Abstract
In recent years, the Comprehensive Geriatric Assessment (CGA), which is used in gerontology to assess functioning in elderly individuals, has been said to be useful in geriatric oncology. Therefore, we examined whether items in the CGA were associated with survival time in elderly patients with non-Hodgkin lymphoma (NHL). We conducted the CGA for 93 patients aged ≥ 65 years who had undergone treatment for NHL retrospectively. The CGA includes activities of daily living, instrumental activities of daily living, mood, cognition, nutrition, and the Charlson comorbidity index. For each category, we divided subjects into a “good” group and a “poor” group. In regard to the Charlson comorbidity index, patients were divided into two groups using different cutoffs to divide the groups; the two groups were established according to the division with the largest significant difference in survival time. Multivariate analysis was then performed with the following prognostic factors affecting survival: all CGA items, NHL classification, stage, performance status, and doxorubicin use/non-use. We also performed similar analysis for 43 diffuse large B-cell lymphoma (DLBCL) patients who had undergone anthracycline treatment. Results are factors affecting survival in NHL cases included comorbidity score ≥ 6 (P < 0.0001), doxorubicin non-use (P = 0.005), and cognitive impairment (P = 0.0488). In cases of DLBCL, survival was affected by comorbidity score ≥ 5 (P = 0.0016). High comorbidity score was strongly associated with survival in both NHL and DLBCL.
Keywords: non-Hodgkin lymphoma, overall survival, comprehensive geriatric assessment, Charlson comorbidity index
INTRODUCTION
Due to the rapid aging of Japanese society following World War II, Japan now has one of the highest percentages of elderly citizens among developed countries. Consequently, according to the data of Ministry of Health, Labour, and Welfare of Japan; 69% of cancer patients and 80% of patients who die of cancer are aged ≥ 65 years. As elderly individuals’ lifespans grow longer, their mental and physical functions decline, often causing them to fall into a pathologic state known as geriatric syndrome. In addition to suffering from mental and physical impairment, many elderly people are socially and economically disenfranchised.1 Daily living, high medical expenses, and the absence of care typically raise barriers to cancer treatment. Thus, treatment of elderly individuals requires a comprehensive assessment of factors such as the background.2
The field of gerontology already employs the Comprehensive Geriatric Assessment (CGA), a multifaceted assessment of aspects such as activities of daily living (ADL),3 mood4 and cognition.5 The results of the CGA are used as a basis for performing therapy and rehabilitation, which are used to improve survival rates and physical functioning.6
The use of the CGA has also been attempted in the treatment of elderly cancer patients. The National Comprehensive Cancer Network guidelines, which are used worldwide, also recommend the use of the CGA as a tool for assessing benefits and the risk of adverse events in cancer treatment for elderly patients.2 In this study, we report on our retrospective assessment of patient characteristics, performance status (PS), and CGA items in 93 patients with incipient malignant lymphoma; as well as our analysis of malignant lymphoma classification, stage, treatment content, and chemotherapy dose intensity.
