Summary
To develop a targeted implementation strategy for a municipal health policy guideline, implementation targets of two guideline users [Regional Health Services (RHSs)] and guideline developers of leading national health institutes were made explicit. Therefore, characteristics of successful implementation of the guideline were identified. Differences and similarities in perceptions of these characteristics between RHSs and developers were explored. Separate concept mapping procedures were executed in two RHSs, one with representatives from partner local health organizations and municipalities, the second with RHS members only. A third map was conducted with the developers of the guideline. All mapping procedures followed the same design of generating statements up to interpretation of results with participants. Concept mapping, as a practical implementation tool, will be discussed in the context of international research literature on guideline implementation in public health. Guideline developers consider implementation successful when substantive components (health issues) of the guidelines, content are visible in local policy practice. RHSs, local organizations and municipalities view the implementation process itself within and between organizations as more relevant, and state that usability of the guideline for municipal policy and commitment by officials and municipal managers are critical targets for successful implementation. Between the RHSs, differences in implementation targets were smaller than between RHSs and guideline developers. For successful implementation, RHSs tend to focus on process targets while developers focus more on the thematic contents of the guideline. Implications of these different orientations for implementation strategies are dealt with in the discussion.
Keywords: policy and implementation, municipality, integrated health promotion, network analysis, evidence-based guidelines
INTRODUCTION
This study refers to guideline implementation in public health and focuses on characteristics for implementation (strategies) of a local health policy guideline in health service organizations. In the Netherlands, local authorities and Regional Health Services (RHSs) struggle with implementation of local health policy and research shows that guideline use lags behind (National Institute for Public Health and the Environment, 2008). Therefore, this study aims at developing building blocks for an implementation strategy of guidelines in public health practice. General research knowledge on diffusion and dissemination theories as well as specific research in implementation of policy instruments in health service organizations provide a basis for guideline implementation models.
The systematic review by Greenhalgh et al. (Greenhalgh et al., 2004), is considered a landmark in implementation research (Best and Holmes, 2010). Greenhalgh identified 13 research areas with relevant evidence for the diffusion of innovations in health service organizations, and distinguished two contrasting approaches: the ‘rational model’ and the ‘participatory model’ for implementation. According to Greenhalgh, early implementation studies, reflect a more rational approach, stressing the individual innovation and/or individual adopter as the most relevant unit of analysis, and are characterized mainly by a linear representation of the implementation process. Greenhalgh states that later studies, particularly in the area of health promotion research, show the emergence of a more radical ‘developmental’ agenda, in which a one-way transmission of advice from the change agency tot the target group has been replaced with various models of partnership and community development (Greenhalgh et al. 2004). These studies represent the participation model, using people’s and organizations’ needs and experiences in everyday practice as a starting point for dissemination of an innovation.
The so-called Blurring Boundaries model which was developed in Australian public health research and resulted from critical evaluation of current implementation perspectives (Knowledge Translation and Actor Network Theories) is an example that builds further on the participation model. This model facilitates shared decision making and shared priority setting through recognizing values of ‘the other' without denying differences of actors involved. Regarding knowledge translation, and in order to achieve conditions for effective connections between actors, the Blurring Boundaries model points at the necessity to find facilitators and appropriate actions that can serve integration of research, policy and practice, and that can also explain how and why the actions work (de Leeuw et al. 2007, 2008). Armstrong's research in knowledge translation strategies partly answers this question by developing the ‘KT4LG’ intervention (Knowledge Translation for Local Government), which includes group focus on relevance and priority of public health issues to bridge the evidence-practice gap (Armstrong et al, 2013).
Systematic reviews and evaluation of knowledge translation strategies in Canadian public health arrive at similar conclusions: to be effective, knowledge translation strategies in public health need more emphasis on identification of organizational factors to meet the needs of individual participants, organizations and knowledge providers (Dobbins et al., 2009; Dobbins and Traynor, 2015; LaRocca et al., 2012).
