Abstract
Background:
Health-seeking behaviours (HSB) are closely linked with the health status of a nation and thus its economic development. Several studies have described HSB within the context of various diseases. However, knowledge of HSB among population sub-groups is still scanty. This study aims to determine factors most important to civil servants when seeking health care.
Methods:
A descriptive cross-sectional study was conducted among 337 civil servants working in the Federal Secretariat, Ibadan, Nigeria. An intervieweradministered semi-structured questionnaire was used to collect information. Chi-square tests were used to test for associations while binary logistic regression test was used for determining predictors. All data analysis were done at 5% level of significance.
Results:
Members of the poorest quartile were 6 times more likely to have inappropriate HSB than the richest quartile (Q4:Q1= 5.83;O.R: 16.12, 95% C.I: 2.61-11.03). Visits to the hospital or clinic (62.2%) was the most common source of healthcare sought. This was followed by visits to the chemist (33.0%), traditional healers (4.3%). A little more than one-third (34.5%) of respondents considered good service delivery as the most important factor affecting HSB. This was followed by proximity (23.9%), affordability (20.4%), prompt attention (8.8%) and readily-available drugs (7.1%). Completing only basic education [O.R: 0.24 (0.06, 0.96)] and out of pocket payment [O.R: 0.04 (9.16, 82.45)] were associated with a reduction in the likelihood of seeking healthcare from formal sources.
Conclusion:
Appropriate health-seeking behaviour was found to be high among civil servants. However, lower cadre workers and those with lower levels of education need to be targeted during policy formulation to improve health-seeking behaviour. In addition, health insurance schemes should be extended to cover more of the population in order to improve health-seeking behaviour.
Keywords: Health seeking behaviour, Civil servants, Healthcare provider, Service-based characteristics.
INTRODUCTION
Healthcare seeking behaviour (HSB) has been defined as, "any action or inaction undertaken by individuals who perceive themselves to have a health problem or to be ill for the purpose of finding an appropriate remedy".1 Health seeking behaviour can also be referred to as illness behaviour or sick-term behaviour. Health seeking behaviour is situated within the broader concept of health behaviour, which encompasses activities undertaken to maintain good health, to prevent ill health, as well as dealing with any departure from a good state of health.2
Studies that have attempted to describe factors that significantly affect health seeking behaviour during illness episodes can be broadly classified into two groups.2-4 The first group are studies which emphasize the utilization of the formal system, or the health care seeking behaviour of people. The studies that fall under this category involve the development of models that describe the series of steps people take towards health care. These models are sometimes referred to as 'pathway models'.5 While there are several variations of these models, the Health Belief Model and Andersen's Health Behaviour Model are often used as a basis in discussions involving HSB.5,6 The second group comprises those studies which emphasize the process of illness response, or health seeking behaviour. These studies demonstrate that the decision to engage with a particular medical channel is influenced by a variety of factors such as socio-economic status, sex, age, the social status, the type of illness, access to services and perceived quality of the service.7,8 Majority of the studies under this second category focus on specific genres of determinants which lie between patients and services such as geographical, social, economic, cultural and organizational factors.9-11 For example, access to health facilities, socio-economic status and perceived quality of service have been found to be significant influencers of health seeking decisions among different population segments.9,12,13
Inappropriate HSB has been linked to worse health outcomes, increased morbidity and mortality and poorer health statistics.14,15 Research into HSB in LMICs suggests several factors influence the HSB of the population and certain segments of the population are more likely to use appropriate HSB than others. Inappropriate HSB and its previously mentioned effects have been found to be skewed among different population segments. For example, in Pakistan, households whose average income was below the minimum wage were less likely to seek formal medical care for their illness than those whose incomes were above the minimum wage.16 In Kenya, almost 70% of pregnant women within households in the upper socio-economic stratum were found to have their deliveries in health facilities compared with 42% among pregnant women in the middle socio-economic stratum and 38% in the low socio-economic stratum.13
In a study in Nigeria, as many as 71% of rural dwellers have reported inappropriate HSB during their last illness episode while only 53% of urban dwellers reported inappropriate HSB during their last illness episode.17 Similarly, Nigerian women living in areas where the ratio of population to Primary Healthcare Centre (PHC) was high (more than 9,000:1) were less likely to have a skilled birth attendant present during childbirth than areas where the ratio of population to Primary Healthcare Centre (PHC) was lower (less than 6,000:1).18 This disparity makes it necessary to determine the factors affecting HSB among different segments of the population. This is essential to guide policy formulation and implementation. An important aspect of HSB is the choice of healthcare provider made by people when responding to illness episodes. This study seeks to identify which socio-demographic and health service-based factors influence HSB among civil servants, who represent a sizeable proportion of the working population in the country.
