Abstract
The study was conducted to ascertain whether the quantification of circulating cell-free DNA (cfDNA) in serum has value as a diagnostic or for monitoring the progression of non-small cell lung cancer (NSCLC). The serum/plasma cfDNA concentration was quantified by absolute qPCR of long interspersed nuclear element-1 (LINE1) in 60 NSCLC patients and 68 controls in good health. Receiver operating characteristic (ROC) curve analysis was performed to determine the diagnostic utility and cut-off levels of cfDNA, CEA, and CYFRA21-1 in NSCLC patients. Correlations between cfDNA and age, sex, tumour stage and progression-free survival (PFS) were analysed. A follow-up study was conducted on 4 NSCLC patients, and serum cfDNA, CEA, and CYFRA21-1 were quantified throughout disease progression. Serum cfDNA levels were significantly higher in NSCLC patients than those in normal controls. Elevated serum cfDNA concentration was also significantly associated with advanced tumour stage. Serum cfDNA had a ROC area under the curve comparable to that of CEA and CYFRA21-1 for the diagnosis of NSCLC, and the combined cfDNA/CEA/CYFRA21-1 indicator had the highest diagnostic efficiency. Moreover, increased serum cfDNA levels were strongly correlated with tumour progression and poor PFS. This study preliminarily confirmed that cfDNA can monitor disease progression in NSCLC patients, and the lead time was 1–7 months compared with clinical medical imaging. Serum cfDNA may be useful in monitoring NSCLC progression, suggesting that the non-invasive quantification of serum cfDNA by LINE1 qPCR is a viable option for predicting progression and disease severity when repeated invasive tissue biopsy is not possible.
Keywords: circulating cell-free DNA, serum, non-small cell lung cancer, progression
Introduction
In many countries, the majority of cancer-related deaths occur in people with lung cancer (1). Non-small cell lung cancer (NSCLC) is the most prominent form of lung cancer, accounting for ~85% of cases (2). More than half of NSCLC patients are diagnosed with advanced metastatic disease, and have a poor prognosis (3). Identifying non-invasive and convenient biomarkers relevant to diagnosis and prognosis may be conducive to improving the clinical outcome of NSCLC patients.
Circulating cell-free DNA (cfDNA) is released into circulation by various pathological and normal physiological mechanisms during the turnover of apoptotic and necrotic cells (4). cfDNA in peripheral blood can be obtained via ‘liquid biopsy’, and quantification of cfDNA can be combined with representative tumour information in cancer patients (5). Thus, the potential significance of cfDNA in plasma or serum as a diagnostic or prognostic indicator or for monitoring disease status has attracted increasing attention. In patients suffering from cancer, higher cfDNA levels were shown to be significantly correlated with poorer outcome (6). Some studies have reported that the quantification of cfDNA can be used as an effective biomarker to discriminate patients with NSCLC from healthy individuals (7–10). Since there is a close relationship between the peripheral blood and lung cancer cells, cfDNA quantification could be exploited for future diagnostic applications in lung cancer (11). However, as various pre-analytical factors related to blood sampling and processing can affect cfDNA concentrations, the optimal conditions for processing, cryopreserving and storing cfDNA must be established before the detection of cfDNA concentration can be applied clinically (12–15). In addition, cfDNA levels in serum and their usefulness in predicting cancer metastases and patient outcome have not been established.
This study was initially performed to assess the value of cfDNA in serum samples as a diagnostic marker and predictor of metastasis and poor prognosis in NSCLC. Furthermore, we aimed to establish optimal conditions for processing, cryopreserving and storing cfDNA, and to develop a standard protocol for the quantification of circulating cfDNA by absolute qPCR of long interspersed nuclear element-1 (LINE1). The results lay the foundation for the development of serum cfDNA as a new class of cancer biomarkers in liquid biopsies.
Materials and methods
Sample collection and processing
Serum samples from 60 patients with histologically confirmed NSCLC and 68 healthy controls, were collected at the Shanghai Sixth People's Hospital East Campus between October 2014 and June 2016. The Ethics Committee of Shanghai Sixth People's Hospital East Affiliated to Shanghai University of Medicine & Health Sciences (Shanghai, China) approved this study. The NSCLC patient group consisted of 34 patients with primary lung cancer and 26 patients with recurrent lung cancer. The staging of all 60 NSCLC patients was performed according to the tumour node metastasis (TNM) classification of malignant tumours, and peripheral blood was collected from these patients for cfDNA extraction. Four patients underwent multiple blood collections over time to determine whether the levels of cfDNA, CEA and CYFRA21-1 correlate with disease progression. In NSCLC patients, progressive disease is defined as an increase in target lesion size of at least 20% or the appearance of new lesions (16). All participants provided written informed consent. Peripheral blood was collected from patients in separate gel pro-coagulation vacuum tubes and EDTA vacutainer tubes (BD Biosciences, Franklin Lakes, NJ, USA), and serum and plasma were then separated by centrifugation at 1,200 × g for 10 min at room temperature, transferred to new tubes and centrifuged at 16,000 × g for 10 min at 4°C to remove cell debris. Plasma and serum were stored at −80°C prior to DNA extraction. To determine the optimal sample preparation and storage conditions for cfDNA quantification, venous blood samples from 4 healthy volunteers (2 females and 2 males; 26–48 years) were simultaneously collected for the preparation of serum samples. Serum was separated and then stored at room temperature (25°C) for 2, 6, or 10 h; at 4°C for 24 h; at −25°C for 1 month; or at −80°C for 1, 3, or 6 months.