In guideline implementation literature wherein the emphasis is placed on the individual adopter, Fullan (Fullan, 2007) stresses taking into account theory and views or beliefs of practitioners who are intended to use the innovation (bottom-up). Available research from predominantly clinical settings shows that adherence to guidelines is associated with many factors, such as the users' outcome expectancies, knowledge and attitudes (Cabana et al., 1999; Paulussen et al., 2007), organizational and economic conditions (Damanpour, 1991; Weiner, 2009), administrative involvement (Watt et al., 2005), commitment of the parties involved (Grol and Grimshaw, 2003) and factors associated with the implementation process itself (Rogers, 2003; Grol et al., 2009; Forsner et al., 2010). In implementation research by Moulding (Moulding et al., 1999), besides emphasis on social and behavioral theories for exploring clinical implementation barriers at the individual level, we also find an argument for pre-implementation assessment of ‘views of groups and individuals outside the immediate hospital environment’ to define individual and organizational levels at which interventions for implementation should be targeted. These conclusions seem to indicate increasing relevance of the participation model in which network perspectives come into play. An overall feature in the theoretical perspectives of these authors includes the use of both bottom-up and top-down strategies in implementation processes, for which Matland's policy implementation theory laid the basis (Matland, 1995). Matland's insights contributed to the bottom-up versus top-down debate by conceiving the implementation process as influenced by local conditions such as resources, coalitions, activities and distribution of power (Kalkan, 2014).
Recent research shows an emergence of health policy guidelines at national and local levels in many high income countries. Although these guidelines contain recommendations for action, they are still ‘limited in their ability to organize and implement concrete bottom-up (i.e. local) action’ (Weiss et al., 2016). This study wants to contribute to the expressed need of developing practical approaches that can support local policy makers, researchers and practitioners in enhancing knowledge-based collaboration.
In the Netherlands, municipalities have a statutory role in protecting and promoting the health of their citizens (Dutch Public Health and Preventive Measures Act, 2003). Since 2003, based on the National Public Health Status and Forecast Report, the Dutch Ministry of Health has at national policy level given priority attention to the prevention of obesity, diabetes, alcohol abuse, smoking and depression (Ministry of Health, Welfare and Sport, 2003). Subsequently, the Ministry has encouraged local authorities to develop policies aimed at diminishing these health problems. As a regular Municipal Contractual, the RHS has a key role in providing advice and support to local authorities for developing their health policies. Since 2006, the Ministry has equipped municipalities and health services with guidelines to support the development and implementation of local health policies. Four guidelines, also incorporating recommended interventions to address obesity, alcohol abuse, smoking and depression were issued separately and were published sequentially in a period of 2 years.
As the Ministry of Health aims to ensure better alignment between national and local development of health policy, it calls on municipalities to acquire the national priorities of health issues in their local memorandum. The four guidelines were expected to contribute to the diffusion of this alignment. However, preliminary research indicated that they were insufficiently used by the municipalities, RHSs and health care providers (National Institute for Public Health and the Environment, 2008). In 2010, the four separate guidelines were merged into one guideline, the ‘Healthy Community Guideline’ (hereafter ‘guideline’) (National Institute for Public Health and the Environment, Centre for Healthy Living, 2010).To develop a targeted implementation strategy, implementation targets for the revised guideline need to be made explicit. Therefore, this study aims to identify specific goals for improving local implementation of the guideline in public health practice.
Guideline users' and developers' perspectives of implementation can be best explained by both individual and contextual factors. These contextual factors may refer to the professionals' own organization or to external organizations (Fleuren et al., 2010). Since the guideline contained no usage protocol nor clear end goals for its implementation (National Institute for Public Health and the Environment, Centre for Healthy Living, 2012), we presumed that among users and developers, divergent ideas could exist on implementation as intended. Subsequently, these particular targets would require different choices for the implementation strategy.
For this study, we consider concept mapping for exploring characteristics of successful implementation of policy guidelines consistent with current views, developments and demands in participative implementation research for public health policy. By this approach, we follow conclusions of research in effective dissemination approaches by Harris, who developed a dissemination framework in which tailoring approaches to individual organizations is considered a necessary phase. The implementation process ‘is organization-specific and involves a complex series of steps’ (Harris, 2012).