METHODS
Study design
This descriptive cross-sectional study was conducted between August and September 2014 at the Federal Secretariat Complex, Ikolaba, Ibadan, Nigeria. Ibadan is the ancient capital city of Oyo State, located in the south-west of Nigeria. The inhabitants are mainly Yorubas, with clusters of Igbos and Hausas living in several areas. The Federal Secretariat is situated at Ikolaba.
Study population
The population under study were the Federal civil servants working at the Federal Secretariat Complex, Ikolaba, Ibadan. There are 8 ministries and 13 agencies located within the secretariat with a staff strength of 853 working within the Complex as at April 2014. A minimum sample size of 246 was calculated using 5% level of significance, 5% level of precision and 20% as the proportion of people who use appropriate HSB.19 Selection of respondents was through a multistage sampling technique. The first stage involved the selection of 3 ministries and 6 agencies randomly out of the 8 ministries and 15 agencies in the secretariat by balloting. The second stage was the selection of staff in the chosen ministries and agencies. This was done by proportionally allocating the required sample size to the selected ministries and agencies according to their individual staff strength after which required respondents were selected at regular intervals of the sampling fraction. The sampling fraction was obtained by dividing the required number of respondents in the ministry or agency by the total number of staff (Table 1).
Table 1:
Distribution of staff and sample size
| S/N | MINISTRY/PARASTATAL | Staff Strength | Minimum Sample size required | Sample size Obtained |
|---|---|---|---|---|
|
| ||||
| 1 | Ministry of Lands and Housing | 45 | 64 | |
| 2 | Ministry Of Works | 140 | 71 | 101 |
| 3 | Ministry of Steel and Mines | 33 | 17 | 24 |
| 4 | National Commission for Mass Literacy, Adult Literacy and Non-formal Education | 70 | 35 | 51 |
| 5 | Office of the Auditor-General of the Federation | 24 | 12 | 17 |
| 6 | National Films and Video Censure Board | 13 | 7 | 9 |
| 7 | Nigerian Population Commission | 15 | 8 | 11 |
| 8 | National Bureau of Statistics | 21 | 11 | 15 |
| 9 | National Directorate on Employment | 79 | 40 | 58 |
| TOTAL | 483 | 246 | 350 | |
Inclusion and exclusion criteria
The study included all Federal civil servants working within the Secretariat who have been employed for at least one year as at the time of the study but excluded all temporary staff or contract staff under the employment of any of the agencies or ministries.
Study variables
In this study, appropriate HSB was defined as consulting a qualified medical professional or seeking healthcare at orthodox health facilities such as private clinics, primary health centres, and general hospitals during illness episodes or any situation requiring medical attention.10,20 Inappropriate HSB comprises seeking healthcare from patent medicine vendors (PMVs), chemists, traditional healers, family members or doing nothing at all. Traditional healers are nonqualified persons who treat the sick children using traditional nonmedical methods. Patent Medicine Vendors (PMVs) or chemists are nonqualified persons who sell drugs without medical prescription.
Study variables used to determine the factors influencing HSB included socio-demographic subject characteristics such as age, marital status, highest level of education completed, family size and socioeconomic status. Respondents were grouped into wealth quartiles using the Wealth Index and Principal Component Analysis (PCA). Wealth Index (WI) is one of the methods of evaluating wealth distribution. It is a composite index composed of key asset ownership and is often used as a proxy indicator of level of household wealth.21 Principal components analysis was employed to produce a factor score for each household based on ownership of certain assets such as fan, radio, television sets, etc. Based on the total factor score of each household, the respondents were then grouped into wealth quartiles (poorest, poor, rich and richest) representing their socio-economic class.22 Health service characteristics are explanatory factors associated with the performance of the formal healthcare system which can influence HSB.23 These include accessibility to health facilities, availability of drugs, quality of medical care, and attitude of health workers and affordability of medical care cost. For the purpose of inferential statistics, educational qualification was categorized according to the level of school education completed. Basic education was defined as completing only secondary school education while tertiary education was defined as having any form of formal post-secondary educational qualification. Respondents were also categorized into cadres based on their salary grade level. Junior cadre workers were defined as workers from salary grade level 1 to 6 while mid-level workers are classified as those with salary grade level 7 and 10. Senior level workers are those on salary grade level 11 and above.
Data collection
Data was collected with the aid of intervieweradministered semi-structured questionnaires. Four research assistants who had at least completed secondary school were trained and used for the data collection procedure. The questionnaire was divided into the following sections: socio-demographic information, socio-economic information, HSB patterns of respondents and HSB patterns of their immediate family members. The questionnaire was pretested among 40 civil servants of the Ibadan North Local Government Secretariat and necessary adjustments were made.
