Abstract
Background:
Psychosocial hazards pose a great threat to the mental health of health care workers. There is a dearth of research on this type of hazard in hospital settings in Nigeria.
Objective:
This study aimed to assess the psychosocial hazards and the corresponding risks among health care workers in a tertiary health facility in Rivers State.
Methods:
A cross sectional study was carried out in the University of Port Harcourt Teaching Hospital, Rivers State, Nigeria using qualitative method. Data on the psychosocial hazards were obtained from medical and surgical clinics, medical and surgical wards, theatre, laboratory, radiology and administrative sections of the hospital via key informant interviews. The risk assessment matrix was used to ascertain the risk scores and levels of identified hazards. The scores were summarized using medians and interquartile ranges and the differences in the median scores across the sections were compared using Kruskal Wallis statistics.
Results:
A total of eighteen subjects were interviewed from the sections of the hospital. Work overload had the highest proportion of all the psychosocial hazards in the theatre (83%), radiology (71%), clinic (52%), ward (42%) and laboratory (38%). Other psychosocial hazards were poor interpersonal relationship, assault from patient relatives and job dissatisfaction/boredom. The differences in the median psychosocial hazard risk scores across the sections were not statistically significant (P =0.915).
Conclusion:
This study showed that health care workers are exposed to psychosocial hazards in the workplace. Work policies targeted at addressing these hazards among this group of workers need to be implemented.
Keywords: Psychosocial, Hazards, Health care, Workers, Nigeria
INTRODUCTION
Hospitals are places of treatment and healing for patients, however, they may present a significant number of hazards to the health care workers, which could negatively impact on their health and safety. Health care workers are exposed to one of the most hazardous occupational settings.1,2
Occupational hazards refer to workplace factors, which have a potential to cause harm, injury or ill health.2,3 These hazards could be physical, chemical, mechanical, biological or psychosocial.2,4 In recognition of occupational hazards among health care workers, the 2006 world health report of the World Health Organization (WHO) called for the support and the protection of the health work force.5 The report stated that the working condition of health workers contributes to work attrition in many countries due to work-related illness and injury.5 Noteworthy, the influence of work on health dates back to the late 18th Century, when Bernadino Ramazzinni identified the role of occupation in the dynamics of health and disease.6
Of the various types of hazards, psychosocial hazards impacts the most on the mental wellbeing of health care workers.5,6 Psychosocial hazards refer to those aspects of work design, work organization and management, including their social context, which have potential of inflicting psychological or physical harm.7 Work-related psychosocial hazards include interpersonal relationships at work, work overload, work stress, low job control, bullying, violence and poor organizational justice.2 Prolonged exposure to these psychosocial hazards is related to increased health problems, such as cardiovascular diseases8, and could also contribute to psychiatric disorders, including depression.9,10
Psychosocial hazards are thus associated with the experience of work-related stress. Work-related stress is common and the economic burden of this problem is quite huge. It has a high cost in terms of workers' health, absenteeism and reduced job performance.11 Leka et al. 12 noted that 6.5 million working days are lost each year in the United Kingdom due to workrelated stress. Also, nearly 28% of European workers reported that their mental well-being were hampered following exposure to psychosocial hazards.13 Noteworthy, 50-60% of all lost working days can be attributed to work-related stress and psychosocial risks.13
In spite of the increasing research on psychosocial aspects of work in high-income countries, a dearth of this problem exists in Africa and specifically, Nigeria.14 Hence, there is need to explore the psychosocial hazards among health care workers in low-income countries. Furthermore, this could serve as a basis for instituting occupational health and safety policy and programs tailored to health care workers. This study aimed to identify the psychosocial hazards and ascertain the risks among health care workers in a tertiary health facility in the south-south region of Nigeria.
