Abstract
Hesperidin is a vitamin P flavonoid compound primarily present in citrus fruits, which possesses an anti-inflammatory effect. The functional role of hesperidin in interleukin (IL)-1β-stimulated human osteoarthritis (OA) chondrocytes is still unknown. In the present study, anti-inflammatory effects of hesperidin in IL-1β-stimulated chondrocytes were investigated. The results demonstrated that hesperidin treatment markedly decreased nitric oxide and prostaglandin E2 production and markedly downregulated inducible nitric oxide synthase and cyclooxygenase-2 expression in IL-1β-stimulated OA chondrocytes. In addition, hesperidin markedly reduced IL-1β-induced matrix metalloproteinase (MMP)-3 and MMP-13 expression in human OA chondrocytes. Furthermore, hesperidin markedly decreased the activation of nuclear factor (NF)-κB in human OA chondrocytes. In conclusion, it was revealed for the first time that hesperidin inhibited inflammatory responses in IL-1β-stimulated human chondrocytes, potentially through inhibiting the activation of the NF-κB signaling pathway. These data suggest that hesperidin may be a potential agent for the treatment of OA.
Keywords: hesperidin, osteoarthritis, inflammation, nuclear factor κB
Introduction
Osteoarthritis (OA) is a degenerative disease, with patients exhibiting joint pain, joint swelling, restricted movement and joint deformities (1). OA is an autoimmune disease and an increasing number of patients (~8%) with OA have been diagnosed in the clinic since 2008 worldwide (2–4). OA is divided into primary and secondary OA, according to the presence of local and systemic risk factors, including inflammation and genetic factors (5). The causes of OA are complex, including genetic, physical and chemical factors, which are difficult to classify with regards to a systematic model (6). The pathogenesis associated with this disease is not well understood and OA is frequently misdiagnosed as rheumatoid arthritis or ankylosing spondylitis in clinical settings (7–9).
Hesperidin is a flavanone glycoside, which is a vitamin P flavonoid compound (10). A previous study reported biological activities of hesperidin and its molecular mechanisms, including involvement in the nuclear factor erythroid 2-related factor/extracellular signal-regulated kinase, No/cGFP and phosphoinositide 3-kinase/mitogen-activated protein kinase signaling pathways in neuropharmacology (11). In addition, the therapeutic effects of hesperidin on cardiac tissue and renal and hepatic damage have been evaluated in several reports (12–14). Another study revealed that hesperidin presented protective effects against radiation-induced hepatic injury and damage to peripheral blood lymphocytes (15). Furthermore, hesperidin ameliorates oxidative stress and mitochondrial dysfunction by activation of antioxidant enzymes, including superoxide dismutase, catalase and glutathione-S-transferase (16). In addition, hesperidin alleviates acetaminophen-induced toxicity in Wistar rats by abrogation of oxidative stress, apoptosis and inflammation (17). However, the anti-inflammatory effects of hesperidin on inflammation in human osteoarthritis chondrocytes remain unclear.
A previous study indicated that cyclooxygenase (COX)-2-selective inhibitors may be used for the treatment of rheumatoid arthritis (18). Matrix metalloproteinase (MMP) protein and activity levels are upregulated in synovial fluid from patients with joint injury, inflammatory arthritis and osteoarthritis compared to healthy controls (19). Notably, nuclear factor (NF)-κB activation has been observed to increase in OA articular chondrocytes (20). In the current study, the efficacy of hesperidin in interleukin (IL)-1β-stimulated human chondrocytes was investigated. The study further explored potential mechanisms mediated by hesperidin in human chondrocytes and reported an association between hesperidin and NF-κB signaling pathway activation in IL-1β-stimulated human chondrocytes.
Materials and methods
Cell culturing and treatment
Human OA chondrocytes were obtained from the Department of Anatomy & Neurobiology, Northeast Ohio Medical University (Ohio, USA) and cultured in RPMI 1640 medium (Thermo Fisher Scientific, Inc., Waltham, MA, USA) supplemented with 10% heat-inactivated fetal bovine serum (Thermo Fisher Scientific, Inc.) at 37°C in 5% CO2. Cells were treated with IL-1β (2.0 mg/ml, Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) and/or hesperidin (2.0 mg/ml), NF-κB inhibitor (NF-κBIR; cat. no. LY-294.002; 2.0 mg/ml, Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) or PBS (Sigma-Aldrich; Merck KGaA, Darmstadt, Germany) for 24 h at 37°C. The groups are as follows: PBS, IL-1β, NF-κBIR, hesperidin and IL-1β+hesperidin.
