Abstract
Objectives:
Cardiopulmonary resuscitation (CPR) is lifesaving. Yet, cardiac arrest survival remains low despite CPR intervention. Education has been highlighted as a strategy to overcome this issue. Virtual Reality technology has been gaining momentum in the field of clinical education. Published studies report benefits of virtual reality for CPR education; yet, perceptions of CPR instructors towards virtual reality remain unexplored. CPR instructors are key stakeholders in CPR education and their perceptions are valuable for the design and adoption of virtual reality-enhanced learning. The purpose of this study is therefore to understand the perceptions of CPR instructors towards using virtual reality for health professionals’ CPR education. The aim was addressed via three research questions: (1) What are the perceptions of CPR instructors towards current health professionals’ CPR education? (2) What are the perceptions of CPR instructors towards features of virtual reality ideal for health professionals’ CPR education? (3) What are the perceptions of CPR instructors towards the potential role of virtual reality in health professionals’ CPR education?
Methods:
A total of 30 CPR instructors were surveyed on their views towards current health professionals’ CPR education and the use of virtual reality for health professionals’ CPR education, before and after interacting with a CPR virtual reality simulation. Responses were analysed using interpretative thematic analysis.
Results:
CPR instructors perceived current health professionals’ CPR education as limited due to unideal test preparation (resources, practice, motivation, and frame of mind) and performance. They perceived fidelity, engagement, resource conservation, and memory enhancement as features of virtual reality ideal for health professionals’ CPR education. Virtual reality was viewed by CPR instructors as having potential as a blended learning tool, targeting both ‘novice’ and ‘experienced’ health professionals.
Conclusion:
The study highlighted the gaps in current health professionals’ CPR education that can be addressed using virtual-reality-enabled learning. Future research could investigate virtual reality simulations with features desirable for CPR education of target populations.
Keywords: Medical education, cardiopulmonary resuscitation, virtual reality, educational technology
Introduction
Cardiopulmonary resuscitation education
Cardiopulmonary resuscitation (CPR) is an emergency procedure which comprises artificial ventilation and chest compressions to preserve circulation to the brain when cardiac arrest has occurred. CPR can save lives.1–3 However, survival rates remain low at 11.4% for out-patient cardiac arrest and 23.8% for in-hospital cardiac arrest (2015)4 even when CPR intervention is implemented. The Formula for Survival proposes education as a strategy to improve survival rates,5 making education crucial in narrowing gaps between actual and ideal CPR performance. Effective CPR education requires both the acquisition of knowledge and skills and ultimately the ability to demonstrate its application in actual performance. With regard to knowledge acquisition, two main modes of CPR training exist – (1) instructor-led training often in the face-to-face setting and (2) independent learning usually delivered using eLearning. Challenges remain in terms of the ability to provide CPR education at scale and in the realm of health professionals’ lifelong learning.
Virtual reality
The advent of emerging technologies has seen progress in many fields, including medical education.6 Medical Simulation involves artificial representation of clinical scenarios to achieve educational goals via experimental learning.7,8 Virtual Reality (VR) technology has been gaining momentum in this field.9 VR renders a computer-generated, three-dimensional portrayal of places in the real or imaginary world.10 It provides an immersive experience for users, resulting in improvements in procedural memory,11 speed, accuracy, and transfer of skills to real-life scenarios, compared to instructor-led training.12 VR could enable effective technology-enhanced CPR education in the context of increasing numbers of CPR-trained personnel and improving the standard of skills and knowledge acquired by enabling more convenient and frequent opportunities for learning.13 While published studies report on the benefits of VR for CPR education, in the form of improved skills,14,15 the perceptions of CPR instructors towards VR remain unexplored. CPR instructors are key stakeholders in CPR education and their perceptions are valuable for the design and adoption of VR-enhanced learning and assessment activities. Furthermore, CPR instructors are experts in CPR education who are experienced in teaching and assessing first-time students (‘novice’ learners) and qualified students awaiting recertification (‘experienced’ learners). They have the most realistic expectations of CPR survival compared to laypersons, nurses, and physicians.16
Aim
The overall purpose of this study is to understand the perceptions of CPR instructors towards using VR for health professionals’ CPR education. The aim was addressed via three research questions: (1) What are the perceptions of CPR instructors towards current health professionals’ CPR education? (2) What are the perceptions of CPR instructors towards features of VR ideal for health professionals’ CPR education? (3) What are the perceptions of CPR instructors towards the potential role of VR in health professionals’ CPR education?