cfDNA extraction and fragment analysis
Circulating DNA was separated from 1 ml serum and plasma samples with the PME free-circulating DNA extraction kit (Analytik Jena AG, Jena, Germany), according to the manufacturer's instructions for up to 1-ml extractions with the lysis solution SE/binding solution SBS mechanism. The process consisted of several steps as follows: i) capturing cfDNA in the polymer by mixing serum/plasma with 30 µl of VCR-1 and 150 µl of VCR-2, followed by centrifugation at 18,500 × g for 3 min at room temperature; ii) washing the polymer/DNA complex with 1 ml of ddH2O; iii) adding 400 µl of lysis solution SE to dissolve the pellet; iv) adding 50 µl of PK and incubating the samples for 15 min at 70°C; v) adding 400 µl of binding solution SBS and transferring the samples to spin filters; vi) washing the samples by adding 500 µl of washing solution GS and 650 µl of washing solution BS, followed by centrifugation at 13,500 × g for 1 min at room temperature; and vii) eluting cfDNA in 50 µl of water and storing the cfDNA at −80°C until further analysis. The presence of cfDNA and its fragment size distribution were evaluated by using the Agilent High Sensitivity DNA kit (Agilent Technologies, Inc., Santa Clara, CA, USA) on the 2100 Bioanalyzer.
cfDNA quantification by LINE1 qPCR
Genomic LINE1 sequences are distributed over all chromosomes; a short fragment (97 bp) of LINE1 was amplified and quantified by absolute qPCR quantification, using the standard curve method to indicate the total amount of serum and plasma cfDNA (17). LINE1 primer sequences were as follows: forward, 5′-TGGCACATATACACCATGGAA-3′; and reverse, 5′-TGAGAATGATGGTTTCCAATTTC-3′. The housekeeping gene β-actin was amplified with forward primer 5′-CCACACTGTGCCCATCTACG-3′ and reverse primer 5′-AGGATCTTCATGAGGTAGTCAGTCAG-3′, producing products of 99 bp. The reaction mixture for qPCR included 10 µl of SYBR® Premix Ex Taq II (Tli RNaseH Plus; Takara Biotechnology Co., Ltd., Dalian, China), 2 µl of cfDNA template, 0.4 mM primer, 0.4 µl of ROX II and 6 µl of double-distilled water in a final reaction volume of 20 µl. The qPCR was performed with an Applied Biosystems 7500 real-time PCR system (ABI; Thermo Fisher Scientific, Inc., Waltham, MA, USA), and was conducted by using the following protocol: 95°C for 8 min, followed by 40 cycles of 95°C for 5 sec and 60°C for 34 sec. A standard curve generated by serial dilution (from 1.0–10,000 ng/ml) of the LINE1-pCEP plasmid was used to determine the absolute equivalent amount of cfDNA in each sample. Melting curve analysis was conducted to confirm the amplification of a single peak. Each assay was performed in triplicate.
Reference values of serum cfDNA, CEA and CYFRA21-1
The levels of serum CEA and CYFRA21-1 were detected with a CEA and Cyfra21-1 test kit (Roche Diagnostics, Shanghai, China) by Cobas e601 Analyzer. The normal range was <4.7 ng/ml for CEA and <3.3 ng/ml for CYFRA21-1. A receiver operating characteristic (ROC) curve was created to quantify the diagnostic potential of serum cfDNA, CEA and CYFRA21-1. Youden's index (YI = sensitivity + specificity−1) was used to select cut-off values. The area under the ROC curve (AUC) was used to measure the discriminatory power of the test.
Statistical analysis
SPSS Statistics 19.0 (IBM Corp., Armonk, NY, USA) and MedCalc statistical software were used to conduct the statistical analyses. Figures were generated by using GraphPad Prism 6.0 software (GraphPad Software, Inc., La Jolla, CA, USA). The Mann-Whitney U test and Kruskal-Wallis H test were applied to compare serum cfDNA concentrations between groups. Dunn's post hoc tests were carried out on each pair of groups following Kruskal-Wallis test. The diagnostic values of cfDNA, CEA and CYFRA21-1 for NSCLC were assessed by using ROC curves. A univariate Cox regression model was used to analyse survival data for progression-free survival (PFS). The Kaplan-Meier method was used to estimate the PFS, which was evaluated by the log-rank test. Results were considered significant at two-tailed P<0.05.
Results
Comparison of serum and plasma cfDNA
To compare cfDNA concentrations between plasma and serum, we extracted cfDNA from 1 ml each of serum and plasma from the same donor, and quantified the amount of cfDNA by LINE1 qPCR. LINE1 is a transposable element belonging to the group of LINEs found in all mammalian DNA, comprising ~17% of the human genome. cfDNA concentrations were ~1-to 8-fold higher in serum samples than those in plasma samples (Fig. 1A). By fragment analysis, we observed an enrichment of plasma cfDNA fragments at 166 bp and 350 bp in NSCLC patients (Fig. 1B; upper plot); in serum cfDNA, there were multiple additional peaks within the range of 580-3,200 bp (Fig. 1B; lower plot), showing that the fragment distribution of cfDNA is more complex in serum than that in plasma.
Figure 1.
Effects of different sample preparation and incubation conditions on cfDNA yield. (A) Assessment of cfDNA yield in matched serum and plasma samples by LINE1 qPCR. (B) Fragment size bias of plasma cfDNA (top) and serum cfDNA (bottom). Comparison of (C) different storage temperatures and (D) times on serum cfDNA yield. *P<0.05 indicates statistical significance. cfDNA, cell-free DNA; LINE1, long interspersed nuclear element-1.