The international research provides an extensive amount of knowledge when it comes to barriers for clinical guideline implementation. Less has been written on guidelines for public health priority setting within a political-administrative context (Green, 2009; Kalkan, 2014) In addition to the aim of reaching common goals and shared understanding of successful guideline implementation, by focusing at potential differences in stakeholders'- and guideline developers' views, this study responds to the need for knowledge of specific tailoring strategies that fit within the structure and workflow of public health organizations aiming at local health policies (Glasgow et al., 2012). For guideline developers the results may provide clues and practical directions for incorporating effective dissemination instructions and tools for local implementation, of which recent research has noted the need of further investigation (Gagliardi and Brouwers 2012; Gagliardi et al., 2014; Weiss et al., 2016).
Therefore, this study aimed to answer the following questions:
What are the characteristics of successful implementation of the Healthy Community Guideline as perceived by professionals in RHS settings and guideline developers?
What are the similarities and differences in these characteristics between professionals in RHS settings and guideline developers?
METHODS
Concept mapping
Our main interest was to explore similarities and differences in perceived characteristics that play a significant role in the complex process of implementing the Healthy Community Guideline at the local level. To uncover these characteristics by two RHS user groups and guideline developers, and due to its participatory basis, we preferred to choose ‘concept mapping’ as research method in order to meet these specific demands (Bon-Martens et al., 2011). Concept mapping is a method by which groups jointly conceptualize a complex topic to serve as a framework to guide planning and evaluation. The concept mapping process ends up with an interpretable pictorial map of ideas and thoughts of involved participants. It is primarily a group process and so it is well-suited for situations where teams or groups of stakeholders have to work together.
The method as described by Trochim was used. This approach involves an inductive group process combined with deductive statistical analysis and consists of six steps: preparation (identification and inclusion of participants and defining the brainstorm focus), generating statements, structuring statements, graphical representation of statements on a map, the interpretation of the map and utilization in line with the initial question or focus (Trochim, 1989; Kane and Trochim, 2007) (presented in Table 1).
Table 1.
Composition of participant groups and involvement stages for concept mapping (CM)
| Study | Participants | 1. Preparation | 2. Generation of statements | 3. Structuring of statements | 4: Graphical Reproduction | 5: Interpretation |
|---|---|---|---|---|---|---|
| Conceptualizing characteristics of successful implementation of the Dutch guideline for municipal health policy (Healthy Community Guideline) | CM 1: Regional Public Health Service (RHS) policy officers (7); RHS project staff (3); RHS operational team managers (6); municipal policy officers (3); Mental Health/Substance Use policy officers and project staff (4); Homecare manager and dietician (2); Primary care policy advisors (2); sports consultant (2). | RHS 1 aimed to set implementation targets in their own policy, as well as in the policy of other stakeholders. External stakeholders were invited to participate. | In two separate brainstorming sessions, (12 and 17) participants produced 102 statements; 7 duplicate statements were removed by researchers and conductor. Final calculation with 95 statements. | Statements (on separate index cards) were sent by email to the participants for rating and sorting.Sorting and rating tasks were completed by 18 participants. (excluded 11 forms for incompleteness or absence)Errors were corrected through telephone contacts. | The researcher and project leader entered the statements in the PC. The point map and the cluster solutions were represented graphically, and were discussed by the researchers and the project leader. | The final concept map was discussed by the researchers and a subset of participants. Researchers added final labels to the concept maps' clusters and axes for interpretation. |
| CM 2: RHS manager/head of department (1); RHS policy officers (4); RHS epidemiologists (6); RHS project staff (4). | RHS 2 choose to invite their staff members only to set their own implementation targets. | In one brainstorming session, 15 participants produced 63 statements, 8 duplicates were removed. Final calculation with 55 statements. | In the same session all statements were rated and sorted by 15 participants individually. Errors were corrected on the spot. | The researcher and project leader entered the statements in the PC. The point map and cluster solutions were constructed by the researcher and four participants. | The final concept map was discussed by the researchers and all participants. Researchers added final labels to the concept maps' clusters and axes for interpretation. | |
