In recent years, different classifications of muscle injury have been proposed based on topographic location within the bone-tendon-muscle chain.1,3,4,7 Furthermore, because the degree and level of extracellular matrix (ECM) involvement might vary greatly, we propose to include histoarchitectural considerations in the gross anatomic description of muscle injuries.
Anatomic Description of Muscle Injuries
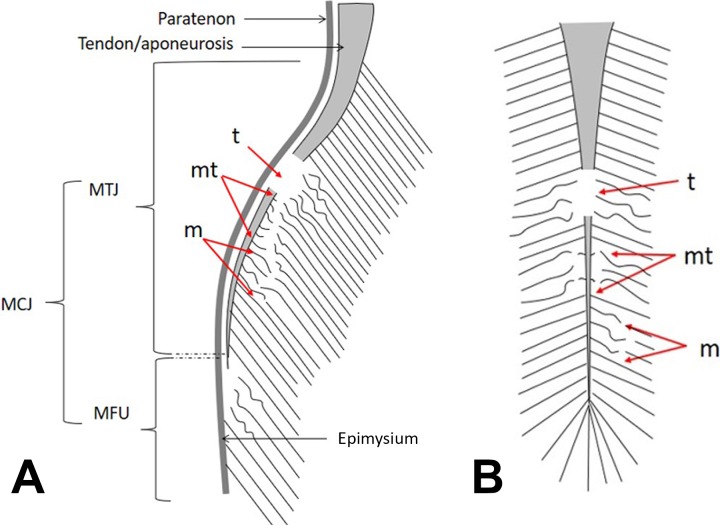
Most muscle injuries occur at the myoconnective junction (MCJ), which plays both a mechanical and a structural role within the muscle organ. MCJ lesions can occur in 2 different muscle histological structures: the musculotendinous junction (MTJ) and the myofascial unit (MFU) (Figure 1).
Figure 1.
(A) Peripheral myoconnective junction (MCJ) injury. (B) Internal or central MCJ injuries. m, muscular; MFU, myofascial union; mt, musculotendinous; MTJ, musculotendinous junction; t, tendinous.
The MTJ corresponds to the interface of muscle-tendon and aponeurosis and is the most frequently affected structure. The MTJ contributes mainly to the transmission of force instead of providing structural muscle framing, so that injuries in this area lead to a greater degree of disability than those in other areas.
The MFU is adjacent to the MTJ. The MFU has greater functional implications in contributing to overall muscle structural framing than to mechanical force transmission. Thus, the term unit instead of junction better reflects the fact that the cytoskeleton of the muscle fiber is linked to the proteins of the ECM through its sarcolemma all along its length.2
However, these 2 components of the MCJ cannot be understood as independent elements because they are a continuum of different types of connective tissue and the related muscle fibers. The transition between one and the other can be clearly identified in gross anatomy. The MTJ is composed of dense, regular connective tissue, which macroscopically has a fibrous and whitish aspect. In contrast, the MFU is composed of irregular and/or loose connective tissue; thus, macroscopically the MFU appears as a translucent to transparent layer. However, from a clinical and imaging perspective, it is sometimes complicated to define whether the injured area corresponds to the MTJ or MFU. Thus, we agree that the injury is located at the MTJ when the connective tissue component injured is identified through magnetic resonance imaging as a dark line on T2; if no line can be seen, the injury is then placed at the MFU. Examples of MTJ and MFU injuries are hamstring injuries and some of the proximal peripheral injuries of the rectus femoris, respectively.
Another important consideration for MCJ injuries is that they can be found at 2 levels in relation to the muscle belly: peripheral MCJ injuries (Figure 1A), usually occurring in unipennate muscles, and internal or central MCJ injuries (Figure 1B), usually occurring in bipennate muscles. These injuries are classically known as central tendon injuries and are typical of the rectus femoris muscle.
Histoarchitectural Description of Muscle Injuries
All injuries at any MCJ, including both peripheral and central MCJs, affect muscle fibers and their surrounding ECM. However, ECM characteristics vary depending on the histoarchitectural level affected (Figure 2). This fact has an important clinical implication, because it directly influences specific aspects of tissue repair and therefore return to play and risk of reinjury.5,6 Depending at which specific level the ECM is affected, injuries can be described as tendon, musculotendinous, or muscular ECM injuries.
Figure 2.