MATERIALS AND METHODS
Patients and surveillance design
Patients aged 65 years or older who were admitted for the first time to the Department of Medical Oncology, Hematology, and Infectious Diseases, Fukuoka University Hospital for the treatment of non-Hodgkin lymphoma (NHL) were consecutively enrolled in this study during the period of January 2004 and December 2008. Their background characteristics were collected and CGA was conducted by reviewing the medical records at the time of initial examination when they were hospitalized. Patient characteristics consisted of age, sex, histological classification, stage, PS, and international prognostic index (IPI).7 Items for the CGA consisted of ADL,3 instrumental activities of daily living (IADL),8 mood,4 cognition,5 nutrition,9 and comorbidities.10
CGA was performed using detailed daily review of medical records by physicians, nurses, and pharmacists. Assessment of ADL was based on the Barthel index3; patients who required at least one item of assistance with feeding, bathing, walking, dressing, toilet use, or grooming were deemed to be impaired in their ADL. In assessing IADL, we referred to the ability to manage one’s own medication and go shopping by oneself, which are items on the IADL scale8; patients who required at least one item of assistance in either of these were deemed to be impaired in their IADL. As for mood, although all patients naturally demonstrated some level of anxiety, those who were diagnosed as depressive or having depressive tendencies based on the Geriatric Depression Scale4 were considered to be impaired in their mood. In assessing cognition, patients were deemed to have cognitive impairment if described as such by their attending physician or a nurse. For patients in whom cognitive impairment was suspected, we administered the revised version of Hasegawa’s dementia scale.5 Nutrition was assessed based on the Mini Nutritional Assessment; patients with body mass index < 19 were deemed to suffer from undernutrition.9 Comorbidity was assessed using the Charlson comorbidity index.10
Comorbidities were scored as follows: myocardial infarction, congestive heart failure, peripheral vascular disease, cerebrovascular disease, dementia, chronic pulmonary disease, connective tissue disease, ulcer disease, mild liver disease, and diabetes were each scored as one point; hemiplegia, moderate or severe renal disease, diabetes with end organ damage, any tumor, leukemia, and lymphoma were each scored as two points; moderate or severe liver disease was scored as three points; and metastatic solid tumor and acquired immune deficiency syndrome were scored as six points. All individual scores were added together to yield a total comorbidity score. We also examined the relationship between dose intensity and prognosis and safety profiles in patients with diffuse large B-cell lymphoma (DLBCL), the most common type of lymphoma among our subjects, who had received a standard combination chemotherapy consisting of rituximab, cyclophosphamide (CPA), doxorubicin (ADR), vincristine (VCR), and prednisolone (R-CHOP) chemotherapy.11 We then analyzed these cases using patient characteristics, CGA, and dose intensity as variables.
Statistical analysis
We examined the association of CGA with using a simple and a multiple proportional hazard model. For the multivariate analysis, a variables selection was conducted by the stepwise method in order to determine the simplest model. For all cases of lymphoma, in addition to CGA items, we included PS, age, stage, lymphoma classification, and the use or non-use of doxorubicin as explanatory variables. For cases of DLBCL, in addition to CGA items, we included PS, age, IPI, and average relative dose index (ARDI).
Of the CGA items analyzed in the proportional hazards model, ADL, IADL, cognition, mood, and nutrition were divided into a “good” group and a “poor” group. In regard to the Charlson comorbidity index, patients were divided into two groups using different cutoffs to divide the groups (for example, 1–2 points vs ≥ 3 points, 1–3 points vs ≥ 4 points, etc.), and cut off point was determined using the proportional hazard analysis: the two groups were established according to the division that demonstrated the largest significant difference in survival time. As for PS, patients were divided into groups with relatively favorable (0–1) or poor statuses (2–4). Depending on age, patients were divided into an early-elderly group (65–74 years) and a late-elderly group (≥ 75 years). Depending on the treatment, patients were divided into the group that used doxorubicin (the key drug in lymphoma treatment) and the group that did not. Depending on the disease stage, patients were divided into an early-stage group (I–II) and an advanced-stage (III–IV). Depending on the classification, patients were divided into an “aggressive” group (moderate- or high-grade malignant lymphoma) and an “indolent” group (low-grade malignant lymphoma). As for IPI, patients were divided into two groups: a low and low-intermediate group and a high-intermediate and high group.
Next, we determined ARDI to examine the association between the intensity of R-CHOP chemotherapy and adverse events. The standard usages and doses of drugs in R-CHOP was as follows. For rituximab, 375 mg/m2 was infused intravenously the day before beginning CHOP. CPA, ADR, and VCR were each injected intravenously on day 1 in respective doses of 750 mg/m2, 50 mg/m2, and 1.4 mg/m2. Prednisolone was administered for five days beginning on day 1 at a dose of 100 mg/day. These latter four drugs were administered every three weeks. Rituximab rarely results in serious adverse events other than infusion reactions and has little effect on the treatment schedule; therefore, it was excluded from examinations of dose intensity. Prednisolone was also excluded. The dose intensity of CPA, ADR, and VCR were determined in terms of dosage per week (mg/m2/week), and the dosages actually administered were divided by the respective standard dosages to determine their respective relative dose intensities. The relative dose intensity of these three drugs was then averaged to determine ARDI. To examine the association of ARDI with survival time, we examined survival time in 5% increments starting at 100%. We then determined proportional hazards and used the ARDI with the largest significant difference as a cutoff point to divide ARDI into two groups. Survival curves were drawn by the Kaplan-Meier method.
