Abstract
Autism spectrum disorder (ASD) is a set of complex neurodevelopmental disorders. Recent studies reported that children with ASD have altered gut microbiota profiles compared with typical development (TD) children. However, few studies on gut bacteria of children with ASD have been conducted in China. Here, in order to elucidate changes of fecal microbiota in children with ASD, 16S rRNA sequencing was conducted and the 16S rRNA (V3-V4) gene tags were amplified. We investigated differences in fecal microbiota between 35 children with ASD and 6 TD children. At the phylum level, the fecal microbiota of ASD group indicated a significant increase of the Bacteroidetes/Firmicutes ratio. At the genus level, we found that the relative abundance of Sutterella, Odoribacter and Butyricimonas was much more abundant in the ASD group whereas the abundance of Veillonella and Streptococcus was decreased significantly compared to the control group. Functional analysis demonstrated that butyrate and lactate producers were less abundant in the ASD group. In addition, we downloaded the association data set of microbe–disease from human microbe–disease association database and constructed a human disease network including ASD using our gut microbiome results. In this microbe–disease network based on microbe similarity of diseases, we found that ASD is positively correlated with periodontal, negatively related to type 1 diabetes. Therefore, these results suggest that microbe-based disease analysis is able to predict novel connection between ASD and other diseases and may play a role in revealing the pathogenesis of ASD.
Introduction
Autism spectrum disorder (ASD) refers to a group of complex neurodevelopmental disorders with early life stage, characterized by deficits in social communication and by restricted and fixated behavior. A meta-analysis of the public health and primary care centers in the UK estimated that the prevalence of autism was 26.6 per 10,000 in mainland, based on eighteen epidemiological studies1. It is now well accepted that both genetic and environment factors are related to the aetiology of ASD2. Common non-neurological symptoms in ASD patients are gastrointestinal (GI) disorders3. Rigid-compulsive behaviors, unusual sleeping or eating habits and oppositional behavior were associated with GI disorders4,5.
Emerging evidence suggests that various diseases are associated with altered gut microbiota, including ASD, schizophrenia, depression and Parkinson’s disease6. The gut microbiota may control the central nervous system (CNS) through gut-brain axis7. The gut-brain axis consists of bidirectional communication between the central and the enteric nervous system, linking emotional and cognitive centers of the brain with peripheral intestinal functions8. The mechanisms of the bidirectional communication between microbiota and gut-brain axis, including neural, immune, endocrine and metabolic pathways, are complicated9–11. GI symptoms have a strong association with mitochondrial disease and a large subgroup of individuals with ASD demonstrate abnormalities in mitochondrial function as well as GI symptoms12. Gut microbiota with its metabolites and components can impact the host physiology, disrupt mitochondrial function, adjusting gut barrier function, energy homeostasis, mucosal inflammation and behavior13–15. Changes in the microbiota and their metabolic end products could lead to abnormal redox and mitochondrial metabolism, as well as immune dysfunction. It has been hypothesized that disruptions in the microbiome may be involved in etiology and/or pathophysiology of ASD16. Clostridiales and Bacteroidetes/Firmicutes ratios were increased in ASD children with functional gastrointestinal disorders17. Some clinical studies revealed that patients with ASD had increased inflammation18,19, immune system dysfunction20,21, mitochondrial disorders22 altered metabolic capacity23,24, GI disorders, seizures25 and gut microbial disorders26–28.
One research on ASD children in Slovakian showed increases in the amount of Lactobacillus spp and Desulfovibrio spp and a significant reduction of the Bacteroidetes/Firmicutes ratio in the fecal microbiota26. Another study on regressive autism also showed that Desulfovibrio was more common in autistic subjects than in controls29. Analysis of real-time PCR data indicated that mean counts of Clostridium clusters I and XI in ASD children were greater than those in TD children30. Conversely, ASD children possessed lesser amounts of Bifidobacterium than TD children31. Bifidobacterium are associated with the biosynthesis and cellular content of folate32. The decreased abundance in Bifidobacteria potentially leaded to reduced folate production by microbiota in individuals with ASD. ASD has been related to abnormalities in folate metabolism and folate pathway abnormalities may be a major metabolic disturbance in ASD33. These studies have emphasized that alterations in the composition of the gut microbiota have been implicated in ASD.
However, most studies of the gut microbiota in patients with ASD have been focused on Western populations, it is important to expand these studies to non-Western diet populations in order to fully understand the range of variation of the gut microbiota in patients with ASD and how gut microbes affect the pathogenesis of ASD. Thus, we performed 16S rRNA sequencing of stool samples from 40 children with ASD and 7 TD children in China, aiming to elucidate changes in fecal microbiota in children with ASD and find the effects of microbiota changes on metabolism. In addition, we downloaded the association data set of microbe–disease from human microbe–disease association database (HMDAD) and constructed a microbe-based human disease network(HMDN) including ASD based on microbiome similarity34.
Results
Subject characteristics
A total of 40 children with ASD and 7 TD children were initially recruited. Five of the 40 children with ASD and one of the 7 TD children had low quality reads. Therefore, 35 children with ASD and 6 TD children were included in the final analysis. All children were between 3 to 8 years old, with a mean (±SD) age of 4.9 (±1.5) years for the ASD group and 4.6(±1.1) years for the control group (Table 1).
Table 1.