MATERIALS AND METHODS
This study was carried out in the University of Port Harcourt Teaching Hospital (UPTH), a tertiary health facility located in Rivers State, South-South Nigeria. Although a tertiary health facility, it provides primary, secondary and tertiary health care to people in Rivers state and the neighbouring states. A cross-sectional study design using a qualitative approach was employed in the study. The study population comprised health care workers from the medical and surgical clinics, medical and surgical wards, theatre, laboratory, radiology and administrative sections of the hospital. Health care workers who had worked in these sections for at least five years and who served as the most senior available staff at the time of study constituted key informants.
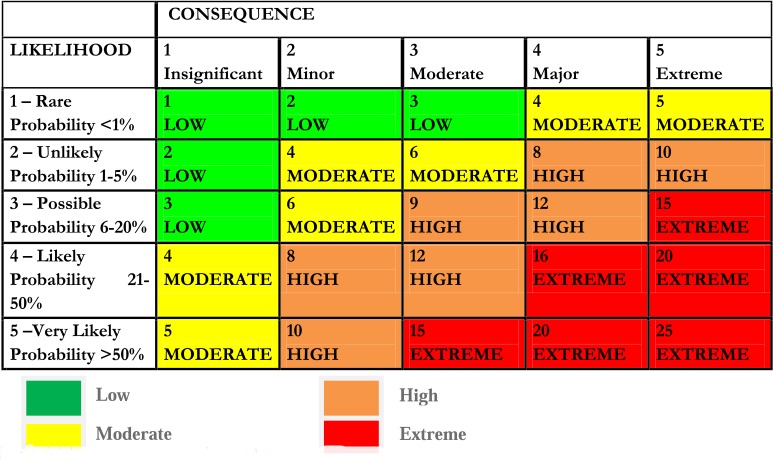
Key Informant Interviews (KII) via a structured guide were used to obtain information on the psychosocial hazards and the risk related to the identified hazards. The risk related to each of the hazards was assessed using the Risk Assessment Matrix (RAM).15 The matrix comprised likelihood of exposure to the hazard, consequence, risk ranking and risk level of the identified hazards. The likelihood (L) of exposure for each hazard was graded on a 1-5 scale representing- Rare, Unlikely, Possible, Likely and Very Likely. The consequence (C) of each exposure was also graded on a scale of 1-5 representing: Insignificant, Minor, Moderate, Major and Extreme. The Risk Ranking scores (rated on scale 1-25) were obtained from the product of the likelihood of exposure and consequence of exposure (L x C). Risk levels were obtained from the risk ranking scores and classified as Low (score of 1-3), Moderate (score of 4-6), High (score of 8-12) or Extreme (score of 15-25). The matrix is represented in Figure 1.
Fig. 1:
Risk Assessment Matrix (RAM)
Data obtained from interviews were analyzed via thematic analysis. The identified themes constituted the psychosocial hazards reported. The risk scores and levels for each of the identified hazards were generated based on the RAM. The risk ranking scores were summed and proportions calculated for each of the identified hazard. The distribution of the identified psychosocial hazards was presented in tabular form. The risk levels of the identified psychosocial hazards were highlighted using the colour-coded matrix.
Data on the psychosocial hazard risk ranking scores were tested for normality using Kolmogorov-Smirnov statistics. Consequently, medians and interquartile range (IQR) were used to summarize the psychosocial risk ranking scores of each section. Kruskal Wallis test was performed to compare the differences in the scores across the sections.
Informed consent was obtained from the participants prior to the interview session. Confidentiality and anonymity were maintained. The note-taking approach during interview sessions was adapted instead of voice recording to further buttress confidentiality of information. The heads of the various units in the hospital granted permission for the study to be conducted.
RESULTS
The study had a total of eighteen subjects, comprised of six females (33.3%) and twelve males (66.7%). Work overload, assault from patients/patients' relatives, poor interpersonal relationship and dissatisfaction/ boredom were the psychosocial hazards identified. The distribution of the risk ranking scores of the identified hazards across the sections of the hospital is shown in Table 1.
