Abstract
Aim
This retrospective study was performed to rule out any jeopardizing effect of extraction therapy of four first premolars on airway at any level of its anatomic course.
Materials and methods
Lateral cephalograms of 50 adolescent patients divided into two groups of 25 each, based on orthodontic treatment by first premolar extraction as group I and without extraction as group II, were selected for the study. 13 angular and 11 linear measurements were compared pre-and post-treatment via statistical analyses using SPSS (Version 17.5, SPSS, Chicago) software. Paired ‘t’ tests were used to assess the variability. P-value < 0.05 was considered to be statistically significant.
Results
Comparison of angular parameters showed that the average percentage (%) change in SNA, SNB, ANB, IMPA, FMA, saddle, articulare, gonial, total angle and hyoid did not differ significantly across two study groups (P > 0.05), but values of UI/LI, UI/NA, LI/NB, differed significantly among both groups. Similarly, linear parameters showed that the average % change in nasopharyngeal airway space (NAS) and width of soft palate differed significantly across two study groups (P-value<0.05), whereas the average % change in posterior airway space (PAS), hypopharyngeal airway space (HAS), hyoid distance and length of tongue did not differ significantly (P-value>0.05). However, no significant differences were observed during intragroup and intergroup comparisons of the combined angular and linear measurements of both groups.
Conclusions
Present study showed no significant change on airway after therapeutic orthodontic tooth movement with or without extraction treatment.
Keywords: Airway, Hyoid bone, Premolar extraction, Tongue
1. Introduction
The airway has always been an area of interest to an orthodontist because the oro- and naso-pharyngeal structures play an indispensable role in the growth and development of the craniofacial complex.1
Brodie et al.2 contended that movement of the teeth for resolution of malocclusion must be confined to the existing dental arch. Proponents of orthodontic extractions contend that functional limits of arch size are genetically predetermined.3 Consequently, extracting teeth is necessary for orthodontic correction in order to respect the limits of the dentition and achieve proper esthetics, health of the oral tissues and occlusal stability.2, 3, 4, 5, 6
On the contrary, dramatic reduction in tongue space is one of the prominent concerns of extraction therapy.7 Some clinicians theorize that by closing extraction spaces, the maxilla and the mandible retrude,8 resulting in constriction of the oro-pharyngeal airway.9,10 A retruded mandibular position may be associated with airway constriction via the lingual musculature and its attachment to the hyoid bone.11 According to orthotropists, a retrusive mandibular position results in excessive vertical facial growth which leads to downward and backward positioning of the mandible.12 It further leads to stretching of the lingual muscular attachment to the hyoid bone, with resultant dorsal and inferior positioning of hyoid bone. An inferior displacement of the hyoid bone along with increased lower facial height are predisposing factors for upper airway obstruction.13
Various studies have analyzed the impact of airway physiology on the craniofacial complex development, dental arch morphology and occlusion. However, to the best of our knowledge, no studies have been performed investigating the effects of dento-alveolar movement by orthodontic extraction and non-extraction therapy on total pharyngeal air way starting from naso-pharynx to laryngo-pharynx. With consideration of the hypothesis that orthodontic treatment with extraction of four premolars would not affect airway passage at nasal, oral and laryngeal level in comparison to non-extraction treatment modality, a retrospective cross-sectional study was planned to rule out any jeopardizing effect of extraction therapy of four first premolars on airway at any level of its anatomic course.
2. Materials and methods
Considering the test power of 0.80 (with an allowable error of 15%), calculated for an effect size (r) equal to 0.38 at an ά level of 0.05 and 95% confidence coefficient, the sample consisted of randomly selected lateral cephalograms of 50 adolescent patients who had undergone orthodontic treatment from 2009 to 2015 in the Department of Orthodontics at Government service hospital, India. Good quality records of all the treated patients were collected and analyzed. Two groups were established based on the treatment procedure: Group 1 consisted of pre-and post-treatment lateral cephalograms of 25 patients (8 males, 17 females) who had been treated by therapeutic extraction of four first premolars. Similarly, group 2 comprised pre-and post-treatment lateral cephalograms of 25 patients (9 males, 16 females) that had been treated without extraction of any teeth. The subjects were aged from 13 to 18 years (mean age 14.2 ± 3.2 years; median, 15 years for group 1; and mean age 15.8 ± 3.5 years; median, 16 years for group 2).
Inclusion criteria were as follows:
-
(i)
Group 1 included subjects with Angle's Class I type 2 malocclusion with bidental protrusion treated with extraction of four premolars with maximum anchorage.
-
(ii)
Subjects in group 2 had been classified as borderline Angle's Class I type 2 malocclusion cases with moderate maxillary and mandibular spacing, and treated without extractions by means of the consolidation of existing spaces, interproximal stripping and en-masse distalization for retraction of upper and lower incisors.
-
(iii)
Cephalometrically, the subjects in groups 1 and 2 were skeletal Class I with upper incisor to maxillary plane angle (U1-Max) > 115°, lower incisor to mandibular plane angle (L1-Mand) > 99°, and interincisal angle less than 124.8°, and normal to mild hyperdivergent growth pattern.
