Abstract
BACKGROUND:
In the Veterans Health Administration (VHA) there is growing interest in the use of non-pharmacologic treatment (NPT) for low back pain (LBP) as pain intensity and interference do not decrease with opioid use.
OBJECTIVES:
To describe overall and facility-level variation in the extent to which specific NPT modalities are used in VHA for LBP, either alone or as adjuncts to opioid medications, and to understand associations between veterans’ clinical and demographic characteristics and type of treatment.
RESEARCH DESIGN:
Our retrospective cohort study examined use of opioids and 21 specific NPT modalities used by veterans.
SUBJECTS:
VHA-enrolled Iraq and Afghanistan veterans who utilized care in (“linked” to) 130 VHA facilities within 12 months after their separation from the Army between fiscal years 2008–11, and who were diagnosed with LBP within 12 months after linkage (n=49,885).
MEASURES:
Measures included per patient: days’ supply of opioids, number of visits for NPT modalities, and pain scores within one year after a LBP diagnosis.
RESULTS:
Thirty-four percent of veterans filled a prescription for opioids, 35% utilized at least one NPT modality, and 15% used both within the same year. Most patients with LBP receiving NPT, on average, had moderate pain (36%), followed by low pain (27%), and severe pain (15%), no pain (11%). Eleven percent had no pain scores recorded.
CONCLUSIONS:
About 65% of VHA patients with a LBP diagnosis did not receive NPT, and about 43% of NPT users also were prescribed an opioid. Understanding utilization patterns and their relationship with patient characteristics can guide pain management decisions and future study.
Keywords: low back pain, non-pharmacologic treatment, opioids
INTRODUCTION
The problem of acute and chronic pain in the United States is so immense that it has been labeled a public health crisis.1 As with civilian healthcare systems, a focus on pain management has become a high priority for the Military Health System (MHS) and Veterans Health Administration (VHA), as chronic pain diagnoses have increased among soldiers in recent years.2 There has been an influx of new enrollees with a high prevalence of pain to VHA from MHS. The majority of veterans returning from conflicts in Iraq and Afghanistan report chronic pain to their primary care provider.3
There is currently an effort to move away from using opioids for the treatment of pain.4 Specifically for veterans, the Comprehensive Addiction and Recovery Act (CARA) of 2016 and VA’s response recommends non-pharmacologic pain management and cautions against opioid pain management. This is due to the fact that pain intensity often does not decrease with opioid use5, does not produce better clinical results than non-opioids,6 and because of opioids’ addictive nature, side effects, and potential for adverse events, including overdose.7 Due to these negative effects of opioids, there is growing interest in the use of non-pharmacologic treatment (NPT) modalities to treat pain. To date, there is mixed evidence on the effectiveness of various forms of NPT to treat pain. For example, the VA’s Evidence Synthesis Program found heterogeneity in results for spinal manipulative therapy for the treatment of lower back pain (LBP)8 and of massage for back pain.9
A previous report documented that most VHA facilities provide complementary and alternative medicine (CAM) and that back pain is the fifth most common condition treated with CAM at VHA.10 In that survey, the most commonly reported CAM modalities reported by facilities included, in descending order: medication, stress management relaxation therapy, guided imagery, progressive muscle relaxation, biofeedback, animal-assisted therapy, music therapy, acupuncture, yoga, and hypnosis/hypnotherapy.11 These therapies were most commonly provided by midlevel providers, including nurse practitioners, clinical nurse specialists, and physician assistants, followed by psychologists, physicians, and CAM-specific providers.
Despite the contributions of this survey and other studies, there is still limited literature on the types of NPT used for specific types of pain,12,13 including commonly occurring LBP – with Army soldiers at greater risk for LBP than other service branches (Air Force, Navy, and Marines)14. Furthermore, the use of NPT or opioids by themselves or in conjunction with one another is not well understood, including any association with pain severity. A deep understanding of utilization patterns and relationships with clinical and demographic characteristics can help guide desired changes in pain management and future study. Our study examined specific NPT modalities used for LBP, overall and facility-level utilization of NPT, distributions of use per patient, concurrent NPT use with opioids, and associated numeric rating scale (NRS) pain scores. In this study, NPT includes CAM and other modalities, and does not include invasive treatments (e.g., surgery, injection).
METHODS
The current study is part of a grant funded by the National Center for Complementary and Integrative Health (NCCIH; R01AT008404) – “Longitudinal Study of Post-Deployment CAM Pain Management using DoD [Department of Defense] & VA Data”, which is examining the prevalence of postdeployment chronic pain, whether NPT is used as a complement or substitute for prescription opioids, and if NPT is associated with any improvements in health outcomes. In the study reported here, we examined the use of opioids and 21 specific NPTs delivered by health practitioners in the VHA to veterans within one year after a LBP diagnosis. The institutional review board process was completed at Brandeis University, Stanford University, and the Human Research Protection Program of the Under Secretary of Defense for Personnel and Readiness.