Effects of different storage conditions on serum cfDNA yield
Strict standardization of blood collection and serum preparation methods is mandatory, before serum cfDNA concentration can be used as a potential marker of clinical disorders. The time and temperature of blood storage after centrifugation significantly impacted the serum cfDNA concentration (Fig. 1C and D). Compared with the cfDNA concentration in serum prepared immediately after venepuncture (0 h at room temperature), the cfDNA concentrations in serum decreased after storage at room temperature for 2 or 10 h. However, the changes in cfDNA concentration in serum after storage at 4°C for 24 h, −25°C for 1 month, or −80°C for 1, 3, or 6 months were not significant. Based on these findings, serum samples from NSCLC patients or normal controls were frozen at −80°C immediately after collection.
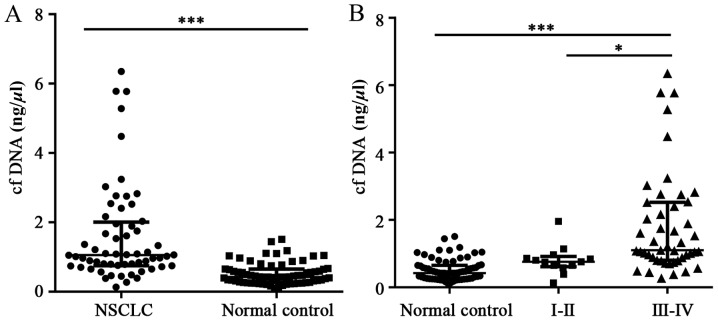
Serum cfDNA concentration in NSCLC patients with different clinical characteristics
To determine whether cfDNA concentration correlates with NSCLC status or any other clinical parameters, we quantified cfDNA in serum specimens from 60 NSCLC patients and 68 normal controls in good health by LINE1 qPCR. Analysis of cfDNA in different subgroups of NSCLC patients indicated that serum cfDNA is independent of sex and age: there was no significant difference (P>0.05) in serum cfDNA concentration between NSCLC patients aged 39–60 years or 61–85 years, or between NSCLC patients of different sex (35 males and 25 females) (Table I). When patients were stratified by NSCLC status, the results showed that the cfDNA concentration was significantly higher in NSCLC patients [1.06 (0.75–2.01) ng/µl] than that in normal controls [0.42 (0.27–0.65) ng/µl] (Fig. 2A). NSCLC patients with more advanced disease (stage III–IV) had considerably higher cfDNA concentrations than those in either normal controls or patients with stage I–II disease (Fig. 2B). In line with the finding that patients with stage III–IV disease have higher cfDNA levels; NSCLC patients with lymph node metastasis and distant metastases also had significantly higher cfDNA levels than patients without metastasis (Table I).
Table I.
The clinical characteristics of 60 NSCLC patients.
| Clinical characteristics | No. | cfDNA (ng/µl) median (IQR 25–75) | P-value |
|---|---|---|---|
| All | 60 | 1.055 (0.751–2.011) | |
| Age (years) | |||
| 39–60 | 21 | 1.061 (0.752–1.923) | 0.859 |
| 61–85 | 39 | 1.020 (0.748–2.164) | |
| Sex | |||
| Male | 35 | 1.092 (0.792–2.538) | 0.132 |
| Female | 25 | 1.012 (0.678–1.271) | |
| Tumour stage (TNM) | |||
| I–II | 13 | 0.757 (0.615–0.914) | 0.0032 |
| III–IV | 47 | 1.100 (0.801–2.523) | |
| N0 | 26 | 0.825 (0.634–1.040) | 0.0002 |
| N1-N3 | 34 | 1.449 (0.100–2.756) | |
| M0 | 20 | 0.825 (0.653–1.122) | 0.0109 |
| M1 | 40 | 1.156 (0.822–2.535) |
NSCLC, non-small cell lung cancer; cfDNA, cell-free DNA; TNM, tumor node metastasis.
Figure 2.
Serum cfDNA concentration in NSCLC patients and normal controls. (A) Serum cfDNA concentration in 60 NSCLC patients and 27 normal controls as determined by LINE1 qPCR. (B) Comparison of serum cfDNA concentrations between NSCLC patients at different tumour stages and normal controls. *P<0.05 and ***P<0.001 indicate statistical significance. cfDNA, cell-free DNA; NSCLC, non-small cell lung cancer; LINE1, long interspersed nuclear element-1.
Diagnostic utility of serum cfDNA in NSCLC patients
ROC curves were generated to distinguish NSCLC patients from normal healthy controls based on serum cfDNA, CEA or CYFRA21-1 levels (Fig. 3). CEA and CYFRA21-1 are established biomarkers for the diagnosis of NSCLC (18). The AUC of cfDNA for distinguishing NSCLC patients from normal controls was 0.848 (95% CI: 0.774–0.905), which was comparable to that of CEA [0.829 (95% CI: 0.753–0.890)] and CYFRA21-1 [0.833 (95% CI: 0.756–0.893)]. No obvious differences were found between the AUC values of each indicator (P>0.05). YI was the largest at 0.67 ng/µl cfDNA, which was defined as the cut-off value of cfDNA, and yielded a sensitivity of 81.67% and a specificity of 77.94%. By comparison, at the cut-off values of CEA and CYFRA21-1, the sensitivity of CEA was 61.67% with a specificity of 97.06%, and the sensitivity of CYFRA21-1 was 63.33% with a specificity of 91.18%. To determine whether cfDNA quantification could be used in combination with existing biomarkers to maximize the diagnostic efficiency for NSCLC patients, the ROC AUC was calculated after combining CEA and CYFRA21-1 with cfDNA. The integration of cfDNA with CEA and CYFRA21-1 (AUC 0.915; sensitivity 83.33%; and specificity 85.29%) resulted in an improved diagnostic efficiency for NSCLC (Table II).