Methods
Participants
Participants are certified CPR instructors (n = 30, doctors and nurses) from an academic hospital in Singapore which employs eLearning for health professionals’ CPR education. The sample demographics are as follows. The mean age of participants was 40 years and the standard deviation was 7.1 years. Mean years of experience as CPR instructors were 7 years, with the standard deviation being 3.8 years. Of the population studied, in terms of gender, 5 were males and 25 were females. With regard to profession, 5 were doctors and 25 were nurses.
Participants were recruited through contact with staff from the hospital’s Medical Education and Human Resource Department. At the time of the study, the hospital had 150 certified CPR instructors, all of whom were contacted, but only 30 CPR instructors registered for the study. Prior to the commencement of the study, participants signed a consent form, acknowledging that they understood the provided information and were willing to participate. Ethical approval was granted by the Nanyang Technological University Institutional Review Board (IRB-2016-07-035) to carry out the study with health professionals.
CPR VR solution
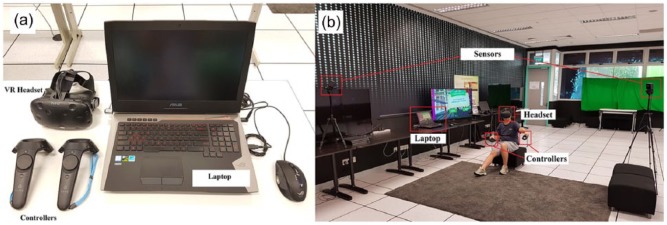
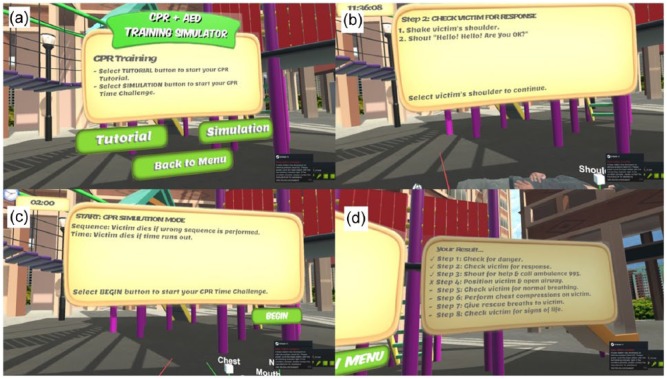
The CPR + automated external defibrillator (AED) VR Simulation, created by the members of the Institute of Technical Education (Singapore), was used. It is a VR simulation which focuses on CPR and AED procedural training, which involves familiarising oneself with the CPR steps and mastering their sequence. Skills such as chest compressions and ventilations are performed by the avatar, and not the user. The CPR + AED VR Simulation uses Steam VR technology and is deployed on HTC VIVE, with sensors detecting the VR headset and controllers tracking users’ location and input (Figure 1). Two game modes exist – (1) Tutorial (step-by-step instructions on CPR procedures) and (2) Simulation (test on CPR steps with time limit and performance feedback) (Figure 2).
Figure 1.
CPR + AED VR Simulation: (a) Equipment and (b) Set-up.
Figure 2.
CPR + AED VR Simulation game modes: (a) Game mode options, (b) Tutorial mode step-by-step instructions, (c) Simulation mode test rules, and (d) Simulation mode performance feedback.