Data analysis
The data were coded, checked, and processed with version 20 Statistical Package for the Social Sciences. Descriptive statistics, such as means, standard deviations (SD), frequencies, and proportions, were used to summarize variables. Chi-square tests were used to identify associations between categorical variables using a P-value of 0.05 as the significance level. Logistic regression analysis was conducted to determine significant predictors of outcomes with estimation of the odds ratio and 95% CI (Confidence Interval). Only explanatory variables found to be significantly associated in the Chi-square analyses were entered into the logistic regression model.
Ethical considerations
The University College Hospital (UCH) Ethics Review Committee reviewed and approved the study protocol (Approval number: UI/EC/14/0171). Permission and approval to conduct the study was also obtained from the heads of the selected ministries and departments. In addition, the purpose of the study was explained to the participants and their consent obtained before the questionnaire were administered.
RESULTS
Socio-demographic Characteristics
A total of 337 questionnaires were completed out of the 350 questionnaires administered giving a response rate of 96.3%. Exactly 187 (55.5%) of the respondents being male and 150 (44.5%) were female. The mean age of the respondents was 41.5 ± 9.6 years with 262 (77.7%) of the respondents being married and 67 (19.6%) being single. Three (0.9%) respondents were divorced or separated from their partners while 5 (1.5%) were widowed. Over half 188 (55.8%) were mid-level workers with 51 (15.1%) working as senior level workers and the remaining 98 (29.1%) were low cadre workers. Two hundred and forty (71.5%) reported having completed tertiary education, only 96 (28.5%) completed only basic education. The mean household size was 4.2 ± 2.1 persons with only 24 (7.1%) respondents having over six members in their household (Table 2). Two hundred and fifteen (63.5%) of the respondents had a health problem within the last month and 187 (86.5%) of them sought treatment. The average delay among those who sought treatment within the past month was 2.5 ± 1.9 days.
Table 2:
Socio-demographic characteristics (N=337)
| n | % | |
|---|---|---|
|
| ||
| Gender | ||
| Male | 187 | 55.5 |
| Female | 150 | 44.5 |
| Marital status | ||
| Single | 67 | 19.9 |
| Married | 262 | 77.7 |
| Separated/Divorced | 3 | 0.9 |
| Widowed | 5 | 1.5 |
| Age Group (in years) | ||
| ≤ 29 | 43 | 12.8 |
| 30-39 | 107 | 31.8 |
| 40-49 | 110 | 32.6 |
| ≥ 50 | 77 | 22.8 |
| Grade Category | ||
| Junior | 98 | 29.1 |
| Mid-level | 188 | 55.8 |
| Senior level | 51 | 15.1 |
| Household size | ||
| ≤6 | 313 | 92.9 |
| >6 | 24 | 7.1 |
| Level of Education | ||
| Basic | 96 | 28.5 |
| Tertiary | 241 | 71.5 |
| Socio-Economic Status (SES) | ||
| Poorest (Q1) | 60 | 17.8 |
| Poor (Q2) | 109 | 32.3 |
| Rich (Q3) | 84 | 24.9 |
| Richest (Q4) | 84 | 24.9 |
Socio-demographic Factors associated with HSB of the respondents
Exactly 37.0% of the male respondents who sought healthcare within the past month and 36.7% of their female counterparts sought care from an informal source. However, a greater percentage of respondents who completed only basic education engaged informal health sources (72.2%) compared to those who used formal health sources (27.8%) as shown in Table 3.