| CM 3: Guideline developers: Representatives of National Health Institutes for obesity (2), alcohol (1), smoking (1), depression (1), consumer safety (1), sexual health (3), Dutch National Institute for Public Health and the Environment (2, including Head of Coordination for the guideline). | Guideline developers (authors) were invited as representatives of national priority health topics. | 6 Participants took part in the brainstorm session. 5 participants contributed to the list of statements by mail. The final calculation of the map was completed with 71 statements. | Statements (on separate index cards)were sent by email to the participants for rating and sorting.Sorting and rating tasks were completed by 11 participants. Errors were corrected by mail and through telephone contacts. | The researcher entered the statements in the PC. The researcher and project leader discussed the cluster solutions and labels with the project leader of Guideline developers. | The final concept map was discussed by the researcher and project leader with Guideline developers. Researchers added final labels to the concept maps' clusters and axes for interpretation. |
Participant groups and stages of concept mapping
In order to compare RHS perspectives among themselves and with those of guideline developers, three concept map procedures were done separately for two RHS user groups and the development group. In addition, separate results allowed the RHSs to define their own targets and subsequent strategies for a pilot implementation to be executed (beyond the reach of this study). Preferably, the brainstorming session in the concept mapping method is performed with a wide and diverse group of 10–20 participants (Trochim, 1989). A larger number can be involved in generating statements and subsequent stages of the process. This variety ensures the inclusion of many different viewpoints, helps to reach a shared understanding and can support broad adoption of the final conceptual framework. For all three concept map procedures, the participants were selected through purposive sampling (Boeije, 2006).
Prior to their participation in the concept map meetings, participants were informed that contributions included in the results would be made anonymous. Results would not be reducible to individuals or individual organizations. On the basis of these conditions and prior to the execution of the concept map meetings recorded on tape, participants agreed to take part and gave verbal informed consent to use the results in publications on the concept maps. This study was not subject to the Dutch Medical Research Involving Human Subjects Act and therefore medic ethical assessment was not compulsory. Table 1 shows the participants and all stages of concept mapping from preparation to interpretation.
In each concept map procedure, participants were asked to complete the following task in a brainstorm meeting: Formulate specific characteristics of successfully achieved implementation of the Healthy Community Guideline for municipal health.
At the start of all four brainstorming sessions, summarized information on the guidelines' content and on the rules for brainstorming was similarly provided to achieve a common mindset for the purpose of the meetings. During the process of generating statements, no discussion was allowed on the items' relevance, though questions to clarify and specify characteristics were encouraged.
Participants were asked to perform their structuring tasks individually. They rated the statements on a five-point Likert scale by dividing the cards into five equal piles of increasing importance. Secondly, participants piled the statements into groups, based on their meaning or their content, and gave these groups covering labels. For each task, participants subsequently filled out the rating and sorting forms with the numbered statements.
For analyzing the data we used Ariadne software for concept mapping (Severens, 1995). The program uses the sorting data as input for a principal component analysis (PCA), which translates correlations between statements into coordinates in a multidimensional space. The first two dimensions (horizontal and vertical) of the PCA solution for each statement are projected onto a point map (Severens, 1995). Through cluster analysis, the program determines which statements belong together and form groups of statements on the map. Based on the ratings by participants, the software provides a mean rating to the statements as well as to the clusters. The program gives a default cluster solution of 18 clusters. By varying the number of clusters and checking the resulting statements by content in each cluster, a final number of clusters was chosen that still made sense for their conceptualization. This was done for each concept map by subset groups of three or four participants. Finally, the subset groups formulated labels that best described the content of the clusters, based on the statements. The researchers then ascribed the final cluster labels. The axes of the maps were qualitatively interpreted and labeled by the researchers.
