Overview
Introduction
The open posterior approach to the knee to address avulsion fractures of the posterior cruciate ligament (PCL) at its tibial insertion utilizes the interval between the gastrocnemius and semimembranosus muscles to access the knee capsule while protecting the popliteal neurovascular structures.
Indications & Contraindications
Step-by-Step Description of Procedure
Step 1: Patient Positioning
Place the patient prone with the osseous prominences well padded.
Step 2: Surgical Exposure
Make an L-shaped skin incision and develop the interval between the gastrocnemius and semimembranosus bluntly (Video 4).
Step 3: Capsular Incision
Step 4: Osseous Bed Preparation
Examine the osseous fragment(s) to assess for the appropriate method of fixation and remove all debris (Video 5).
Step 5: Fracture Reduction
Perform reduction and provisional fixation (Fig. 5 and Video 5).
Step 6: Fracture Fixation
Step 7: Closure
Irrigate the wound and then perform layered closure of the capsule, subcutaneous tissues, and skin.
Step 8: Postoperative Care and Rehabilitation
Apply a specialized long leg, hinged knee brace and lock it in extension.
Results
An avulsion injury of the tibial attachment of the PCL continues to be a problem requiring surgery, and our systematic review data3 demonstrated satisfactory complication rates and outcomes with both open and arthroscopic surgical approaches in the majority of cases.
Pitfalls & Challenges
Abstract
Background:
The true prevalence of displaced tibial-sided avulsion injuries of the posterior cruciate ligament (PCL; Video 1) is unknown, and the majority of data regarding management has been published in areas other than the Western world, such as China and India (perhaps due to the higher prevalence of two-wheeler motorcycle accidents in these areas). Despite the rarity of data, a better understanding of the approach, fixation techniques, and outcomes is necessary to provide quality patient care. These injuries generally require surgical intervention as nonoperative management leads to complications—specifically, knee arthrofibrosis1,2. There is no consensus regarding the optimal surgical approach for these injuries. A recent systematic review demonstrated that both open and arthroscopic surgical treatment provide satisfactory complication rates and outcomes in the majority of cases3. However, the arthroscopic approach can be performed by only a highly skilled arthroscopist; thus, in this article we focus on the open approach to reach a broader audience of capable surgeons.
Description:
The principal steps for open reduction and internal fixation of the tibial avulsion fracture include the following:
Place the patient in a prone position and utilize a curvilinear L-shaped incision with the longitudinal portion over the medial head of the gastrocnemius muscle and the transverse portion starting distal to the joint line and extending laterally past the midline.
Develop the interval between the semimembranosus and medial gastrocnemius muscles, as originally described by Burks and Schaffer4. Lateral retraction of the gastrocnemius muscle exposes the posterior aspect of the capsule, allowing for a vertical capsular incision to adequately visualize the avulsed osseous fragment.
Prepare the osseous bed and remove hematoma and/or debris.
Reduce the avulsed fragment and obtain provisional fixation with Kirschner wires.
Confirm reduction under fluoroscopy with emphasis on sagittal plane alignment.
Obtain definitive fixation with the method dictated by the fracture orientation. Options include screw(s) with or without a washer, sutures, Kirschner wires, staples, and toothed plates2,5-7.
Alternatives:
An arthroscopic approach can be performed, with results that are similar to those of an open procedure, but considerable expertise is required to perform this procedure arthroscopically. Nonsurgical management is not recommended as it frequently leads to loss of knee motion.
Rationale:
The exact operative indications for PCL injuries remain in question, but we believe that displaced tibial avulsion injuries at the PCL attachment always require operative treatment.
Introductory Statement
The open posterior approach to the knee to address avulsion fractures of the posterior cruciate ligament (PCL) at its tibial insertion utilizes the interval between the gastrocnemius and semimembranosus muscles to access the knee capsule while protecting the popliteal neurovascular structures.
Indications & Contraindications (Video 2)
Video 1.
PCL anatomy and function.
Video 2.
Indications for surgical treatment of a PCL tibial avulsion fracture.
Indications
Displaced PCL tibial-sided avulsion fractures (Figs. 1-A, 1-B, and 2). There is no known amount of displacement for which nonoperative treatment is acceptable.
Fig. 1-A.
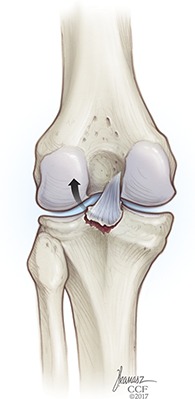
Anterior depiction of a PCL tibial avulsion fracture. Reproduced with permission, Cleveland Clinic Center for Medical Art & Photography © 2018. All rights reserved.
Fig. 1-B.