Table 3:
Factors associated with HSB of respondents who were sick within the past one month (N=187)
| Care sought from informal source | Care sought from formal source | |||||
|---|---|---|---|---|---|---|
| Characteristics | n | % | n | % | X2 | p-value |
|
| ||||||
| Gender | 0.002 | 0.96 | ||||
| Male | 40 | 37.0 | 68 | 63.0 | ||
| Female | 29 | 36.7 | 50 | 63.3 | ||
| Marital Status | 0.38 | 0.54 | ||||
| Currently Single | 11 | 42.3 | 15 | 57.7 | ||
| Married | 58 | 36.0 | 103 | 64.0 | ||
| Age Group | 1.90 | 0.59 | ||||
| < 29 | 4 | 25.0 | 12 | 75.0 | ||
| 30-39 | 21 | 42.9 | 28 | 57.1 | ||
| 40-49 | 23 | 37.7 | 38 | 62.3 | ||
| > 50 | 21 | 34.4 | 40 | 65.6 | ||
| Level of Education | 40.69 | <0.01 | ||||
| Basic | 39 | 72.2 | 15 | 27.8 | ||
| Tertiary | 30 | 22.6 | 103 | 77.4 | ||
| Grade Level | 43.76 | <0.01 | ||||
| Junior-level | 32 | 78.0 | 9 | 22.0 | ||
| Mid-level | 33 | 31.1 | 73 | 68.9 | ||
| Senior Level | 4 | 10.0 | 36 | 90.0 | ||
| Household Size | * | 0.02 | ||||
| <6 | 60 | 34.5 | 114 | 65.5 | ||
| >6 | 9 | 62.9 | 4 | 30.8 | ||
| Payment Method | 73.17 | <0.01 | ||||
| OOP | 48 | 81.4 | 11 | 18.6 | ||
| NHIS | 21 | 16.4 | 107 | 83.6 | ||
| Insurance Status | 73.43 | <0.01 | ||||
| Insured | 25 | 18.4 | 111 | 81.6 | ||
| Uninsured | 44 | 86.3 | 7 | 13.7 | ||
| SES | ||||||
| Poorest | 35 | 70.0 | 15 | 30.0 | 36.83 | <0.01 |
| Poor | 12 | 33.3 | 24 | 66.7 | ||
| Rich | 16 | 34.8 | 30 | 65.2 | ||
| Richest | 6 | 10.9 | 49 | 89.1 | ||
| Poorest-richest ratio | 5.83 | 0.3 | ||||
Fishers Exact Test
A greater proportion of insured respondents (111; 81.6%) used the formal healthcare system as opposed to only seven (13.7%) of individuals without insurance. The association between socio-economic status and health seeking behaviour was also statistically significant with care from the formal health sector being increasing sought as the SES improved. This was with the exception of the rich who had a slightly lower proportion of respondents (30, 65.2%) using formal health care sources than the poor (24; 66.7%)
Reasons for choice of health facility/ health provider utilized
Respondents who had sought healthcare in the past one month were asked what the most important reason for selecting the health provider. With regards to the most important service factor affecting respondents' choice of healthcare provider, 34.5% of respondents considered the good services provided by the provider as the most important reason for their patronage of such provider. This was followed by proximity (23.9%), affordability of services (20.4%), prompt attention (8.8%) and readily available drugs (7.1%). Politeness and courtesy among health workers was least considered a factor in selecting healthcare provider (5.3%).
Affordability (33.3%) was the important reason for selecting health provider among respondents who completed only basic education. On the contrary, affordability was the second least popular reason (6.8%) for selecting health provider among respondents who completed tertiary education.
While provision of good services was the most important reason among married respondents, affordability was the most important reason among currently single respondents. Similarly, affordability was the most important reason for junior staff and respondents aged 29 and lower. A little more than a quarter of junior staff cited proximity as their reason for selecting healthcare provider while 10.3% of senior staff cited politeness of health provider as the main reason for their choice of healthcare provider. (Table 4).
Table 4:
Association between service characteristics and socio-demographic characteristics
| Good services provided | Readily available drugs | Near | Affordable services | Prompt attention | Polite Workers | X p-value* | |
|---|---|---|---|---|---|---|---|
| n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | n (%) | |
|
| |||||||
| Gender | |||||||
| Male | 41(37.4) | 13 (12.1) | 20 (18.7) | 15(14.0) | 14 (13.1) | 5(4.7) | 0.75 |
| Female | 33(41.8) | 12 (15.2) | 14 (17.7) | 12(15.2) | 7(8.9) | 1(1.3) | |
| Level of Education | |||||||
| Basic | 7 (13.0) | 16 (29.6) | 12 (22.2) | 18(33.3) | 1(1.9) | 0(0.0) | <0.001 |
| Tertiary | 66 (50.0) | 9(6.8) | 22 (16.7) | 9(6.8) | 20 (15.2) | 6(4.5) | |
| Marital Status | |||||||
| Single | 5 (20.8) | 1(4.2) | 6(25.0) | 7(29.2) | 5(20.8) | 0(0.0) | 0.06 |
| Married | 67 (42.1) | 24 (15.1) | 27 (17.0) | 19(11.9) | 16 (10.1) | 6(3.8) | |
| Separated/Divorced | 0(0.0) | 0(0.0) | 0(0.0) | 1(100.0) | 0(0.0) | 0(0.0) | |
| Widowed | 1(50.0) | 0(0.0) | 1(50.0) | 0(0.0) | 0(0.0) | 0(0.0) | |
| Grade Level | <0.01 | ||||||
| Junior Staff | 2(4.9) | 10(24.4) | 11(26.8) | 16(39.0) | 2 (4.9) | 0(0.0) | |
| Mid-level Staff | 47(44.3) | 15(14.2) | 20(18.9) | 10(9.4) | 12 11.3) | 2(1.9) | |
| Senior Staff | 21(61.5) | 0 (0.0) | 3(7.7) | 1(2.6) | 7(17.9) | 4 10.3) | |
| Age Group | <0.01 | ||||||
| 29 and less | 4(25.0) | 0(0.0) | 3(18.8) | 5(31.2) | 4(25.0) | 0(0.0) | |
| 30-39 | 15(30.6) | 5(10.2) | 13(26.5) | 8(16.3) | 8(16.3) | 0(0.0) | |
| 40-49 | 25(41.0) | 13(21.3) | 13(21.3) | 5(8.2) | 4(6.6) | 1(1.6) | |
| >50 | 29(48.3) | 7(11.7) | 5(8.3) | 9(15.0) | 5(8.3) | 5(8.3) | |
| Occurrence of CHE | <0.01 | ||||||
| Yes | 6(14.6) | 8(19.5) | 10(24.4) | 15(36.6) | 2(4.9) | 0(0.0) | |
| No | 67(47.2) | 17(11.7) | 24(16.6) | 12(8.3) | 19(13.1) | 6(4.1) | |
Fishers Exact Test