Exclusion criteria for both groups were presence of:
-
(i)
missing teeth
-
(ii)
congenital anomalies affecting the craniofacial region
-
(iii)
medical history of naso-oro-laryngopharyngeal obstruction
-
(iv)
snoring
-
(v)
obstructive sleep apnea
-
(vi)
adenoidectomy and tonsillectomy
All subjects in the study had undergone fixed orthodontic treatment with 0.018” Roth bracket prescription (Gemini, 3M Unitek, Calif, USA). Maximum retraction of anterior teeth (Group ‘A’ anchorage) were ensured by using trans-palatal arch in maxilla and lingual arch in mandible along with mini-implants (AbsoAnchor, Dentos, Korea) placed between 1st molar and second premolar region for anchorage preservation. Case was included in the sample as maximum retraction in which more than 6 mm of retraction had been performed. The average maxillary and mandibular incisor retraction in Group 1 were 11.9 ± 4.5 and 9.3 ± 2.9 mm, respectively. The average maxillary and mandibular incisor retraction in Group 2 were 6.1 ± 1.3 and 5.2 ± 0.9 mm, respectively. Average treatment duration in Group 2 was 2 years, whereas average treatment duration in Group 1 was 2 years 6 months. The mean interval between pre- and post-treatment lateral cephalograms was 2 years 3 months.
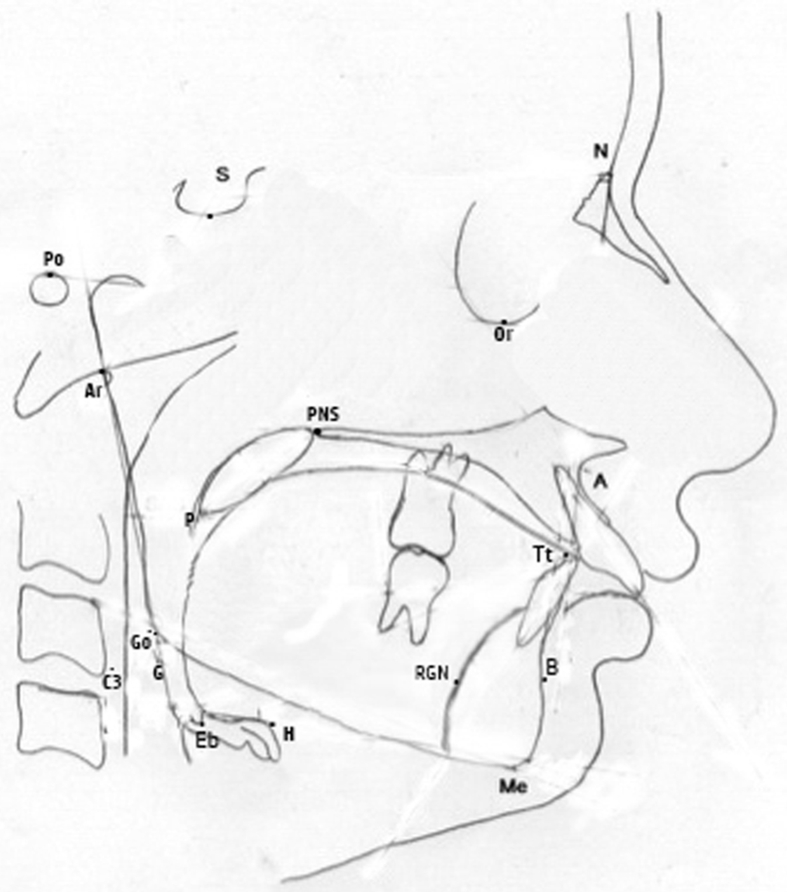
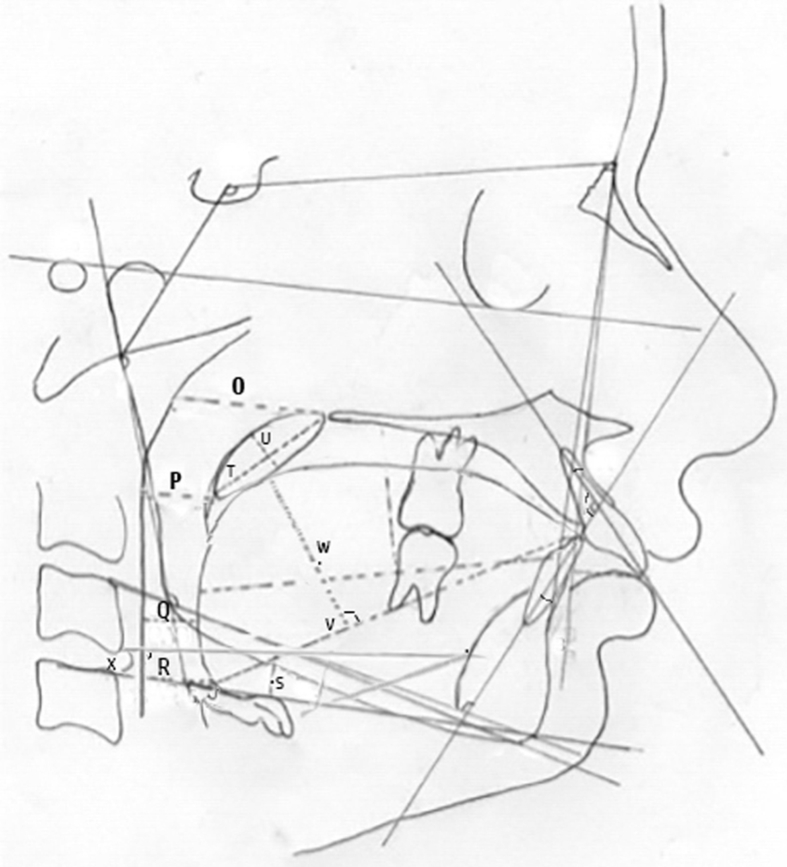
Pre- and post-treatment lateral cephalograms of all patients were traced manually using 3H pencil on a 0.003” acetate matte tracing paper in 1 sitting by first investigator, and then randomly rechecked for anatomic contour and landmark identification and tracing superimpositions by a second investigator to rule out any error (Fig. 1). Any disagreements were resolved by retracing the landmark or structure to the satisfaction of both investigators. The tracing procedure was performed in the darkened room with the viewing screen blanked off, showing only the radiograph. All the radiographs were corrected for magnification and calibrated according to the consistent magnification factor (8%) using radiopaque metal ruler which had had been used retrospectively before and after taking radiographs. All cephalometric measurements were performed manually using a ruler & vernier caliper to the nearest 0.1 mm for linear measurements, and protractor to the nearest 1° for angular measurements. The parameters selected for analysis of total airway were derived from composite norms of Sharma et al.,14 Valiathan et al.15 and Stefanovic et al.,16 who reported study on similar subjects. A customized digitization regimen and analysis were also used to generate 24 cephalometric measurements (13 angular and 11 linear) which were compared for total airway dimension (Fig. 2) Cephalometric landmarks, skeleto-dentoalveolar parameters and airway parameters assessed are depicted in Table 1, Table 2, Table 3, respectively.