Table 1:
Distribution of psychosocial hazards and risk scores across the sections of the hospital
| Psychosocial hazards | |||||
|---|---|---|---|---|---|
| Work Overload | Assault from Patient Relatives | Poor Inter Personal Relationship | Dissatisfaction/Boredom | Total | |
| Sections of the hospital | Risk score (%) | Risk score (%) | Risk score (%) | Risk score (%) | Risk score (%) |
|
| |||||
| Laboratory | 15 (38%) | 12 (31%) | 12 (31%) | 0 (0%) | 39 (100%) |
| Radiology | 15 (71%) | 0 (0%) | 6 (29%) | 0 (0%) | 21 (100%) |
| Clinic | 16 (52%) | 9 (29%) | 6 (19%) | 0 (0%) | 31 (100%) |
| Theatre | 15 (83%) | 0 (0%) | 3 (17%) | 0 (0%) | 18 (100%) |
| Ward | 15 (42%) | 9 (5%) | 12 (33%) | 0 (0%) | 36 (100%) |
| Administrative | 0 (0%) | 0 (0%) | 12 (44%) | 15 (56%) | 27 (100%) |
In all sections of the hospital except the administrative, the psychosocial hazard with the highest risk scores was work overload. Poor interpersonal relationship was the only psychosocial hazard that occurred in all the sections of the hospital. Job dissatisfaction/ boredom was identified only among the administrative section.
Work overload accounted for 38% and 71% of the total psychosocial risk in the laboratory and radiology sections respectively. In the clinics, work overload had the highest proportion (52%) of the psychosocial risk, followed by assault from patients' relatives (29%). More than 80% of the total psychosocial risk among health care workers in the theatre section was attributed to work overload. In the wards, the psychosocial hazards identified were work overload (42%), poor interpersonal relationship (33%) and assault from patients' relatives (25%). In the administrative section, job dissatisfaction/boredom contributed the highest proportion in the risk ranking scores (56%) followed by poor interpersonal relationship (44%). There was no significant difference in the psychosocial risk scores across the sections (Kruskal Wallis = 1.48; P= 0.915) as shown in Table 2.
Table 2:
Comparison of the psychosocial hazards risk ranking scores across the sections of the hospital
| Sections | Psychosocial hazard risk ranking scores | |
|---|---|---|
| Median risk score | Interquartile range (IQR) | |
|
| ||
| Laboratory | 12.0 | 3.0 – 14.3 |
| Radiology | 3.0 | 0.0 – 12.8 |
| Clinic | 7.5 | 1.5 – 14.3 |
| Theatre | 1.5 | 0.0 – 12.0 |
| Ward | 10.5 | 2.3 – 14.3 |
| Administrative | 6.0 | 0.0 – 14.3 |
Kruskal Wallis test =1.48; P = 0.915
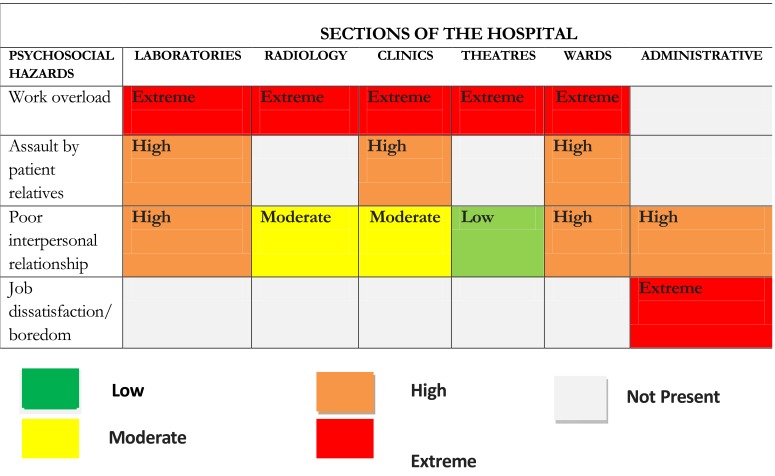
Concerning the risk levels of the identified psychosocial hazards, work overload and job dissatisfaction had extreme risk levels. Assault from patients' relatives had high risk levels while poor interpersonal relationship had risk levels ranging from poor to high depending on the section. The risk levels of the identified psychosocial hazard are represented in the colourcoded matrix (Fig. 2).