Data collection
Data collection was conducted in Singapore English. Participants completed Questionnaire A (10 min), which focused on their perceptions towards current health professionals’ CPR education. They next attempted Tutorial and Simulation modes of the CPR + AED VR Simulation (15 min), followed by Questionnaire B (10 min), which obtained opinions on VR use for health professionals’ CPR education. The questionnaires were not validated but rather formulated based on the research questions and gaps in current knowledge between VR and CPR education. Participation observation was employed. The first author was present while participants completed the questionnaires and attempted the simulation. Participant responses were clarified as they attempted the questionnaires (Table 1).
Table 1.
Items in Questionnaires A and B.
| Questionnaire A – items | Questionnaire B – items |
|---|---|
| • Candidates pass their CPR test easily on their first try. (five Likert-type scale from strongly agree to strongly disagree) • What are some common mistakes made by CPR test candidates? (open-ended) • Why do you think such mistakes are made? (open-ended) • Virtual Reality (VR) is a technology which uses computers to generate 3D portrayal of places in the real or imaginary world. Scenarios can be implanted for student training, e.g., cardiac arrest situation used to teach CPR. - Do you have any experience with VR technology? If yes, please provide details. (open-ended) - What is your view on using VR as part of CPR education? (open-ended) |
• What are your opinions towards using the CPR + AED VR Simulation as part of CPR education? (open-ended) • What role can the CPR + AED VR Simulation play in CPR education? (open-ended) • Any other comments? (open-ended) |
CPR: cardiopulmonary resuscitation; AED: automated external defibrillator.
Analysis
We used six steps proposed by Braun and Clarke17 to conduct an interpretive thematic analysis. First, the open-ended answers data collected using the two questionnaires (A and B) were transcribed verbatim and the first and second authors read all the transcripts multiple times to familiarise themselves with the content. A reflective segment was also used at this stage by these same authors to record initial impressions and note similarities and differences. Second, these same authors separately identified features in a systematic manner using general codes across the collected data set, writing these codes in the margins of each transcript. Third, the researchers met and discussed their preliminary codes and collated interpretations into further themes. Data saturation was reached when further coding was no longer feasible. Fourth, the coded data were developed by consensus into a thematic map, whereby the researchers considered the alignment of themes and sub-themes. Fifth, to refine each theme, clear definitions were derived for each label. As thematic analysis can go beyond organising and describing to interpreting, Braun and Clarke’s sixth step was employed to theorise the significance of the patterns and their broader meanings and implications beyond a surface level. This sixth step comprised selecting compelling extracts and relating these back to the research questions and the literature.
Results
Current CPR education
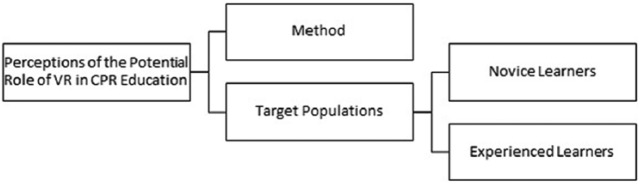
CPR instructors perceived current health professionals’ CPR education as limited (Figure 3) due to unideal test preparation. A cause of this is inadequate resources, such as teaching material (eLearning) which does not consider the different learning styles of students. CPR practice opportunities are also insufficient, as students only practice during biannual refresher tests, unless they work in acute settings which require frequent, real-life CPR performance, such as the Emergency Department and Intensive Care Unit. Unideal test preparation is also attributed by participants to lack of motivation. Many students do not study eLearning materials prior to the test, possibly due to complacency or lack of prioritisation. In addition, CPR test candidates are perceived by CPR instructors as having suboptimal frames of mind for tests. Their anxiety results in hurried performance, and they are easily distracted during tests, which leads to impaired CPR execution.
Figure 3.
CPR instructors’ perceptions of current CPR education.
CPR instructors also commented that test performance of CPR test candidates is unideal, as supported by the common mistakes made, including poor technique, jumbled steps and sequence, and inaccurate landmark identification.