Sample
The MHS data sampling frame includes 643,205 Army soldiers who returned from deployments during fiscal years (FY) 2008–11.15 Of those, 299,145 Army soldiers demobilized (Reserve or National Guard) or separated (Active Duty) from the Army during FY2008–11. Of those 299,145 Army soldiers, 153,008 (51%) enrolled and utilized care in (“linked” to) VHA within 12 months after demobilization or separation. Of those, 49,885 (32%) had a LBP diagnosis. Thus, our cohort consisted of Army Active Duty, National Guard, and Reserve soldiers who returned from deployments to Iraq or Afghanistan between FY2008–11 who linked to VHA within 12 months after their demobilization/separation, and who were diagnosed with LBP within 12 months after linkage (n=49,885) (Figure 1). These individuals were treated in 130 of VHA’s medical centers. LBP diagnoses were identified using International Classification of Diseases Ninth Revision (ICD-9) codes 720–724 (except 720.0, 723.4, 723.8) and 756.1.16,17
Figure 1.
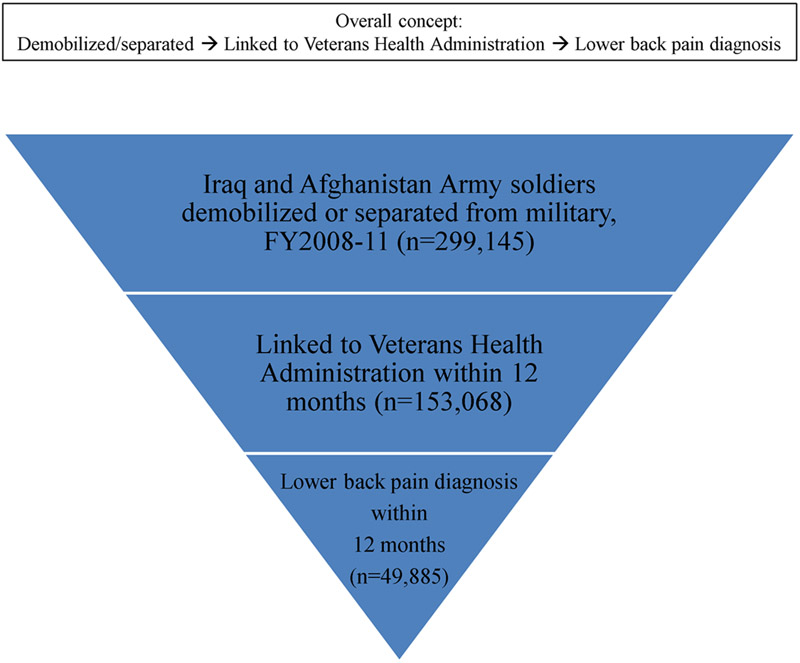
Lower Back Pain Sample
Data Sources
Veterans’ separation and demobilization dates were identified using data obtained from the Defense Manpower Data Center. The index deployment, defined as a deployment ending in FY2008–11, was identified in the Contingency Tracking System. Healthcare enrollment and utilization data came from the VHA’s electronic healthcare records, which are available in the VHA’s Corporate Data Warehouse (CDW). Specifically, we extracted diagnosis, procedures, prescription medication, and pain scores, and the station and date where these were recorded. We included inpatient and outpatient records for veterans who were alive during our observation window. We excluded VHA purchased care, that is care paid for by VHA, but provided through community providers, because a previous study showed that it was rarely used for alternative medicine services by Iraq and Afghanistan veterans18. We included all filled prescriptions for opioids in VHA, which included: buprenorphine, butorphanol, codeine, dihydrocodeine, fentanyl, hydrocodone, hydromorphone, levorphanol, meperidine, methadone, morphine, oxycodone, oxymorphone, pentazocine, propoxyphene, tapentadol, and tramadol. Twenty-one NPT modalities were identified with ICD-9, Current Procedural Terminology (CPT) and Healthcare Common Procedure Coding System (HCPCS) codes (see Table A (Appendix).
NPT and Opioid Measures
Measures were constructed from VHA healthcare data within one year after a LBP diagnosis for each cohort member and included: days per year with an opioid prescription; number of cohort members by NPT modality; number of facilities by NPT modality; overall NPT penetration rate; facility-level penetration rate by NPT modality; number of cohort members with both opioid treatment and NPT; average of NRS pain scores across NPT modalities; average of NRS pain scores within each NPT modality; range of NRS pain scores across NPT modalities; range of NRS pain scores within NPT modalities; and change in NRS pain scores.
Days per year with an opioid prescription was calculated as days’ supply of opioids that was dispensed to a cohort member in VHA in the year following a LBP diagnosis. Multiple opioid prescriptions could occur on a single day.
Number of cohort members by NPT modality included the number of cohort members using each type of NPT in either outpatient or inpatient settings. The LBP diagnosis had to occur in the same NPT outpatient visit or inpatient stay, within one year after linkage to VHA. In constructing our indicator for receipt of NPT, we used a broad range of procedures for active self-care, complementary and integrative approaches to pain management identified in literature reviews,19,20 supplemented with procedure codes based on our own review, including several seminal military and veteran reports10,21,22.
Number of facilities by NPT modality included the number of facilities, out of 130 that provided NPT, in which each of the NPT modalities was used by at least one cohort member during the year following a LBP diagnosis.
Overall NPT penetration rate indicated the portion of cohort members in a facility who received any type of NPT treatment. This penetration rate was standardized to the number of cohort members in each facility.