Summary of subject characteristics.
| ASD group | Control group | |
|---|---|---|
| Total participants | 35 | 6 |
| Age(years) | 4.9 ± 1.5# | 4.6 ± 1.1 |
| Male/Female | 29/6 | 5/1 |
| Constipation | 11 | 0 |
| Diarrhea | 2 | 0 |
| abdominal distention | 8 | 0 |
#All values are mean ± standard deviation.
Microbiota changes in children with ASD
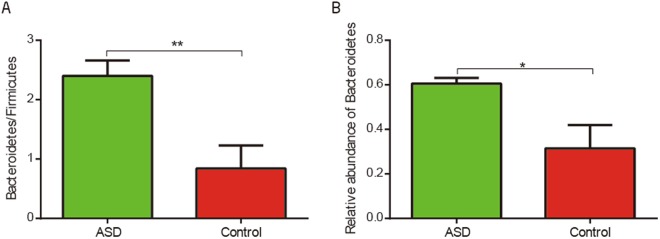
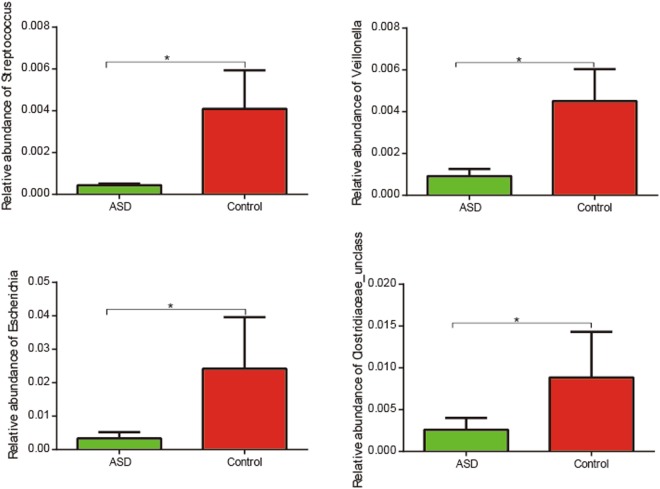
Our study discovered the difference in the fecal microbiota between ASD and control groups. Intestinal flora imbalance of children with ASD was mainly represented by a different bacterial abundance at the level of phylum, as well as at the level of genus (Table 2, Fig. S1). At the level of phylum, the ratio of Bacteroidetes/Firmicutes (p < 0.05, Wilcoxon rank-sum test; Fig. 1a.) was significantly higher in the ASD group compared to the control group due to a significant increase of the relative abundance of Bacteroidetes (FDR-corrected p < 0.05, Wilcoxon rank-sum test; Fig. 1b). Genus level analysis showed Bacteroides, Faecalibacterium, Lachnospiraceae_unclass and Oscillospira were abundant in both ASD and control subjects (Supporting Dataset S1). We observed that Streptococcus, Veillonella and Escherichia were was significantly less abundant in ASD group compared to control group (Fig. 2).
Table 2.
The bacterial abundance at the level of phylum and genus in two groups with significant difference (q-value < 0.05).
| ASD (mean) | Control(mean) | p-value | q-value | |
|---|---|---|---|---|
| phylum level | ||||
| p__Bacteroidetes | 0.6057 | 0.3149 | 0.00586 | 0.03246 |
| p__Firmicutes | 0.3349 | 0.6299 | 0.01279 | 0.03246 |
| p__Bacteria_unclass | 0.0142 | 0.1866 | 0.01623 | 0.03246 |
| genus level | ||||
| g__Streptococcus | 0.000437 | 0.024549 | 0.00043 | 0.01576 |
| g__Veillonella | 0.000919 | 0.027029 | 0.00182 | 0.03097 |
| g__Escherichia | 0.003306 | 0.024151 | 0.00330 | 0.04700 |
| g__Clostridiaceae_unclass | 0.002599 | 0.053084 | 0.00297 | 0.04567 |
| g__Actinomyces | 0.000009 | 0.00009 | 2.76E + 01 | 0.00467 |
| g__Parvimonas | 0.00009 | 0.00830 | 0.001832 | 0.03097 |
| g__Bulleidia | 0.000002 | 0.000014 | 0.001432 | 0.03024 |
| g__Peptoniphilus | 0 | 0.000011 | 0.000653 | 0.01576 |
Figure 1.
(A) Comparison of the ratio of Bacteroidetes/Firmicutes between ASD children and typical development children (**p < 0.005, Wilcoxon rank-sum test). (B) Box plot representation of the relative abundance of Bacteroidetes (*FDR-corrected p < 0.05, Wilcoxon rank-sum test). The boxes represent the mean ± Standard Error of Mean (SEM).
Figure 2.
Box plot representation of the relative abundances of bacterial genera that significantly decreased in ASD group compared with control group. The boxes represent the mean ± SEM, *FDR-corrected p < 0.05, Wilcoxon rank-sum test.