Features of VR ideal for CPR education
CPR instructors identified fidelity, engagement, resource conservation, and memory enhancement as features of VR ideal for health professionals’ CPR education (Figure 4). Fidelity is the degree with which real experiences are reproduced by a system.18 Participants valued fidelity, as they commented that VR simulations allow easy visualisation of real-life situations, and that hands-on practice is ideal since CPR is a technical skill. CPR instructors also regarded engagement as a useful VR feature. They felt that the gaming approach of VR is fun and innovative, and hence interesting to young learners, possibly promoting better understanding and willingness to learn. Conversely, difficulties may be faced by the older generation. Conserving resources, such as manpower, was another attractive aspect to participants. VR achieves this by encouraging independent revision. Finally, CPR instructors attributed importance on memory enhancement, attained by controlling distractions, having a focused task (in this context, procedural steps recall), and clarity of content.
Figure 4.
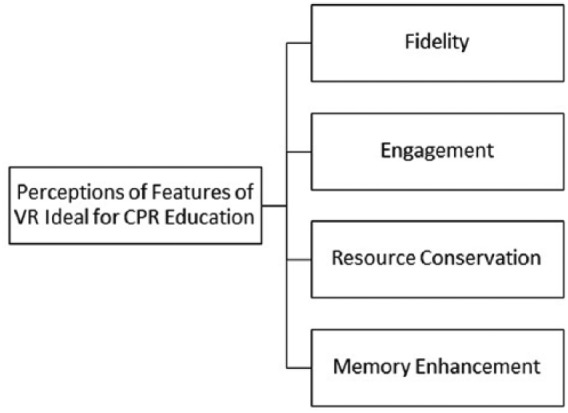
CPR instructors’ perceptions of features of VR ideal for CPR education.
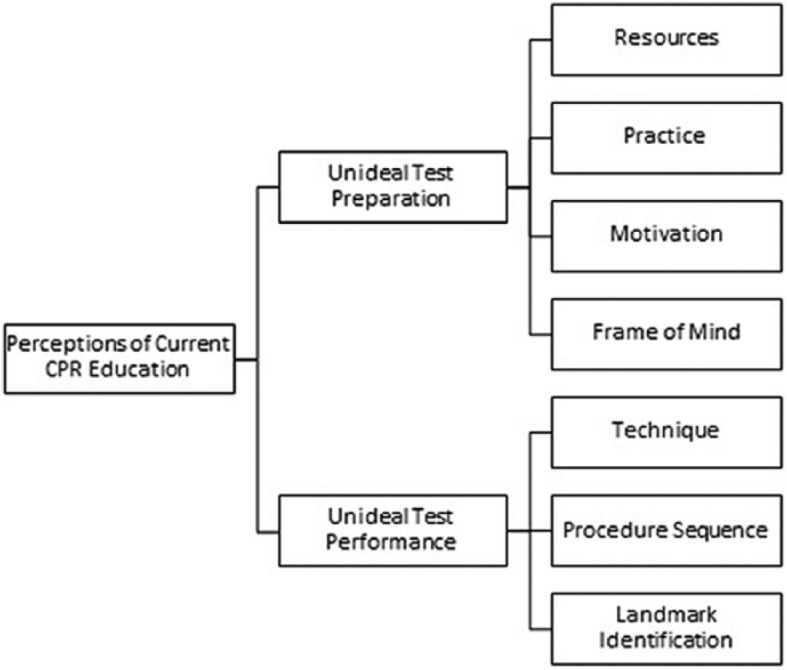
Potential role of VR in CPR education
Participants saw potential in VR as a tool for health professionals’ CPR education (Figure 5). They proposed the use of VR as a blended learning tool, together with eLearning, as it could increase students’ attention and motivation to learn. They also identified potential learner profiles who can benefit from VR in CPR education. VR may enhance the training process of novice learners, who have just started learning CPR. VR can also be useful for experienced learners who have previously passed the CPR test, by allowing revision of knowledge and skills.
Figure 5.
CPR instructors’ perceptions of the potential role of VR in CPR education.