Evaluation of adverse events
Chi-square tests were performed between each of the items in the CGA and ≥ grade 3 hematologic toxicity, as well as between CGA items and the manifestation of febrile neutropenia (FN). We similarly examined the development of constipation, stomatitis, and peripheral neuropathy, all of which are known to be frequent adverse events in CHOP chemotherapy.11
RESULTS
Patient characteristics
Ninety-nine elderly patients with NHL were enrolled in the study between January 2004 and December 2008. Since 6 patients were excluded because of being unable to obtain complete CGA data from their medical records, the present study were comprised of 93 patients whose characteristics were listed in Table 1. The median age was 77 (range, 65–90) years. Forty-three patients were male and 50 were female. Seventy-seven patients had aggressive lymphoma including 66 of DLBCL, while 16 patients had indolent lymphoma including 9 with follicular lymphoma and 5 of MALT lymphoma. A total of 91 patients received anti-lymphoma treatment including chemotherapy in 82, radiation alone in 5 and surgery alone in 4, while 2 patients underwent best supportive care. R-CHOP therapy was given in 55 patients and CHOP in 9 (Table 1).
Table 1. Baseline clinical features of 93 non-Hodgkin lymphoma patients.
| Characteristics | No. of patients (%) |
|---|---|
| Median
age 65-74 75-90 Sex (male/female) Classifying of NHL Indolent type Follicular lymphoma MALT lymphoma Lymphoplasmacytic lymphoma Nodal marginal zone lymphoma Aggressive type Diffuse large B-cell lymphoma Angioimmunoblastic T-cell lymphoma Peripheral T-cell lymphoma NK/T-cell lymphoma Mantle cell lymphoma Anaplastic large cell lymphoma Adult T-cell leukaemia/ lymphoma Burkitt lymphoma Ann-Arbor stage I-II III-IV Performance status 0-1 2-4 Treatment Chemotherapy R-CHOP CHOP Methotrexate R-COP Others Radiation Surgery Best supportive care Treatment of doxorubicin Including doxorubicin Without doxorubicin |
77 53 (57) 40 (43) 43/50 16 (17) 9 (10) 5 (5) 1 (1) 1 (1) 77 (83) 66 (71) 2 (2) 2 (2) 2 (2) 2 (2) 1 (1) 1 (1) 1 (1) 41 (44) 52 (56) 73 (78) 20 (22) 82 (88) 55 (59) 9 (10) 4 (4) 3 (3) 11 (12) 5 (5) 4 (4) 2 (2) 66 (71) 27 (29) |
NHL, non-Hodgkin lymphoma; MALT, extranodal marginal zone lymphoma of mucosa-associated lymphoid tissue type; R-CHOP, rituximab, cyclophosphamide, doxorubicin, vincristine, prednisolone; R-COP, rituximab, cyclophosphamide, vincristine, prednisolone
Since Charlson comorbidity index scores malignant lymphoma as 2 points, all patients had a comorbidity score of ≥ 2. A total of 52 patients (56%) had a score of 2, while nine patients had a score of ≥ 5. Cognitive impairment was deemed present in four patients, three of whom had undergone Hasegawa’s dementia scale and scored 27, 21, and 12 (Table 2).