Figure 3.
Diagnostic utility of serum cfDNA, CEA and CYFRA21-1 in NSCLC patients. (A) ROC curves of serum cfDNA, CEA, CYFRA21-1 and the combination of the three markers for distinguishing NSCLC patients from normal controls. (B) ROC curves of pairwise combinations of cfDNA, CEA, and CYFRA21-1 for distinguishing NSCLC patients from normal controls. cfDNA, cell-free DNA; NSCLC, non-small cell lung cancer; ROC, receiver operating characteristic.
Table II.
Diagnostic value of serum cfDNA, CEA and CYFRA21-1 for NSCLC patients.
| Marker | AUC | Sensitivity (%) | Specificity (%) | Positive predictive value (%) | Negative predictive value (%) |
|---|---|---|---|---|---|
| cfDNA | 0.85 | 81.67 | 77.94 | 76.60 | 82.80 |
| CEA | 0.83 | 61.67 | 97.06 | 94.90 | 74.20 |
| CYFRA21-1 | 0.83 | 63.33 | 91.18 | 86.40 | 73.80 |
| CEA + CYFRA21-1 | 0.87 | 70.00 | 94.12 | 91.30 | 78.00 |
| cfDNA + CEA | 0.908a | 75.00 | 92.65 | 90.00 | 80.80 |
| cfDNA + CYFRA21-1 | 0.894a | 73.33 | 92.65 | 89.80 | 79.70 |
| cfDNA + CEA + CYFRA21-1 | 0.915a | 83.33 | 85.29 | 83.30 | 85.30 |
cfDNA, cell-free DNA; NSCLC, non-small cell lung cancer.
P<0.05 vs. cfDNA group.
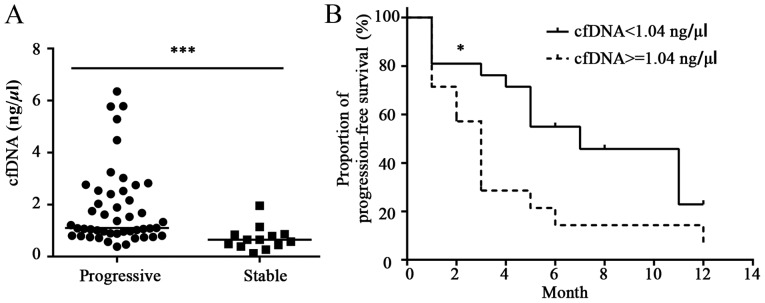
Connection between serum cfDNA and clinical NSCLC progression
To assess whether the cfDNA concentration is different in samples obtained from NSCLC patients with progressive rather than stable disease, the 60 NSCLC patients were divided into the progression and stable groups. The cfDNA concentration was higher in NSCLC patients with progressive disease than that in patients with stable disease (Fig. 4A). In addition, the Kaplan-Meier curve revealed that serum cfDNA ≥1.04 ng/µl was related to poorer PFS than serum cfDNA <1.04 ng/µl (median PFS: 7.0 vs. 3.0 months, hazard ratio [HR], 0.43; 95% confidence interval [CI]: 0.19–0.96, P<0.05) (Fig. 4B).
Figure 4.
The cfDNA concentration in NSCLC patients with stable vs. progressive disease. (A) Comparison of serum cfDNA concentrations in NSCLC patients with progressive or stable disease. (B) Kaplan-Meier curves of PFS based on serum cfDNA levels in NSCLC patients. P-values were calculated by using the Mann-Whitney test. *P<0.05 and ***P<0.001 indicate statistical significance. cfDNA, cell-free DNA; NSCLC, non-small cell lung cancer; PFS, progression-free survival.