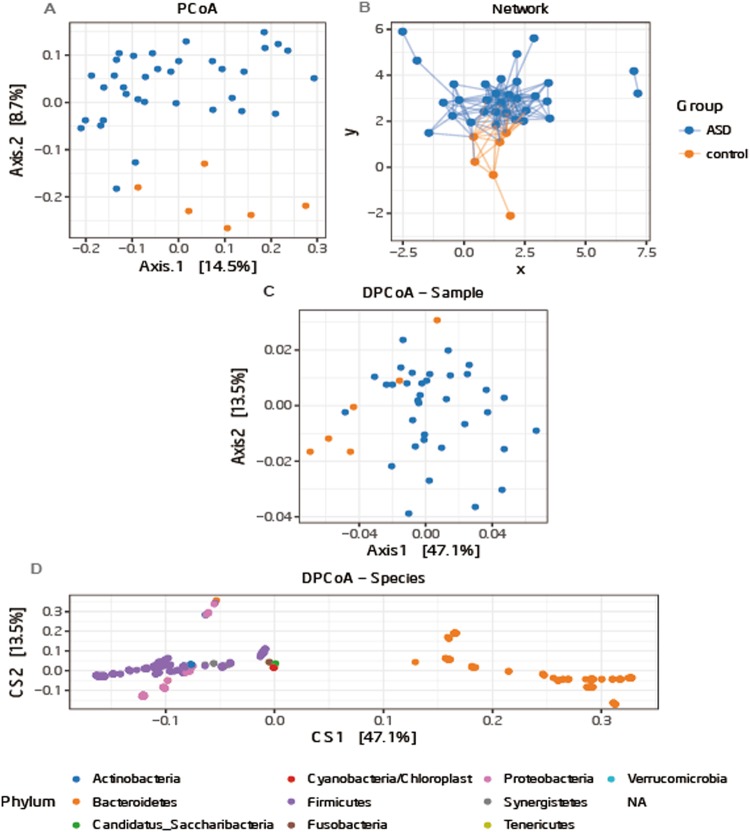
Shannon index which reflects the alpha diversity revealed no significant differences between ASD and control groups, but the diversity of most of the children with ASD was lower than that of TD children (Fig. S2). Analysis of the beta diversity calculated on the Bray-Curtis dissimilarity and the network revealed that the bacterial microbiota of ASD group clusters apart from that of control group (Fig. 3a,b, Permutation test, p = 0.002). Analysis of DPCoA showed that the differences between gut microbiota in the two groups were Bacteroidetes at the phylum level (Fig. 3c,d).
Figure 3.
(A) PCoA of bacterial beta diversity based on the Bray-Curtis dissimilarity. ASD and control subjects are coloured in blue and orange, respectively. (B) Network of ASD and control group based on Bray-Curtis dissimilarity; (C) community and (D) species points for DPCoA.
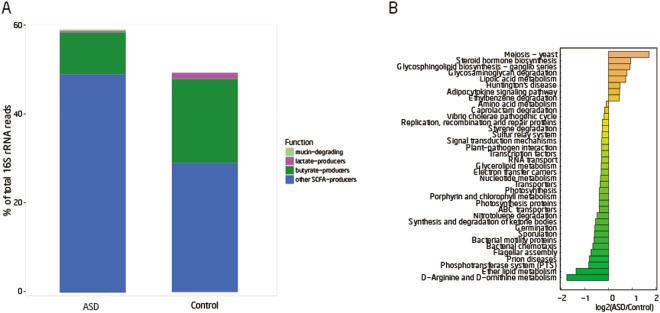
Functional analysis
In this study, we compared the differences of four groups of functional bacteria of short chain fatty acids (SCFA) producers between ASD and control groups. We found that butyrate and lactate producers were more abundant in the control group while mucin-degraders and other SCFA-producers were more abundant in the ASD group (Fig. 4a) although these differences of relative abundance were not statistically significant. Butyric acid can promote the synthesis of mucin35 and enhance intestinal tight junction integrity36. The lower relative abundances of mucolytic Akkermansia muciniphila bacterium in children with autism caused mucus barrier changes37. A high percentage of abnormal intestinal permeability has been reported in patients with autism38. Research stated that the genera Fusobacterium, Eubacterium, Anaerostipes, Subdoligranulum, Faecalibacterium and Roseburia could produce butyrate while Lactoabcillus, Bifidobacterium, Streptococcus, and Lactococcus produce lactate and the genera Prevotella and Akkermansia could produce mucin39. In our study, Faecalibacterium and Roseburia was decreased in the ASD group compared with the control group although this difference of relative abundance was not supported by the statistical analysis. The alteration of bacteria producing butyric acid may be related to the abnormally-elevated intestinal permeability in ASD patients.
Figure 4.
(A) Mean proportion of four functional groups between ASD and control. The genera depicted are known to degrade mucin and produce lactate, butyrate, or other short chain fatty acids (SCFA) such as propionate, succinate, or acetate. (B) Thirty-seven known functions that differ significantly between cases and controls (p < 0.05) as determined by the log of the ration between ASDs and controls. Twenty-nine of these functions are the highest in ASDs relative to controls while eight are the highest in controls relative to ASDs.
In our study, we investigated 254 KEGG pathways.The result of KEGG pathways analysis showed that D−Arginine and D−ornithine metabolism, ether lipid metabolism, bacterial chemotaxis, neurodegenerative diseases -prion diseases, phosphotransferase system (PTS) and flagellar assembly genes were more abundant in ASD group than that of control group while meiosis-yeast, steroid hormone biosynthesis, glycosaminoglycan degradation and lipoic acid metabolism were enriched in the control group (p value < 0.05, Wilcoxon rank-sum test, Fig. 4b, Supporting Dataset S2). PTS system, which was enriched in ASD is also related to diabetes40. However, after FDR correction, no pathways were significantly different between two groups.