Table 2. Comprehensive geriatric assessment of 93 non-Hodgkin lymphoma patients.
| Item | Group | No. (%) | Reference |
|---|---|---|---|
| Activities of daily living | good/poor | 67 (72%)/26 (28%) | Barthel index3 |
| Instrumental activities of daily living | good/poor | 64 (73%)/29 (27%) | Instrumental activities of daily livings (Lawton & Brody)8 |
| Mood | good/poor | 79 (85%)/14 (15%) | Geriatric depression scale4 |
| Cognition | good/poor | 89 (96%)/ 4 (4%) | The revised version of Hasegawa's dementia scale5 |
| Nutrition | good/poor | 55 (49%)/38 (51%) | Mini nutritional assessment9 |
| Comorbidity score | 2 | 52 (56%) | Charlson comorbidity index10 |
| 3 | 22 (23%) | ||
| 4 | 10 (12%) | ||
| 5 | 3 (3%) | ||
| 6 | 1 (1%) | ||
| 7 | 1 (1%) | ||
| 8 | 3 (3%) | ||
| 9 | 1 (1%) |
Comprehensive geriatric assessment and overall survival
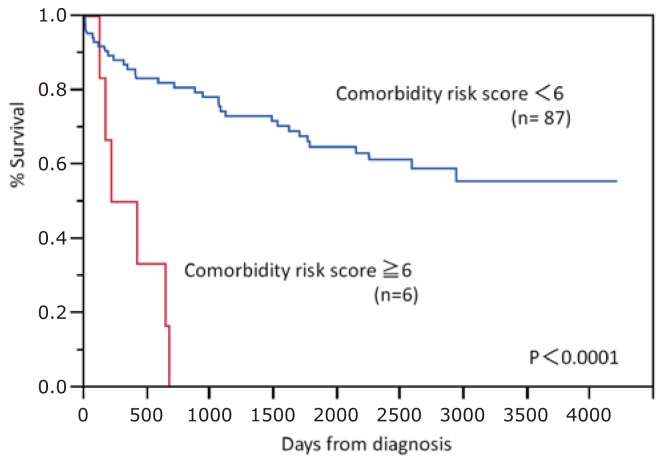
We also analyzed the relationship between Charlson comorbidity index and survival rates. Chi-square tests demonstrated the greatest significant difference between scores of 2–5 and ≥ 6 in NHL and between scores of 2–4 and ≥ 5 in cases of DLBCL. These respective points were used to divide patients into two groups for use as variables in multivariate analysis. In multivariate analysis of CGA and survival time among the 93 NHL patients, the largest significant difference was observed in the Charlson comorbidity index (P < 0.0001)(Table 3). The next largest significant differences observed were in doxorubicin use/non-use (P = 0.005) and cognition (P = 0.049). In regard to the Charlson comorbidity index which demonstrated the greatest significant difference, we drew survival curves for scores of ≥ 6 and < 6 (Fig. 1).
Table 3. Prognostic factors affecting survival by univariate and multivariate analysis of 93 non-Hodgkin lymphoma patients.
| Prognostic factor | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| p-value | OR (95% CI) | p-value | OR (95% CI) | |||
| Activities of daily living | 0.054 | 2.00 (0.99-3.86) | ||||
| Instrumental activities of daily living | 0.015 | 2.32 (1.18-4.43) | ||||
| Mood | 0.871 | 1.08 (0.37-2.54) | ||||
| Cognition | 0.119 | 2.96 (0.71-8.27) | 0.0488 | 4.28 (1.01-12.38) | ||
| Nutrition | 0.572 | 1.20 (0.63-2.28) | ||||
| Comorbidity score | 0.0005 | 7.59 (2.68-18.94) | < 0.0001 | 10.80 (3.69-28.37) | ||
| Age | 0.140 | 1.63 (0.85-3.10) | ||||
| Classifying of non-Hodgkin lymphoma | 0.450 | 1.42 (0.60-4.15) | ||||
| Stage | 0.049 | 1.93 (1.00-3.90) | ||||
| Performance status | 0.238 | 0.24 (0.23-1.36) | ||||
| Treatment of doxorubicin | 0.023 | 2.23 (1.12-4.27) | 0.0051 | 2.80 (1.38-5.49) | ||
OR, Odds’s ratio; CI, confidence interval
Fig. 1.
Overall survival curves of 93 non-Hodgkin lymphoma patients by Charlson comorbidity index. A clear difference was observed between the comorbidity scores of ≥ 6 and < 6.