Reverse transcription-quantitative polymerase chain reaction (RT-qPCR) analysis
Total RNA from human OA chondrocytes (1×108 cells) was extracted using an RNAeasy Mini kit (Qiagen Sciences, Inc., Gaithersburg, MD, USA) following the manufacturer's protocol. RNA was reverse transcribed into cDNA at 42°C for 2 h using the High Capacity cDNA Reverse Transcription kit (Thermo Fisher Scientific, Inc.) according to the manufacturer's protocol. Expression levels of mRNAs in cells were measured by qPCR. Forward and reverse primers were synthesized by Invitrogen (Thermo Fisher Scientific, Inc.; Table I). PCR amplification started with a preliminary denaturation step at 94°C for 2 min, followed by 45 cycles of 95°C for 30 sec, 56°C for 30 sec (annealing) and 72°C for 45 sec. The reaction volume was 20 µl, containing 50 ng genomic cDNA, 200 µM dNTPs, 200 µM primers, 2.5 U Taq DNA polymerase and 2.5 U SYBR-Green (Thermo Fisher Scientific, Inc.). Relative mRNA expression changes were calculated by the 2−ΔΔCq method (21). Results are presented as the n-fold change compared with β-actin.
Table I.
Primers for reverse transcription-quantitative polymerase chain reaction.
| Gene | Forward (5′-3′) | Reverse (5′-3′) |
|---|---|---|
| IL-6 | TTCCATCCAGTTGCCTTCTTGG | TTCTCATTTCCACGATTTCCCAG |
| IL-1β | GGCTGCTTCCAAACCTTTGA | GAAGACACGGATTCCATGGT |
| IL-17A | ATGCACAGCCACCGCGACTT | CTTCATGACTGCCTCCAAGTAG |
| IL-10 | CAGTGCAGAAGAGTCGACTGCAAG | CGCTTGAGATCCTGAAATATA |
| COX-2 | TCAAAACCGAGGTGTA | GTGGGTAAGTATGTAGTGC |
| iNOS | GTTGGTACATGGGCACTGAG | TATGGTGGTCGGTAATGGTG |
| MMP-3 | TCCCTCAGGAAGCTTGAACCTGAA | AAACCTAGGGTGTGGATGCCTCTT |
| MMP-13 | TGCTTCCTGATGACGATGTAC | TCCTCGGAGACTGGTAATGG |
| β-actin | CGGAGTCAACGGATTTGGTC | AGCCTTCTCCATGGTCGTGA |
IL, interleukin; COX-2, cyclooxygenase-2; iNOS, inducible nitric oxide synthase; MMP, matrix metalloproteinase.
Cell viability
Human OA chondrocytes (1×103/well) were seeded in 96-well plates following treatment with IL-1β (2.0 mg/ml) and/or hesperidin (2.0 mg/ml; IL-1β, IL-1β+hesperidin and hesperidin groups) for 24 h at 37°C, and treated with 10 µl MTT (5 mg/ml, Sigma-Aldrich; Merck KGaA) for 3 h at 37°C. Following incubation, purple formazan crystals were dissolved using isopropanol (15 µl). The absorbance was recorded using a microplate reader (Multiskan FC, Thermo Fisher Scientific, Inc.) at 570 nm. The effects of hesperidin on cell viability were determined by the percent of cell viability, calculated as the ratio between mean absorbance of three samples and mean absorbance of the IL-1β group.
Cell transfection
Human OA chondrocytes (1×106/well, untreated cells) were cultured in six-well plates for 12 h at 37°C. The NF-κB overexpression plasmid was synthesized by cloning human NF-κB cDNA into plasmid pcDNA3.1 (pNF-κB; Suzhou GenePharma Co., Ltd., Suzhou, China) and the empty plasmid pcDNA3.1 served as the control (pControl). Cells were transfected pNF-κB (100 pmol) or pControl (100 pmol) using Lipofectamine 3000 reagent (Invitrogen, Thermo Fisher Scientific, Inc.) according to the manufacturer's protocol. Following 48 h transfection, NF-κB-overexpressed cells were treated with hesperidin (2.0 mg/ml) for 24 h at 37°C further analysis.
Production of nitric oxide (NO) and prostaglandin E2 (PGE2)
After 48 h transfection, NF-kB-overexpressed cells, treated with hesperidin or PBS, were used to detect NO and PGE2 production. Production of NO was assessed by measuring the nitrite content in the culture supernatant was obtained via centrifugation at 4,000 × g at room temperature for 10 min following mixing of the culture with Griess reagent (1% sulphanilamide, 0.1% N−1-naphthylenediamine dihydrochloride and 2.5% phosphoric acid). The absorbance was measured at 540 nm following 10 min of incubation at 37°C. The levels of PGE2 were analyzed using the Prostaglandin E2 Parameter Assay kit (KGE004B, Bio-Rad Laboratories, Inc., Hercules, CA, USA) according to the manufacturer's instructions.