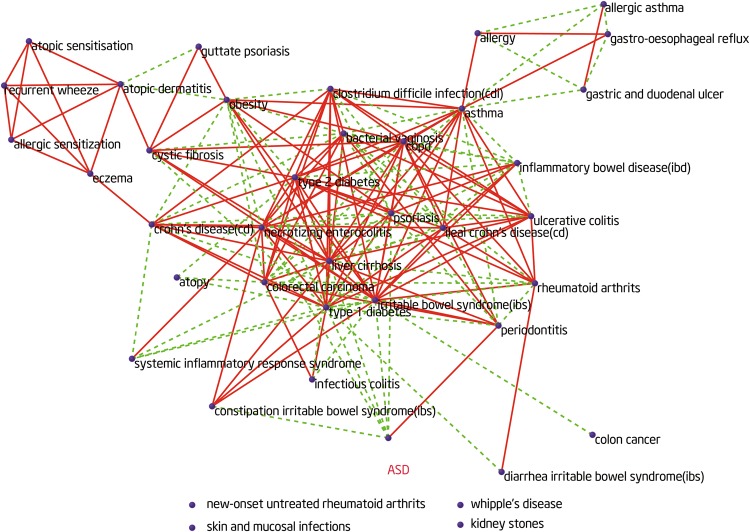
Construction of the HMDN including ASD
Based on the human microbe–disease association database (HMDAD)34,we calculated the microbe similarity between ASD and other diseases. We constructed a network (Fig. 5) with a total 188 links (links represent microbe similarities between diseases), including 114 positive links (consistent changes in microbiome) and 74 negative links (reversed changes in microbiome) among 40 diseases. In this network, each node represents one disease. The red solid lines or the green dotted lines represent a positive or negative microbe-based link between two diseases, respectively. We found that ASD and periodontal have similar microbiota changes. In contrast, ASD and type 1 diabetes, constipation irritable bowel syndrome, psoriasis have opposite microbiota changes (Fig. 6). However, the correlation of these diseases was unclear. Clinical evidence will be needed to verify our finding in the future.
Figure 5.
The human microbe-based disease network (HMDN) including ASD. In the network, each node represents one disease. The green dotted lines or the red solid lines represent a negative or positive microbe-based link between two diseases, respectively.
Figure 6.
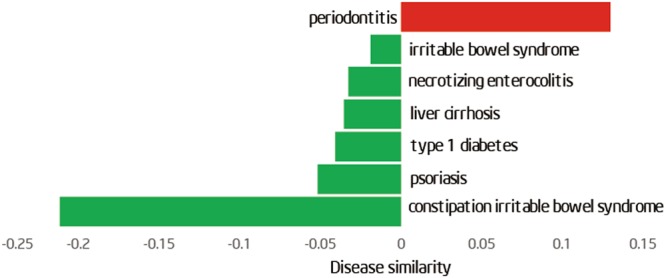
Microbiota changes between ASD and the diseases in the microbe-based disease network. Height of the green (red) bars represents the strength of negative (positive) similarity between ASD and corresponding diseases.
Discussion
The frequent occurrence of GI issues in ASD patients imply the possible involvement of the gut microbiota in gastrointestinal pathophysiology of ASD. Thus, it is important to detect the change of gut microbiota in ASD children. Our results demonstrated that the ratio of Bacteroidetes/Firmicutes was significantly higher in children with ASD emanating from the higher abundance of Bacteroidetes phylum. Inconsistently with other observations, a decreased Bacteroidetes/Firmicutes ratio has been reported in subjects with autism due to a significant reduction of Bacteroidetes in these individuals26,41. Gut microbiota of children in a rural African village in Burkina Faso showed an increase in Bacteroidetes and a decrease in Firmicutes relative to European children38. The decreased Bacteroidetes/Firmicutes ratio in Slovakia and Italy population and the increased Bacteroidetes/Firmicutes ratio in Chinese population may be due to different living environment and eating habits. Western diet habits may affect the composition of the gut microbiota42. Most studies of the gut microbiota in patients with ASD have been focused on Western populations, it is important to expand these studies to non-Western diet populations in order to fully understand the range of variation of the gut microbiota in patients with ASD and how gut microbes affect the pathogenesis of ASD. Furthermore, we discovered that the abundance of Veillonella was significantly decreased in stools of children with ASD. Consistently with this observation, the decrease of Veillonella has been reported also in subjects with autism41. Veillonella can ferment lactate43, indicating that the decreased Veillonella may disturb the fermentation of lactate in children with ASD. Our study also suggested Streptococcus and Escherichia were depleted in ASD subjects in comparison to control subjects, in line with the results obtained in previous study44.
As the ‘second genome’ of human beings45, gut microbiota play important roles in human health and diseases. Carbohydrates are essential sources of energy for human beings and microbiota, but our own enzymes can’t degrade most complex polysaccharides and plant cellulose. These indigestible carbohydrates can be fermented by microbiota in the gut and produce energy related products (such as SCFA, mainly including acetic acid, propionic acid and butyric acid). SCFAs are plausibly linked to ASD and can induce widespread effects on gut, brain and behavior46. Butyrate is recognized as an anti-inflammatory SCFA that contributes to colon health47,48. Research showed that butyrate could rescue ASD cells during oxidative stress and enhance mitochondrial function in the context of physiological stress49. Butyrate can modulate neurotransmitter gene expression50 and the ASD-related genes in cell line models51. We found that butyrate and lactate producers were less abundant in stools of children with ASD, although the difference was not statistically significant in this small study. It indicated that the altered gut microbiota in ASD children could influence the production of SCFA and then disturb intestinal health.