Fig. 1.
Cephalometric tracing showing different points and landmarks used in the study.
Fig. 2.
Cephalometric tracing showing different parameters assessed in the study.
Table 1.
Cephalometric points and landmarks used for evaluation of skeleto-dentoalveolar and airway structures.
| Legend | Cephalometric points and landmarks | Description |
|---|---|---|
| 1 | S | Midpoint of the sella turcica of the sphenoid bone |
| 2 | N | Most anterior point of the frontonasal suture in the midsagittal plane |
| 3 | Po | Superior most point of the external auditory meatus |
| 4 | Or | Lowest point in the inferior margin of the orbit |
| 5 | Point A | Most posterior point in the concavity between anterior nasal spine and the dental alveolus |
| 6 | Point B | Most posterior point on the concavity along the anterior surface of the symphysis |
| 7 | Ar | Point of intersection of the contour of the posterior border of the mandibular condylar process and the inferior border of the basilar part of the occipital bone |
| 8 | Go | The most convex point along the inferior border of the ramus |
| 9 | Me | The most inferior point of the symphysis |
| 10 | Rgn | Retrognathic point, i.e. the most posterior point of symphysis |
| 11 | H | The most superior and anterior points on the body of the hyoid bone |
| 12 | Tt | Tongue tip |
| 13 | Eb | Base of epiglottis |
| 14 | P | Tip of soft palate |
| 15 | C3 | Antero-inferior limit of the third cervical vertebra |
| 16 | PNS | Tip of the posterior nasal spine |
| 17 | MnP | Mandibular plane, a line joining menton (Me) and gonion (Go) |
| 18 | Go–B line | A line joining Go and point B |
| 19 | U1 | Axial inclination of the maxillary incisor |
| 20 | L1 | Axial inclination of the mandibular incisor |
| 21 | Frankfort horizontal plane (FHP) | Horizontal plane connecting porion and orbitale |
| 22 | Middle pharyngeal wall (Mpw) | Junction of perpendicular line from P to the posterior pharyngeal wall |
| 23 | Lower pharyngeal wall (Lpw) | Junction of perpendicular line from V to the posterior pharyngeal wall |
| 24 | Hyoid plane (HP) | Line connecting the most superior anterior point on the body of the hyoid bone (Hyoidale, H-point) and the most posterior point of the greater horn of the hyoid bone (G-point). |
Table 2.
Description of skeleto-dentoalveolar parameters related to retraction of teeth.
| Legend | Cephalometric parameters | Description |
|---|---|---|
| A | SNA | SN to NA angle |
| B | SNB | SN to NB angle |
| C | ANB | NA to NB angle |
| D | UI x LI | Angle between long axis of upper incisor and lower incisor |
| E | UI x NA | Upper incisor long axis to NA angle |
| F | UI - NA | Distance between most anterior point of crown of upper incisor and NA line |
| G | LI x NB | Lower incisor long axis to NB angle |
| H | LI - NB | Distance between most anterior point of crown of lower incisor and NB line |
| I | IMPA | Angle between the long axis of the mandibular incisor and Mandibular plane |
| J | FMA | Frankfurt mandibular plane angle |
| K | Saddle angle | Angle between SN plane and line joining S and Ar |
| L | Articulare angle | Angle between line joining S and Ar, and line joining Ar and Go |
| M | Gonial angle | Angle between Ar-Go plane and Go-Me plane |
| N | Total Bjork angle | Sum of saddle, articular and gonial angles |
Table 3.