A logistic regression was performed to ascertain the effects of socio-demographic factors, socio-economic status and payment method on the likelihood that respondents seek health care from formal sources. The model explained 61% (Nagelkerke R2) of the variance in health-seeking behavior and correctly classified 62.9% of cases. Significant variables in the model included educational status, payment method. Of these, completing only basic education and increased delay in seeking treatment were associated with a reduction in the likelihood of seeking healthcare from formal sources while enrolled members of NHIS were 27.49 times more likely to seek healthcare from formal sources than respondents who pay OOP Table 5.
Table 5:
Factors associated with HSB (N=187)
| Coefficient* | S.E** | O.R*** | 95% C.I | ||
|---|---|---|---|---|---|
| Lower | Upper | ||||
|
| |||||
| Level of Education | |||||
| Basic | -1.42 | 0.73 | 0.24 | 0.06 | 0.96 |
| Tertiary | 1.00 | ||||
| Household size | |||||
| <6 | 0.48 | 1.27 | 1.62 | 0.133 | 19.67 |
| >6 | 1.00 | ||||
| Grade Level | |||||
| Junior | -1.76 | 1.08 | 0.17 | 0.02 | 1.43 |
| Mid-level | -1.16 | 0.77 | 0.31 | 0.07 | 1.41 |
| Senior level | 1.00 | ||||
| Socio-Economic Status (SES) | |||||
| Poorest | -0.68 | 1.02 | 0.51 | 1.07 | 3.79 |
| Poor | -0.03 | 0.84 | 0.98 | 0.19 | 5.09 |
| Rich | -1.16 | 0.73 | 0.31 | 1.08 | 3.30 |
| Richest | 1.00 | ||||
| Payment Method | |||||
| NHIS | 3.31 | 0.56 | 27.49 | 9.16 | 82.45 |
| OOP | 1.00 | ||||
Coefficient expressed in logits
Standard Error
Odds Ratio
DISCUSSION
The health-seeking behaviour of civil servants in the study was remarkably better than that of the general population. 24,25 In this study, 63.1% of the respondents used formal healthcare sources. This proportion of respondents with appropriate HSB is higher than reported by Onwujekwe et al (2011), and other Nigerian studies who measured HSB using the source of healthcare provider.17,25,26 These studies reported only about 30% to 40% of the population as seeking health care at formal health centres as compared with the 63.1% found in this study. This is to be expected though, as these studies were carried out either wholly or in part with the rural populace in South-eastern Nigeria. The proportion is however consistent with findings from other studies who used federal civil servants as their study population.25,27 With respect to the specific health provider, only 4.3% of respondents used informal health care centres. This is considerably lower than was reported in other studies. For example, Oyibo (2011) reported that as much as 17.1% of civil servants used herbal medicines as a form health treatment.28 This may be because the study included other government workers who are not yet covered by NHIS. However, this proportion is similar to that reported by Onwujekwe et al (2011) and Uzochukwu et al (2008) indicating that civil servants may not differ from the urban population in terms of their proportions that use traditional medicine.17,29 This proportion, though, is also lower than is reported in urban areas of other LMICs showing that civil servants in Nigeria may have better health seeking behaviour than similar countries where source of healthcare was used to measure HSB. About sixty percent of respondents used the hospital or clinic as the first source of treatment. This is considerably higher than has been found in other studies where values ranged from between 8% and 30%.30,31 This is further indication of better health-seeking behaviour among federal civil servants than the general population. However, chemists or patent medicine vendors were the most sought healthcare providers among those who pay OOP. This is consistent with findings in other Nigerian studies among populations who pay primarily OOP.24,28,32
In general, the majority of the respondents believed that provision of good services was the most important reason for their choice of health provider. The study reports affordability of services as the most important factor respondents who used out-of-pocket payment. This concurs with other Nigerian studies investigating factors influential to choice of provider among out of pocket.33,34 For example, Omotoso (2010) discovered that populations without insurance consider affordability as most important along to closeness to their residence.24 This study further revealed that the likelihood of seeking appropriate healthcare improved as socio-economic status improved. This concurs with findings that inability to pay for health services is a major factor determining the utilization of health services.28,35 This further affirms that underutilization of formal health services especially by the poor and disadvantaged remains a chronic problem in developing countries even though there is a huge unmet need for health care.36
Unlike in some previous studies, women in this study were found to be as likely to have appropriate healthseeking behaviour as men.10,37 This may indicate that female federal civil servants are aware of the importance of appropriate treatment service and its sources. One possible explanation for this could be that they have enough access to information due to their constant exposure to sources of information at their workplace. Furthermore, they are economically less dependent on their husbands as they are income earners. In addition, they have enough education to participate in making household decisions including seeking healthcare in time of illness and do not totally depend on their husbands' decisions.