Discussion
The results reveal that CPR instructors considered current health professionals’ CPR education as limited due to unideal test preparation and performance of test participants. Test preparation is hindered by resource inadequacy, which is also a worldwide issue.19–21
CPR instructors in the study saw VR as having potential to manage the limitations of health professionals’ CPR education established in the previous paragraph. CPR instructors identified fidelity, engagement, resource conservation, and memory enhancement as features of VR that make it ideal for health professionals’ CPR education. Fidelity can be a useful feature for tackling anxiety, as in Exposure-based Therapy, where VR promotes processing and acceptance of difficult situations by presenting realistic simulations in a safe environment.22 The need for hands-on practice was also highlighted, since CPR is a technical skill.23 Also significant was the belief that VR would be more engaging for younger students, which is possible24 given that older adults use fewer types of technology,25 resulting in difficulties absorbing information.26 Memory enhancement was perceived to be achieved by controlling distractions, having a focused task, and clear content. VR can indeed improve memory via increasing attention, conditioning, and organisation.27
Participants perceived potential in VR as a blended learning tool (combined with eLearning) for health professionals’ CPR education. Its usefulness lies in its ability to remedy highlighted limitations in eLearning, such as the lack of motivation to review study materials, and the paucity of practice opportunities, through the ideal features mentioned in the ‘Results’ section. Potential learners, and how they can benefit from VR, were considered. Both newly enrolled novice learners and experienced learners awaiting their refresher test could benefit in the knowledge and psychomotor domains of learning. VR features can help newly enrolled novice CPR test candidates in memory and skill mastery processes,27,28 which may otherwise prove challenging due to lack of prior knowledge. VR could also be a convenient practice tool for experienced refresher test students, in between biannual recertification tests, to achieve suggested optimal training intervals of less than 7 months29 despite resource scarcity.
Learners learn in different ways,30 and conventional eLearning cannot accommodate them all. VR can address this as it caters to various learning styles.31,32 Practice opportunities are also scarce, but necessary, as CPR knowledge and skills deteriorate over 3 to 6 months,33–37 which may result in non-optimal CPR performance, compromising patient survival.38–42 Motivation is likewise key in test preparation as it drives learning,43 but was highlighted by CPR instructors as lacking in students. Suboptimal frames of mind, in the form of anxiety, lowers CPR skills retention,44 and delays CPR initiation.45 The effect of this is not limited to the test setting, and unfortunately extends to real-life situations, resulting in reduced survival.38–42,46 Another form of suboptimal frame of mind is the inability to focus on the given task due to distractions. Distractions need to be controlled in order for learning to be maximised.47 Education influences test performance. Other aspects include psychological, physical, and socio-economic factors.48 Techniques and procedure sequence are determinants of CPR success,49,50 so there is a need to ensure that quality CPR is performed. CPR instructors’ opinions exposed the necessity for a tool which can overcome the limitations of current CPR education.
A limitation of this study is that participant factors, such as the inability to recall events and exaggeration, must be considered. The lack of suggestions by CPR instructors to use VR in isolation, after interacting with the VR simulation, implies that VR is not without drawbacks. For example, VR consists of pre-designed simulations, which may result in scopes of knowledge being limited.10 CPR instructors were not exposed to different CPR VR simulations created worldwide, each with their unique features. The exposure to a single simulation would have affected CPR instructors in this study, as they would have had an incomplete understanding of VR, and this might have influenced their responses. The use of a single site for data collection is also a limitation. While the cost of the HTC VIVE VR set is not inexpensive, it can be shared by numerous students over a long period of time as they can utilise it at different timings at a common location.
Conclusion
The study highlighted gaps in current health professionals’ CPR education that could be addressed using VR-enabled learning and assessment activities. CPR instructors identified fidelity, engagement, resource conservation, and memory enhancement as features of VR that make it ideal for health professionals’ CPR education. From an instructional design perspective, the study participants perceived potential in VR as a blended learning tool. With regard to the CPR VR solution used in the study which focuses on CPR procedural training, learners who would benefit most are both novice and experienced healthcare professionals.
As both the VR technology and its applications evolve, future research could further investigate CPR VR simulations with the features desirable for CPR education, preferably based on user-centric, design-based research approach. As the solutions mature with regard to their ecological validity, focus should be on performance to bring us closer to the goal of improved health professionals’ CPR education and consequently, decreased cardiac arrest deaths.