For the 43 DLBCL patients who underwent R-CHOP chemotherapy, we analyzed the relationship between the ARDI of ADR/CPA/VCR and survival rate; we consequently found the greatest significant difference in ARDI ≥ 75% (P = 0.028). Thus, patients were divided into an ARDI ≥ 75% group and an ARDI < 75% group, which were included along with the variables analyzed for overall lymphoma. In multivariate analysis related to survival rates for these 43 patients, leaving only the Charlson comorbidity index (P = 0.0016) as a significant variable (Table 4). Only comorbidity score was selected as a result of the stepwise method in the multivariate analysis, and therefore the results of univariate and multivariate analysis for comorbidity score are consistent.
Table 4. Prognostic factors who received R-CHOP for 43 diffuse large B-cell lymphoma patients.
| Prognostic factor | Univariate | Multivariate | ||||
|---|---|---|---|---|---|---|
| p-value | OR (95% CI) | p-value | OR (95% CI) | |||
| Activities of daily living | 0.284 | 0.48 (0.07-1.72) | ||||
| Instrumental activities of daily living | 0.712 | 0.81 (0.23-2.34) | ||||
| Mood | 0.830 | 0.85 (0.13-3.06) | ||||
| Cognition | 0.277 | 5.11 x 10-9 (3.42-3.42) | ||||
| Nutrition | 0.802 | 1.14 (0.39-3.09) | ||||
| Comorbidity score | 0.0016 | 11.60 (2.80-45.32) | 0.0016 | 11.60 (2.80-45.32) | ||
| Age | 0.538 | 1.38 (0.48-3.81) | ||||
| Performance status | 0.090 | 0.24 (0.01-1.20) | ||||
| International prognostic index | 0.312 | 1.37 (0.60-4.55) | ||||
| Average relative dose intensity | 0.028 | 3.25 (1.13-11.65) | ||||
R-CHOP, rituximab, cyclophosphamide, doxorubicin, vincristine, prednisolone; OR, Odds’s ratio; CI, confidence interval
Comprehensive geriatric assessment and adverse events
Within the CGA, items associated with hematological toxicity were observed at a significantly higher frequency in patients with low ADL and in the development of anemia due to undernutrition. However, there were no risk factors related to leukocyte count, infection, or FN (Table 5). Also, there were no associations between CGA and the non-hematological toxicities of constipation, stomatitis, and peripheral neuropathy.
Table 5. Association between comprehensive geriatric assessment and hematological toxicity and infection in diffuse large B-cell lymphoma 43 patients.
| White blood cell | Absolute neutrophil count |
Hemoglobin | Platelet | Febrile neutropenia/Infection | |
|---|---|---|---|---|---|
| Activities of daily living | 1.0 | 1.0 | 0.045 | 1.0 | 0.092 |
| Instrumental activities of daily living | 1.0 | 1.0 | 0.278 | 0.312 | 0.728 |
| Mood | 1.0 | 1.0 | 0.174 | 0.571 | 0.393 |
| Cognition | 1.0 | 1.0 | 0.372 | 1.0 | 1.0 |
| Nutrition | 0.458 | 0.451 | 0.007 | 0.161 | 0.219 |
| Comorbidity score | 0.188 | 0.226 | 0.372 | 0.372 | 0.465 |
DISCUSSION
Japanese studies on lymphoma in elderly individuals have not produced data for examinations of indices other than PS. Although the present study is a retrospective study and therefore limited in terms of items examined, we were able to analyze the relationship between survival rates and CGA items.
In this study, we found that a Charlson comorbidity index score of ≥ 6 (P < 0.0001) was found to be a high risk factor for incipient NHL in individuals aged ≥ 65 years. The most common comorbidities in patients with scores ≥ 6 were metastatic solid tumors. Because malignant lymphomas are relatively easy to control with drug therapy and radiotherapy, it is understandable that metastatic solid cancers would be objects of focus as prognostic factors. But this fact that the Charlson comorbidity index score is a high risk factor for survival is very important for making decision of treatment.