Facility-level penetration rate by NPT modality indicated the portion of cohort members in a facility who received a particular NPT. These penetration rates were standardized to the number of cohort members with LBP in each facility.
Number of cohort members with both opioid treatment and NPT included cohort members who used both opioids and NPT in the year following a LBP diagnosis.
Average of NRS pain scores across NPT modalities was calculated by taking the mean of each cohort member’s NRS pain scores. NRS pain scores ranged from 0–10. The Defense and Veterans Pain Rating Scale, which uses the NRS as its foundation, describes scores of 0 as “no pain,” 1 as “hardly notice pain,” 2 as “notice pain, does not interfere with activities,” 3 as “sometimes distracts me,” 4 as “distracts me, can do usual activities,” 5 as “interrupts some activities,” 6 as “hard to ignore, avoid usual activities,” 7 as “focus of attention, prevents doing daily activities,” 8 as “awful, hard to do anything,” 9 as “can’t bear the pain, unable to do anything,” and 10 as “as bad as it could be, nothing else matters.” NRS pain scores were used in the calculation only if they were collected during an outpatient visit or inpatient stay with a LBP diagnosis to maximize the chance that the pain score was related to LBP. A very small portion (1%) of our cohort members had more than 18 back pain diagnoses with associated pain scores; we excluded these individuals from our analysis as they were not representative of the rest of our sample. For the purpose of interpretability, we categorized NRS pain scores as low (1–3), moderate (4–6), and severe (7–10).23
Average of NRS pain scores within each NPT modality was calculated in the same manner as the average across NPT modalities, with one exception – that the NRS pain score had to be collected during the same outpatient visit or inpatient stay as the particular NPT modality that was received.
Range of NRS pain scores across NPT modalities was calculated by taking the maximum value of each patient’s NRS pain scores and subtracting the minimum of that same patient’s NRS pain scores. Thus, NRS pain scores ranged from 0 to 10.
Range of NRS pain scores within NPT modalities was calculated in the same manner as the range across NPT modalities, with one exception – that the NRS pain score had to be collected during the same outpatient visit or inpatient stay as the particular NPT modality.
Change in NRS pain scores was determined by subtracting the last registered pain score from the first registered pain score.
Demographic Measures
Age, sex, marital status, race/ethnicity, component, rank, number of deployments before index deployment, and cohort (i.e., year of index deployment end date) were derived from the Contingency Tracking System of the Defense Manpower Data Center and the Defense Enrollment Eligibility Reporting System.
Analysis
Descriptive statistics (i.e., sums, proportions, means, and ranges) were calculated for variables described in the NPT and Opioid Measures section. Crosstabs and accompanying ANOVAs or chi-2 tests were calculated for these NPT and Opioid Measures by the Clinical and Demographic Measures. We also ran a mixed-effects logistic regression model to predict receipt of any NPT and/or opioids (yes/no), with a random effect for facility to account for clustering of members within a facility.
RESULTS
From FY2008 to FY2011, 153,068 of the 299,145 (51%) Iraq and Afghanistan soldiers who had demobilized or separated from the military, linked to VHA within 12 months after demobilization or separation, a rate similar to that found in other studies (Figure 1).24,25 Of those who linked, 49,885 (32%) had a LBP diagnosis within 12 months of linkage.
Of the 49,885 veterans in our study with LBP diagnosis, 34% filled at least one prescription for opioids, 35% utilized at least one NPT modality, and 15% used both within one year after a LBP diagnosis. NPT users were more frequently prescribed opioids than those who did not use NPT – 43% versus 29%, respectively. Additionally, veterans receiving NPT were supplied opioids for more days during the year after diagnosis than veterans without NPT (median 60 vs. 40 days). Compared to veterans without NPT, more veterans with NPT received opioid supplies for three months or longer (39% vs. 29%), whereas fewer veterans with NPT received opioids for one month or less (37% vs. 47%). No differences were observed between the NPT and no NPT groups for one-to-two month opioid supplies (both 14%) or for two-to-three month opioid supplies (both 9%).
There was considerable range in the portion of patients that used any NPT modality, the portion of facilities that delivered a particular NPT modality, and the penetration rate of a NPT modality at the facility-level (Table 1). Any given NPT modality was used by 0 to 17% of our cohort. Some NPT modalities were used at nearly all VHA facilities while others were used at few or no locations. For example, the NPT modality in most frequent use at the facility-level was exercise therapy (99%), while Christian Science practitioner and monochromatic infrared energy (MIRE) modalities were not delivered at any VHA facilities. Penetration rates, or the portion of patients with a LBP receiving NPT, also ranged considerably. For any NPT use, the minimum penetration rate was 8% and the maximum penetration rate was 77% for a facility. Facility-level penetration rates, or the portion of patients with a LBP receiving treatment in a facility, also ranged considerably by NPT modality. For example, the lowest facility-level penetration rates were for biofeedback and cold laser at less than 1%, and the highest facility-level penetration rate was for self-management at over 70%.
Table 1.