Description of airway parameters assessed.
| Legend | Cephalometric parameters | Description |
|---|---|---|
| O | Nasopharyngeal airway space (NAS) | Palatal pharyngeal distance on the line passing from PNS, parallel to FHP |
| P | Superior airway space (SAS) | Depth of oropharyngeal airway space from P to Mpw, parallel to FHP |
| Q | Posterior airway space (PAS) | Narrowest sagittal airway space between the base of tongue and the posterior pharyngeal wall, parallel to FHP |
| R | Hypopharyngeal airway space (HAS) | Depth of the airway space from vallecula (junction of epiglottis and base of tongue) to lower pharyngeal wall, parallel to FHP. |
| S | Hyoid distance | Perpendicular distance from hyoid bone to mandibular plane (MnP) |
| T | Length (Ln) of Soft Palate | Distance from PNS to P |
| U | Width (Wd) of Soft Palate | Maximum thickness of soft palate measured on line perpendicular to PNS-P line |
| V | Length of tongue (TGL) | Eb-Tt |
| W | Height of Tongue (TGH) | Maximum height of tongue along perpendicular line of Eb-Tt line to tongue dorsum |
| X | Hyoid plane angle (HP angle) | Angle formed by the intersection of HP with the C3-Rgn plane, representing angular position of the hyoid bone in relation to the mandible |
2.1. Statistical analysis
Data were processed using SPSS software for Windows (Version 17.5, SPSS, Chicago). Application of an exploratory Shapiro-Wilks t-test showed normality of data distribution. Application of Levene test indicated equality of variances for the examined parameters. Analysis was done by using the arithmetic means and the standard deviations calculated for all cephalometric measures. Inferential statistics included a Student's ‘t’ test used to analyze the differences among means for intragroup and intergroup comparisons of the combined angular and linear measurements. Tests of significance were two-tailed, and the minimum level of significance was set at P < 0.05.
2.2. Error of the method
To account for intraobserver and interobserver errors, all measurements of randomly chosen 40 lateral cephalograms were repeated by the same operator after 4 weeks and by a second operator to measure the intra-observer and inter-observer reliabilities respectively. Both the intra- and inter-observer repeatability and reproducibility of the cephalometric measurements showed excellent agreements with intra-class correlation coefficients (ICC) ranging from 0·91 to 0.93 and 0·87 to 0·90 respectively for both groups.
3. Results
The present study evaluated randomly selected pre-and post-treatment lateral cephalogram of 50 patients for airway changes after orthodontic treatment with and without first premolar extraction.
3.1. Comparison of angular measurements
Intra-group comparison of angular measurements showed that the average post-treatment values of UI/LI, UI/NA, LI/NB, IMPA, FMA, articular, gonial, total angle and hyoid angle showed significant differences compared to the corresponding pre-treatment measurements in group 1. However, the average post-treatment values of SNA, SNB, ANB and saddle angles did not differ significantly compared to corresponding pre-treatment measurements in group 1. (Table 4).
Table 4.
Intra-group and inter-group comparison of pre- and post-treatment angular measurements in each study group.
| Angular Measurements (deg) | Group 1 (n = 25) Extraction Group |
Group 2 (n = 25) Non-Extraction Group |
P-value (Inter-Group) [Group 1 vs Group 2] |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-treatment | Post-treatment | % Change | P-value [Pre- vs Post] | Pre-treatment | Post-treatment | % Change | P-value [Pre-vs Post] | Pre-treatment | Post-treatment | % Change | |
| SNA | 82.8 ± 2.9 | 82.8 ± 3.1 | 1.5 | 0.805 (NS) | 82.5 ± 1.7 | 81.9 ± 1.3 | 1.4 | 0.040 (S) | 0.600(NS) | 0.237(NS) | 0.592(NS) |
| SNB | 80.6 ± 2.9 | 80.3 ± 2.8 | 1.0 | 0.164 (NS) | 80.1 ± 1.6 | 79.7 ± 1.3 | 1.7 | 0.170 (NS) | 0.402(NS) | 0.342(NS) | 0.210(NS) |
| ANB | 2.6 ± 1.0 | 2.5 ± 0.7 | 3.8 | 0.714 (NS) | 2.4 ± 0.6 | 2.3 ± 0.6 | 4.2 | 0.574 (NS) | 0.418(NS) | 0.275(NS) | 0.146(NS) |
| UI x LI | 106.7 ± 4.5 | 132.2 ± 3.5 | 24.1 | 0.001 (S) | 117.0 ± 3.2 | 130.3 ± 2.2 | 13.1 | 0.001 (S) | 0.001(S) | 0.848(NS) | 0.001(S) |
| UI x NA | 33.1 ± 4.0 | 23.2 ± 2.1 | 28.6 | 0.001 (S) | 27.7 ± 1.4 | 23.1 ± 1.0 | 16.5 | 0.001 (S) | 0.001(S) | 0.739(NS) | 0.001(S) |
| LI x NB | 32.8 ± 2.8 | 24.8 ± 1.5 | 24.1 | 0.001 (S) | 27.8 ± 1.8 | 25.8 ± 0.5 | 11.3 | 0.001 (S) | 0.001(S) | 0.999(NS) | 0.001(S) |
| IMPA | 105.4 ± 2.3 | 94.6 ± 2.4 | 10.3 | 0.001 (S) | 103.2 ± 1.9 | 95.9 ± 1.4 | 9.9 | 0.001 (S) | 0.001(S) | 0.006(S) | 0.501(NS) |
| FMA | 25.7 ± 2.5 | 27.6 ± 3.8 | 10.7 | 0.001 (S) | 26.6 ± 1.7 | 28.2 ± 1.7 | 6.1 | 0.001 (S) | 0.154(NS) | 0.532(NS) | 0.163(NS) |
| Saddle | 126.3 ± 4.4 | 126.4 ± 4.6 | 0.5 | 0.574 (NS) | 125.4 ± 5.2 | 125.8 ± 4.8 | 0.8 | 0.031 (S) | 0.505(NS) | 0.673(NS) | 0.175(NS) |
| Articulare | 141.5 ± 5.9 | 142.9 ± 5.4 | 1.4 | 0.003 (S) | 142.8 ± 5.8 | 143.6 ± 5.6 | 0.8 | 0.001 (S) | 0.429(NS) | 0.647(NS) | 0.324(NS) |
| Gonial | 125.0 ± 4.4 | 126.7 ± 4.1 | 2.1 | 0.010 (S) | 128.9 ± 3.7 | 129.6 ± 3.7 | 0.9 | 0.003 (S) | 0.001(S) | 0.011(S) | 0.211(NS) |
| Total | 392.8 ± 7.1 | 395.4 ± 7.1 | 0.9 | 0.003 (S) | 397.1 ± 5.4 | 399.0 ± 4.8 | 0.5 | 0.001 (S) | 0.020(S) | 0.041(S) | 0.118(NS) |
| Hyoid | 14.2 ± 5.4 | 15.5 ± 4.4 | 27.7 | 0.035 (S) | 17.7 ± 4.6 | 18.6 ± 3.6 | 14.1 | 0.090 (NS) | 0.016(S) | 0.010(S) | 0.179(NS) |
Values are Mean ± Standard Deviation. P-values by paired t-test after confirming the underlying normality assumption of difference in each measurement. P-value<0.05 is statistically significant. S, statistically Significant; NS, statistically Non-Significant.