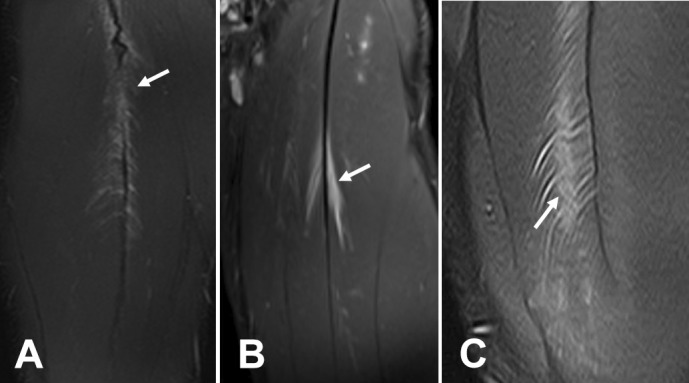
Central myoconnective junction injury of the rectus femoris. Proton density fat saturation sequence axial and coronal magnetic resonance study. (A) Tendinous defect in the central tendon (arrow) and surrounding small edema. (B) Musculotendinous injury (arrow) with intact central tendon and surrounding buildup of liquid and edema. (C) Small muscular defect (arrow) and edema located 1 cm from the septum with loss of tension and tendon displacement in the opposite direction of the rupture.
Tendon ECM injuries are characterized by a significant destruction of the tendon ECM (t in Figure 1), resulting in a clear gap as shown by imaging techniques. This type of injury occurs at the MTJ and must be distinguished from that known as a “free tendon injury,” where the injury is purely tendinous and does not affect the MTJ or even the MCJ itself.
Musculotendinous ECM injuries are characterized by a lesser involvement of the tendon ECM at the MTJ that may or may not result in a focal tendon thinning but with no evident tendinous gap when observed by imaging techniques. The involvement of the ECM mainly concerns the perimysium when it converges into the tendon. The torn muscle fibers are partially separated from their surrounding ECM, with a portion of the muscle fiber still anchored to the tendon-aponeurosis (mt in Figure 1) while the other is retracted toward the opposite direction.
Muscular ECM injuries occur farther from the MCJ and are classically referred to as intramuscular injuries (m in Figure 1). They have less ECM involvement and exclusively affect the MFU (perimysium and/or endomysium). The connective tissue affected in MFU detachment injuries cannot be directly detected with imaging methods.
Involvement of the histoarchitecture at the 3 levels mentioned can coexist in the same injury. Based on the amount of ECM affected and the specific histoarchitectural levels involved, the injury will entail a longer time for return to play with a higher probability of torpid evolution. Likewise, when the injury is intramuscular and imaging does not show an effect on the ECM, the prognosis of the injury will be better than for injuries that do affect the ECM.
Conclusion
Two injuries in the same macroscopic or gross anatomic topographical location and with the same treatment could evolve differently based on the type of specific microscopic or histoarchitectural ECM involvement. Thus, the amount of involvement of the ECM plays an important role in both prognosis and reinjury. Therefore, studying the anatomic and topographical location of the injury will help physicians make more specific and precise diagnoses for muscle injuries and allow for better understanding of some reinjury patterns.
Footnotes
The authors declared that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
References
- 1. Chan O, Del Buono A, Best TM, et al. Acute muscle strain injuries: a proposed new classification system. Knee Surg Sports Traumatol Arthrosc. 2012;20:2356–2362. [DOI] [PubMed] [Google Scholar]
- 2. Gumerson JD, Michele DE. The dystrophin-glycoprotein complex in the prevention of muscle damage. J Biomed Biotechnol. 2011;2011:210797. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Mueller-Wohlfahrt H-W, Haensel L, Mithoefer K, et al. Terminology and classification of muscle injuries in sport: the Munich consensus statement. Br J Sports Med. 2013;47:342–350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Pollock N, James SLJ, Lee JC, et al. British athletics muscle injury classification: a new grading system. Br J Sports Med. 2014;48:1347–1351. [DOI] [PubMed] [Google Scholar]
- 5. Pollock N, Patel A, Chakraverty J, et al. Time to return to full training is delayed and recurrence rate is higher in intratendinous (“c”) acute hamstring injury in elite track and field athletes: clinical application of the British Athletics Muscle Injury Classification. Br J Sports Med. 2016;50:305–310. [DOI] [PubMed] [Google Scholar]
- 6. Prakash A, Entwisle T, Schneider M, et al. Connective tissue injury in calf muscle tears and return to play: MRI correlation. Br J Sports Med. 2018;52(14):929–933. [DOI] [PubMed] [Google Scholar]
- 7. Valle X, Tol Alentorn-Geli E, et al. Muscle injuries in sports: a new evidence-informed and expert consensus-based classification with clinical application. Sports Med. 2017;47(7):1241–1253. [DOI] [PubMed] [Google Scholar]