The KEGG database is an important functional database that is used to annotate genes52. Genes can be projected into the KEGG PATHWAY database reveal interactions with other genes that may influence the health of the host53. The 16 Sr RNA mining of our data showed that some genes were much more abundant in ASD group than that of control group. Major function category including amino acid metabolism, bacterial chemotaxis, RNA transport and porphyrin and chlorophyll metabolism genes was much more abundant in terms of the % of total reads in control group than that of ASD group. Lipoic acid metabolism and Glycosphingolipid biosynthesis was much more abundant in ASD group (supporting dataset S2). The above differences in gene abundances were not statistically significant, but are worthy of further investigation.
An important discovery in the study is that the microbe-based similarity between ASD and periodontitis is positive, indicating that the changes of the shared microbes tend to be similar in the two diseases. Children with ASD had significantly higher periodontal treatment needs compared with unaffected controls54. In addition to, autistic children had higher dental caries prevalence than that in their unaffected peers55. This finding further presents a potential reason or mechanism by which ASD is positively correlated with periodontitis. Strikingly, type 1 diabetes shows a negative microbe-based similarity with ASD, indicating that ASD is negatively correlated with type 1 diabetes in their shared microbiota. For example, Veillonella is decreased in ASD but increased in type 1 diabetes56. However, the exact relationship between type 1 diabetes and ASD is complex and deserves further study.
Our discoveries add to available clinical evidence that altered gut microbiota could be linked to the development of ASD. More importantly, we found that microbe-based disease analysis could predict novel connection between ASD and other diseases; it may offer a promising prospect for revealing the pathogenesis of ASD. In the future, we can explore the pathogenesis of autism and divide ASD into different subtypes based on alteration of gut microbiota and microbe-based disease analysis.
However, there is limitation exist in our study. First, the sample size of controls in this study is small. Because gut microbiota is closely related to ASD, our results may be significant despite that limitation. Second, the HMDAD we used has not been updated since it was established. Hence, the available microbe–disease associations only represent a small number of microorganisms and human diseases before the date (July 2014).
Subjects and Methods
Participants
All children with ASD participating in this study were diagnosed with autistic spectrum disorder according to DSM-5 (Diagnostic and Statistical Manual of Mental Disorders-5th Edition). They were enrolled from one local family fraternity group, a group of unrelated autistic families. Children who had fragile X syndrome, tuberous sclerosis, significant sensory impairment, clinically evident inflammatory conditions, coeliac disease, special diet (such as ketogenic diet) and brain anomalies detected by magnetic resonance imaging were excluded.
Control group children were recruited from two kindergartens through pediatricians. Children who had psychiatric conditions (such as depressive disorder, schizophrenia and bipolar disorder) were excluded according to their medical examinations for enrollment and parent interview. All subjects did not take antibiotics, antipsychotics, probiotics and prebiotics in the past month prior to the sample collection.
At last, 40 children with ASD and 7 typically developing children were enrolled in Beijing. The ages of autistic children and control children were 3 to 8 years. This study has been approved by the Institutional Review Board of Peking University (Ethical Review Document No: IRB00001052-16059). We only use stool samples to analyze the related genes of the microbiota. The study group gained informed consent from the parents/guardians for the collection of stool samples and trial information. We confirmed that all methods were performed in accordance with relevant guidelines and regulations.
Stool collection
Fecal specimens were collected in the homes of the participants by their parents. Immediately deep freezing was required to preserve the specimens, and then fecal specimens were shipped to Medical informatics laboratory in Peking University Health Science Center on the same day where each specimen was frozen at −80 °C until DNA extraction.
Library preparation and Illumina sequencing
The mixture of purified PCR products was generated for Next-generation sequencing (NGS) library using NEXTflex Rapid DNA-Seq kit for Illumina (BIOO SCIENTIFIC, USA) following manufacturer’s recommendations. The library quality was quantified by Qubit dsDNA HS Assay Kit with the Qubit 2.0 fluorometer system (Invitrogen, Life Technologies, Grand Island, NY, USA). The multiplexed amplicons were sequenced using the Illumina HiSeq. 2500 platform to generate 250 bp paired-end reads. The sequencing and analysis were performed at SinoGenoMax Co., Ltd, Beijing, China.
Microbiome bioinformatics
Firstly, we got high quality reads through filtering the original paired-end reads, then obtained longer sequences by splicing sequence, compared longer sequences with the 16 S reference database, removed chimeric sequences. Eventually filtered sequences were classified according to a certain threshold. Multiple sequence clustering operational taxonomic units (OTUs) was obtained at the end.
Representative sequences were taxonomically annotated using QIIME’s RDP Classifier57 against the Greengenes reference database. Alpha and beta diversity analyses were performed using QIIME’s core_diversity_analyses.py. For beta diversity analysis, the similarities between samples were calculated using Unweighted Unifrac58. Functional analyses were performed using PICRUSt software59 (a computational approach to predict the functional composition of a metagenome using marker gene data and a database of reference genomes).
Construction of the HMDN including ASD
Based on the human microbe–disease association database (HMDAD)(http://www.cuilab.cn/hmdad), we calculated the microbe similarity between ASD and other diseases and constructed a network including ASD34.