Similarly, in group 2, intra-group comparison of angular measurements showed that the average post-treatment values of UI/LI, UI/NA, LI/NB, IMPA, saddle, FMA, articular, gonial and total angle differed significantly compared to the corresponding pre-treatment measurements in group 2. However, the average post-treatment values of SNA, SNB, ANB and hyoid angles did not differ significantly compared to corresponding pre-treatment measurements in group 2. (Table 4).
Inter-group comparison of pre-and post-treatment angular measurements revealed that pre-treatment values of the average SNA, SNB, ANB, FMA, saddle and articular angle did not differ significantly across two study groups. However, the average values of UI/LI, UI/NA, LI/NB, IMPA, gonial, total angle and hyoid showed significant differences among two study groups. Similarly, comparison of post-treatment values showed that the average SNA, SNB, ANB, UI/LI, UI/NA, LI/NB, FMA, saddle and articular angle did not differ significantly across two study groups, but the average, IMPA, gonial, total angle and hyoid angle differed significantly (Table 4).
Comparison of post-treatment % changes showed that the average % change in SNA, SNB, ANB, IMPA, FMA, saddle, articular, gonial, total angle and hyoid differs did not differ significantly across two study groups, but values of UI/LI, UI/NA and LI/NB differed significantly (Table 4).
3.2. Comparison of linear measurements
As for the airway analysis, intragroup comparison of linear measurements showed that in group 1, the average post-treatment values of UI/NA, LI/NB, HAS, hyoid distance and length of tongue differed significantly compared to the corresponding pre-treatment linear measurements, whereas NAS, SAS, PAS, length of soft palate, width of soft palate and height of tongue did not differ significantly compared to the corresponding pre-treatment measurements in group 1 (Table 5).
Table 5.
Intra-group and Inter-group comparison of pre- and post-treatment linear measurements in each study group.
| Linear Measurements (mm) | Group 1 (n = 25) Extraction Group |
Group 2 (n = 25) Non-Extraction Group |
P-Value (Inter-Group) [Group 1 vs Group 2] |
||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Pre-treatment | Post-treatment | % Change | P-value [Pre- vs Post] | Pre-treatment | Post-treatment | % Change | P-value [Pre- vs Post] | Pre-treatment | Post treatment | % Change | |
| UI – NA | 10.0 ± 2.4 | 4.4 ± 0.9 | 53.1 | 0.001 (S) | 6.9 ± 1.2 | 4.1 ± 0.4 | 39.1 | 0.2653 (NS) | 0.001 (S) | 0.164 (NS) | 0.001 (S) |
| LI - NB | 10.6 ± 1.6 | 5.1 ± 0.8 | 50.9 | 0.001 (S) | 6.9 ± 1.4 | 4.2 ± 0.4 | 37.8 | 0.2149 (NS) | 0.001 (S) | 0.001 (S) | 0.001 (S) |
| NAS | 25.9 ± 3.5 | 25.7 ± 3.8 | 8.1 | 0.682 (NS) | 26.6 ± 3.5 | 25.5 ± 3.4 | 4.4 | 0.0297 (S) | 0.496 (NS) | 0.877 (NS) | 0.032 (S) |
| SAS | 12.2 ± 2.4 | 12.9 ± 3.8 | 11.5 | 0.480 (NS) | 15.0 ± 2.3 | 14.2 ± 2.2 | 6.8 | 0.2141 (NS) | 0.001 (S) | 0.141 (NS) | 0.055 (NS) |
| PAS | 11.6 ± 2.0 | 11.4 ± 2.5 | 12.2 | 0.656 (NS) | 13.0 ± 2.4 | 11.6 ± 2.0 | 10.8 | 0.9082 (NS) | 0.026 (S) | 0.709 (NS) | 0.544 (NS) |
| HAS | 16.9 ± 3.8 | 16.1 ± 4.1 | 10.1 | 0.013 (S) | 16.9 ± 3.7 | 15.6 ± 3.6 | 9.7 | 1.000 (NS) | 0.970 (NS) | 0.638 (NS) | 0.853 (NS) |
| Hyoid dist. | 11.5 ± 3.1 | 10.1 ± 3.5 | 15.8 | 0.001 (S) | 11.3 ± 3.0 | 11.2 ± 3.1 | 11.7 | 1.000 (NS) | 0.818 (NS) | 0.270 (NS) | 0.191 (NS) |
| Ln Soft Palate | 35.4 ± 2.9 | 35.4 ± 3.2 | 1.9 | 0.877 (NS) | 33.6 ± 3.1 | 33.6 ± 3.1 | 0.0 | 1.000 (NS) | 0.039 (S) | 0.044 (S) | 0.003 (S) |
| Wd Soft Palate | 11.5 ± 2.1 | 11.4 ± 2.1 | 3.2 | 0.491 (NS) | 12.7 ± 2.5 | 12.7 ± 2.5 | 0.0 | 0.0225 (S) | 0.060 (NS) | 0.052 (NS) | 0.002 (S) |
| Ln Tongue | 72.8 ± 4.6 | 71.1 ± 4.1 | 3.1 | 0.001 (S) | 75.4 ± 2.7 | 73.6 ± 2.7 | 2.3 | 0.664 (NS) | 0.021 (S) | 0.011 (S) | 0.081 (NS) |
| Ht Tongue | 28.2 ± 3.4 | 28.9 ± 3.6 | 4.0 | 0.134 (NS) | 30.4 ± 2.2 | 30.4 ± 2.2 | 0.0 | 1.00 (NS) | 0.009 (S) | 0.089 (NS) | 0.020 (S) |