Cohort Members and Facilities Using Each NPT Modality
| NPT modality | No. (%) patients treated with NPT modalitya (N=49,885) |
No. (%) facilities using NPT modalitya (N=130) |
Minimum penetration rate (%) in a facility | Maximum penetration rate (%) in a facility |
|---|---|---|---|---|
| Any NPT modality | 17,484 (35.0) | 130 (100.0) | 16/197 (8.1) |
351/453 (77.5) |
| Acupuncture | 315 (.6) | 51 (39.2) | 1/1543 (0.1) |
60/387 (15.5) |
| Biofeedback | 31 (.1) | 19 (14.6) | 1/1543 (0.1) |
5/212 (2.4) |
| Chiropractic | 1218 (2.4) | 34 (26.1) | 2/732 (0.3) |
126/478 (26.4) |
| Christian Science practitioner | 0 (0) | N/A | N/A | N/A |
| Cold laser | 178 (.4) | 30 (23.1) | 1/1622 (0.1) |
56/251 (22.3) |
| Coordinated care | 4196 (8.3) | 128 (98.5) | 1/166 (0.6) |
32/122 (26.2) |
| Exercise therapy | 8715 (17.4) | 129 (99.2) | 4/281 (1.4) |
404/650 (62.1) |
| Hypnotherapy | 3 (.0) | 2 (1.5) | 1/901 (0.1) |
2/418 (0.5) |
| Lumbar supports | 390 (.8) | 43 (33.1) | 1/1164 (0.1) |
80/363 (22.0) |
| Massage | 2549 (5.1) | 117 (26.1) | 1/833 (0.1) |
39/120 (32.5) |
| Medical nutrition therapy | 309 (.6) | 26 (20.0) | 1/1207 (0.1) |
177/643 (27.5) |
| MIRE | 0 (0) | N/A | N/A | N/A |
| Occupational stress education /stress education | 1280 (2.6) | 90 (69.2) | 1/1164 (0.1) |
610/1543 (39.5) |
| Other physical therapy | 6988 (13.9) | 121 (93.1) | 1/498 (0.2) |
93/242 (38.4) |
| Recreational therapy | 78 (.2) | 26 (20.0) | 2/1534 (0.1) | 24/901 (2.7) |
| Self-management | 5743 (11.5) | 124 (95.4) | 1/251 (0.4) |
318/453 (70.2) |
| Spinal manipulation | 125 (.2) | 23 (17.7) | 2/1622 (0.1) | 34/581 (5.8) |
| Superficial heat | 2891 (5.8) | 122 (93.8) | 1/525 (0.2) |
69/328 (21.0) |
| TENS and other electrical modulation | 2711 (5.4) | 124 (95.4) | 1/643 (0.2) |
49/234 (20.9) |
| Traction | 1116 (2.2) | 113 (86.9) | 2/1543 (0.1) | 18/120 (15.0) |
| Ultrasound | 1320 (2.6) | 113 (86.9) | 1/732 (0.1) |
21/120 (17.5) |
Not mutually exclusive; veterans can use more than one NPT modality and multiple NPT modalities can be provided at each facility.
MIRE, monochromatic infrared energy; N/A, not applicable – when no patients were treated with the NPT modality; NPT, non-pharmacologic therapy; TENS, transcutaneous electrical nerve stimulation
The average NRS pain scores for the greatest portion of patients with LBP receiving NPT were moderate (36%), followed by low (27%), and severe (15%), and no pain (11%) scores; pain scores were missing for 4,837 patients (11%). This pattern held after excluding missing scores; the greatest portion of patients using NPT had moderate scores (33%), followed by low (26%), no pain (22%), and severe (20%) scores (Table 2). By NPT modality, patients with pain scores were most likely to have moderate pain, except for the cases of: biofeedback, where having no, low, or moderate pain were equally common; self-management where having low or moderate pain were equally common; coordinated care, where having severe pain was most common; and for stress education and medical nutrition therapy where having no pain was most common. However, it should be noted that there was a considerable amount of missing pain scores when we required that they be collected in the same visit as the particular NPT modality as opposed to across all NPT modalities; this is evidenced by comparing the number of patients by NPT modality in Table 1 and Table 2.
Table 2.