Western blot analysis
After 48 h transfection, NF-kB-overexpressed human OA chondrocytes (1×107) treated with hesperidin or PBS were lysed using radioimmunoprecipitation lysis buffer (Thermo Fisher Scientific, Inc.). Protein concentrations were measured using a BCA protein assay kit (Thermo Fisher Scientific, Inc.). Equal amounts of proteins (10 µg) were separated using 12% SDS-PAGE and transferred to a polyvinylidene fluoride membrane (Merck KGaA). Following blocking with 5% bovine serum albumin for 2 h at 37°C, membranes were incubated with primary antibodies for 12 h at 4°C: IL-1β (1:1,000; ab200478; Abcam, Cambridge, UK), IL-17A (1:1,000; ab193955; Abcam), IL-6 (1:1,000; ab7737; Abcam), IL-10 (1:1,000; ab19969; Abcam), COX-2 (1:1,000; ab15191; Abcam), PGE-2 (1:1,000; ab181249; Abcam), inducible nitric oxide synthase (iNOS; 1:1,000; ab15323; Abcam), MMP-3 (1:1,000; ab53015; Abcam), MMP-13 (1:1,000; ab39012; Abcam) and β-actin (1:2,000; ab8226; Abcam). Horseradish peroxidase-conjugated anti-rabbit IgG antibody (1:2,000; PV-6001; OriGene Technologies, Inc., Beijing, China) was incubated with the membrane for 24 h at 4°C. Membranes were washed with PBS and visualized with an electrochemiluminescence western blotting detection reagent (Amersham; GE Healthcare, Chicago, IL, USA). The band intensities were analyzed by ImageJ software 1.0 (National Institutes of Health, Bethesda, MD, USA).
NF-κB activity
NF-kB-overexpressed with or without hesperidin human OA chondrocytes (1×106/well) were cultured in six-well plates for 12 h at 37°C. The 3′-untranslated region (3′-UTR) sequence of NF-κB was inserted into the pGL3 control vector (Promega Corporation, Madison, WI, USA). The construct was referred to as NF-κB-3′-UTR. Cells were washed with PBS and transfected with NF-κB-3′-UTR or control (NF-κB-3′-mimic; Promega Corporation) using Lipofectamine 3000 (Thermo Fisher Scientific, Inc.) according to the manufacturer's instructions. Cells were collected using centrifugation in 4,000 × g at room temperature for 15 min after 48 h at 37°C and Renilla luciferase activity was measured using the Dual-Luciferase Reporter Assay system (Promega Corporation) according to the manufacturer's protocols. Results were obtained from three independent experiments performed in duplicate and normalized to Renilla.
Statistical analysis
Data are expressed as the mean ± standard deviation and statistical analysis was performed with SPSS 18.0 (SPSS, Inc., Chicago, IL, USA). Statistically significant differences between groups were analyzed by one-way analysis of variance followed by Tukey's honest significant difference test. P<0.01 was considered to indicate a statistically significant difference.
Results
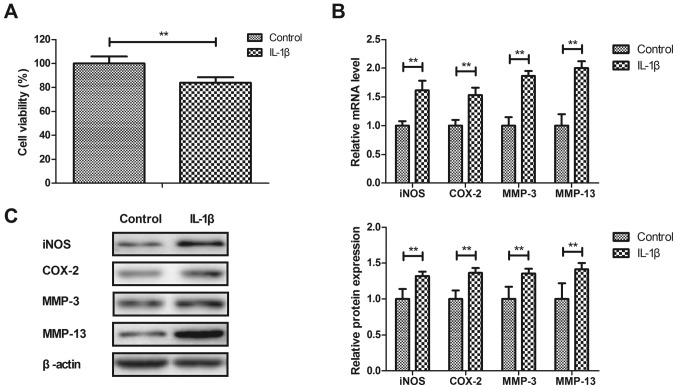
IL-1β stimulates inflammation in human OA chondrocytes
Anti-inflammatory effects of IL-1β on human OA chondrocytes were investigated in vitro. As illustrated in Fig. 1A, IL-1β significantly decreased the viability of human OA chondrocytes after 24 h compared with the control (P<0.01). IL-1β significantly increased iNOS, COX-2, MMP-3 and MMP-13 gene and protein expression in human OA chondrocytes compared with the PBS-treated cells (P<0.01; Fig. 1B and C). These results indicated that IL-1β stimulated inflammation in human OA chondrocytes.