Inappropriate health-seeking behaviour was observed among participants from larger family sizes in this study. This might be due to the fact that those who had larger family members shouldered more family responsibilities and experienced severe socioeconomic hardships, which prevented them from visiting appropriate healthcare facilities for their illnesses. This corresponds with findings by Manzi et al (2014) in Rwanda.38
A potential bias in this study was recall bias. This might have been present as is usual in self-reported prevalence surveys. Recall bias was reduced by limiting enquiries on health-seeking to one month. This cut-off has been used widely by researchers in several countries.26,39 Another limitation is that income earned were likely to have been overestimated.27 Analysis was therefore not based on only income. Presence of household assets were used to derive wealth quartiles. The cros-ssectional nature of this study does not allow inferences to be made from its results. The results of this study can also be representative of civil servants living only in Oyo State.
CONCLUSION
Respondents' characteristics such as completing tertiary education, having lower household sizes, belonging to higher socio-economic status quartile and participation in National Health Insurance Scheme were significantly associated with seeking appropriate health seeking behaviour. Providing good services, affordability of such services and proximity were considered the most important service characteristics in seeking health seeking behaviour. Thus, policy formulation and implementation should be directed towards improving access to healthcare services. This can be done by increasing the number of health facilities in under-served areas. The quality of care provided at health facilities also requires attention as mentoring, supportive supervision and other measures could be embarked upon in order improve quality of care. Issues concerning affordability of such health services can be addressed by up-scaling the coverage of the National Health Insurance Scheme, the country's flagship insurance scheme. This would provide financial protection for households with lower socioeconomic status in order to encourage use of appropriate healthcare sources during illness episodes.
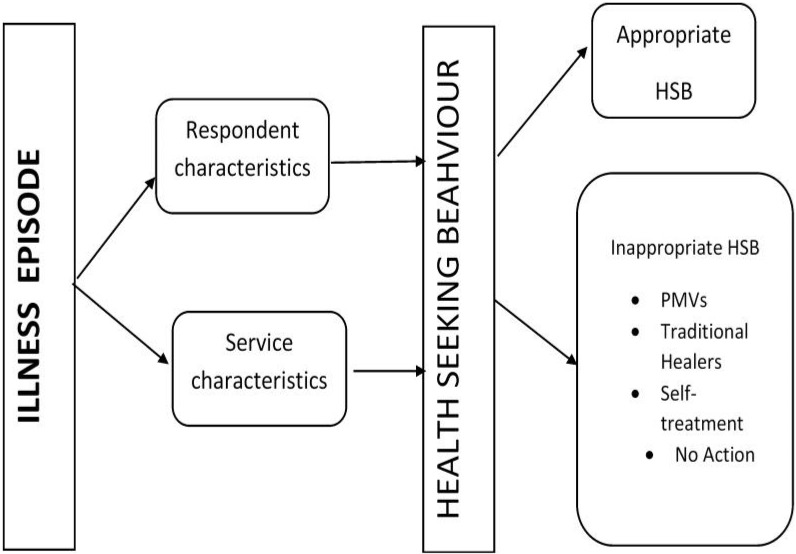
Fig. 1:
Framework for the study
(HSB – Health Seeking Behaviour; PMVs – Patent Medicine Vendors)
REFERENCES
- 1.Olenja J. Editorial Health seeking behaviour in context. 2004. [DOI] [PubMed]
- 2.MacKian S. A review of health seeking behaviour: problems and prospects. Health Systems Development Programme. 2003.