Fig. 2:
Colour-coded matrix of risk levels of psychosocial hazards across the sections of the hospital
DISCUSSION
The finding of high work overload among health care workers in the current study has also been documented in other national 16,17,18 and international studies.19,20 It has long been established that both work overload21,22 and work under load22,23 can pose problems for workers. These problems include physical and psychological problems.23 Also, patients could suffer more loss stemming from errors of the health care workers due to the physical and mental fatigue resulting from work overload.24
The presence of poor interpersonal relationship reported in all the sections of the hospital highlights need to institute policies that map out work boundaries and promote cordial working relationships among health care workers within the Nigerian tertiary health facilities. This is because human resources are the most important of all the resources in an organization.25 Furthermore, other researches10,26,27 have linked poor interpersonal relationship in workplace with anxiety, emotional exhaustion, job tension and low job satisfaction with an increased risk of cardiovascular disease.
Although the psychosocial hazard of job dissatisfaction was only reported in the administrative section in this study, it probably exposes the need to introduce non-monotonous elements and possibly widen the scope of work among this group of health care workers. It has been shown that exposure to repetitive and monotonous work is often associated with job dissatisfaction and boredom.28 This hazard has also been linked to poor psychological health22, postural and musculoskeletal problems.29
Assault of health care workers by patients' relatives was not reported in the theatre, administrative and radiology sections. The health care workers in theatre and the administrative sections have a reduced contact period with patients, which may have accounted for the absence of this hazard within these sections of the hospital. It is noteworthy, however, that reducing patient's waiting time and granting warm reception to patient/patient relatives may go a long way in reducing the anxiety that drives the assault on health care workers.30
The comparison of the risk scores across the various psychosocial hazards showed statistically significant differences, with work overload having the highest risk score and job dissatisfaction/boredom, the least risk score. Although, this exposes the need for health facility managers to focus on tackling the issue of high work overload, it is also important for the other forms of psychosocial hazards to be addressed.
The colour-coded matrix highlighting the varying risk levels of the identified hazards showed that work overload had extreme risk levels. This finding further buttresses the need for health managers to prioritize prompt employment of health care workers to fill up deficient positions. The use of the risk assessment matrix in psychosocial hazards is hereby advocated for studies in other health facilities as this could serve as a viable tool in planning and instituting programs for optimal health of the health care workers.
The strength of this study anchors on the presentation of psychosocial hazards risk scores and risk levels, which were obtained from a risk assessment matrix. However, the absence of studies exploring hazards using risk scores and risk levels among health care workers limits comparison to other findings. More studies on occupational hazards among health care workers utilizing these formats are thus needed for comparison of research findings and adoption of best practices. This study did not explore the determinants of the identified hazards in the hospital, nonetheless, the authors recommend future studies using mixed methods of quantitative and qualitative data collection to address this gap in knowledge.
CONCLUSION
This study identified high work overload, poor interpersonal relationships, assault by patients' relatives and job dissatisfaction as the psychosocial hazards experienced by health care workers. The risk levels of these hazards among health care workers varied from low to extreme. Hence, the need to institute workplace policies aimed at curbing these hazards among workers whose work is primarily to ensure the optimal health of the Nigerian populace.