Figure 1.
Effects of IL-1β on viability and inflammatory cytokine expression in human OA chondrocytes. (A) Effects of IL-1β on viability of human OA chondrocytes in vitro. IL-1β increased iNOS, COX-2, MMP-3 and MMP-13 (B) gene and (C) protein expression in human OA chondrocytes. **P<0.01. OA, osteoarthritis; IL, interleukin; iNOS, inducible nitric oxide synthase; COX-2, cyclooxygenase-2; MMP, matrix metalloproteinase. Control group, PBS-treated cells.
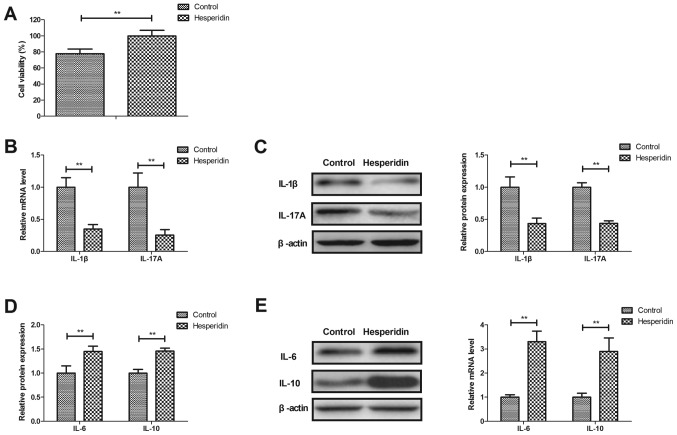
Hesperidin attenuates inflammation in IL-1β-stimulated human OA chondrocytes
Effects of hesperidin on inflammation in IL-1β-stimulated human OA chondrocytes were investigated in vitro. Hesperidin significantly increased the viability of human OA chondrocytes compared with the PBS-treated group (P<0.01; Fig. 2A). Hesperidin treatment significantly decreased IL-1β and IL-17A gene and protein expression (P<0.01; Fig. 2B and C) and significantly increased IL-6 and IL-10 gene and protein expression in IL-1β-stimulated human OA chondrocytes compared with the PBS-treated cells (P<0.01; Fig. 2D and E). These results indicated that hesperidin may attenuate inflammation in IL-1β-stimulated human OA chondrocytes.
Figure 2.
Hesperidin regulates inflammation in IL-1β-stimulated human OA chondrocytes. (A) Hesperidin increases the viability of human OA chondrocytes in vitro. Effects of hesperidin on IL-1β and IL-17A (B) gene and (C) protein expression in IL-1β-stimulated human OA chondrocytes. Effects of hesperidin treatment on IL-6 and IL-10 (D) gene and (E) protein expression in IL-1β-stimulated human OA chondrocytes. **P<0.01. OA, osteoarthritis; IL, interleukin. Control group, PBS-treated cells.
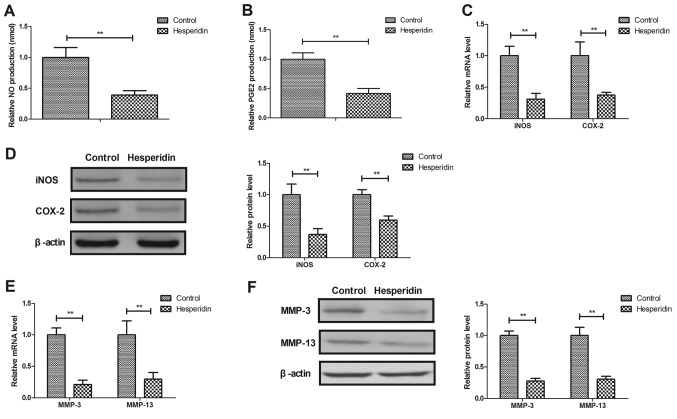
Hesperidin inhibits IL-1β-induced MMP-3 and MMP-13 release in human OA chondrocytes
Hesperidin effects on NO, PGE2, iNOS and COX-2 expression in IL-1β-stimulated human OA chondrocytes were further investigated. It was revealed that hesperidin significantly decreased NO and PGE2 production (P<0.01; Fig. 3A and B) and significantly inhibited iNOS and COX-2 gene and protein expression in IL-1β-stimulated OA chondrocytes compared with the PBS-treated cells (P<0.01; Fig. 3C and D). Hesperidin further significantly inhibited IL-1β-induced MMP-3 and MMP-13 release in human OA chondrocytes compared with the control (PBS-treated cells; P<0.01; Fig. 3E and F). These results suggested that hesperidin may inhibit the IL-1β-induced NO and MMP signaling pathways in human OA chondrocytes.