Pain Levela by NPT modality, for Patients with NRS Pain Scores
| NPT Modality | No. (%) no pain | No. (%) low pain | No. (%) moderate pain | No. (%) severe pain |
|---|---|---|---|---|
| Any NPT modality (n=6,031) | 1,307 (21.7) | 1,565 (25.9) | 1,970 (32.7) | 1,189 (19.7) |
| Acupuncture (n=79) | 12 (15.2) | 18 (22.8) | 29 (36.7) | 20 (25.3) |
| Biofeedback (n=7) | 2 (28.6) | 2 (28.6) | 2 (28.6) | 1 (14.3) |
| Chiropractic (n=47) | 47 (16.0) | 85 (29.0) | 114 (40.00) | 47 (16.0) |
| Christian Science practitioner (n=0) | N/A | N/A | N/A | N/A |
| Cold laser (n=24) | 3 (12.5) | 5 (20.8) | 11 (45.8) | 5 (20.8) |
| Coordinated care (n=653) | 79 (12.1) | 98 (15.0) | 218 (33.4) | 258 (39.8) |
| Exercise therapy (n=2,145) | 535 (24.9) | 585 (27.3) | 669 (31.2) | 356 (16.6) |
| Hypnotherapy (n=0) | N/A | N/A | N/A | N/A |
| Lumbar supports (n=182) | 39 (21.4) | 31 (17.0) | 58 (31.9) | 54 (29.7) |
| Massage (n=331) | 61 (18.4) | 98 (29.6) | 118 (35.6) | 54 (16.3) |
| Medical nutrition therapy (n=272) | 104 (38.2) | 60 (22.1) | 72 (26.5) | 36 (13.2) |
| MIRE (n=0) | N/A | N/A | N/A | N/A |
| Occupational stress education / Stress education (n=1,048) | 340 (32.4) | 318 (30.3) | 240 (22.9) | 156 (14.57) |
| Other physical therapy (n=1,230) | 190 (15.4) | 329 (26.7) | 438 (35.6) | 273 (22.2) |
| Recreational therapy (n=13) | 2 (15.4) | 4 (30.8) | 5 (38.5) | 2 (15.4) |
| Self-management (n=2,300) | 536 (23.3) | 676 (29.4) | 673 (29.3) | 415 (18.0) |
| Spinal manipulation (n=77) | 12 (15.6) | 18 (23.4) | 33 (42.9) | 15 (18.0) |
| Superficial heat (n=411) | 68 (16.5) | 101 (24.6) | 158 (38.4) | 84 (20.4) |
| Traction (n=132) | 18 (13.6) | 31 (23.5) | 52 (39.4) | 31 (23.5) |
| TENS and other electrical modulation (n=403) | 61 (15.1) | 97 (24.1) | 154 (38.2) | 91 (22.6) |
| Ultrasonography | 24 (14.1) | 49 (28.8) | 68 (40.0) | 29 (17.1) |
MIRE, monochromatic infrared energy; N/A, not applicable – when no patients had a NRS pain score associated with a particular NPT modality; NPT, non-pharmacologic therapy; NRS, numeric rating scale; TENS, transcutaneous electrical nerve stimulation.
Pain levels were assigned based on the average pain score.
When patients with missing NRS pain scores and only one pain score were excluded – since change in pain scores could not be assessed for this group – 44% of NPT users had NRS pain scores that did not change from first to last measurement (Table 3). For those patients with pain scores by NPT modality, the largest portion (between 32-100%) had unchanged pain scores, with the exceptions of chiropractic, massage, recreational therapy, superficial heat, and ultrasonography, where veterans experienced a decrease in NRS pain scores.
Table 3.
Change in NRS Pain Scores by NPT modality, for Patients with 2 or More Pain Scoresa
| NPT Modality | No. (%) decreased | No. (%) no change | No. (%) increased |
|---|---|---|---|
| Any NPT modality (n=2,073) | 639 (30.8) | 913 (44.0) | 521 (25.1) |
| Acupuncture (n=36) | 13 (36.1) | 15 (41.7) | 8 (22.2) |
| Biofeedback (n=1) | 1 (100.0) | 0 (0.0) | 0 (0.0) |
| Chiropractic (n=105) | 41 (39.0) | 34 (32.4) | 30 (28.6) |
| Christian Science practitioner (n=0) | N/A | N/A | N/A |
| Cold laser (n=4) | 0 (0.0) | 4 (100.0) | 0 (0.0) |
| Coordinated care (n=144) | 37 (25.7) | 84 (58.3) | 23 (16.0) |
| Exercise therapy (n=577) | 169 (29.3) | 296 (51.3) | 112 (19.4) |
| Hypnotherapy (n=0) | N/A | N/A | N/A |
| Lumbar supports (n=45) | 7 (15.6) | 33 (73.3) | 5 (11.1) |
| Massage (n=95) | 39 (41.1) | 29 (30.5) | 27 (28.4) |
| Medical nutrition therapy (n=40) | 13 (32.5) | 20 (50.0) | 7 (17.5) |
| MIRE (n=0) | N/A | N/A | N/A |
| Occupational stress education / Stress education (n=341) | 97 (28.4) | 151 (44.3) | 93 (27.3) |
| Other physical therapy (n=333) | 112 (33.6) | 136 (40.8) | 85 (25.5) |
| Recreational therapy (n=4) | 3 (75.0) | 0 (0.0) | 1 (25.0) |
| Self-management (n=664) | 185 (27.9) | 303 (45.6) | 176 (26.5) |
| Spinal manipulation (n=27) | 7 (25.9) | 15 (55.6) | 5 (18.5) |
| Superficial heat (n=123) | 48 (39.0) | 43 (35.0) | 32 (26.0) |
| Traction (n=38) | 13 (34.2) | 17 (44.7) | 8 (21.1) |
| TENS and other electrical modulation (n=86) | 26 (30.2) | 39 (45.3) | 21 (24.4) |
| Ultrasonography (n=40) | 18 (45.0) | 13 (32.5) | 9 (22.5) |
MIRE, monochromatic infrared energy; N/A, not applicable – when no patients had a NRS pain score associated with a particular NPT modality; NPT, non-pharmacologic therapy; NRS, numeric rating scale; TENS, transcutaneous electrical nerve stimulation.
Change was determined based on the difference between the first and the last pain score.