RESULTS
Main characteristics of the three separate concept maps
The central objective of all three concept map procedures was to conceptualize the perceived characteristics of successful implementation of the Healthy Community Guideline. Table 2 represents the main outcomes of the three concept maps. The full list of statements and clusters for each concept map can be retrieved from the corresponding author.
Table 2.
Results on items, clusters and dimensions of three concept maps
| Map | Top three items and mean ratings | Number of clusters | Top three clusters and mean ratings (scale 3.25–3.50) |
|---|---|---|---|
| RHS 1a | (n = 95)
|
10 |
|
| RHS 2 | (n = 55)
|
13 |
|
| MDb | (n = 71)
|
12 |
|
Regional Health Services.
Guideline developers: representing National Health Institutes for obesity, alcohol, smoking, depression, consumer safety, sexual health, Dutch National Institute for Public Health and the Environment.
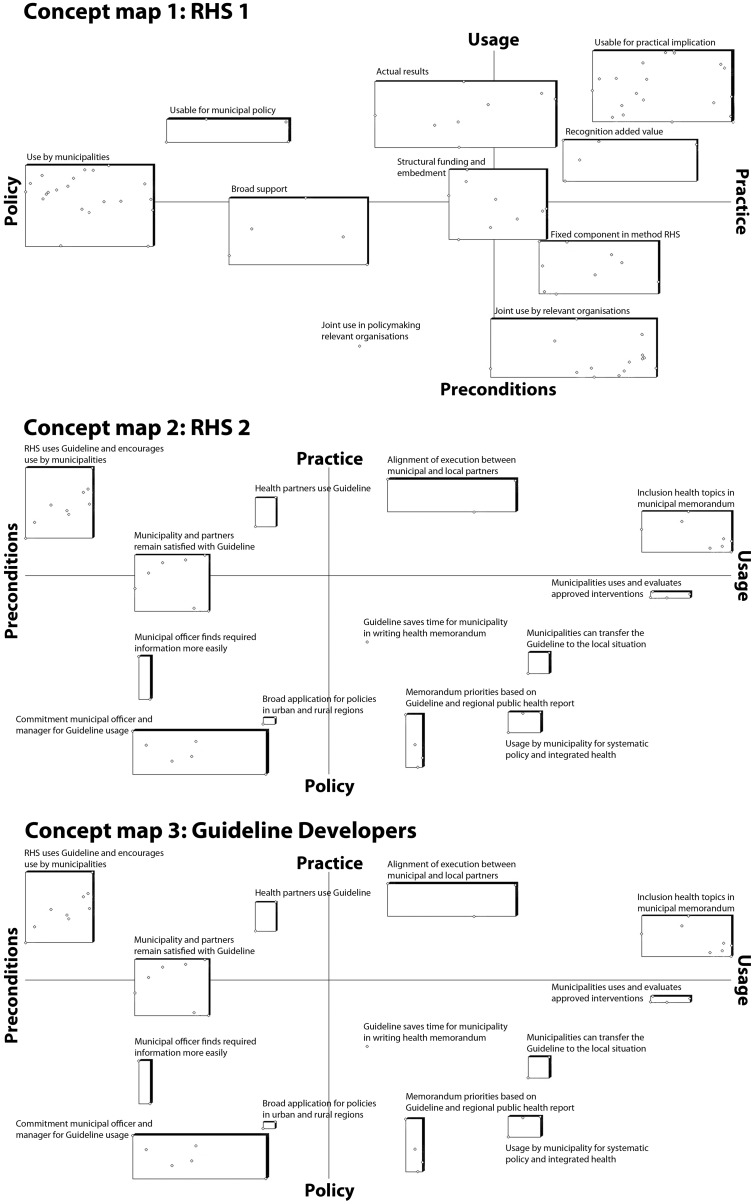
Concept map 1 (RHS 1) includes 95 statements of RHS members, municipal policy officers and local health organizations. This map shows highest ratings on the clusters ‘usability of the guideline for municipal policy’, ‘joint use in policymaking of relevant organizations’ and ‘usability for practical implementation’.