Intra-group comparison of linear measurements showed that in group 2, except for NAS and width of soft palate measurements which showed statistically significant differences, the average post-treatment values of UI/NA, LI/NB, SAS, PAS, HAS, hyoid distance, length of soft palate, length of tongue and height of tongue did not differ significantly compared to the corresponding pre-treatment linear measurements in group 2 (Table 5).
Inter-group comparison of linear measurements revealed significant differences in pretreatment measurements of the average UI/NA, LI/NB, SAS, PAS, length of soft palate, length of tongue and height of tongue values across two study groups. However, the average NAS, HAS, hyoid distance and width of soft palate did not differ significantly among two study groups. In intergroup comparison of post-treatment measurements, the average LI/NB, length of soft palate and length of tongue showed significant differences among two study groups, but the average UI/NA, NAS, SAS, PAS, HAS, hyoid distance, width of soft palate and height of tongue did not differ significantly across two study groups.
Furthermore, comparison of post-treatment % change in measurements showed statistically significant differences in UI/NA, LI/NB, NAS, length of soft palate, width of soft palate, and height of tongue across two study groups; whereas the average % change in PAS, HAS, hyoid distance and length of tongue did not differ significantly across two study groups (Table 5).
4. Discussion
The present study was conducted to assess the changes in upper, middle and lower airway in orthodontically treated adolescent patients with and without therapeutic extraction of first premolars by comparing pre- and post-treatment lateral cephalograms.
Radiographic cephalometry represents one of the most significant technological advancements in orthodontic diagnosis and treatment planning. Despite limitations of 2-D assessment, lateral cephalometry remains a mainstay in orthodontic diagnosis as it aids in evaluation of the spatial relationships of both skeletal and dental structures with high resolution.17,18 Although airway can be visualized and analyzed in three dimensions (3D) using traditional computed tomography (CT), the radiation dose and the expenses involved are substantially high.19 Magnetic resonance imaging (MRI) is another possible method for 3D upper airway visualization, but it is also a costly procedure and requires significantly longer examination time, when compared to conventional cephalogram. This may result in decreased airway image quality due to motion artifacts.20 Another disadvantage of using CT or MRI is that they are usually available only in selected hospital settings, making their use less accessible in routine clinical settings.20
Intra-group comparison of extraction samples revealed significant changes in upper and lower incisors inclination with respect to cranial base and each other after treatment with controlled opening of bite in both groups. The results of present study showed that majority of malocclusion correction in both groups could be attributed to dental movement with almost negligible skeletal change. It was also observed that only extraction group showed significant change in the position of hyoid bone, which moved posteriorly and inferiorly.
Comparison of pre-and post-treatment percentage change showed that the average change in the values of incisors inclination differed significantly between both study groups. This may be due to variability in the degree of severity of malocclusion requiring greater magnitude of dento-alveolar correction in extraction group as compared to non-extraction group. Since group 2 patients were treated without extraction, the changes reflected within U1/NA (angular and linear), L1/NB (angular and linear) & IMPA, could be due to combination of various adjunctive modalities i.e. consolidation of existing spaces, interproximal stripping and en-masse distalization performed to retract upper and lower incisors.3,6 However, in comparison to group 1, only 50% change was observed in the values of upper and lower incisors in reference to point A and B, respectively. Mean linear change in group 1 was 6.4 ± 1.5 and 2.8 ± 0.8 in relation to UI/NA and 5.5 ± 0.8 and 2.7 ± 1.0 in reference to LI/NB.