Supplemental Material
Supplemental material, Raw_Data_(2) for Clinical instructors’ perceptions of virtual reality in health professionals’ cardiopulmonary resuscitation education by Marie Ann Mae En Wong, Shien Chue, Michelle Jong, Ho Wye Kei Benny and Nabil Zary in SAGE Open Medicine
Acknowledgments
The authors would like to thank the team at the Institute of Technical Education College Central (Singapore) that developed the CPR VR prototype used in the study and their assistance during the data collection.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Ethical approval for this study was obtained from the Nanyang Technological University Institutional Review Board (IRB-2016-07-035).
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Written informed consent was obtained from all subjects before the study.
ORCID iD: Marie Ann Mae En Wong  https://orcid.org/0000-0001-6419-8165
https://orcid.org/0000-0001-6419-8165
References
- 1. Kouwenhoven WB, Jude JR, Knickerbocker G. Closed-chest cardiac massage. JAMA 1960; 173: 1064–1067. [DOI] [PubMed] [Google Scholar]
- 2. Herlitz J, Ekström L, Wennerblom B, et al. Effect of bystander initiated cardiopulmonary resuscitation on ventricular fibrillation and survival after witnessed cardiac arrest outside hospital. Br Heart J 1994; 72: 408–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Noordergraaf G, Ottesen JT, Scheffer G, et al. Cardiopulmonary resuscitation: biomedical and biophysical analysis (Chapter XXX). In: Bronzino JD. (ed.) Biomedical engineering handbook. 3rd ed. Boca Raton, FL: Taylor & Francis Group, 2004, p. 3. [Google Scholar]
- 4. Benjamin EJ, Blaha MJ, Chiuve SE, et al. Heart disease and stroke statistics-2017 update: a report from the American Heart Association. Circulation 2017; 135: e146–e603. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Søreide E, Morrison L, Hillman K, et al. The formula for survival in resuscitation. Resuscitation 2013; 84: 1487–1493. [DOI] [PubMed] [Google Scholar]
- 6. Kosakowski J. The benefits of information technology. ERIC Digest. ERIC Digest, 1998. [Google Scholar]
- 7. Al-Elq AH. Simulation-based medical teaching and learning. J Family Community Med 2010; 17: 35–40. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Flanagan B, Nestel D, Joseph M. Making patient safety the focus: crisis resource management in the undergraduate curriculum. Med Educ 2004; 38: 56–66. [DOI] [PubMed] [Google Scholar]
- 9. Kneebone R. Simulation in surgical training: educational issues and practical implications. Med Educ 2003; 37: 267–277. [DOI] [PubMed] [Google Scholar]
- 10. Moo FOA, Ezeani I, Okonkwo OR. Virtual reality and environments. London: IntechOpen, 2012 [Google Scholar]
- 11. Kim BR, Chun MH, Kim LS, et al. Effect of virtual reality on cognition in stroke patients. Ann Rehabil Med 2011; 35: 450–459. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Nagendran M, Gurusamy KS, Aggarwal R, et al. Virtual reality training for surgical trainees in laparoscopic surgery. Cochrane Database Syst Rev 2013; 8: CD006575. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Taplin J, McConigley R. Advanced life support (ALS) instructors experience of ALS education in Western Australia: a qualitative exploratory research study. Nurse Edu Today 2015; 35: 556–561. [DOI] [PubMed] [Google Scholar]
- 14. Semeraro F, Frisoli A, Loconsole C, et al. Motion detection technology as a tool for cardiopulmonary resuscitation (CPR) quality training: a randomised crossover mannequin pilot study. Resuscitation 2013; 84: 501–507. [DOI] [PubMed] [Google Scholar]
- 15. Semeraro F, Frisoli A, Loconsole C, et al. A new Kinect-based system for the analysis of performances in cardiopulmonary resuscitation (CPR) training. Resuscitation 2012; 83: e20. [Google Scholar]