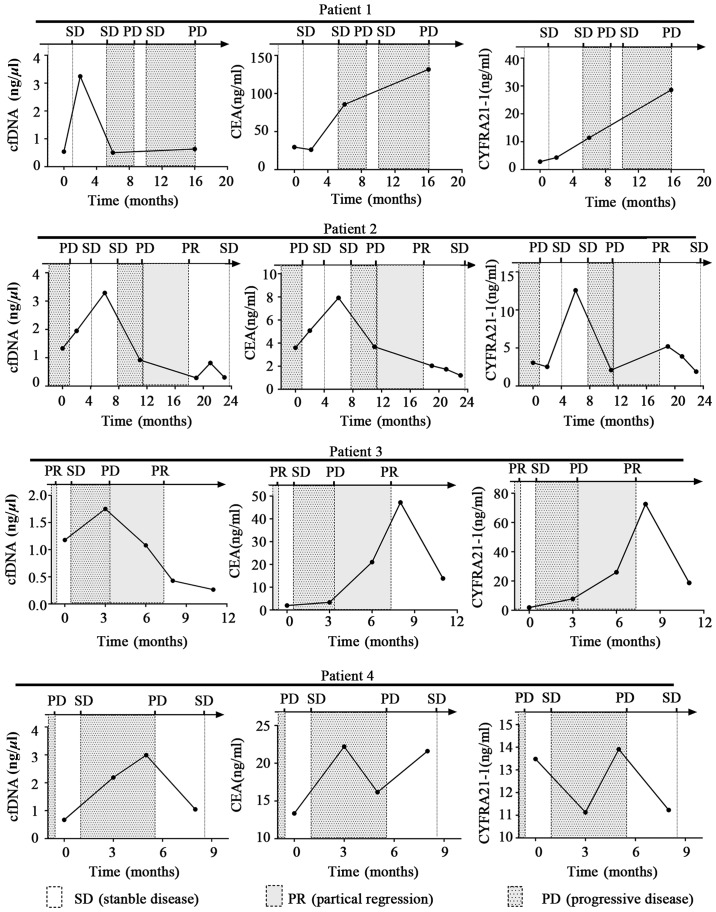
Serum cfDNA level dynamics in NSCLC patients
To identify the predictive value of cfDNA in NSCLC progression, cfDNA, CEA and CYFRA21-1 levels were analysed in serum samples from 4 NSCLC patients with progressive disease at several time-points. The line charts were plotted to describe the changes in cfDNA, CEA and CYFRA21-1 levels during cancer progression. As shown in Fig. 5, the time-dependent changes in the three markers in patient 2 were nearly identical, but were inconsistent with the changes in the other 3 NSCLC patients. During the course of the disease, there was a general trend of cfDNA concentration decreasing or remaining stable before periods of disease stability, and increasing before periods of disease progression. Interestingly, cfDNA levels often peaked before a period of disease progression, and the lead time was 1–7 months compared with clinical medical imaging. Alterations in serum levels of CEA and CYFRA21-1 occurred in line with disease progression, and did not show such peaks.
Figure 5.
Line charts of serum cfDNA, CEA and CYFRA21-1 concentrations at serial time-points in patients with NSCLC. SD, stable disease; PR, partial response; PD, progressive disease; cfDNA, cell-free DNA; NSCLC, non-small cell lung cancer. Disease was detected by medical imaging.
Discussion
In this study, we established optimal conditions for processing, cryopreserving, and storing cfDNA and developed a standard protocol for the quantification of circulating cfDNA by absolute LINE1 qPCR. We utilized this approach to examine serum cfDNA levels in 60 NSCLC patients with different stage disease and 68 normal controls to determine whether changes in serum cfDNA levels have diagnostic and predictive value for NSCLC, and we compared the diagnostic value of serum cfDNA, CEA and CYFRA21-1 by ROC curve analysis. Furthermore, we examined the time-dependent changes in serum cfDNA levels in 4 NSCLC patients during cancer progression.
There is some controversy about the optimal source of cfDNA for analysis. Previous studies suggested that plasma may be a more reliable source than serum owing to higher background levels of non-tumour wild-type DNA in serum (19). However, there are some other studies that have suggested the use of serum cfDNA in the diagnosis of malignancies such as hepatocellular carcinoma and endometrial cancer (20,21). In addition, serum samples are prepared without anticoagulants, and there is no need for specialized blood collection tubes, as there is for plasma. Serum is still considered as the gold standard, and used more widely than plasma in clinical laboratory. Therefore, we extracted cfDNA from serum samples for analysis, and showed that the quantification of circulating cfDNA levels in serum have value as a diagnostic for NSCLC or for monitoring disease progression.
There are no clear criteria for blood collection or storage conditions for cfDNA analysis. There is a concern, for instance, that the in vitro lysis of leukocytes during the coagulation/fibrinolysis phase of sample preparation will lead to higher serum cfDNA concentrations. In our study, compared with the cfDNA concentrations in serum prepared immediately after venepuncture (0 h at room temperature), the cfDNA concentrations in serum samples were decreased when serum was stored at room temperature up to 10 h, but were not significantly different after storage at lower temperatures, such as 4, −25 or −80°C. This phenomenon may be due to the degradation of cfDNA at room temperature by DNase activity, which is inhibited at lower temperatures. According to these results, serum samples for cfDNA quantification were frozen at −8°C immediately after collection. Two main sources of cfDNA have been proposed: release from apoptotic or necrotic cells or release of intact cells in the bloodstream (22). In our study, the size profile of cfDNA in plasma samples showed a major peak at 166 bp and another outstanding peak at 350 bp. Interestingly, serum cfDNA profiling showed more peak diversity. In addition to the relatively short 166-bp cfDNA fragments, cfDNA fragment peaks were observed ranging from 580 to 3,200 bp. We propose that the 166-bp peak probably represents DNA coiled around a nucleosome core unit (~146 bp) with a linker section of DNA (~20 bp), while the remaining peaks likely result from inter-nucleosome cleavage of genomic DNA.
cfDNA levels can be quantified by several techniques, including DNA Dipstick, PicoGreen, Agilent 2100 Bioanalyzer and real-time PCR. Moreover, several studies have quantified cfDNA by using real-time PCR with various reference genes such as human β-actin, hTERT, GAPDH, ALU and LINE-1 (10,23). In our study, we carried out a pre-experiment to optimize quantification of cfDNA before formal test. The pre-experiment results demonstrated that the levels of cfDNA of NSCLC patients quantified by qPCR results using primer of β-actin and LINE-1 have the same varying trend. Also, the amplification efficiency was greater with LINE-1 primer (data not shown). Therefore, we used absolute qPCR analysis of LINE-1 to quantify serum and plasma cfDNA in the present study. The cfDNA concentrations were 1- to 8-fold higher in fresh serum samples than those in fresh plasma samples, which is consistent with previous reports that serum samples contain 2- to 24-fold higher levels of cfDNA than plasma samples (24,25). Moreover, the cfDNA level in NSCLC patients [1.06 (0.75–2.01) ng/µl] was significantly higher than that in normal controls [0.47 (0.23–0.86) ng/µl], which is consistent with the previous reports.