The results of the present study also demonstrate that hypo pharyngeal airway space, hyoid distance and length of tongue differ significantly in extraction group after treatment, with no effect on nasopharyngeal, superior and posterior airway space, soft palate and height of tongue. However, in non-extraction group, linear parameters showed that the average % change in nasopharyngeal airway space (NAS) and width of soft palate differed significantly (P-value<0.05). Results showing changes in only laryngo-pharyngeal space after extraction of first premolars (as depicted by significant change in HAS and hyoid bone position values) remain non-conclusive as non-extraction group also showed significant changes in NAS and width of soft palate. The hyoid bone tends to move in a posterior and inferior direction in young adolescents. The present study also proved direct correlation of tongue to oropharynx and hypo-pharynx. Post-extraction tongue position directly influenced the hyoid, which further explains anatomical dependence of hyoid on the hyoglossal muscle.
One common assertion is that the extraction of premolars with subsequent canine retraction, results in constriction of the palate, tongue space, and oro-pharyngeal airway.14 Present study concurs the above findings with final comparison of post-treatment % change in measurements between two groups showing significant differences in the average % change in incisors position, upper airway, soft palate and height of tongue between two study groups. This could be attributed to fact that extraction group undergoes more dento-alveolar correction then non-extraction group.
Germec-Cakanet et al.21 reported a statistically significant increase in the superior and middle airway size in subjects treated with extractions and minimum anchorage, while Valiathan et al.15 noticed a non-significant increase in the airway volume and area of maximum constriction in extraction subjects, but used a smaller sample size and restricted the measurement to the oro-pharyngeal area. Similarly, Stefanovic et al.16 reported that either an extraction or non-extraction choice for orthodontic treatment would not differently affect the pharyngeal airway. However present study showed that there may be some changes in upper airway, which decrease with extraction therapy, but middle and lower airway didn't get affected much with decision of extraction for orthodontic purpose. The present finding is in agreement to the findings of Pliska et al.22 who showed that extraction treatment did not significantly constrict the volume of upper airway in adults; and both the extraction and non-extraction patients exhibited similar oropharyngeal measurements.
Contrary to the above findings, Sharma et al.14 observed that the pharyngeal airway size became narrower after extraction of four premolars in relation to velopharyngeal, glossopharyngeal and hypopharyngeal area. They also proved direct correlation of tongue to oro-pharynx and hypo-pharynx. Similarly, Nuvusetty et al.23 also found a significant narrowing of pharyngeal airway behind soft palate, uvula, and at the base of the tongue following retraction in Class I bimaxillary dentoalveolar protrusion cases. Significant inferior positioning of the hyoid bone occurred as an adaptation preventing an encroachment of the tongue into the pharyngeal airway. These variations among the results of previous studies could be attributed to differences in the parameters selected for measurement, and different diagnostic methods used to measure changes.
Renata de Cassia Gonçalves et al.24 reported no significant gender differences in the upper airway widths of the patients who were between 6 and 18 years of age. They further showed that the lower airway width demonstrated variable growth with no statistical differences among any of the age groups. In addition, there was no sexual dimorphism in the 2D lateral cephalometric analyses or the 3D airway measurements of preadolescents. Similarly, Adamidis and Spyropoulos25 reported no gender differences in the lower airway width of patients who were an average of 9.3 years of age. Present study also affirmed the same finding.
Considering the prevalent availability of data and financial constraints, 2D lateral cephalogram had been used to assess the airway. However, further studies can be performed using CBCT or digital imaging systems, considering present study as the base the foundation of advance research.
5. Conclusion
The present study infers that there is no significant change at any level of airway on its anatomic course due to orthodontic therapy either by extraction or by non-extraction approach.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.jobcr.2018.09.004.
Contributor Information
Maj Raj kumar Maurya, Email: bracedbyraj@gmail.com.
Col Prasanna Kumar, Email: drprasannamp@gmail.com.
Lt Col Mohit Sharma, Email: dr.ms16@gmail.com.
Harpreet Singh, Email: drhpreet_mamc04@yahoo.co.in.
Prabhat Kumar Chaudhari, Email: dr.prabhatkc@gmail.com.