Table 3:
Comparison of the risk ranking scores across the identified psychosocial hazard categories
| Category of psychosocial hazard | Psychosocial hazard risk ranking scores | |
|---|---|---|
| Median risk score | Interquartile range (IQR) | |
|
| ||
| Work overload | 15.0 | 11.3 – 15.3 |
| Assault from patients' relatives | 4.5 | 0.0 – 9.8 |
| Poor inter personal relationship | 9.0 | 5.3 – 12.0 |
| Dissatisfaction/Boredom | 0.0 | 0.0 – 3.8 |
Kruskal Wallis test =9.328; P = 0.025*
*Statistically significant
ACKNOWLEDGEMENTS
The authors acknowledge the contributions of Dr Ibitein N. Okeafor and the support from the staff of Eagles Watch Research Centre and Care during the period of the preparation of this work. We also appreciate the efforts of Dr I.M. Offorma and the encouragement by members of staff of the Department of Community Medicine, University of Port Harcourt Teaching Hospital., Port Harcourt, Rivers State, Nigeria.
CONFLICT OF INTEREST
The authors have no conflict of interest in carrying out this research work.
REFERENCES
- 1.Ndejjo R, Musinguzi G, Yu X, et al. Occupational Health Hazards among Healthcare Workers in Kampala, Uganda. J Env Public Health. 2015. pp. 1–9. [DOI] [PMC free article] [PubMed]
- 2.European Agency for Safety and Health at Work. Risk assesment in health care. 2016. [cited 2016 Nov 1]. pp. 1–8. Available from: http://www.osha.mddsz.gov.si/resources/files/pdf/E-fact_18_-_Risk_assesment_in_health_care.pdf .
- 3.United States Health and Safety Authority. Hazard and Risk. 2013. [cited 2016 Nov 1]. Available from: www.hsa.ie/eng/topics/hazards .
- 4.Asuzu MC. Principles and Practice of Occupational Health. 2nd Ed. Ibadan: Afrik Publshers; 2002. Occupational Hazards; p. 6. [Google Scholar]
- 5.World Health Organization. Health workforce. World Health Report 2006; Geneva. [cited 2016 Oct 11]. Available from: www.who.int/hrh/whr06/en/index.html .
- 6.Franco G, Franco F. Bernardino Ramazzini: The Father of Occupational Medicine. Am J Public Health. 2001;91(9):1382. doi: 10.2105/AJPH.91.9.1382. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Cox T, Griffiths AJ. The assessment of psychosocial hazards at work. In: Schabracq MJ, J.A.M. Winnubst JAM, Cooper CL, editors. Handbook of Work and Health Psychology. Chichester: Wiley & Sons; 1996. [Google Scholar]
- 8.Backe EM, Seidler A, Latza U, et al. The role of psychosocial stress at work for the development of cardiovascular diseases: a systematic review. Int.Arch. Occup. Environ. Health. 2012;85(1):67–79. doi: 10.1007/s00420-011-0643-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cottini E, Lucifora C. Mental health and working conditions in Europe. Ind Labor Relat Rev. 2013;66(4):958–88. [Google Scholar]
- 10.Jain A, Leka S. Health impact of psychosocial hazards at work:an overview. World Health Organization. 2010. [cited 2016 Nov 7]. pp. 1–136. Available from: http://apps.who.int/iris/bitstream/10665/44428/1/9789241500272_eng.pdf .
- 11.International Labour Organization. Psychosocial risks and work-related stress. Work Health Promotion well-being. 2016. [cited 2016 Nov 7]. Available from: http://www.ilo.org/safework/areasofwork/workplace-health-promotion-and-well-being/WCMS_108557/lang en/index.htm .
- 12.Leka S, Jain A, Iavicoli S, et al. An Evaluation of the Policy Context on Psychosocial Risks and Mental Health in the Workplace in the European Union: Achievements, Challenges, and the Future. Biomed Res Int. 2015. pp. 1–18. [DOI] [PMC free article] [PubMed]
- 13.Basiri S, Aria N, Basiri N, et al. Psychological Effects of Stress in the Workplace: A Case study of Stress Management. IJAMCE. 2015;3:439–447. [Google Scholar]
- 14.Owolabi AO, Owolabi MO, OlaOlorun AD, et al. Work-related stress perception and hypertension amongst health workers of a mission hospital in Oyo State, south-western Nigeria. African J Prim Heal Care Fam Med. 2012;14(4(1)) [Google Scholar]
- 15.Portsmouth hospital NHS. Risk Assessment Matrix. Risk Assess Policy Version 4. 2013.
