Int J Epidemiol. 2014;43(5):1520-1530. [DOI] [PubMed] [Google Scholar]
- 28.Rück C, Larsson KJ, Lind K, et al. . Validity and reliability of chronic tic disorder and obsessive-compulsive disorder diagnoses in the Swedish National Patient Register. BMJ Open. 2015;5(6):e007520. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Brander G, Rydell M, Kuja-Halkola R, et al. . Perinatal risk factors in Tourette’s and chronic tic disorders: a total population sibling comparison study [published online March 27, 2018]. Mol Psychiatry. doi: 10.1038/mp.2017.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Allison PD. Fixed Effects Regression Models. Thousand Oaks, CA: Sage Publications; 2009. [Google Scholar]
- 31.Bloch MH, Peterson BS, Scahill L, et al. . Adulthood outcome of tic and obsessive-compulsive symptom severity in children with Tourette syndrome. Arch Pediatr Adolesc Med. 2006;160(1):65-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Leckman JF, Bloch MH, Scahill L, King RA. Tourette syndrome: the self under siege. J Child Neurol. 2006;21(8):642-649. [DOI] [PubMed] [Google Scholar]
- 33.Mataix-Cols D, Isomura K, Pérez-Vigil A, et al. . Familial risks of Tourette Syndrome and chronic tic disorders. a population-based cohort study. JAMA Psychiatry. 2015;72(8):787-793. [DOI] [PubMed] [Google Scholar]
- 34.Shakeshaft NG, Trzaskowski M, McMillan A, et al. . Strong genetic influence on a UK nationwide test of educational achievement at the end of compulsory education at age 16. PLoS One. 2013;8(12):e80341. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Pettersson E, Anckarsäter H, Gillberg C, Lichtenstein P. Different neurodevelopmental symptoms have a common genetic etiology. J Child Psychol Psychiatry. 2013;54(12):1356-1365. [DOI] [PubMed] [Google Scholar]
- 36.Pettersson E, Larsson H, Lichtenstein P. Common psychiatric disorders share the same genetic origin: a multivariate sibling study of the Swedish population. Mol Psychiatry. 2016;21(5):717-721. [DOI] [PubMed] [Google Scholar]
- 37.Pinto R, Monzani B, Leckman JF, et al. . Understanding the covariation of tics, attention-deficit/hyperactivity, and obsessive-compulsive symptoms: A population-based adult twin study. Am J Med Genet B Neuropsychiatr Genet. 2016;171(7):938-947. [DOI] [PubMed] [Google Scholar]
- 38.Sacks O. An Anthropologist on Mars: Seven Paradoxical Tales. New York, NY: Alfred A. Knopf; 1996. [Google Scholar]
- 39.Barber L. An Unlikely Strength: Tourette Syndrome and the Search for Happiness in 60 Voices. New York, NY: SQ Press; 2016. [Google Scholar]
- 40.D’Onofrio BM, Lahey BB, Turkheimer E, Lichtenstein P. Critical need for family-based, quasi-experimental designs in integrating genetic and social science research. Am J Public Health. 2013;103(suppl 1):S46-S55. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. ICD codes used in the study.
eTable 2. Sensitivity analyses (1).
eTable 3. Sensitivity analyses (2).