Statistical analysis
The Fisher’s exact test, randomization test and Wilcoxon signed-rank test analysis were performed using R (http://cran.r-project.org/). All p values reported in the study were from two-tailed tests and p values lower than 0.05 were accepted as significant in clinical data analysis. All p values for bacterial microbiome analyses were corrected using the Benjamini-Hochberg false discovery rate (FDR) correction, and the resulting corrected values were referred to as q values. q values lower than 0.05 were accepted as significant.
Electronic supplementary material
Acknowledgements
We are very grateful to the children, families and school staff, who kindly took part in this research. This study has been partly supported by the National Natural Science Fund (award number: 81473236).
Author Contributions
Juan Wang designed the research; Mengxiang Zhang and Yi He programmed the task and collected the data; Juan Zhang contacted the hospital; Mengxiang Zhang and Wei Ma analyzed the data and drafted the manuscript. All authors reviewed and approved the manuscript.
Data Availability
All data generated during or analyzed during the current study are available from the corresponding author on reasonable request.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-32219-2.
References
- 1.Sun X, Allison C, Matthews FE, Sharp SJ. Prevalence of autism in mainland China, Hong Kong and Taiwan a systematic review and meta-analysis. Molecular autism. 2013;4:7. doi: 10.1186/2040-2392-4-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Kim YS, Leventhal BL. Genetic Epidemiology and Insights into Interactive Genetic and Environmental Effects in Autism Spectrum Disorders. Biol Psychiat. 2015;77:66–74. doi: 10.1016/j.biopsych.2014.11.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Bauman ML. Medical comorbidities: in autism Challenges to diagnosis and treatment. Neurotherapeutics. 2010;7:320–327. doi: 10.1016/j.nurt.2010.06.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Peters B, et al. Rigid-Compulsive Behaviors are Associated with Mixed Bowel Symptoms in Autism Spectrum Disorder. Journal of autism and developmental disorders. 2014;44:1425–1432. doi: 10.1007/s10803-013-2009-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Maenner MJ, et al. Brief Report: Association Between Behavioral Features and Gastrointestinal Problems Among Children with Autism Spectrum Disorder. Journal of autism and developmental disorders. 2012;42:1520–1525. doi: 10.1007/s10803-011-1379-6. [DOI] [PubMed] [Google Scholar]
- 6.Dinan, T. G. & Cryan, J. F. Gut Instincts: microbiota as a key regulator of brain development, ageing and neurodegeneration. The Journal of physiology, 10.1113/JP273106 (2016). [DOI] [PMC free article] [PubMed]
- 7.Grenham S, Clarke G, Cryan JF, Dinan TG. Brain-gut-microbe communication in health and disease. Frontiers in physiology. 2011;2:94. doi: 10.3389/fphys.2011.00094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Carabottia MSA, Severi C, Maselli MA. The gut-brain axis interactions between enteric microbiota,central and enteric nervous systems. Ann Gastroenterology. 2015;28:203–209. [PMC free article] [PubMed] [Google Scholar]
- 9.Sommer F, Backhed F. Know your neighbor: Microbiota and host epithelial cells interact locally to control intestinal function and physiology. BioEssays: news and reviews in molecular, cellular and developmental biology. 2016;38:455–464. doi: 10.1002/bies.201500151. [DOI] [PubMed] [Google Scholar]
- 10.Koh A, De Vadder F, Kovatcheva-Datchary P, Backhed F. From Dietary Fiber to Host Physiology: Short-Chain Fatty Acids as Key Bacterial Metabolites. Cell. 2016;165:1332–1345. doi: 10.1016/j.cell.2016.05.041. [DOI] [PubMed] [Google Scholar]
- 11.El Aidy S, Dinan TG, Cryan JF. Gut Microbiota: The Conductor in the Orchestra of Immune-Neuroendocrine Communication. Clinical therapeutics. 2015;37:954–967. doi: 10.1016/j.clinthera.2015.03.002. [DOI] [PubMed] [Google Scholar]
- 12.Frye RE, Rose S, Slattery J, MacFabe DF. Gastrointestinal dysfunction in autism spectrum disorder: the role of the mitochondria and the enteric microbiome. Microbial ecology in health and disease. 2015;26:27458. doi: 10.3402/mehd.v26.27458. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Hooper LV, Littman DR, Macpherson AJ. Interactions between the microbiota and the immune system. Science. 2012;336:1268–1273. doi: 10.1126/science.1223490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Tremaroli V, Backhed F. Functional interactions between the gut microbiota and host metabolism. Nature. 2012;489:242–249. doi: 10.1038/nature11552. [DOI] [PubMed] [Google Scholar]
- 15.Frye RE, Melnyk S, Macfabe DF. Unique acyl-carnitine profiles are potential biomarkers for acquired mitochondrial disease in autism spectrum disorder. Translational psychiatry. 2013;3:e220. doi: 10.1038/tp.2012.143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Slattery J, MacFabe DF, Frye RE. The Significance of the Enteric Microbiome on the Development of Childhood Disease: A Review of Prebiotic and Probiotic Therapies in Disorders of Childhood. Clinical medicine insights. Pediatrics. 2016;10:91–107. doi: 10.4137/CMPed.S38338. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Luna RA, et al. Distinct Microbiome-Neuroimmune Signatures Correlate With Functional Abdominal Pain in Children With Autism Spectrum Disorder. Cellular and Molecular Gastroenterology and Hepatology. 2017;3:218–230. doi: 10.1016/j.jcmgh.2016.11.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Theoharides TC, Stewart JM, Panagiotidou S, Melamed I. Mast cells, brain inflammation and autism. European journal of pharmacology. 2016;778:96–102. doi: 10.1016/j.ejphar.2015.03.086. [DOI] [PubMed] [Google Scholar]
