Abstract
Status dystonicus, also known as the dystonic storm or dystonic crisis, is rare but may prove fatal due to respiratory and bulbar complications. In adults, the condition is rare and possibly under-reported. The lack of awareness of this condition among emergency and acute physicians may lead to an incorrect or delayed diagnosis, which should be avoided. We report a case of a 23-year-old man with athetoid cerebral palsy who presented to a district general hospital with uncontrolled dystonic movements, which were diagnosed as status dystonicus. This was successfully treated with intravenous clonidine, with full recovery returning to baseline functional state.
Keywords: epilepsy and seizures, movement disorders (other than parkinsons)
Background
Status dystonicus is a rare and potentially fatal condition,1 in which patients develop generalised dystonia and rigidity. In severe cases, this can follow the involvement of bulbar and respiratory muscles, rhabdomyolysis and even death. We describe below a case of a young 23-year-old male patient who presented to the acute medical unit at a district general hospital with status dystonicus. This case demonstrates the importance of identifying and treating status dystonicus in a timely fashion in order to prevent a potentially fatal outcome.
Case presentation
A 23-year-old man was admitted to the acute medical unit at a district general hospital with uncontrollable continuous dystonic movements of the arms and legs. His medical history included stable athetoid cerebral palsy, epilepsy and cholesteatoma. His epilepsy was well controlled on lamotrigine, and he was seizure free for the last 5 years. He was fed through percutaneous enteral gastrostomy and was normally a wheelchair user. He was able to smile and communicate with the simple yes and no responses, vocalise and obey some commands. His baseline Glasgow Coma Scale (GCS) was 12 (E4M6V2). The movements had been noted by the family for the last few weeks to months but these were usually self-limiting.
The neurological examination revealed continual violent choreoathetoid movements of the neck, arms, trunk and legs. These movements were a combination of dystonia, choreoathetosis and these were not stereotyped. There was marked dystonic posturing of the neck with marked retrocollis and laterocollis. With the allowance of these movements, no focal weakness was elicited. His GCS at best was 9 (E3M5V1).
Investigations
He underwent an emergency CT scan, followed by MRI scan of the brain, both showed generalised cortico-subcortical atrophy and ventricular system dilatation with no midline shifts. There was no space-occupying lesion or focal signal change within the brain parenchyma (figure 1).
Figure 1.

Axial T2 fluid-attenuated inversion recovery MRI of the patient at the level of the centrum semiovale, showing global brain atrophy, more prominent at the frontoparietal regions, with compensatory hydrocephalus.
His blood tests showed a slightly elevated creatine kinase levels of 477 IU/L (normal range 40–320 IU/L), with the creatinine level of 49 μmol/L (normal range 64–104 μmol/L) and elevated urea of 11.3 mmol/L (normal range 2.5–7.8 mmol/L). The rest of his blood tests were unremarkable with a normal neutrophil count and only modest elevated C-reactive protein (CRP) of 14.70 mg/L (normal range 0–5 mg/L).
He underwent a lumbar puncture with some difficulty in view of his movements which was essentially unremarkable. The cerebrospinal fluid (CSF) protein level was 0.26 g/L (normal range 0.15–0.40 g/L), with CSF glucose of 3.4 mmol/L (normal range 2.22–3.89 mmol/L). There were no white blood cells in CSF (normal range 0–5/mm3) and no organisms seen on gram stain. There was no growth on culture and viral PCR for enterovirus, herpes simplex and varicella zoster virus was also negative.
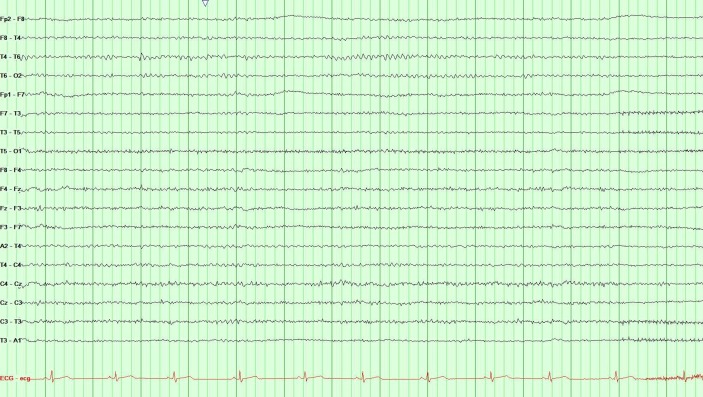
He also underwent a portable electroencephalogram (EEG) which did not show generalised or focal epileptiform discharges, during the episodes of dystonic movements (figure 2).
Figure 2.
Portable electroencephalogram trace of the patient, performed at the intensive care unit showing diffuse low-voltage beta rhythm with well-organised background activity.
Differential diagnosis
Toxins/poisoning/ medications (lamotrigine)/unknown ingestions.
Status epilepticus.
Meningoencephalitis.