- 3.Geldsetzer P, Williams TC, Kirolos A, et al. The recognition of and care seeking behaviour for childhood illness in developing countries: a systematic review. PloS one. 2014;9(4):e93427. doi: 10.1371/journal.pone.0093427. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Moyer CA, Adongo PB, Aborigo RA, et al. "It's up to the woman's people": how social factors influence facility-based delivery in Rural Northern Ghana. Maternal and child health journal. 2014;18(1):109–119. doi: 10.1007/s10995-013-1240-y. [DOI] [PubMed] [Google Scholar]
- 5.Rosenstock IM. Why people use health services. Milbank Quarterly. 2005;83(4) [Google Scholar]
- 6.Andersen RM. Revisiting the behavioral model and access to medical care: does it matter? Journal of health and social behavior. 1995;1:10. [PubMed] [Google Scholar]
- 7.Cronin T, Sheppard J, de Wildt G. Health-seeking behaviour for schistosomiasis: a systematic review of qualitative and quantitative literature. The Pan African medical journal. 2013;16 doi: 10.11604/pamj.2013.16.130.3078. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Webair HH, Bin-Gouth AS. Factors affecting health seeking behavior for common childhood illnesses in Yemen. Patient Preference & Adherence. 2013;7 doi: 10.2147/PPA.S51124. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gao W, Dang S, Yan H, Wang D. Care-seeking pattern for diarrhea among children under 36 months old in rural western China. PloS one. 2012;7(8):e43103. doi: 10.1371/journal.pone.0043103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Senbeto M, Tadesse S, Tadesse T, Melesse T. Appropriate health-seeking behavior and associated factors among people who had cough for at least two weeks in northwest Ethiopia: a population-based cross-sectional study. BMC public health. 2013;13(1):1222. doi: 10.1186/1471-2458-13-1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Worku AG, Yalew AW, Afework MF. Maternal complications and women's behavior in seeking care from skilled providers in North Gondar, Ethiopia. PLoS One. 2013;8(3):e60171. doi: 10.1371/journal.pone.0060171. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Babalola S, Fatusi A. Determinants of use of maternal health services in Nigeria-looking beyond individual and household factors. BMC pregnancy and childbirth. 2009;9(1):43. doi: 10.1186/1471-2393-9-43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Phiri SNa, Kiserud T, Kvale G, et al. Factors associated with health facility childbirth in districts of Kenya, Tanzania and Zambia: a population based survey. BMC pregnancy and childbirth. 2014;14(1):219. doi: 10.1186/1471-2393-14-219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Atuyambe LM. Adolescent motherhood in Uganda: Dilemmas, health seeking behaviour and coping responses. 2008.
- 15.Mwase I. Social capital and household healthseeking behaviour for children in the context of urban neighbourhoods. The case of Khayelitsha in Western Cape, South Africa: University of Cape Town. 2015.
- 16.Rehman A, Shaikh BT, Ronis KA. Health care seeking patterns and out of pocket payments for children under five years of age living in Katchi Abadis (slums), in Islamabad, Pakistan. International journal for equity in health. 2014;13(1):30. doi: 10.1186/1475-9276-13-30. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Onwujekwe O, Onoka C, Uzochukwu B, Hanson K. Constraints to universal coverage: inequities in health service use and expenditures for different health conditions and providers. International journal for equity in health. 2011;10(1):50. doi: 10.1186/1475-9276-10-50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ononokpono DN, Odimegwu CO. Determinants of maternal health care utilization in Nigeria: a multilevel approach. The Pan African medical journal. 2014;17(Suppl 1) doi: 10.11694/pamj.supp.2014.17.1.3596. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Ewelukwa O, Onoka C, Onwujekwe O. Viewing health expenditures, payment and coping mechanisms with an equity lens in Nigeria. BMC health services research. 2013;13(1):87. doi: 10.1186/1472-6963-13-87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Ogunlesi TA, Olanrewaju DM. Sociodemographic factors and appropriate health careseeking behavior for childhood illnesses. Journal of tropical pediatrics. 2010;56(6):379–385. doi: 10.1093/tropej/fmq009. [DOI] [PubMed] [Google Scholar]