There were notable differences between clinical and demographic characteristics by NPT and opioid use as well as average pain score by demographic characteristics. Distributions of average pain level, age, marital status, race/ethnicity, component, rank, number of deployments before index deployment, and cohort differed significantly (p<.0001) by treatment status – NPT only, opioids only, or NPT & opioids (Appendix Table B). However, sex did not differ significantly by those categories (p=0.26). Notably, from the FY2008 to FY2011 cohort, the portion of veterans receiving neither NPT nor opioids & the portion of veterans receiving NPT only increased, while the portion of veterans with opioids only & the portion of veterans with NPT & opioids declined. The distribution of the aforementioned demographic characteristics also differed significantly by average pain level (Appendix Table C; p<.0001 for all except sex, where p<.01). In the mixed effect logistic regression predicting therapy (NPT and/or opioids) versus no therapy, veterans who were: older (OR=1.01); female (versus male; OR=1.07); and with low (OR=2.31), moderate (OR=3.64) or severe (OR=4.79) versus no pain were more likely to receive therapy (Table 4). Veterans who were: non-Hispanic African American (OR=0.90) versus non-Hispanic White; in the Guard (OR=0.83) or Reserve (OR=0.82) versus Active Duty components; higher ranks versus Junior Enlisted – senior enlisted (OR=0.81), junior officer (OR=0.59), senior officer (OR=0.56), and warrant officer (OR=0.65); with one deployment before index deployment (OR=0.93) versus none; and cohorts later than FY2008 – FY2009 (OR=0.94), FY2010 (OR=0.89), and FY2011 (OR=0.81) were less likely to receive therapy.
Table 4.
Clinical and Demographic Predictors of Treatment (Non-Pharmacologic and/or Opioid Treatment) for Army Veterans with Low Back Pain
| Army veterans with low back pain (N=44,937) |
||
|---|---|---|
| Characteristicsa | OR | 95% CI |
| Pain level (reference: none) | ||
| Low | 2.31 | 2.18-2.45 |
| Moderate | 3.64 | 3.44-3.85 |
| Severe | 4.79 | 4.46-5.13 |
| Age in years | 1.01 | 1.01-1.01 |
| Female (reference: male) | 1.07 | 1.00-1.15 |
| Married (reference: not married) | 1.02 | 0.98-1.06 |
| Race/Ethnicity (reference: Non-Hispanic White) | ||
| Non-Hispanic African American | 0.90 | 0.84-0.96 |
| Hispanic | 0.97 | 0.89-1.04 |
| Asian or Pacific Islander | 0.94 | 0.86-1.02 |
| American Indian/Alaska Native | 0.97 | 0.79-1.19 |
| Other | 0.84 | 0.64-1.10 |
| Component (reference: Active Duty) | ||
| Guard | 0.83 | 0.78-0.87 |
| Reserve | 0.82 | 0.77-0.88 |
| Rank (reference: Junior enlisted) | ||
| Senior enlisted | 0.81 | 0.77-0.86 |
| Junior officer | 0.59 | 0.53-0.67 |
| Senior officer | 0.56 | 0.48-0.65 |
| Warrant officer | 0.65 | 0.54-0.79 |
| Number of deployments before index deploymentb (reference: 0) | ||
| 1 | 0.93 | 0.89-0.97 |
| 2 or more | 0.98 | 0.91-1.06 |
| Cohortc (reference: 2008) | ||
| 2009 | 0.94 | 0.89-0.99 |
| 2010 | 0.89 | 0.84-0.94 |
| 2011 | 0.81 | 0.76-0.88 |
Measured at month before index deployment unless indicated.
Index refers to a deployment ending in FY2008-2011.
Cohort refers to fiscal year of index deployment end date.
CI = confidence interval; OR = odds ratio
DISCUSSION
Given increasing concern with the use of opioids and their frequent use for chronic pain,26 we examined the use of NPT for LBP in VHA. Approximately one-third of veterans with a LBP diagnosis used NPT, approximately one-third used opioids, and 15% used both within the same year. This rate of opioid use is consistent with a prevalence of 34% reported by Mosher et al. for FY2012 in their study of VHA primary care patients.27 With respect to NPT use in our study, the NPT modalities with the greatest number of users (e.g., exercise therapy, other physical therapy) were also the NPT modalities used at the greatest number of facilities.
While NPT was used frequently by veterans with LBP, there was variability in the use of different modalities at the individual and facility levels. Some NPT modalities were used by thousands of veterans throughout the US and at every or nearly every VHA facility (e.g., exercise therapy, other physical therapy), while others were infrequently used (e.g., biofeedback, hypnotherapy). More work should be done to investigate whether the utilization patterns we see here reflect the preferences of veterans for care, or if these patients are not aware of or do not have access to various treatments at their VHA facilities. Specifically, it has been difficult for VHA to hire acupuncturists and massage therapists since job descriptions and duties for acupuncturists were not officially formulated by the VHA until 2017 and those for massage therapists are still being formulated; thus, the maximum penetration rate per facility for those NPT modalities may be open to interpretation.
The bivariate and multivariate statistics presented demonstrate that there are differences in NPT and opioid use amongst Iraq and Afghanistan veterans by clinical and demographic characteristics. These data can be used to inform strategy if treatment changes are desired. For example, differences in rates of opioid use by race/ethnicity may not be desired, and outreach to certain communities may be important.