General cancer treatment guidelines for elderly individuals are as follows.2 First, the patient’s remaining life expectancy is compared with the survival time that would be yielded by treatment. If treatment would be able to sufficiently prolong the patient’s remaining life expectancy, treatment is proactively performed; otherwise, palliative or supportive therapy is considered. Our analysis strongly indicated that patients with a high Charlson comorbidity index score have extremely poor prognosis. So treatment for such cases should not strive for standard therapy to maintain high ARDI, but rather should reduce dosages and discontinue doxorubicin (the key drug) with the goal of controlling the tumor. Moreover it is preferable we propose that such cases are discussed by cancer board, where multi-disciplinary cancer team meet together.12
From among the 93 NHL patients in this study, we abstracted 43 DLBCL patients who underwent R-CHOP chemotherapy. We analyzed for survival time not only CGA items, but also IPI and ARDI (which are prognostic factors for DLBCL); in univariate analysis, ARDI was significantly correlated with survival rates. However, in multivariate analysis, high comorbidity score emerged as a significant risk factor (P = 0.0016) as well as 93 NHL patients.
Studies on prognosis for malignant lymphoma have seldom considered the CGA. As retrospective analysis of 348 DLBCL patients in 2008 who underwent a CHOP-like regimen, Bosly et al.13 said ARDI, IPI, PS, and age as important prognostic factors, with particular emphasis of the importance of ARDI. In Japan, in 1999, Mori et al.14 have conducted prospective trials to determine optimal CHOP doses for elderly patients. In a prospective study in which patients were administered a 1/2 dose, 7/12 dose, 5/6 dose, or a standard dose, they reported that the optimal schedules for patients aged < 80 years and patients aged ≥ 80 years were 5/6 and 7/12 of the standard dose. Treatment was decided by patients’ age not CGA. In another study conducted by the same researchers with 57 elderly patients, patients aged 65–79 years and patients aged ≥ 80 years were administered 5/6 and 7/12, respectively, of the standard CHOP dose. The researchers reported respective three-year survival rates of 58% and 30%.15 These results thus indicate that elderly lymphoma patients who are at least healthy enough to participate in clinical trials demonstrate better outcomes with a higher ARDI in CHOP. These results show that ARDI is related to survival time.
As shown in Table 2, patients who Charlson comorbidity scores of ≥ 5 (which strongly affect prognosis) only accounted for approximately 10%. However, as Japanese society further ages, the number of patients with comorbidities will increase; therefore, it becomes more important to consider high comorbidity score’s patients for providing appropriate treatment. In an examination of CGA items and other prognostic factors in 154 DLBCL patients who had undergone R-CHOP chemotherapy, Wieringa et al.16 said Charlson comorbidity score ≥ 4 (P = 0.02) and IPI (P = 0.01) are prognostic factors; this report supports our results.
In addition to comorbidities, the use of doxorubicin also emerged as a factor favorably affecting survival times in the 93 malignant lymphoma patients in the present study (P = 0.005). In multivariate analysis of therapeutic outcomes for DLBCL and mantle cell lymphoma using CGA and the use/non-use of anthracycline-based treatment as variables, Marchesi et al. similarly found doxorubicin to be an independent factor contributing to improved survival rates. This finding supports the idea that doxorubicin is the key drug for aggressive lymphoma.17
Our study also suggested that cognitive impairment would affect survival in multivariate analysis (P = 0.0488). Raji et al. reported older patients who had cognitive impairment were associated with high mortality than those of no mental problems in patients with breast, colon, and prostate cancer.18 This report supports our results.
In regard to CGA and adverse events among DLBCL patients, patients with impaired ADL and patients with undernutrition demonstrated a significantly high frequency of ≥ grade 3 anemia (P = 0.045 and P = 0.007, respectively). In a prospective trial related to CGA and adverse events conducted among 500 patients with various cancers,19,20 not only low hemoglobin value, but also low leukocyte count and infection were noted significantly more frequently in patients with poor CGA outcomes. In this study, FN and infection yielded no differences in patients with poor CGA outcomes; this lack of difference may have been due to proper adjustment of anticancer drug dosages.