In the present study, we also found that NSCLC patients with lymph node metastasis and distant metastases had a significantly higher cfDNA level. Furthermore, NSCLC patients with advanced stage (III–IV) disease had considerably higher cfDNA levels than that in normal controls or patients with stage I–II disease, which was consistent with previous reports. Importantly, no significant differences were detected between normal controls and patients with stage I–II disease or between NSCLC patients of different ages or sex. We suspect that serum cfDNA may not be sensitive enough for early detection of NSCLC patients, further studies are needed to confirm this hypothesis. Previous studies have suggested the cfDNA levels are affected by cancer-dependent variables, including tumour size, location, and stage, as well as other elements related to risk and prognosis (6). Consequently, while it is evident that serum cfDNA levels are correlated with advanced tumour stage and metastasis in NSCLC patients, they are not closely related to age or sex.
Tumour biomarkers in serum from NSCLC patients, such as CEA and CYFRA21-1, are not sufficient to diagnose or monitor lung cancer due to the lack of sensitivity and specificity to a particular type of cancer, and the levels of these factors may be increased by irrelevant issues (26,27). According to the results, the AUC of serum cfDNA for distinguishing NSCLC patients from normal controls was comparable to that of CEA and CYFRA21-1. In addition, compared with the diagnostic efficiency of serum cfDNA, serum CEA or CYFRA21-1 alone, the combination of these three factors into one indicator improved the diagnostic efficiency for NSCLC. This result indicates that cfDNA is a good screening tool for NSCLC that may be used in combination with existing biomarkers to improve the diagnostic efficacy.
Our results also showed that the serum cfDNA concentration was higher in NSCLC patients with progressive disease than that in those with stable disease. In addition, higher serum cfDNA levels were related to poorer PFS in patients with NSCLC. In patients suffering from different carcinomas, higher cfDNA concentrations have been shown to be an independent predictor of a worse outcome regarding overall survival or an interval irrelevant to disease (28–33). Increasing cfDNA levels suggest tumour progression during therapy, while decreasing levels indicate an early treatment response (34,35). By tracking the serum cfDNA concentration at several time-points in 4 NSCLC patients, we found that cfDNA levels decreased in samples from NSCLC patients with stable disease, and tended to increase during or before periods of disease progression, with a lead time of 1–7 months compared with clinical medical imaging. Although the number of cases was small, and further confirmation is needed, these findings show that increasing serum cfDNA values in patients during follow-up may indicate progression earlier than that in clinical imaging studies.
In conclusion, the present investigation indicates that serum cfDNA might be a valuable new biomarker for diagnosing NSCLC and monitoring metastatic progression. Quantification of cfDNA may therefore contribute to molecular staging, and to optimizing advanced personalized medicine for NSCLC. Future studies on a larger number of NSCLC patients with a sufficient follow-up time are now required to further validate the clinical utility of serum cfDNA.
Acknowledgements
Not applicable.
Funding
This study was supported by the Seed Fund Program of Shanghai University of Medicine & Health Sciences (no. HMSF-16-21-020).
Availability of data and materials
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.
Authors' contributions
LW and WW designed the study, carried out the experiment and wrote the manuscript. LH and WY collected and analyzed the data. YD conceived the original idea and analyzed the results. All authors read and approved the final manuscript.
Ethics approval and consent to participate
The study was approved by the Ethics Committee of Shanghai Sixth People's Hospital East Affiliated to Shanghai University of Medicine & Health Sciences (Shanghai, China). Patients who participated in this research, signed an informed consent and had complete clinical data.
Patient consent for publication
Not applicable.
Competing interests
The authors declare that they have no competing interests.
References
- 1.Ettinger DS, Akerley W, Bepler G, Blum MG, Chang A, Cheney RT, Chirieac LR, D'Amico TA, Demmy TL, Ganti AK, et al. NCCN Non-Small Cell Lung Cancer Panel Members, corp-author. Non-small cell lung cancer. J Natl Compr Canc Netw. 2010;8:740–801. doi: 10.6004/jnccn.2010.0056. [DOI] [PubMed] [Google Scholar]
- 2.Torre LA, Bray F, Siegel RL, Ferlay J, Lortet-Tieulent J, Jemal A. Global cancer statistics, 2012. CA Cancer J Clin. 2015;65:87–108. doi: 10.3322/caac.21262. [DOI] [PubMed] [Google Scholar]