Figure 3.
Effects of hesperidin on IL-1β-induced inflammation in human OA chondrocytes. Effects of hesperidin on (A) NO and (B) PGE2 production in IL-1β-stimulated OA chondrocytes. Effects of hesperidin on iNOS and COX-2 (C) gene and (D) protein expression in IL-1β-stimulated human OA chondrocytes. Effects of hesperidin on IL-1β-induced MMP-3 and MMP-13 (E) gene and (F) protein expression in human OA chondrocytes. **P<0.01 vs. control. OA, osteoarthritis; IL, interleukin; NO, nitric oxide; PGE2, prostaglandin E2; iNOS, inducible NO synthase; COX-2, cyclooxygenase-2; MMP, matrix metalloproteinase. Control group, PBS-treated cells.
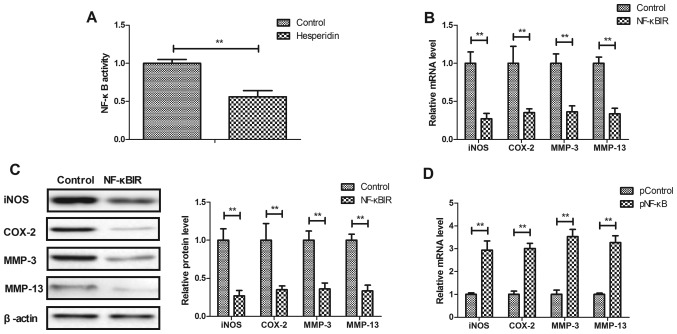
Hesperidin affects IL-1β-stimulated inflammation by inhibiting NF-κB activity in human OA chondrocytes
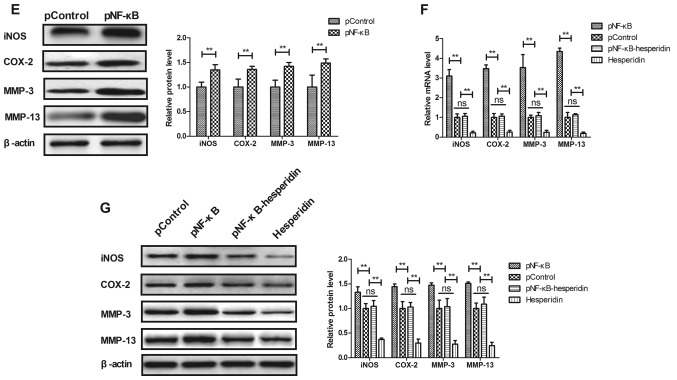
The potential mechanism mediated by hesperidin was analyzed in human OA chondrocytes. It was observed that hesperidin significantly decreased the activity of NF-κB in IL-1β-stimulated human OA chondrocytes compared with the PBS-treated cells (P<0.01; Fig. 4A). Additionally, NF-κBIR treatment significantly decreased iNOS, COX-2, MMP-3 and MMP-13 gene and protein expression in IL-1β-stimulated human OA chondrocytes compared with the PBS-treated cells (P<0.01; Fig. 4B and C). NF-κB overexpression, induced by transfection with pNF-κB, significantly increased iNOS, COX-2, MMP-3 and MMP-13 gene and protein expression in IL-1β-stimulated human OA chondrocytes compared with the pControl (P<0.01; Fig. 4D and E). The results also demonstrated that NF-κB overexpression reversed hesperidin-inhibited iNOS, COX-2, MMP-3 and MMP-13 gene and protein expression in IL-1β-stimulated human OA chondrocytes compared with the PControl group (Fig. 4F and G). These results indicated that hesperidin inhibited IL-1β-stimulated inflammation by the inhibiting NF-κB activity in human OA chondrocytes.
Figure 4.