In the present study, the Charlson comorbidity index was found to be a significant prognostic factor in NHL. There have been almost no attempts in the past to assess functioning in elderly individuals, conduct a prospective study based on such an assessment, or to examine its association with prognosis like this. One possible reason is that no standard usage, dosage, or treatment has been established for malignant lymphoma among the elderly. Elderly individuals are frail compared to young individuals; therefore, they demonstrate greater diversity in host factors and require more individualized treatment. Consequently, stratification involves many factors, making prospective comparative studies difficult to organize. Tucci et al. have reported among unfit patients who are problem in CGA, their outcomes did not differ between curative treatment and palliative care.21 They suggests that the curability of DLBCL may not only depend on its biological characteristics, but also patient-related factors, which may be linked particularly to the parameters analyzed by CGA.
In this study, comorbidity score and cognition were associated with prognosis. As the number of elderly malignant lymphoma patients in Japan is expected to continue increasing, treatment guidelines for such patients need to be established.
ACKNOWLEDGMENTS
We thank project managers Y. Ito, N. Gushima, K. Nakata, E. Kumakawa, N. Ikoma, and S. Nagamori, and the medical doctors N. Kunami, K. Tsutsumi, T. Tanaka, A. Mogi, T. Goto, Y. Ikari, M. Masaki, Y. Nakashima, M. Ishizu, A. Shirahashi, E. Sato, Y. Kitai, T. Takata, A. Togawa, Y. Obata, M. Yoshimura, H. Katsuya, K. Ishitsuka, C. Kawai, T. Maeda and M. Fujita for valuable assistance in conducting the present study.
Footnotes
CONFLICT OF INTEREST STATEMENT: Yasushi Takamatsu received honoraria for writing promotional material for Janssen and Celgene. Yoshiko Naito, Hidenori Sasaki, Fumiaki Kiyomi, and Kazuo Tamura have no conflict of interest.
REFERENCES
- 1.Jeffrey BH, Joseph GO, Mary ET, Stephanie S, Kevin PH, et al.: Hazzard’s Geriatric Medicine and Gerontology. 6th ed, New York, McGraw Hill, pp.621-738, 2009 [Google Scholar]
- 2.Hurria A: Management of elderly patients with cancer. J Natl Compr Canc Netw 11(suppl): 698-701, 2013. 10.6004/jnccn.2013.0205 [DOI] [PubMed] [Google Scholar]
- 3.Mahoney FI, Barthel DW: Functional evaluation: The Barthel Index. Md State Med J 14: 61-65, 1965 [PubMed] [Google Scholar]
- 4.Yesavage JA, Brink TL, Rose TL, Lum O, Huang V, et al. : Development and validation of a geriatric depression screening scale: a preliminary report. J Psychiatr Res 17: 37-39, 1982-1983. 10.1016/0022-3956(82)90033-4 [DOI] [PubMed] [Google Scholar]
- 5.Jeong JW, Kim KW, Lee DY, Lee SB, Park JH, et al. : A normative study of the Revised Hasegawa Dementia Scale: comparison of demographic influences between the Revised Hasegawa Dementia Scale and the Mini-Mental Status Examination. Dement Geriatr Cogn Disord 24: 288-293, 2007. 10.1159/000107592 [DOI] [PubMed] [Google Scholar]
- 6.Applegate WB, Miller ST, Graney MJ, Elam JT, Burns R, et al. : A randomized, controlled trial of a geriatric assessment unit in a community rehabilitation hospital. N Engl J Med 322: 1572-1578, 1990. 10.1056/NEJM199005313222205 [DOI] [PubMed] [Google Scholar]
- 7.No authors listed. A predictive model for aggressive non-Hodgkin’s lymphoma. The International Non-Hodgkin’s Lymphoma Prognostic Factors Project. N Engl J Med 329: 987-994, 1993. 10.1056/NEJM199309303291402 [DOI] [PubMed] [Google Scholar]