Lateral depiction of a PCL tibial avulsion fracture. Reproduced with permission, Cleveland Clinic Center for Medical Art & Photography © 2018. All rights reserved.
Fig. 2.
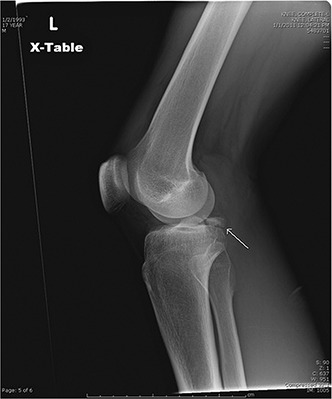
Lateral radiograph of a knee with a PCL tibial avulsion fracture (arrow).
Contraindications
Nondisplaced PCL tibial-sided avulsion fractures.
Moderate or severe preexisting knee osteoarthritis.
Low-demand or elderly patient.
Step-by-Step Description of Procedure (Video 3)
Video 3.
Overview of the surgical procedure for treatment of a PCL tibial avulsion fracture.
Step 1: Patient Positioning
Place the patient prone with the osseous prominences well padded.
Place the patient in the standard prone position.
Ensure that all osseous prominences are well padded.
Apply a tourniquet to the proximal part of the thigh of the affected extremity with the knee in 30° of flexion.
Step 2: Surgical Exposure
Make an L-shaped skin incision and develop the interval between the gastrocnemius and semimembranosus bluntly (Video 4).
Identify and mark the popliteal crease (Fig. 3).
Make the skin incision in an inverted-L fashion over the posteromedial corner of the knee joint with the vertical component at the medial edge of the gastrocnemius muscle and the transverse component just distal to the joint line.
Once through the skin and subcutaneous tissues, incise the fascia overlying the medial border of the gastrocnemius longitudinally.
Develop the interval between the gastrocnemius and semimembranosus bluntly with subsequent retraction of the gastrocnemius laterally, allowing for protection of the popliteal neurovascular structures and exposure of the posterior aspect of the capsule.
Fig. 3.

Intraoperative photograph with the skin incision marked over the popliteal fossa.
Video 4.
Posterior approach to the knee and exposure of the fracture fragment.
Step 3: Capsular Incision
Make a vertical capsular incision (Fig. 4 and Video 4).
Palpate the PCL facet, which lies just proximal to the popliteus muscle belly. The avulsed osseous fragment can create variability at this point as the PCL can draw the insertion site proximally and anteriorly, making palpation through the capsule difficult.
Make a vertical midline incision through the oblique popliteal ligament and posterior aspect of the capsule and lateral to the posterior attachment of the medial meniscus, exposing the osseous structures of the knee, including the tibial attachment of the PCL.
Fig. 4.
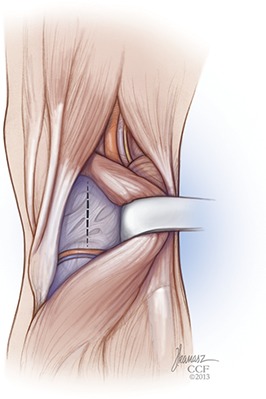
Illustration of the vertical capsulotomy incision used to access the osseous avulsion fracture. Reproduced with permission, Cleveland Clinic Center for Medical Art & Photography © 2018. All rights reserved.
Step 4: Osseous Bed Preparation
Examine the osseous fragment(s) to assess for the appropriate method of fixation and remove all debris (Video 5).
Remove any soft tissue or blood clots adherent to the fragment and, in cases of chronic injury, completely debride granulation tissue on both the osseous fragment and the posterior tibial rim to render a fresh osseous bed.
Determine the method of fixation as dictated by the fracture orientation; options include screw(s) with or without a washer, sutures, Kirschner wires, staples, and toothed plates.
Video 5.
Fixation of the fracture fragment with a partially threaded cannulated screw and washer.
Step 5: Fracture Reduction
Perform reduction and provisional fixation (Fig. 5 and Video 5).
Obtain provisional fixation with Kirschner wire(s) placed in an orthogonal orientation to the fracture line (if this is possible and the fracture is noncomminuted).
Reduction can be aided by an anterior drawer force on the tibia relaxing the PCL.
Assess for anatomic alignment with fluoroscopic examination, especially in the sagittal plane.
Fig. 5.

Lateral radiograph showing preliminary fixation of the PCL tibial avulsion fracture.
Step 6: Fracture Fixation
Initiate permanent fixation (Fig. 6 and Video 5).
Initiate permanent fixation in a standard AO fashion with appropriate drilling, measurement, and placement of a 4.0 or 6.5-mm partially threaded, cannulated cancellous screw, dependent on the size of the avulsed fragment. Using a washer as well can help to capture more comminuted fragments and/or improve osseous purchase. If the fragment is especially comminuted, alternative methods for fixation can be utilized, specifically sutures or toothed plates.