Hesperidin inhibits IL-1β-stimulated inflammation by reducing NF-κB activity in human OA chondrocytes. (A) Hesperidin decreases the activation of NF-κB in IL-1β-stimulated human OA chondrocytes. Effects of NF-κBIR on iNOS, COX-2, MMP-3 and MMP-13 (B) gene and (C) protein expression in IL-1β-stimulated human OA chondrocytes. Effects of pNF-κB on iNOS, COX-2, MMP-3 and MMP-13 (D) gene and (E) protein expression in IL-1β-stimulated human OA chondrocytes. Effects of pNF-κB on hesperidin-inhibited IL-1β-stimulated iNOS, COX-2, MMP-3 and MMP-13 (F) gene and (G) protein expression in IL-1β-stimulated human OA chondrocytes. **P<0.01. OA, osteoarthritis; IL, interleukin; NF-κB, nuclear factor-κB; NO, nitric oxide; PGE2, prostaglandin E2; iNOS, inducible nitric oxide synthase; COX-2, cyclooxygenase-2; MMP, matrix metalloproteinase; NF-κBIR, NF-κB inhibitor; pNF-κB, NF-κB overexpression; pControl, empty pcDNA3.1.
Discussion
A previous study revealed that hesperidin attenuates inflammation and oxidative damage in the pleural exudates and the liver of a rat model of pleurisy (22). However, the role of hesperidin in human OA chondrocytes is yet to be elucidated. In the current study, the role of hesperidin in IL-1β-stimulated human OA chondrocytes was analyzed. The findings revealed that hesperidin significantly decreased IL-1β and IL-17A gene and protein expression, while it increased IL-6 and IL-10 gene and protein expression in IL-1β-stimulated human OA chondrocytes compared with the PBS group. The current study observed that hesperidin inhibited IL-1β-stimulated inflammation in human OA chondrocytes.
Currently, anti-IL-1β therapy is an efficient treatment method for patients with OA (23). Liu et al (24) indicated that IL-17 serves a crucial role in the pathogenesis of OA and is closely associated with pain, which suggests that blocking the IL-17 signaling pathway may contribute to the treatment of OA. It was reported in the current study that hesperidin decreased IL-1β and IL-17A and increased IL-6 and IL-10 gene and protein expression in human OA chondrocytes, which has previously been indicated to be beneficial in OA therapy (24).
Suppressing NF-κB activity attenuates pain and inflammation in rats with osteoarthritis (25). Hesperidin has been reported to suppress oxidative stress and inflammation via activation of the protein kinase B/nuclear factor erythroid 2-related factor 2 signaling pathway, inhibition of the receptor for advanced glycation end products/NF-κB signaling pathway and further confers neuroprotection (26). In the current study, it was revealed that hesperidin significantly inhibited NF-κB activity in IL-1β-stimulated human OA chondrocytes.
Suppression of PGE2 and MMP expression was indicated to inhibit cartilage degradation by pomegranate fruit extracts in a model of posttraumatic osteoarthritis (27). Another study reported that patients with OA exhibited significantly higher COX-2 levels compared with the healthy control group (28). In the current study, findings demonstrated that hesperidin significantly decreased PGE2 and COX-2 expression in IL-1β-stimulated human OA chondrocytes compared with PBS-treated cells. A previous study has demonstrated that demethylation of an NF-κB enhancer element induced iNOS production in OA and is associated with an altered chondrocyte cell cycle (29). In the current study, results revealed that hesperidin inhibited iNOS and COX-2 gene and protein expression in IL-1β-stimulated human OA chondrocytes compared with PBS-treated cells. Findings suggested that hesperidin regulated iNOS and COX-2 expression via the inhibition of NF-κB activity in IL-1β-stimulated human OA chondrocytes compared with PBS-treated cells.
In conclusion, the findings of the current study suggest that hesperidin downregulated inflammation in IL-1β-stimulated human OA chondrocytes and highlight the potential application of hesperidin for OA therapy based on decreasing NF-κB activity. The current study suggests that hesperidin may be a potential agent for the inhibition of inflammation in the treatment of OA.
Acknowledgements
Not applicable.
Funding
The current study was supported by the Natural Science Foundation of Guangdong Province (grant no. 2015A030310248).
Availability of data and materials
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors' contributions
ZF designed the experiments. ZC and QX performed the experiments. HL and SX acquired and interpreted all data in the present study. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The current study was approved by the Ethical Committee of Jiangmen Central Hospital, Jiangmen (Jiangmen, China).