- 16. Alves D, Wallace M, Allegra J, et al. Prediction of survival from cardiopulmonary resuscitation by CPR instructors. Am J Emerg Med; 2004; 22: 331–333. [DOI] [PubMed] [Google Scholar]
- 17. Braun V, Clarke V. Using thematic analysis in psychology. Qual Res Psychol 2006; 3: 77–101. [Google Scholar]
- 18. McMahan RP. Exploring the effects of higher-fidelity display and interaction for virtual reality games. PhD, Virginia Polytechnic Institute and State University, Blacksburg, VA, 2011. [Google Scholar]
- 19. Brennan RT, Braslow A. Skill mastery in public CPR classes. Am J Emerg Med 1998; 16: 653–657. [DOI] [PubMed] [Google Scholar]
- 20. Isbye DL, Høiby P, Rasmussen MB, et al. Voice advisory manikin versus instructor facilitated training in cardiopulmonary resuscitation. Resuscitation 2008; 79: 73–81. [DOI] [PubMed] [Google Scholar]
- 21. Meaney PA, Sutton RM, Tsima B, et al. Training hospital providers in basic CPR skills in Botswana: acquisition, retention and impact of novel training techniques. Resuscitation 2012; 83: 1484–1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Botella C, Serrano B, Baños RM, et al. Virtual reality exposure-based therapy for the treatment of post-traumatic stress disorder: a review of its efficacy, the adequacy of the treatment protocol, and its acceptability. Neuropsychiatr Dis Treat 2015; 11: 2533–2545. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Neumar RW, Shuster M, Callaway CW, et al. Part 1: executive summary. 2015 American heart association guidelines update for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2015; 132: S315–S367. [DOI] [PubMed] [Google Scholar]
- 24. Semeraro F, Scapigliati A, Ristagno G, et al. Virtual reality for CPR training: how cool is that? Dedicated to the ‘next generation’. Resuscitation 2017; 121: e1–e2. [DOI] [PubMed] [Google Scholar]
- 25. Olson KE, O’Brien MA, Rogers WA, et al. Diffusion of technology: frequency of use for younger and older adults. Ageing Int 2011; 36: 123–145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. O’Connell B. A poor grade for E-learning. Workforce 2002; 81: 15. [Google Scholar]
- 27. McMahan RP, Herrera NS. AFFECT: altered-fidelity framework for enhancing cognition and training. Front ICT 2016; 3: 29. [Google Scholar]
- 28. Lateef F. Simulation-based learning: just like the real thing. J Emerg Trauma Shock 2010; 3: 348–352. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Woollard M, Whitfield R, Newcombe RG, et al. Optimal refresher training intervals for AED and CPR skills: a randomised controlled trial. Resuscitation 2006; 71: 237–247. [DOI] [PubMed] [Google Scholar]
- 30. Taylor DC, Hamdy H. Adult learning theories: implications for learning and teaching in medical education: AMEE guide no. 83. Med Teach 2013; 35: e1561–e1172. [DOI] [PubMed] [Google Scholar]
- 31. Schultheis MT, Rizzo AA. The application of virtual reality technology in rehabilitation. Rehabil Psychol 2001; 46: 296. [Google Scholar]
- 32. Psotka J. Immersive training systems: virtual reality and education and training. Instr Sci 1995; 23: 405–431. [Google Scholar]
- 33. Niles DE, Nishisaki A, Sutton RM, et al. Improved retention of chest compression psychomotor skills with brief ‘Rolling Refresher’ training. Simul Healthc 2017; 12: 213–219. [DOI] [PubMed] [Google Scholar]
- 34. Bhanji F, Mancini ME, Sinz E, et al. Part 16: Education, implementation, and teams: 2010 American Heart Association guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. Circulation 2010; 122: S920–S933. [DOI] [PubMed] [Google Scholar]