Appendix A. Supplementary data
The following is the Supplementary data to this article:
References
- 1.Amini F., Borzabadi-Farahani A., Behnam-Roudsari G., Jafari A., Shahidinejad F. Assessment of the uvulo-glossopharyngeal dimensions in patients with ß-thalassemia major. Sleep Breath. 2013;17:943–949. doi: 10.1007/s11325-012-0782-3. [DOI] [PubMed] [Google Scholar]
- 2.Brodie A.G., Downs W.B., Goldstein A., Myer E. Cephalometric appraisal of orthodontic results - a preliminary report. Angle Orthod. 1938;8 261-29. [Google Scholar]
- 3.Tweed C.H. Indications for the extraction of teeth in orthodontic procedures. Am J Orthod Oral Surg. 1944;30:405–428. [PubMed] [Google Scholar]
- 4.Strang R.H.W. The fallacy of denture expansion as a treatment procedure. Angle Orthod. 1949;19:12–17. [Google Scholar]
- 5.Al-Qahtani N.D. Impact of different orthodontic treatment modalities on Airway. Pak J Med Sci. 2016;32(1):249–252. doi: 10.12669/pjms.321.8743. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Pearson L.E. Vertical growth in fully-banded orthodontic treatment. Angle Orthod. 1986;43:132–140. doi: 10.1043/0003-3219(1986)056<0205:VCIFOT>2.0.CO;2. [DOI] [PubMed] [Google Scholar]
- 7.Hang W.M. How many years must a profession exist…? Cranio. 2006;24:73–75. doi: 10.1179/crn.2006.012. [DOI] [PubMed] [Google Scholar]
- 8.McDougall P.D., McNamara J.A., Jr., Dierkes J.M. Arch width development in class II patients treated with the Fränkel appliance. Am J Orthod. 1982;82:10–22. doi: 10.1016/0002-9416(82)90541-3. [DOI] [PubMed] [Google Scholar]
- 9.Ozbek M.M., Memikoglu T.U., Gögen H., Lowe A.A., Baspinar E. Oropharyngeal airway dimensions and functional-orthopedic treatment in skeletal class II cases. Angle Orthod. 1998;68:327–336. doi: 10.1043/0003-3219(1998)068<0327:OADAFO>2.3.CO;2. [DOI] [PubMed] [Google Scholar]
- 10.Singh G.D., Garcia-Motta A.V., Hang W.M. Evaluation of the posterior airway space following Biobloc therapy: geometric morphometrics. Cranio. 2007;25:84–89. doi: 10.1179/crn.2007.014. [DOI] [PubMed] [Google Scholar]
- 11.Tsai H.H. Developmental changes of pharyngeal airway structures from young to adult persons. J Clin Pediatr Dent. 2007;31:219–221. doi: 10.17796/jcpd.31.3.023h753711p24273. [DOI] [PubMed] [Google Scholar]
- 12.Kiliaridis S., Mejersjo C., Thilander B. Muscle function and cranio-facial morphology: a clinical study in patients with myotonic dystrophy. Eur J Orthod. 1989;11:131–138. doi: 10.1093/oxfordjournals.ejo.a035975. [DOI] [PubMed] [Google Scholar]
- 13.Mew J.R. Facial changes in identical twins treated by different orthodontic techniques. World J Orthod. 2007;8:174–188. [PubMed] [Google Scholar]
- 14.Sharma K., Shrivastav S., Sharma N., Hotwani K., Murrell M.D. Effects of first premolar extraction on airway dimensions in young adolescents: a retrospective cephalometric appraisal. Contemp Clin Dent. 2014;5:190–194. doi: 10.4103/0976-237X.132314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Valiathan M., El H., Hans M.G., Palomo M.J. Effects of extraction versus non-extraction treatment on oropharyngeal airway volume. Angle Orthod. 2010;80:1068–1074. doi: 10.2319/010810-19.1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stefanovic N., El H., Chenin D.L., Glisic B., Palomo J.M. Three-dimensional pharyngeal airway changes in orthodontic patients treated with and without extractions. Orthod Craniofac Res. 2012;15:1–10. doi: 10.1111/ocr.12009. [DOI] [PubMed] [Google Scholar]
- 17.Lamichane M., Anderson N.K., Rigali P.H., Seldin E.B., Will L.A. Accuracy of reconstructed images from cone-beam computed tomography scans. Am J Orthod Dentofacial Orthop. 2009;136:1–6. doi: 10.1016/j.ajodo.2009.04.006. [DOI] [PubMed] [Google Scholar]
- 18.Mah J., Hatcher D. Three-dimensional craniofacial imaging. Am J Orthod Dentofacial Orthop. 2004;126:308–309. doi: 10.1016/j.ajodo.2004.06.024. [DOI] [PubMed] [Google Scholar]
- 19.Kau C.H., Richmond S., Palomo J.M., Hans M.G. Three-dimensional cone beam computerized tomography in orthodontics. J Orthod. 2005;32:282–293. doi: 10.1179/146531205225021285. [DOI] [PubMed] [Google Scholar]
- 20.De Backer J.W., Vos W.G., Verhulst S.L., De Backer W. Novel imaging techniques using computer methods for the evaluation of the upper airway in patients with sleep-disordered breathing: a comprehensive review. Sleep Med Rev. 2008;12:437–447. doi: 10.1016/j.smrv.2008.07.009. [DOI] [PubMed] [Google Scholar]
- 21.Germec Cakanet D., Taner T., Akan S. Uvuloglossopharyngeal dimensions in non-extraction, extraction with minimum anchorage, and extraction with maximum anchorage. Eur J Orthod. 2011;33:515–520. doi: 10.1093/ejo/cjq109. [DOI] [PubMed] [Google Scholar]
- 22.Pliska B.T., Tam I.T., Lowe A.A., Madson A.M., Almeida F.R. Effect of orthodontic treatment on the upper airway volume in adults. Am J Orthod Dentofacial Orthop. 2016;150:937–944. doi: 10.1016/j.ajodo.2016.05.013. [DOI] [PubMed] [Google Scholar]
- 23.Nuvusetty B., Peddu R., Prakash A.S., Kalyani M., Devikanth L., Chadalawada D. Assessment of changes in pharyngeal airway size and hyoid bone position following orthodontic treatment of Class I bimaxillary dentoalveolar protrusion. J Indian Orthod Soc. 2016;50:215–221. [Google Scholar]
- 24.de Cassia Gonçalves Renata, Barnabé Raveli Dirceu. Ary dos Santos Pinto Effects of age and gender on upper airway, lower airway and upper lip growth. Braz Oral Res. 2011;25(3):241–247. doi: 10.1590/s1806-83242011000300009. [DOI] [PubMed] [Google Scholar]
- 25.Adamidis I.P., Spyropoulos M.N. The effects of lymphadenoid hypertrophy on the position of the tongue, the mandible and the hyoid bone. Eur J Orthod. 1983;5(4):287–294. doi: 10.1093/ejo/5.4.287. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.