- 8.Lawton MP, Brody EM: Assessment of older people: self-maintaining and instrumental activities of daily living. Gerontologist 9: 179-186, 1969. 10.1093/geront/9.3_Part_1.179 [DOI] [PubMed] [Google Scholar]
- 9.Guigoz Y, Lauque S, Vellas BJ: Identifying the elderly at risk for malnutrition. The Mini Nutritional Assessment. Clin Geriatr Med 18: 737-757, 2002. 10.1016/S0749-0690(02)00059-9 [DOI] [PubMed] [Google Scholar]
- 10.Charlson ME, Pompei P, Ales KL, MacKenzie CR: A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 40: 373-383, 1987. 10.1016/0021-9681(87)90171-8 [DOI] [PubMed] [Google Scholar]
- 11.Coiffier B, Lepage E, Briere J, Herbrecht R, Tilly H, et al. : CHOP chemotherapy plus rituximab compared with CHOP alone in elderly patients with diffuse large-B-cell lymphoma. N Engl J Med 346: 235-242, 2002. 10.1056/NEJMoa011795 [DOI] [PubMed] [Google Scholar]
- 12.Blazeby JM, Wilson L, Metcalfe C, Nicklin J, English R, et al. : Analysis of clinical decision-making in multi-disciplinary cancer teams. Ann Oncol 17: 457-460, 2006. 10.1093/annonc/mdj102 [DOI] [PubMed] [Google Scholar]
- 13.Bosly A, Bron D, Van Hoof A, De Bock R, Berrneman Z, et al. : Achievement of optimal average relative dose intensity and correlation with survival in diffuse large B-cell lymphoma patients treated with CHOP. Ann Hematol 87: 277-283, 2008. 10.1007/s00277-007-0399-y [DOI] [PubMed] [Google Scholar]
- 14.Mori M, Murai Y, Suzuki K, Nonaka Y, Sato H, et al. : Study of optimal CHOP dose ranges for elderly patients with non-Hodgkin’s lymphoma. Rinsho Ketsueki 40: 199-204, 1999. [in Japanese] [PubMed] [Google Scholar]
- 15.Mori M, Niitsu N, Takagi T, Tomiyama J, Matsue T, et al. : Reduced-dose chop therapy for elderly patients with non-Hodgkin’s lymphoma. Leuk Lymphoma 41: 359-366, 2001. 10.3109/10428190109057991 [DOI] [PubMed] [Google Scholar]
- 16.Wieringa A, Boslooper K, Hoogendoorn M, Joosten P, Beerden T, et al. : Comorbidity is an independent prognostic factor in patients with advanced-stage diffuse large B-cell lymphoma treated with R-CHOP: a population-based cohort study. Br J Haematol 165: 489-496, 2014. 10.1111/bjh.12765 [DOI] [PubMed] [Google Scholar]
- 17.Marchesi F, Cenfra N, Altomare L, Dessanti ML, Mecarocci S, et al. : A retrospective study on 73 elderly patients (≥ 75 years) with aggressive B-cell non Hodgkin lymphoma: clinical significance of treatment intensity and comprehensive geriatric assessment. J Geriatr Oncol 4: 242-248, 2013. 10.1016/j.jgo.2013.04.003 [DOI] [PubMed] [Google Scholar]
- 18.Raji MA, Kuo YF, Freeman JL, Goodwin JS: Effect of a dementia diagnosis on survival of older patients after a diagnosis of breast, colon, or prostate cancer: implications for cancer care. Arch Intern Med 168: 2033-2040, 2008. 10.1001/archinte.168.18.2033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Hurria A, Togawa K, Mohile SG, Owusu C, Klepin HD, et al. : Predicting chemotherapy toxicity in older adults with cancer: A prospective multicenter study. J Clin Oncol 29: 3457-3465, 2011. 10.1200/JCO.2011.34.7625 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Extermann M, Boler I, Reich RR, Lyman GH, Brown RH, et al. : Predicting the risk of chemotherapy toxicity in older patients: the Chemotherapy Risk Assessment Scale for High-Age Patients (CRASH) score. Cancer 118: 3377-3386, 2012. 10.1002/cncr.26646 [DOI] [PubMed] [Google Scholar]
- 21.Tucci A, Ferrari S, Bottelli C, Borlenghi E, Drera M, et al. : A comprehensive geriatric assessment is more effective than clinical judgment to identify elderly diffuse large cell lymphoma patients who benefit from aggressive therapy. Cancer 115: 4547-4553, 2009. 10.1002/cncr.24490 [DOI] [PubMed] [Google Scholar]