- 19.Theoharides TC, Tsilioni I, Patel AB, Doyle R. Atopic diseases and inflammation of the brain in the pathogenesis of autism spectrum disorders. Translational psychiatry. 2016;6:e844. doi: 10.1038/tp.2016.77. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ashwood P, et al. Elevated plasma cytokines in autism spectrum disorders provide evidence of immune dysfunction and are associated with impaired behavioral outcome. Brain Behav Immun. 2011;25:40–45. doi: 10.1016/j.bbi.2010.08.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Nardone S, Elliott E. The Interaction between the Immune System and Epigenetics in the Etiology of Autism Spectrum Disorders. Frontiers in neuroscience. 2016;10:329. doi: 10.3389/fnins.2016.00329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Rossignol DA, Frye RE. Mitochondrial dysfunction in autism spectrum disorders: a systematic review and meta-analysis. Molecular psychiatry. 2012;17:290–314. doi: 10.1038/mp.2010.136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cheng N, Rho JM, Masino SA. Metabolic Dysfunction Underlying Autism Spectrum Disorder and Potential Treatment Approaches. Frontiers in molecular neuroscience. 2017;10:34. doi: 10.3389/fnmol.2017.00034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Moses L, Katz N, Weizman A. Metabolic profiles in adults with autism spectrum disorder and intellectual disabilities. European psychiatry: the journal of the Association of European Psychiatrists. 2014;29:397–401. doi: 10.1016/j.eurpsy.2013.05.005. [DOI] [PubMed] [Google Scholar]
- 25.Frye, R. A review of traditional and novel treatments for seizures in autism spectrum disorder: findings from a systematic review and expert panel. Frontiers in Public Health1, 10.3389/fpubh.2013.00031 (2013). [DOI] [PMC free article] [PubMed]
- 26.Tomova A, et al. Gastrointestinal microbiota in children with autism in Slovakia. Physiology & behavior. 2015;138:179–187. doi: 10.1016/j.physbeh.2014.10.033. [DOI] [PubMed] [Google Scholar]
- 27.Rosenfeld CS. Microbiome Disturbances and Autism Spectrum Disorders. Drug metabolism and disposition: the biological fate of chemicals. 2015;43:1557–1571. doi: 10.1124/dmd.115.063826. [DOI] [PubMed] [Google Scholar]
- 28.Kang DW, et al. Reduced incidence of Prevotella and other fermenters in intestinal microflora of autistic children. PloS one. 2013;8:e68322. doi: 10.1371/journal.pone.0068322. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Finegold SM. Desulfovibrio species are potentially important in regressive autism. Medical hypotheses. 2011;77:270–274. doi: 10.1016/j.mehy.2011.04.032. [DOI] [PubMed] [Google Scholar]
- 30.Song Y, Liu C, Finegold SM. Real-time PCR quantitation of clostridia in feces of autistic children. Appl Environ Microbiol. 2004;70:6459–6465. doi: 10.1128/AEM.70.11.6459-6465.2004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Adams JB, Johansen LJ, Powell LD, Quig D, Rubin RA. Gastrointestinal flora and gastrointestinal status in children with autism–comparisons to typical children and correlation with autism severity. BMC gastroenterology. 2011;11:22. doi: 10.1186/1471-230X-11-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.D’Aimmo MR, Modesto M, Mattarelli P, Biavati B, Andlid T. Biosynthesis and cellular content of folate in bifidobacteria across host species with different diets. Anaerobe. 2014;30:169–177. doi: 10.1016/j.anaerobe.2014.09.018. [DOI] [PubMed] [Google Scholar]
- 33.Frye RE, Edward JCS, Quadros V. Folate metabolism abnormalities in autism:potential biomarkers. Biomarkers in medicine. 2017;11:687–699. doi: 10.2217/bmm-2017-0109. [DOI] [PubMed] [Google Scholar]
- 34.Ma, W. et al. An analysis of human microbe-disease associations. Briefings in bioinformatics, 10.1093/bib/bbw005 (2016). [DOI] [PubMed]
- 35.Burger-van Paassen N, et al. The regulation of intestinal mucin MUC2 expression by short-chain fatty acids: implications for epithelial protection. The Biochemical journal. 2009;420:211–219. doi: 10.1042/BJ20082222. [DOI] [PubMed] [Google Scholar]
- 36.Peng L, Li ZR, Green RS, Holzman IR, Lin J. Butyrate enhances the intestinal barrier by facilitating tight junction assembly via activation of AMP-activated protein kinase in Caco-2 cell monolayers. The Journal of nutrition. 2009;139:1619–1625. doi: 10.3945/jn.109.104638. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Wang L, et al. Low Relative Abundances of the Mucolytic Bacterium Akkermansia muciniphila and Bifidobacterium spp. in Feces of Children withAutism. Appl Environ Microb. 2011;77:6718–6721. doi: 10.1128/AEM.05212-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.de Magistris L, et al. Alterations of the intestinal barrier in patients with autism spectrum disorders and in their first-degree relatives. Journal of pediatric gastroenterology and nutrition. 2010;51:418–424. doi: 10.1097/MPG.0b013e3181dcc4a5. [DOI] [PubMed] [Google Scholar]