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Onuora S. Osteoarthritis: Molecular imaging detects activated macrophages. Nat Rev Rheumatol. 2016;12:313. doi: 10.1038/nrrheum.2016.70. [DOI] [PubMed] [Google Scholar]
- 2.Meheux CJ, McCulloch PC, Lintner DM, Varner KE, Harris JD. Efficacy of intra-articular platelet-rich plasma injections in knee osteoarthritis: A systematic review. Arthroscopy. 2016;32:495–505. doi: 10.1016/j.arthro.2015.08.005. [DOI] [PubMed] [Google Scholar]
- 3.Monticone M, Frizziero A, Rovere G, Vittadini F, Uliano D, LA Bruna S, Gatto R, Nava C, Leggero V, Masiero S. Hyaluronic acid intra-articular injection and exercise therapy: Effects on pain and disability in subjects affected by lower limb joints osteoarthritis. A systematic review by the italian society of physical and rehabilitation medicine (SIMFER). Eur J Phys Rehabil Med 52: 389–399, 2016. Eur J Phys Rehabil Med 52: 389–399, 2016. 2016;52: 389–399, 2016:389-399, 2016–399, 2016. [PubMed] [Google Scholar]
- 4.Hammond A, Jones V, Prior Y. The effects of compression gloves on hand symptoms and hand function in rheumatoid arthritis and hand osteoarthritis: A systematic review. Clin Rehabil. 2016;30:213–224. doi: 10.1177/0269215515578296. [DOI] [PubMed] [Google Scholar]
- 5.Tang H, He S, Zhang X, Luo S, Zhang B, Duan X, Zhang Z, Wang W, Wang Y, Sun Y. A network pharmacology approach to uncover the pharmacological mechanism of XuanHuSuo powder on osteoarthritis. Evid Based Complement Alternat Med 2016. 2016:3246946. doi: 10.1155/2016/3246946. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Roemer FW, Kwoh CK, Hannon MJ, Hunter DJ, Eckstein F, Grago J, Boudreau RM, Englund M, Guermazi A. Partial meniscectomy is associated with increased risk of incident radiographic osteoarthritis and worsening cartilage damage in the following year. Eur Radiol. 2017;27:404–413. doi: 10.1007/s00330-016-4361-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Malfait AM. Osteoarthritis year in review 2015: Biology. Osteoarthritis Cartilage. 2016;24:21–26. doi: 10.1016/j.joca.2015.09.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Maleki M, Arazpour M, Joghtaei M, Hutchins SW, Aboutorabi A, Pouyan A. The effect of knee orthoses on gait parameters in medial knee compartment osteoarthritis: A literature review. Prosthet Orthot Int. 2016;40:193–201. doi: 10.1177/0309364614547411. [DOI] [PubMed] [Google Scholar]
- 9.Li Y, Su Y, Chen S, Zhang Y, Zhang Z, Liu C, Lu M, Liu F, Li S, He Z, et al. The effects of resistance exercise in patients with knee osteoarthritis: A systematic review and meta-analysis. Clin Rehabil. 2016;30:947–959. doi: 10.1177/0269215515610039. [DOI] [PubMed] [Google Scholar]
- 10.La Torre F, Nicolai AP, Otti M. Hemorrhoids and conservative treatment. Review of the literature on the use of diosmin and micronized hesperidin. Minerva Chir. 1999;54:909–916. (In Italian) [PubMed] [Google Scholar]
- 11.Roohbakhsh A, Parhiz H, Soltani F, Rezaee R, Iranshahi M. Neuropharmacological properties and pharmacokinetics of the citrus flavonoids hesperidin and hesperetin-a mini-review. Life Sci. 2014;113:1–6. doi: 10.1016/j.lfs.2014.07.029. [DOI] [PubMed] [Google Scholar]
- 12.Antunes MS, Goes AT, Boeira SP, Prigol M, Jesse CR. Protective effect of hesperidin in a model of Parkinson's disease induced by 6-hydroxydopamine in aged mice. Nutrition. 2014;30:1415–1422. doi: 10.1016/j.nut.2014.03.024. [DOI] [PubMed] [Google Scholar]
- 13.Wang D, Liu L, Zhu X, Wu W, Wang Y. Hesperidin alleviates cognitive impairment, mitochondrial dysfunction and oxidative stress in a mouse model of Alzheimer's disease. Cell Mol Neurobiol. 2014;34:1209–1221. doi: 10.1007/s10571-014-0098-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kumar A, Chaudhary T, Mishra J. Minocycline modulates neuroprotective effect of hesperidin against quinolinic acid induced Huntington's disease like symptoms in rats: Behavioral, biochemical, cellular and histological evidences. Eur J Pharmacol. 2013;720:16–28. doi: 10.1016/j.ejphar.2013.10.057. [DOI] [PubMed] [Google Scholar]