Treatment
He was initially treated with intravenous cefotaxime and acyclovir to cover meningoencephalitis, which was discontinued once the lumbar puncture results were reported as normal. He was intermittently given benzodiazepines in the form of buccal midazolam and intravenous lorazepam with some improvement in his symptoms. Because of his medical history of epilepsy, his lamotrigine dose was increased, and clobazam and gabapentin were introduced, in case the clinical picture represented an increased frequency of epileptic seizures.
There was no real improvement in his condition and an urgent neurology consultation referral was requested. As the hospital did not have a neurology cover on every day of the week, there was a delay, during which the patient was kept on the above medications. After review by the neurology consultant, a correct diagnosis of status dystonicus was made and the patient was sent to the intensive care unit for an intravenous clonidine infusion. He responded very well to this, and the intravenous clonidine was later switched to a parenteral dose, which was weaned off prior to discharge.
Outcome and follow-up
After 15 days of admission, he was discharged with outpatient follow-up in the community. On his future follow-up appointments, he had returned to his baseline state of athetoid cerebral palsy.
Discussion
Status dystonicus, also known as the dystonic storm or dystonic crisis, is a life-threatening movement disorder emergency.1 In adults, it is less known and possibly under-reported, as 60% of the affected patients are between ages 5 years and 16 years, with a male preponderance.2 It can prove to be fatal because of severe episodes of generalised dystonic spasms and, therefore, requires urgent hospital admission.3 In one of the larger studies done so far, it was found that 69% of the dystonias were continuous, that is, tonic, whereas in the rest these were irregular, that is, phasic.2 The underlying reason for the dystonic crisis is not fully understood, although various mechanisms have been hypothesised such as increased pallidal output, dopaminergic blockage, increased serotonin release, etc.4
Dystonic storm needs to be differentiated from similarly presenting conditions such as neuroleptic malignant syndrome, serotonin syndrome, malignant hyperthermia, intrathecal baclofen withdrawal, epilepsy and acute dystonic reactions.2 5 Diagnosing dystonic storm is sometimes challenging for emergency and acute physicians and can be mistaken for other conditions, as it happened in our case. Therefore, recognition of signs and symptoms is important.
Clinical features of status dystonicus include increasing frequent dystonias along with tachypnoea, tachycardia and sweating. The severe muscular spasms may also result in fever, rhabdomyolysis and renal failure. Complications including autonomic bulbar dysfunction, dysphagia and respiratory failure may follow requiring ventilatory support.1 2 In about two-thirds of the cases, a triggering factor, such as medication adjustment, infection, trauma, etc, can be identified, while the rest of the cases are unprovoked.5 6 With the increasing use of deep brain stimulation (DBS) for status dystonicus, DBS failure is becoming an increasingly frequent cause for status dystonicus.7
As mentioned, in most cases, there is usually a trigger initiating the symptoms. Therefore, the first step should be the identification and removal of the trigger. Supportive measures should be the first-line of treatment, especially in milder cases. Rhabdomyolysis requires intravenous fluids, urine alkalinisation and dialysis in severe cases.8
If the supportive measures fail or the muscular spasms are severe and troublesome, sedation and muscle relaxation would be successful in most cases resulting in prompt resolution of the dystonic spasms.1 Benzodiazepines and opiates are usually used for this purpose; however, a recently published case series has demonstrated effectiveness and safety of clonidine in non-intensive care settings.9 10 It has proven to be very effective in achieving control of dystonias without a respiratory depressant effect. Also, clonidine can be administered via any route, that is, oral, intravenous or enteral. This is definitely promising but needs more evidence. Mechanical ventilation is not always required, except in severe cases or when there is a respiratory compromise.6
Although invasive, DBS has proven to be very effective in terminating chronic dystonic spasms.11 12 This has led to the suggestion that DBS could potentially be used as a first-line treatment for treating status dystonicus in future; however, many do not share this view.13 Among other invasive options, intrathecal baclofen has been successfully used in the recent past,2 14 but due to failure in some cases,15 16 it is generally considered to be inferior to DBS.
Patient’s perspective.
We were privileged to receive this letter from the patient’s mother with consent to share.
‘The GP came out to see our son, most of what he said is a blur I remember the word ‘Sepsis’, I was filled with dread as I watched my son in the ambulance in a vicious spasm and felt helpless. The whole family thought it was his final illness, and we were heart broken. We watched the uncontrollable spasms hour by hour, he needed help and fast! Later that day, a neurologist popped by and said ‘I know what this is and how to treat him’ I wanted to jump up and kiss him! ‘Its status dystonicus’, within an hour he was taken to the ICU and began the recommended intravenous treatment. We watched and waited as our son slowly began to recover, each twitch sent us into panic but every smile he slowly gave us, gave us hope, it meant our beautiful young man was coming back to us.
With heartfelt gratitude and thanks to the consultants, doctors and ICU staff’.
Learning points.