Again confirm anatomic reduction with fluoroscopy, and assess stability with gentle posterior drawer testing.
Fig. 6.

Lateral radiograph showing definitive screw fixation of the PCL tibial avulsion fracture.
Step 7: Closure
Irrigate the wound and then perform layered closure of the capsule, subcutaneous tissues, and skin.
Step 8: Postoperative Care and Rehabilitation
Apply a specialized long leg, hinged knee brace and lock it in extension.
Apply a specialized long leg, hinged knee brace and lock it in extension to keep the tibia translated anteriorly and shield the PCL from stress.
On postoperative day 1, initiate active range of motion as tolerated and gentle passive range of motion at near terminal extension (0° to 40°) with isometric quadriceps, hamstrings, and hip exercises.
Weight-bearing is permitted as tolerated with the brace locked in extension, once the regional anesthetic block has lost effect.
The patient continues with outpatient physical therapy with initiation of closed-chain quadriceps strengthening at 2 weeks and avoidance of active hamstring activation for 6 weeks.
Full weight-bearing without a brace is allowed at 6 weeks, and a progressive running program can start as soon as 3 months after surgery.
Results
An avulsion injury of the tibial attachment of the PCL continues to be a problem requiring surgery, and our systematic review data3 demonstrated satisfactory complication rates and outcomes with both open and arthroscopic surgical approaches in the majority of cases. The open procedure, in our opinion, remains the standard of care and can be used by a greater proportion of orthopaedic surgeons. We found that arthrofibrosis remains the most common complication, with a rate of 0% to 25% with the open posterior approach to the knee, and 65.9% of patients treated with that approach had a grade-A outcome score according the International Knee Documentation Committee (IKDC) system.
Pitfalls & Challenges
Our technique requires an understanding of the anatomy about the posterior aspect of the knee, an area unfrequented by many orthopaedic surgeons.
Partial release of the medial gastrocnemius muscle can aid in lateral retraction in order to expose the site of capsular arthrotomy. In our experience, this is usually not necessary.
Osseous avulsion injuries at the tibial attachment of the PCL can be comminuted and not amenable to screw fixation. The orthopaedic surgeon must be prepared to address this pathological condition with sutures and potentially bone tunnels (that technique is not described here).
Often these injuries are “high energy,” and attention must be paid to potential concomitant pathology. If there are associated injuries that can be addressed arthroscopically, such as meniscal tears, the arthroscopy should be performed prior to the open approach as fluid may extravasate through the posterior capsular incision into the lower leg.
Ligamentous plastic deformation has been described, but evidence regarding its existence is conflicting.
Our systematic review3 demonstrated good results with internal fixation through an open approach.
Footnotes
Published outcomes of this procedure can be found at: Am J Sports Med. 2017 Apr 1:363546517701911. [Epub ahead of print].
Investigation performed at the Cleveland Clinic Foundation, Cleveland, Ohio
Disclosure: The authors indicated that no external funding was received for any aspect of this work. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSEST/A204).
References
- 1.Montgomery SR, Johnson JS, McAllister DR, Petrigliano FA. Surgical management of PCL injuries: indications, techniques, and outcomes. Curr Rev Musculoskelet Med. 2013. June;6(2):115-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Torisu T. Isolated avulsion fracture of the tibial attachment of the posterior cruciate ligament. J Bone Joint Surg Am. 1977. January;59(1):68-72. [PubMed] [Google Scholar]
- 3.Hooper PO, 3rd, Silko C, Malcolm TL, Farrow LD. Management of posterior cruciate ligament tibial avulsion injuries: a systematic review. Am J Sports Med. 2017. April 1:363546517701911. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 4.Burks RT, Schaffer JJ. A simplified approach to the tibial attachment of the posterior cruciate ligament. Clin Orthop Relat Res. 1990. May;254:216-9. [PubMed] [Google Scholar]
- 5.Chen W, Luo W, Chen Z, Jiang Y. Treatment of posterior cruciate ligament avulsion fractures of the tibia using a toothed plate and hollow lag screw. Singapore Med J. 2016. January;57(1):39-44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Meyers MH. Isolated avulsion of the tibial attachment of the posterior cruciate ligament of the knee. J Bone Joint Surg Am. 1975. July;57(5):669-72. [PubMed] [Google Scholar]
- 7.Seitz H, Schlenz I, Pajenda G, Vécsei V. Tibial avulsion fracture of the posterior cruciate ligament: K-wire or screw fixation? A retrospective study of 26 patients. Arch Orthop Trauma Surg. 1997;116(5):275-8. [DOI] [PubMed] [Google Scholar]