- 3.Schiller JH, Harrington D, Belani CP, Langer C, Sandler A, Krook J, Zhu J, Johnson DH, Eastern Cooperative Oncology Group Comparison of four chemotherapy regimens for advanced non-small-cell lung cancer. N Engl J Med. 2002;346:92–98. doi: 10.1056/NEJMoa011954. [DOI] [PubMed] [Google Scholar]
- 4.Stroun M, Lyautey J, Lederrey C, Olson-Sand A, Anker P. About the possible origin and mechanism of circulating DNA apoptosis and active DNA release. Clin Chim Acta. 2001;313:139–142. doi: 10.1016/S0009-8981(01)00665-9. [DOI] [PubMed] [Google Scholar]
- 5.Volik S, Alcaide M, Morin RD, Collins C. Cell-free DNA (cfDNA): Clinical significance and utility in cancer shaped by emerging technologies. Mol Cancer Res. 2016;14:898–908. doi: 10.1158/1541-7786.MCR-16-0044. [DOI] [PubMed] [Google Scholar]
- 6.Jung K, Fleischhacker M, Rabien A. Cell-free DNA in the blood as a solid tumor biomarker—a critical appraisal of the literature. Clin Chim Acta. 2010;411:1611–1624. doi: 10.1016/j.cca.2010.07.032. [DOI] [PubMed] [Google Scholar]
- 7.Chiappetta C, Anile M, Leopizzi M, Venuta F, Della Rocca C. Use of a new generation of capillary electrophoresis to quantify circulating free DNA in non-small cell lung cancer. Clin Chim Acta. 2013;425:93–96. doi: 10.1016/j.cca.2013.07.014. [DOI] [PubMed] [Google Scholar]
- 8.Ulivi P, Mercatali L, Casoni GL, Scarpi E, Bucchi L, Silvestrini R, Sanna S, Monteverde M, Amadori D, Poletti V, et al. Multiple marker detection in peripheral blood for NSCLC diagnosis. PLoS One. 2013;8:e57401. doi: 10.1371/journal.pone.0057401. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Cargnin S, Canonico PL, Genazzani AA, Terrazzino S. Quantitative analysis of circulating cell-free DNA for correlation with lung cancer survival: A systematic review and meta-analysis. J Thorac Oncol. 2017;12:43–53. doi: 10.1016/j.jtho.2016.08.002. [DOI] [PubMed] [Google Scholar]
- 10.Jiang T, Zhai C, Su C, Ren S, Zhou C. The diagnostic value of circulating cell free DNA quantification in non-small cell lung cancer: A systematic review with meta-analysis. Lung Cancer. 2016;100:63–70. doi: 10.1016/j.lungcan.2016.06.013. [DOI] [PubMed] [Google Scholar]
- 11.Sozzi G, Conte D, Leon M, Ciricione R, Roz L, Ratcliffe C, Roz E, Cirenei N, Bellomi M, Pelosi G, et al. Quantification of free circulating DNA as a diagnostic marker in lung cancer. J Clin Oncol. 2003;21:3902–3908. doi: 10.1200/JCO.2003.02.006. [DOI] [PubMed] [Google Scholar]
- 12.Devonshire AS, Whale AS, Gutteridge A, Jones G, Cowen S, Foy CA, Huggett JF. Towards standardisation of cell-free DNA measurement in plasma: Controls for extraction efficiency, fragment size bias and quantification. Anal Bioanal Chem. 2014;406:6499–6512. doi: 10.1007/s00216-014-7835-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Jen J, Wu L, Sidransky D. An overview on the isolation and analysis of circulating tumor DNA in plasma and serum. Ann NY Acad Sci. 2000;906:8–12. doi: 10.1111/j.1749-6632.2000.tb06581.x. [DOI] [PubMed] [Google Scholar]
- 14.Lui YY, Chik KW, Lo YM. Does centrifugation cause the ex vivo release of DNA from blood cells? Clin Chem. 2002;48:2074–2076. [PubMed] [Google Scholar]
- 15.Jung M, Klotzek S, Lewandowski M, Fleischhacker M, Jung K. Changes in concentration of DNA in serum and plasma during storage of blood samples. Clin Chem. 2003;49:1028–1029. doi: 10.1373/49.6.1028. [DOI] [PubMed] [Google Scholar]
- 16.Eisenhauer EA, Therasse P, Bogaerts J, Schwartz LH, Sargent D, Ford R, Dancey J, Arbuck S, Gwyther S, Mooney M, et al. New response evaluation criteria in solid tumours: revised RECIST guideline (version 1.1) Eur J Cancer. 2009;45:228–247. doi: 10.1016/j.ejca.2008.10.026. [DOI] [PubMed] [Google Scholar]
- 17.Holdhoff M, Schmidt K, Diehl F, Aggrawal N, Angenendt P, Romans K, Edelstein DL, Torbenson M, Kinzler KW, Vogelstein B, et al. Detection of tumor DNA at the margins of colorectal cancer liver metastasis. Clin Cancer Res. 2011;17:3551–3557. doi: 10.1158/1078-0432.CCR-10-3087. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang Q, Zheng H, Hu F, Zhang H, Hu Y, Li J, Zhang T, Liu Z, Lu B, Hu A, et al. Serum CYFRA21-1 is correlated with the efficacy of epidermal growth factor receptor-tyrosine kinase inhibitor in non-small cell lung cancer patients harboring EGFR mutations. Zhongguo Fei Ai Za Zhi. 2016;19:550–558. doi: 10.3779/j.issn.1009-3419.2016.08.12. (In Chinese) [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Molina-Vila MA, de-Las-Casas CM, Bertran-Alamillo J, Jordana-Ariza N, González-Cao M, Rosell R. cfDNA analysis from blood in melanoma. Ann Transl Med. 2015;3:309. doi: 10.3978/j.issn.2305-5839.2015.11.23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Chen K, Zhang H, Zhang LN, Ju SQ, Qi J, Huang DF, Li F, Wei Q, Zhang J. Value of circulating cell-free DNA in diagnosis of hepatocelluar carcinoma. World J Gastroenterol. 2013;19:3143–3149. doi: 10.3748/wjg.v19.i20.3143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Cicchillitti L, Corrado G, De Angeli M, Mancini E, Baiocco E, Patrizi L, Zampa A, Merola R, Martayan A, Conti L, et al. Circulating cell-free DNA content as blood based biomarker in endometrial cancer. Oncotarget. 2017;8:115230–115243. doi: 10.18632/oncotarget.23247. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Gormally E, Caboux E, Vineis P, Hainaut P. Circulating free DNA in plasma or serum as biomarker of carcinogenesis: Practical aspects and biological significance. Mutat Res. 2007;635:105–117. doi: 10.1016/j.mrrev.2006.11.002. [DOI] [PubMed] [Google Scholar]