- 21.Fagbamigbe AF, Bamgboye EA, Yusuf BO, et al. The Nigeria wealth distribution and health seeking behaviour: evidence from the 2012 national HIV/AIDS and reproductive health survey. Health economics review. 2015;5(1):5. doi: 10.1186/s13561-015-0043-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Amin R, Shah NM, Becker S. Socioeconomic factors differentiating maternal and child healthseeking behavior in rural Bangladesh: A crosssectional analysis. International journal for equity in health. 2010;9(1):9. doi: 10.1186/1475-9276-9-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Adegoke AA. Correlates of health behavior practices among literate adults of south west, Nigeria. Volume 10 Number 2 December 2010. 2010;26 [Google Scholar]
- 24.Omotoso D. Health seeking behaviour among the rural dwellers in Ekiti State, Nigeria. African Research Review. 2010;4(2) [Google Scholar]
- 25.Ukwaja KN, Alobu I, Nweke CO, Onyenwe EC. Healthcare-seeking behavior, treatment delays and its determinants among pulmonary tuberculosis patients in rural Nigeria: a cross-sectional study. BMC health services research. 2013;13(1):25. doi: 10.1186/1472-6963-13-25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Onwujekwe O, Uzochukwu B, Eze S, et al. Improving equity in malaria treatment: relationship of socio-economic status with health seeking as well as with perceptions of ease of using the services of different providers for the treatment of malaria in Nigeria. Malaria Journal. 2008;7(1):5. doi: 10.1186/1475-2875-7-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Ilesanmi OS, Adebiyi AO, Fatiregun AA. National health insurance scheme: how protected are households in Oyo State, Nigeria from catastrophic health expenditure? 2014. [DOI] [PMC free article] [PubMed]
- 28.Oyibo P. Out-of-pocket payment for health ser vices: constraints and implications for government employees in Abakaliki, Ebonyi State, south east Nigeria. African health sciences. 2011;11(3) [PMC free article] [PubMed] [Google Scholar]
- 29.Uzochukwu BS, Onwujekwe EO, Onoka CA, Ughasoro MD. Rural-urban differences in maternal responses to childhood fever in South East Nigeria. PLoS One. 2008;3(3):e1788. doi: 10.1371/journal.pone.0001788. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Onah MN, Govender V. Out-of-pocket payments, health care access and utilisation in south-eastern Nigeria: a gender perspective. PLoS One. 2014;9(4):e93887. doi: 10.1371/journal.pone.0093887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Onwujekwe O, Dike N, Ojukwu J, et al. Consumers stated and revealed preferences for community health workers and other strategies for the provision of timely and appropriate treatment of malaria in southeast Nigeria. Malaria journal. 2006;5(1):117. doi: 10.1186/1475-2875-5-117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Ujunwa F, Onwujekwe O, Chinawa J. Health services utilization and costs of the insured and uninsured under the formal sector social health insurance scheme in Enugu metropolis South East Nigeria. Nigerian journal of clinical practice. 2014;17(3):331–5. doi: 10.4103/1119-3077.130235. [DOI] [PubMed] [Google Scholar]
- 33.Biya O, Gidado S, Abraham A, et al. Knowledge, care-seeking behavior, and factors associated with patient delay among newly-diagnosed pulmonary tuberculosis patients, Federal Capital Territory, Nigeria, 2010. Pan African Medical Journal. 2014. [DOI] [PMC free article] [PubMed]
- 34.Ibiwoye A, Adeleke IA. Does national health insurance promote access to quality health care? Evidence from Nigeria. The Geneva papers on Risk and insurance issues and practice. 2008;33(2):219–233. [Google Scholar]
- 35.Nyonator F, Kutzin J. Health for some? The effects of user fees in the Volta Region of Ghana. Health policy and planning. 1999;14(4):329–341. doi: 10.1093/heapol/14.4.329. [DOI] [PubMed] [Google Scholar]
- 36.Carrin G, Mathauer I, Xu K, Evans DB. Universal coverage of health ser vices: tailoring its implementation. Bulletin of the World Health Organization. 2008;86(11):857–863. doi: 10.2471/BLT.07.049387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Onifade DA, Bayer AM, Montoya R, et al. Gender-related factors influencing tuberculosis control in shantytowns: a qualitative study. BMC Public Health. 2010;10(1):381. doi: 10.1186/1471-2458-10-381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Manzi A, Munyaneza F, Mujawase F, et al. Assessing predictors of delayed antenatal care visits in Rwanda: a secondary analysis of Rwanda demographic and health survey 2010. BMC pregnancy and childbirth. 2014;14(1):290. doi: 10.1186/1471-2393-14-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Gotsadze G, Bennett S, Ranson K, Gzirishvili D. Health care-seeking behaviour and out-of-pocket payments in Tbilisi, Georgia. Health policy and planning. 2005;20(4):232–242. doi: 10.1093/heapol/czi029. [DOI] [PubMed] [Google Scholar]