One limitation of this study is that we only calculated what was recorded as a procedure in VHA healthcare utilization data. For example, yoga was not counted. Other studies have used self-report or are using natural language processing (NLP) to examine NPT utilization, which likely pick up on more NPT utilization. Each approach has its strengths and weaknesses. Our study provides a conservative estimate of NPT utilization by using only procedure codes. Self-report studies on NPT are likely subject to social desirability bias, which would cause an overestimate of NPT use. For example, Denneson et al. found an 82% rate of CAM use,28 while our study found a 35% rate of NPT use. Those studies using NLP likely overestimate NPT utilization as NLP cannot assure that NPT services were offered in VHA versus outside VHA.29
Another limitation of this study is that pain scores were not studied in a longitudinal manner, precluding any causal signal between pain severity and NPT and/or opioid utilization. Our results could be extended by conducting an in-depth examination of the relationship between NPT and opioid use for pain. We found that a greater portion of veterans with LBP who used NPT also used opioids versus those who did not use NPT. This might be due to pain severity or treatment seeking behavior – that utilization of opioids led to utilization of NPT or vice versa. Understanding the order in which NPT and opioids are used as well as their individual and interactive impacts on pain would be informative. This is difficult to study, however, as pain scores (including in our study) may be partially or wholly related to the type of pain studied (e.g., LBP). Furthermore, NPT and opioids could have benefits for other health conditions; in other words, they could be used for LBP, but also benefit other health issues.
An additional limitation is that our study is not generalizable beyond the Iraq and Afghanistan Army veteran population. In other words, different patterns may be observed in veterans from different conflicts and/or different branches.
At present, data from the current study are useful for operational purposes. VHA can utilize this information to determine if specific NPT modalities for LBP should be expanded to more facilities, thereby increasing access. These data can also be used to inform surveys of veterans to assess their demand for non-pharmacological and pharmacological treatments for LBP. Given the variability in NPT utilization in VHA facilities, there is likely both unmet need and over-prescription of specific NPT modalities for LBP.
Supplementary Material
Acknowledgments
Funders: This study was funded by grant R01AT008404 from the NIH National Center for Complementary and Integrative Health (NCCIH), and built off grant R01DA030150 from the NIH National Institute on Drug Abuse (NIDA). Dr. Vanneman would like to acknowledge research support from the VA Office of Academic Affiliations as well as the University of Utah Health Enhancing Development-Generating Excellence (EDGE) Scholar and Vice President’s Clinical and Translational Scholars (VPCAT) programs. Dr. Harris is supported by a Research Career Scientist award (RCS-14–232) from the VA Health Services Research and Development Service.
Footnotes
Contributors: The authors acknowledge Kennell and Associates, Inc., for compiling data files used in these analyses. The Defense Health Agency’s Privacy and Civil Liberties Office provided access to DoD data. The opinions and assertions herein are those of the authors and do not necessarily reflect the official views of the VA, DoD, University of Utah, Brandeis University, Stanford University, NORC at the University of Chicago, National Institutes of Health (NIH), or NIH National Center for Complementary and Integrative Health (NCCIH).
Prior presentations: None.
Conflict of interest: Drs. Vanneman, Meerwijk, and Harris are employees of and Ms. Chen was an employee of the US Department of Veterans Affairs. No other conflict of interest exists for any of the authors.
REFERENCES
- 1.Carr DB. “Pain Is a Public Health Problem” --What Does That Mean and Why Should We Care? Pain Med. 2016;17(4):626–627. [DOI] [PubMed] [Google Scholar]
- 2.Clark LL, Taubman SB. Brief report: Incidence of diagnoses using ICD-9 codes specifying chronic pain (not neoplasm related) in the primary diagnostic position, active component, U.S. Armed Forces, 2007–2014. MSMR. 2015;22(12):12–15. [PubMed] [Google Scholar]
- 3.Lew HL, Otis JD, Tun C, Kerns RD, Clark ME, Cifu DX. Prevalence of chronic pain, posttraumatic stress disorder, and persistent postconcussive symptoms in OIF/OEF veterans: polytrauma clinical triad. J Rehabil Res Dev. 2009;46(6):697–702. [DOI] [PubMed] [Google Scholar]
- 4.Doctor J, Cowan P, Meeker D, Brukenthal P, Broderick J. Encouraging Integrative, Non-opioid Approaches to Pain: A Policy Agenda. Vol 2018: Health Affairs Blog; 2016. [Google Scholar]
- 5.Dobscha SK. Changes in pain intensity over time in a national cohort of older veterans: exploring associations of pain scores with prescription opioids Portland, OR: Center to Improve Veteran Involvement in Care;2015. [Google Scholar]
- 6.Krebs EE, Gravely A, Nugent S, et al. Effect of Opioid vs Nonopioid Medications on Pain-Related Function in Patients With Chronic Back Pain or Hip or Knee Osteoarthritis Pain: The SPACE Randomized Clinical Trial. JAMA. 2018;319(9):872–882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Bohnert AS, Ilgen MA, Trafton JA, et al. Trends and regional variation in opioid overdose mortality among Veterans Health Administration patients, fiscal year 2001 to 2009. Clin J Pain. 2014;30(7):605–612. [DOI] [PubMed] [Google Scholar]