- 39.Brown CT, et al. Gut microbiome metagenomics analysis suggests a functional model for the development of autoimmunity for type 1 diabetes. PloS one. 2011;6:e25792. doi: 10.1371/journal.pone.0025792. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Qin J, et al. A metagenome-wide association study of gut microbiota in type 2 diabetes. Nature. 2012;490:55–60. doi: 10.1038/nature11450. [DOI] [PubMed] [Google Scholar]
- 41.Strati F, et al. New evidences on the altered gut microbiota in autism spectrum disorders. Microbiome. 2017;5:24. doi: 10.1186/s40168-017-0242-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Wang Y, Kasper LH. The role of microbiome in central nervous system disorders. Brain Behav Immun. 2014;38:1–12. doi: 10.1016/j.bbi.2013.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Gronow S, et al. Complete genome sequence of Veillonella parvula type strain (Te3(T) Stand Genomic Sci. 2010;2:57–65. doi: 10.4056/sigs.521107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Kushak RI, et al. Analysis of the Duodenal Microbiome in Autistic Individuals: Association With Carbohydrate Digestion. Journal of pediatric gastroenterology and nutrition. 2017;64:e110–e116. doi: 10.1097/MPG.0000000000001458. [DOI] [PubMed] [Google Scholar]
- 45.Grice EA, Segre JA. The human microbiome: our second genome. Annual review of genomics and human genetics. 2012;13:151–170. doi: 10.1146/annurev-genom-090711-163814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Macfabe, D. F. Short-chain fatty acid fermentation products of the gut microbiome: implications in autism spectrum disorders. Microbial ecology in health and disease23, 10.3402/mehd.v23i0.19260 (2012). [DOI] [PMC free article] [PubMed]
- 47.Hamer HM, et al. Review article: the role of butyrate on colonic function. Alimentary pharmacology & therapeutics. 2008;27:104–119. doi: 10.1111/j.1365-2036.2007.03562.x. [DOI] [PubMed] [Google Scholar]
- 48.Louis P, Flint HJ. Diversity, metabolism and microbial ecology of butyrate-producing bacteria from the human large intestine. FEMS Microbiology Letters. 2009;294:1–8. doi: 10.1111/j.1574-6968.2009.01514.x. [DOI] [PubMed] [Google Scholar]
- 49.Rose S, et al. Butyrate enhances mitochondrial function during oxidative stress in cell lines from boys with autism. Translational psychiatry. 2018;8:42. doi: 10.1038/s41398-017-0089-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Takuma K, et al. Chronic treatment with valproic acid or sodium butyrate attenuates novel object recognition deficits and hippocampal dendritic spine loss in a mouse model of autism. Pharmacology, biochemistry, and behavior. 2014;126:43–49. doi: 10.1016/j.pbb.2014.08.013. [DOI] [PubMed] [Google Scholar]
- 51.Nankova, B. B., Agarwal, R., MacFabe, D. F. & La Gamma, E. F. Enteric Bacterial Metabolites Propionic and Butyric Acid Modulate Gene Expression, Including CREB-Dependent Catecholaminergic Neurotransmission, in PC12 Cells - Possible Relevance to Autism Spectrum Disorders. PloS one 9,10.1371/journal.pone.0103740 (2014). [DOI] [PMC free article] [PubMed]
- 52.Kanehisa M GS, Kawashima S, Okuno Y, Hattori M. The KEGG resource for deciphering the genome. Nucleic acids research. 2004;32:D277–D280. doi: 10.1093/nar/gkh063. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Altermann E, Klaenhammer TR. PathwayVoyager: pathway mapping using the Kyoto Encyclopedia of Genes and Genomes (KEGG) database. BMC genomics. 2005;6:60. doi: 10.1186/1471-2164-6-60. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Fakroon S, Arheiam A, Omar S. Dental caries experience and periodontal treatment needs of children with autistic spectrum disorder. European archives of paediatric dentistry: official journal of the European Academy of Paediatric Dentistry. 2015;16:205–209. doi: 10.1007/s40368-014-0156-6. [DOI] [PubMed] [Google Scholar]
- 55.Jaber MA. Dental caries experience, oral health status and treatment needs of dental patients with autism. Journal of applied oral science: revista FOB. 2011;19:212–217. doi: 10.1590/S1678-77572011000300006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Murri, M. et al. Gut microbiota in children with type 1 diabetes differs from that in healthy children: a case-control study. Bmc Med11, 10.1186/1741-7015-11-46 (2013). [DOI] [PMC free article] [PubMed]
- 57.Wang Q, Garrity GM, Tiedje JM, Cole JR. Naive Bayesian classifier for rapid assignment of rRNA sequences into the new bacterial taxonomy. Appl Environ Microbiol. 2007;73:5261–5267. doi: 10.1128/AEM.00062-07. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Lozupone C, Knight R. UniFrac: a new phylogenetic method for comparing microbial communities. Appl Environ Microbiol. 2005;71:8228–8235. doi: 10.1128/AEM.71.12.8228-8235.2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Langille MG, et al. Predictive functional profiling of microbial communities using 16S rRNA marker gene sequences. Nature biotechnology. 2013;31:814–821. doi: 10.1038/nbt.2676. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data generated during or analyzed during the current study are available from the corresponding author on reasonable request.