- 23.Fawzy A, Sweify KM, El-Fayoumy HM, Nofal N. Quantitative analysis of plasma cell-free DNA and its DNA integrity in patients with metastatic prostate cancer using ALU sequence. J Egypt Natl Cancer Inst. 2016;28:235–242. doi: 10.1016/j.jnci.2016.08.003. [DOI] [PubMed] [Google Scholar]
- 24.Lo YM, Tein MS, Lau TK, Haines CJ, Leung TN, Poon PM, Wainscoat JS, Johnson PJ, Chang AM, Hjelm NM. Quantitative analysis of fetal DNA in maternal plasma and serum: Implications for noninvasive prenatal diagnosis. Am J Hum Genet. 1998;62:768–775. doi: 10.1086/301800. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Lee TH, Montalvo L, Chrebtow V, Busch MP. Quantitation of genomic DNA in plasma and serum samples: Higher concentrations of genomic DNA found in serum than in plasma. Transfusion. 2001;41:276–282. doi: 10.1046/j.1537-2995.2001.41020276.x. [DOI] [PubMed] [Google Scholar]
- 26.Ma S, Shen L, Qian N, Chen K. The prognostic values of CA125, CA19.9, NSE, AND SCC for stage I NSCLC are limited. Cancer Biomark. 2011-2012;10:155–162. doi: 10.3233/CBM-2012-0246. [DOI] [PubMed] [Google Scholar]
- 27.Rosell R, Carcereny E, Gervais R, Vergnenegre A, Massuti B, Felip E, Palmero R, Garcia-Gomez R, Pallares C, Sanchez JM, et al. Spanish Lung Cancer Group in collaboration with Groupe Français de Pneumo-Cancérologie and Associazione Italiana Oncologia Toracica Erlotinib versus standard chemotherapy as first-line treatment for European patients with advanced EGFR mutation-positive non-small-cell lung cancer (EURTAC): A multicentre, open-label, randomised phase 3 trial. Lancet Oncol. 2012-2012;13:239–246. doi: 10.1016/S1470-2045(11)70393-X. [DOI] [PubMed] [Google Scholar]
- 28.Schwarzenbach H, Müller V, Stahmann N, Pantel K. Detection and characterization of circulating microsatellite-DNA in blood of patients with breast cancer. Ann NY Acad Sci. 2004;1022:25–32. doi: 10.1196/annals.1318.005. [DOI] [PubMed] [Google Scholar]
- 29.Ren N, Qin LX, Tu H, Liu YK, Zhang BH, Tang ZY. The prognostic value of circulating plasma DNA level and its allelic imbalance on chromosome 8p in patients with hepatocellular carcinoma. J Cancer Res Clin Oncol. 2006;132:399–407. doi: 10.1007/s00432-005-0049-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Yoon KA, Park S, Lee SH, Kim JH, Lee JS. Comparison of circulating plasma DNA levels between lung cancer patients and healthy controls. J Mol Diagn. 2009;11:182–185. doi: 10.2353/jmoldx.2009.080098. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Ludovini V, Pistola L, Gregorc V, Floriani I, Rulli E, Piattoni S, Di Carlo L, Semeraro A, Darwish S, Tofanetti FR, et al. Plasma DNA, microsatellite alterations, and p53 tumor mutations are associated with disease-free survival in radically resected non-small cell lung cancer patients: a study of the perugia multidisciplinary team for thoracic oncology. J Thorac Oncol. 2008;3:365–373. doi: 10.1097/JTO.0b013e318168c7d0. [DOI] [PubMed] [Google Scholar]
- 32.Kamat AA, Baldwin M, Urbauer D, Dang D, Han LY, Godwin A, Karlan BY, Simpson JL, Gershenson DM, Coleman RL, et al. Plasma cell-free DNA in ovarian cancer: An independent prognostic biomarker. Cancer. 2010;116:1918–1925. doi: 10.1002/cncr.24997. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Jung K, Stephan C, Lewandowski M, Klotzek S, Jung M, Kristiansen G, Lein M, Loening SA, Schnorr D. Increased cell-free DNA in plasma of patients with metastatic spread in prostate cancer. Cancer Lett. 2004;205:173–180. doi: 10.1016/j.canlet.2003.11.023. [DOI] [PubMed] [Google Scholar]
- 34.Gautschi O, Bigosch C, Huegli B, Jermann M, Marx A, Chassé E, Ratschiller D, Weder W, Joerger M, Betticher DC, et al. Circulating deoxyribonucleic Acid as prognostic marker in non-small-cell lung cancer patients undergoing chemotherapy. J Clin Oncol. 2004;22:4157–4164. doi: 10.1200/JCO.2004.11.123. [DOI] [PubMed] [Google Scholar]
- 35.Kumar S, Guleria R, Singh V, Bharti AC, Mohan A, Das BC. Efficacy of circulating plasma DNA as a diagnostic tool for advanced non-small cell lung cancer and its predictive utility for survival and response to chemotherapy. Lung Cancer. 2010;70:211–217. doi: 10.1016/j.lungcan.2010.01.021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
The datasets used and/or analyzed during the present study are available from the corresponding author on reasonable request.