- 15.Li G, Chen MJ, Wang C, Nie H, Huang WJ, Yuan TD, Sun T, Shu KG, Wang CF, Gong Q, Tang SQ. Protective effects of hesperidin on concanavalin A-induced hepatic injury in mice. Int Immunopharmacol. 2014;21:406–411. doi: 10.1016/j.intimp.2014.05.018. [DOI] [PubMed] [Google Scholar]
- 16.Poetini MR, Araujo SM, Trindade de Paula M, Bortolotto VC, Meichtry LB, Polet de Almeida F, Jesse CR, Kunz SN, Prigol M. Hesperidin attenuates iron-induced oxidative damage and dopamine depletion in Drosophila melanogaster model of Parkinson's disease. Chem Biol Interact. 2018;279:177–186. doi: 10.1016/j.cbi.2017.11.018. [DOI] [PubMed] [Google Scholar]
- 17.Ahmad ST, Arjumand W, Nafees S, Seth A, Ali N, Rashid S, Sultana S. Hesperidin alleviates acetaminophen induced toxicity in Wistar rats by abrogation of oxidative stress, apoptosis and inflammation. Toxicol Lett. 2012;208:149–161. doi: 10.1016/j.toxlet.2011.10.023. [DOI] [PubMed] [Google Scholar]
- 18.Hochberg MC. Treatment of rheumatoid arthritis and osteoarthritis with COX-2-selective inhibitors: A managed care perspective. Am J Manag Care. 2002;8(17 Suppl):S502–S517. [PubMed] [Google Scholar]
- 19.Tchetverikov I, Lohmander LS, Verzijl N, Huizinga TW, TeKoppele JM, Hanemaaijer R, DeGroot J. MMP protein and activity levels in synovial fluid from patients with joint injury, inflammatory arthritis, and osteoarthritis. Ann Rheum Dis. 2005;64:694–698. doi: 10.1136/ard.2004.022434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Xu L, Sun C, Zhang S, Xu X, Zhai L, Wang Y, Wang S, Liu Z, Cheng H, Xiao M, et al. Sam68 promotes NF-κB activation and apoptosis signaling in articular chondrocytes during osteoarthritis. Inflamm Res. 2015;64:895–902. doi: 10.1007/s00011-015-0872-3. [DOI] [PubMed] [Google Scholar]
- 21.Livak KJ, Schmittgen TD. Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) method. Methods. 2001;25:402–408. doi: 10.1006/meth.2001.1262. [DOI] [PubMed] [Google Scholar]
- 22.Adefegha SA, Rosa Leal DB, Olabiyi AA, Oboh G, Castilhos LG. Hesperidin attenuates inflammation and oxidative damage in pleural exudates and liver of rat model of pleurisy. Redox Rep. 2017;22:563–571. doi: 10.1080/13510002.2017.1344013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Chevalier X, Conrozier T, Richette P. Desperately looking for the right target in osteoarthritis: The anti-IL-1 strategy. Arthritis Res Ther. 2011;13:124. doi: 10.1186/ar3436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Liu Y, Peng H, Meng Z, Wei M. Correlation of IL-17 level in synovia and severity of knee osteoarthritis. Med Sci Monit. 2015;21:1732–1736. doi: 10.12659/MSM.893771. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Dai T, Shi K, Chen G, Shen Y, Pan T. Malvidin attenuates pain and inflammation in rats with osteoarthritis by suppressing NF-κB signaling pathway. Inflamm Res. 2017;66:1075–1084. doi: 10.1007/s00011-017-1087-6. [DOI] [PubMed] [Google Scholar]
- 26.Hong Y, An Z. Hesperidin attenuates learning and memory deficits in APP/PS1 mice through activation of Akt/Nrf2 signaling and inhibition of RAGE/NF-κB signaling. Arch Pharm Res. 2018;41:655–663. doi: 10.1007/s12272-015-0662-z. [DOI] [PubMed] [Google Scholar]
- 27.Akhtar N, Khan NM, Ashruf OS, Haqqi TM. Inhibition of cartilage degradation and suppression of PGE2 and MMPs expression by pomegranate fruit extract in a model of posttraumatic osteoarthritis. Nutrition. 2017;33:1–13. doi: 10.1016/j.nut.2016.08.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Fan HW, Liu GY, Zhao CF, Li XF, Yang XY. Differential expression of COX-2 in osteoarthritis and rheumatoid arthritis. Genet Mol Res. 2015;14:12872–12879. doi: 10.4238/2015.October.21.7. [DOI] [PubMed] [Google Scholar]
- 29.de Andrés MC, Takahashi A, Oreffo RO. Demethylation of an NF-κB enhancer element orchestrates iNOS induction in osteoarthritis and is associated with altered chondrocyte cell cycle. Osteoarthritis Cartilage. 2016;24:1951–1960. doi: 10.1016/j.joca.2016.06.002. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.