- 8.Evidence-based Synthesis Program Center. The effectiveness and harms of spinal manipulative therapy for the treatment of acute neck and lower back pain: a systematic review. Los Angeles, CA: West Los Angeles VA Medical Center;2017. [PubMed] [Google Scholar]
- 9.Evidence-based Synthesis Program Center. Massage for pain: an evidence map. Los Angeles, CA: West Los Angeles VA Medical Center;2017. [Google Scholar]
- 10.Department of Veterans Affairs - Veterans Health Administration. Complementary and Alternative Medicine. 2011. [Google Scholar]
- 11.Ezeji-Okoye SC, Kotar TM, Smeeding SJ, Durfee JM. State of care: Complementary and alternative medicine in Veterans Health Administration—2011 Survey Results. Federal Practitioner; 2013:14–19. [Google Scholar]
- 12.Baldwin CM, Long K, Kroesen K, Brooks AJ, Bell IR. A profile of military veterans in the southwestern United States who use complementary and alternative medicine: implications for integrated care. Arch Intern Med. 2002;162(15):1697–1704. [DOI] [PubMed] [Google Scholar]
- 13.Reinhard MJ, Nassif TH, Bloeser K, et al. CAM utilization among OEF/OIF veterans: findings from the National Health Study for a New Generation of US Veterans. Med Care. 2014;52(12 Suppl 5): S45–49. [DOI] [PubMed] [Google Scholar]
- 14.Knox J, Orchowski J, Scher DL, Owens BD, Burks R, Belmont PJ. The incidence of low back pain in active duty United States military service members. Spine (Phila Pa 1976). 2011;36(18):1492–1500. [DOI] [PubMed] [Google Scholar]
- 15.Larson MJ, Adams RS, Mohr BA, et al. Rationale and methods of the Substance Use and Pyschological Injury Combat Study (SUPIC): a longitudinal study of Army service members returning from deployment in FY2008–11. Subst Abus. 2013;48(10):863–879. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Office of Healthcare Inspections. Healthcare inspection - VA patterns of dispensing take-home opioids and monitoring patients on opioid therapy. Washington, DC: Department of Veterans Affairs;2014. [Google Scholar]
- 17.Seal KH, Shi Y, Cohen G, et al. Association of mental health disorders with prescription opioids and high-risk opioid use in US veterans of Iraq and Afghanistan. JAMA. 2012;307(9):940–947. [DOI] [PubMed] [Google Scholar]
- 18.Vanneman ME, Harris AH, Asch SM, Scott WJ, Murrell SS, Wagner TH. Iraq and Afghanistan veterans’ use of Veterans Health Administration and purchased care before and after Veterans Choice Program implementation. Med Care. 2017;55(supply 7 suppl 1):S37–S44. [DOI] [PubMed] [Google Scholar]
- 19.Crawford C, Lee C, Freilich D. Effectiveness of active self-care complementary and integrative medicine therapies: options for the management of chronic pain symptoms. Pain Med. 2014;15 Suppl 1: S86–95. [DOI] [PubMed] [Google Scholar]
- 20.Delgado R, York A, Lee C, et al. Assessing the quality, efficacy, and effectiveness of the current evidence base of active self-care complementary and integrative medicine therapies for the management of chronic pain: a rapid evidence assessment of the literature. Pain Med. 2014;15 Suppl 1: S9–20. [DOI] [PubMed] [Google Scholar]
- 21.Department of Defense. Integrative Medicine in the Military Health System Report to Congress. 2013-2014. [Google Scholar]
- 22.Office of the Army Surgeon General. Pain Management Task Force: Providing a Standardized DoD and VHA Vision and Approach to Pain Management to Optimize the Care for Warriors and their Families. Final Report. 2010. [Google Scholar]
- 23.Goulet JL, Brandt C, Crystal S, et al. Agreement between electronic medical record-based and self-administered pain numeric rating scale: clinical and research implications. Med Care. 2013;51(3):245–250. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Harris AH, Chen C, Mohr BA, Adams RS, Williams TV, Larson MJ. Predictors of Army National Guard and Reserve members’ use of Veteran Health Administration health care after demobilizing from OEF/OIF deployment. Mil Med. 2014;179(10):1090–1098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Vanneman ME, Harris AH, Chen C, et al. Army active duty members’ linkage to Veterans Health Administration services after deployments to Iraq or Afghanistan and following separation. Mil Med. 2015;180(10):1052–1058. PMCID: PMC4625796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.The Opioid Therapy Chronic Pain Work Group. VA/DoD clinical practice guideline for opioid therapy for chronic pain. Washington, DC: Department of Veterans Affairs and Department of Defense;2017. [Google Scholar]
- 27.Mosher HJ, Krebs EE, Carrel M, Kaboli PJ, Weg MW, Lund BC. Trends in prevalent and incident opioid receipt: an observational study in Veterans Health Administration 2004–2012. J Gen Intern Med. 2015;30(5):597–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Denneson LM, Corson K, Dobscha SK. Complementary and alternative medicine use among veterans with chronic noncancer pain. J Rehabil Res Dev. 2011;48(9):1119–1128. [DOI] [PubMed] [Google Scholar]
- 29.Taylor SL, Herman P. The cost-effectiveness of complementary and alternative treatments to reduce pain. Washington, DC: The Department of Veterans Affairs;2017. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