Status dystonicus is a rare neurological disorder that can affect patients with athetoid cerebral palsy or may be provoked by trauma or withdrawal of medication, infection, deep brain stimulation failure, etc.
Complications include bulbar and ventilatory failure, rhabdomyolysis and renal failure, resulting in morbidity and mortality.
Clonidine is an effective and safe way of achieving complete resolution of status dystonicus.
Footnotes
Contributors: MS contributed to the concept and supervision. MFA and EA contributed to the collection of data and revision and editing. MFA, EA and ANB contributed to the literature search and writing the manuscript.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Competing interests: None declared.
Patient consent: Next of kin consent obtained.
Provenance and peer review: Not commissioned; externally peer reviewed.
References
- 1.Allen NM, Lin JP, Lynch T, et al. Status dystonicus: a practice guide. Dev Med Child Neurol 2014;56:105–12. 10.1111/dmcn.12339 [DOI] [PubMed] [Google Scholar]
- 2.Fasano A, Ricciardi L, Bentivoglio AR, et al. Status dystonicus: predictors of outcome and progression patterns of underlying disease. Mov Disord 2012;27:783–8. 10.1002/mds.24981 [DOI] [PubMed] [Google Scholar]
- 3.Teive HA, Munhoz RP, Souza MM, et al. Status Dystonicus: study of five cases. Arq Neuropsiquiatr 2005;63:26–9. 10.1590/S0004-282X2005000100005 [DOI] [PubMed] [Google Scholar]
- 4.Franzini A, Cordella R, Rizzi M, et al. Deep brain stimulation in critical care conditions. J Neural Transm 2014;121:391–8. 10.1007/s00702-013-1122-x [DOI] [PubMed] [Google Scholar]
- 5.Grosso S, Verrotti A, Messina M, et al. Management of status dystonicus in children. Cases report and review. Eur J Paediatr Neurol 2012;16:390–5. 10.1016/j.ejpn.2011.12.007 [DOI] [PubMed] [Google Scholar]
- 6.Manji H, Howard RS, Miller DH, et al. Status dystonicus: the syndrome and its management. Brain 1998;121:243–52. 10.1093/brain/121.2.243 [DOI] [PubMed] [Google Scholar]
- 7.Rohani M, Munhoz RP, Shahidi G, et al. Fatal status dystonicus in tardive dystonia due to depletion of deep brain stimulation’s pulse generator. Brain Stimul 2017;10:160–1. 10.1016/j.brs.2016.10.006 [DOI] [PubMed] [Google Scholar]
- 8.Nirenberg MJ, Ford B, Storm D. Movement disorder emergencies: diagnosis and treatment. 2nd edn New York, NY: Springer, Human Press, 2013:125–35. [Google Scholar]
- 9.Babiker MOE. Managing status dystonicus outside the intensive care setting: time to think clonidine? Eur J Paediatr Neurol 2017;21:801–2. 10.1016/j.ejpn.2017.08.008 [DOI] [PubMed] [Google Scholar]
- 10.Nakou V, Williamson K, Arichi T, et al. Safety and efficacy of high-dose enteral, intravenous, and transdermal clonidine for the acute management of severe intractable childhood dystonia and status dystonicus: an illustrative case-series. European Journal of Paediatric Neurology 2017;21:823–32. 10.1016/j.ejpn.2017.07.007 [DOI] [PubMed] [Google Scholar]
- 11.Aydin S, Abuzayed B, Uysal S, et al. Pallidal deep brain stimulation in a 5-year-old child with dystonic storm: case report. Turk Neurosurg 2013;23:125–8. 10.5137/1019-5149.JTN.4579-11.0 [DOI] [PubMed] [Google Scholar]
- 12.Elkay M, Silver K, Penn RD, et al. Dystonic storm due to Batten’s disease treated with pallidotomy and deep brain stimulation. Mov Disord 2009;24:1048–53. 10.1002/mds.22515 [DOI] [PubMed] [Google Scholar]
- 13.Mishra D, Singhal S, Juneja M. Status dystonicus a rare complication of dystonia. Indian Pediatr 2010;47:883–5. 10.1007/s13312-010-0138-7 [DOI] [PubMed] [Google Scholar]
- 14.Muirhead W, Jalloh I, Vloeberghs M. Status dystonicus resembling the intrathecal baclofen withdrawal syndrome: a case report and review of the literature. J Med Case Rep 2010;4:294 10.1186/1752-1947-4-294 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Kyriagis M, Grattan-Smith P, Scheinberg A, et al. Status dystonicus and Hallervorden-Spatz disease: treatment with intrathecal baclofen and pallidotomy. J Paediatr Child Health 2004;40:322–5. 10.1111/j.1440-1754.2004.00374.x [DOI] [PubMed] [Google Scholar]
- 16.Dalvi A, Fahn S, Ford B. Intrathecal baclofen in the treatment of dystonic storm. Mov Disord 1998;13:611–2. 10.1002/mds.870130344 [DOI] [PubMed] [Google Scholar]