- 16.Mojoyinola J, Ajala E. Burnout syndrome among workers in selected hospitals and industries in Oyo State, Nigeria: Its impacts on their health, wellbeing and job performance. Pakistan J Soc Sci. 2007;4(3):431–436. [Google Scholar]
- 17.Mojoyinola JK. Effects of job stress on health, personal and work behaviour of nurses in public hospitals in Ibadan Metropolis Nigeria. Ethno Med. 2008;2(2):143–148. [Google Scholar]
- 18.Yussuf A, Ajiboye P, Buhari O, Kuranga S. Psychological health problems of resident doctors in a Nigerian teaching hospital environment. SAJP. 2006;12(4):106–111. [Google Scholar]
- 19.Mosadeghrad AM, Ferlie E, Rosenberg D. A study of relationship between job stress, quality of working life and turnover intention among hospital employees. Health Serv Manag Res. 2011;24(4):170–81. doi: 10.1258/hsmr.2011.011009. [DOI] [PubMed] [Google Scholar]
- 20.Beckers Hospital. Top ten challenges facing healthcare workers. Beckers Hospital Review. 2011. [cited 2014 Oct 2]. Available from: www.beckershospiatalreview.com/hospital-management-administration/the-top-10-challenges-facing-health-care-workers.html .
- 21.Portoghese I, Galletta M, Coppola RC, et al. Burnout and Workload Among Health Care Workers: The Moderating Role of Job Control. Safety Health Work. 2014;5(3):152–7. doi: 10.1016/j.shaw.2014.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Shultz KS, Wang M, Olson DA. Role of overload and underload in relation to occupational stress and health. Stress Health. 2010;26(2):99–111. [Google Scholar]
- 23.Harnois G, Gabriel P. Mental health and work: Impact, issues and good practices. World Health Organization. 2010. [cited 2016 Nov 1]. pp. 1–77. Available from: http://www.who.int/mental_health .
- 24.Whitmire AM, Leveton LB, Barger L, et al. Risk of performance errors due to sleep loss, circadian desynchronization, fatigue, and work overload. 2009. [cited 2016 Nov 1]. Available from: https://upload.wikimedia.org/wikipedia/commons/5/51/Effects_of_Sleep_Loss_in_Space.pdf .
- 25.Olise P. Human Resource Management. Fundamental Leadership Management Primary Health Care. Abuja, Ozege Publishers. 2011. p. 103.
- 26.Siegrist J. Chronic psychosocial stress at work and risk of depression: evidence from prospective studies. Eur Arch Psychiatry Clin Neurosci. 2008;258(5):115–9. doi: 10.1007/s00406-008-5024-0. [DOI] [PubMed] [Google Scholar]
- 27.Barth J, Schneider S, von K nel R. Lack of Social Support in the Etiology and the Prognosis of Coronary Heart Disease: A Systematic Review and Meta-Analysis. Psychosom Med. 2010;72(3):229–38. doi: 10.1097/PSY.0b013e3181d01611. [DOI] [PubMed] [Google Scholar]
- 28.Tsai CJ. Boredom at Work and Job Monotony: An Exploratory Case Study within the Catering Sector. Human Resource Development Quarterly. 2016;27(2):207–36. [Google Scholar]
- 29.Haukka E. Musculoskeletal disorders and psychosocial factors at work. Effects of a participatory ergonomics intervention in a cluster randomized controlled trial. Academic Dissertation presented to University of Helsinki. 2010. pp. 1–126.
- 30.Magnavita N, Heponiemi T, Gates D, et al. Violence towards health care workers in a Public Health Care Facility in Italy: a repeated cros-ssectional study. BMC Health Ser v Res. 2012;12(1):108. doi: 10.1186/1472-6963-12-108. [DOI] [PMC free article] [PubMed] [Google Scholar]