- 35. Soar J, Mancini ME, Bhanji F, et al. Part 12: education, implementation, and teams: 2010 international consensus on cardiopulmonary resuscitation and emergency cardiovascular care science with treatment recommendations. Resuscitation 2010; 81(Suppl. 1): e288–330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36. Mancini ME, Soar J, Bhanji F, et al. Part 12: education, implementation, and teams. Circulation 2010; 122: S539–S581. [DOI] [PubMed] [Google Scholar]
- 37. Weaver FJ, Ramirez AG, Dorfman SB, et al. Trainees’; retention of cardiopulmonary resuscitation: how quickly they forget. JAMA 1979; 241: 901–903. [PubMed] [Google Scholar]
- 38. Park GJ, Song KJ, Shin SD, et al. Timely bystander CPR improves outcomes despite longer EMS times. Am J Emerg Med 2017; 35: 1049–1055. [DOI] [PubMed] [Google Scholar]
- 39. Rajan S, Wissenberg M, Folke F, et al. Association of bystander cardiopulmonary resuscitation and survival according to ambulance response times after out-of-hospital cardiac arrest. Circulation 2016; 134: 2095–2104. [DOI] [PubMed] [Google Scholar]
- 40. Abella BS, Alvarado JP, Myklebust H, et al. Quality of cardiopulmonary resuscitation during in-hospital cardiac arrest. JAMA 2005; 293: 305–310. [DOI] [PubMed] [Google Scholar]
- 41. Van Hoeyweghen RJ, Bossaert LL, Mullie A, et al. Quality and efficiency of bystander CPR. Belgian cerebral resuscitation study group. Resuscitation 1993; 26: 47–52. [DOI] [PubMed] [Google Scholar]
- 42. Gallagher EJ, Lombardi G, Gennis P. Effectiveness of bystander cardiopulmonary resuscitation and survival following out-of-hospital cardiac arrest. JAMA 1995; 274: 1922–1925. [PubMed] [Google Scholar]
- 43. Pintrich PR, Schrauben B. Students’ motivational beliefs and their cognitive engagement in classroom academic tasks. Stud Percept Classr 1992; 7: 149–183. [Google Scholar]
- 44. Dracup K, Doering LV, Moser DK, et al. Retention and use of cardiopulmonary resuscitation skills in parents of infants at risk for cardiopulmonary arrest. Pediatr Nurs 1998; 24: 219–225. [PubMed] [Google Scholar]
- 45. Mäkinen M, Niemi-Murola L, Ponzer S, et al. Healthcare professionals hesitate to perform CPR for fear of harming the patient. Resuscitation 2014; 85: e181–e112. [DOI] [PubMed] [Google Scholar]
- 46. Koster RW, Baubin MA, Bossaert LL, et al. European resuscitation council guidelines for resuscitation 2010 section 2. Adult basic life support and use of automated external defibrillators. Resuscitation 2010; 81: 1277–1292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47. Glenberg AM, Schroeder JL, Robertson DA. Averting the gaze disengages the environment and facilitates remembering. Mem Cognit 1998; 26: 651–658. [DOI] [PubMed] [Google Scholar]
- 48. Rasul S, Bukhsh Q. A study of factors affecting students’ performance in examination at university level. Procedia – Soc Behav Sci 2011; 15: 2042–2047. [Google Scholar]
- 49. Abella BS, Sandbo N, Vassilatos P, et al. Chest compression rates during cardiopulmonary resuscitation are suboptimal: a prospective study during in-hospital cardiac arrest. Circulation 2005; 111: 428–434. [DOI] [PubMed] [Google Scholar]
- 50. Sayre MR, Berg RA, Cave DM, et al. Hands-only (compression-only) cardiopulmonary resuscitation: a call to action for bystander response to adults who experience out-of-hospital sudden cardiac arrest: a science advisory for the public from the American Heart Association Emergency Cardiovascular Care Committee. Circulation 2008; 117: 2162–2167. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, Raw_Data_(2) for Clinical instructors’ perceptions of virtual reality in health professionals’ cardiopulmonary resuscitation education by Marie Ann Mae En Wong, Shien Chue, Michelle Jong, Ho Wye Kei Benny and Nabil Zary in SAGE Open Medicine