Concept map 2 (RHS 2) includes 55 statements. Here, RHS members ascribe the highest ratings to the clusters ‘commitment and use by municipal officer and manager’, ‘usage by municipalities for systematic policy and integrated health’ and ‘alignment of execution between municipalities and local partners’.
Concept map 3 (developers) includes 71 statements. Developers ascribe importance to the clusters ‘visibility of guideline components in local health policy and practice’, ‘increased local health policy performance by municipality and RHS’ and ‘contribution to an integrated approach and to local collaboration’.
The axes of both RHS maps are labeled as ‘application’, ranging from policy to practice and as ‘sustainability’, ranging from preconditions to usage. The horizontal axe of the developers' map is labeled as ‘sustainability’, ranging from preconditions to usage, while the vertical axe is labeled as ‘compliance’, ranging from process to content. This axe refers to the consistent use of the guideline at policy, management and practical levels of application, which should come as a result of national and local adoption of the guideline (Table 2, MD, items 1 and 3).
Differences and similarities between the three concept maps
For the two RHS maps, the top three clusters are quite similar, which suggests substantial agreement between participants on the most important characteristics of ‘joint use’ and ‘usability’ of the guideline for municipality and partner organizations. However, in concept map 1, the self-evident use of the guideline is ascribed to the RHS professional (Table 2, RHS1, item 3). In concept map 2, participants see the guideline as a tool that should be used proactively by municipalities, and should be supported by RHS professionals (Table 2, RHS2, items 1 and 2).
While concept map 1 considers joint use and practical applicability of the guideline within the network of public health partners as the highest ranked features (Table 2, RHS 1 clusters 1 and 2), in concept map 2, commitment and usage of the guideline by municipalities would prove implementation success. In concept map 3 (developers), successful implementation is perceived in terms of visible outcomes as a result of the guidelines' thematic content use on an executive level, such as appointing a specific health issue in the local memorandum (Table 2, MD, items 2 and 3, cluster 1).
In comparison with developers, the RHS maps mention the importance of alignment processes and control issues between local authorities and RHS organizations. Though all three maps agree on relevance of collaboration between local public health partners, the RHS maps show elements of process and relations more explicitly and consider these as important elements for successful implementation of the guideline.
Although the horizontal and vertical axe labels of the RHS concept maps have different positions, their cluster labels appear to have a high resemblance (Figure 1). The difference lies in their highest rated clusters, which is ‘usage in policy’ in RHS 1, and ‘preconditions in policy’ in RHS 2. The horizontal axe of the developers’ map corresponds with the axes of ‘sustainability’ of the RHSs. The developers' emphasis on ‘compliance’ with regard to the guideline in the vertical axe deviates from the RHS axes of ‘application’. The thickness of the cluster lines represents the clusters' rating.
Fig. 1:
Separate concept maps of two Regional Health Services and Guideline developers.
DISCUSSION
Characteristics of successfully achieved implementation for RHSs and guideline developers
This study aimed to detect perceived characteristics for successful implementation of a local health policy guideline. We found that these characteristics were dependent on the context of separate RHS organizations and differed from guideline developers' perspectives. The different outcomes of the concept maps lead to different emphases for implementation strategies.
The RHSs' orientations on alignment processes and control issues between local authorities and RHSs indicate that collaborative relationships are highly valued and understood as essential for implementation success. Presumably, RHS experiences with practical collaboration issues, such as dealing with conflicting interests between political and health advocates, will affect the prioritization of characteristics by RHSs. These orientations correspond to contemporary assumptions of ‘integrated or interactive knowledge translation’ in Dutch public health networks (Jansen et al., 2012), as well as to international research findings we mentioned earlier (de Leeuw et al., 2008). At the local level, guideline dissemination has to involve political administrative actors, medical-, social- and citizens organizations. Therefore, to be effective implementation strategies have to account for actors' preferences and behavior, in order to identify suitable approaches for acceptance and use of innovations.
The developers' orientation on clear cut attention to health issues in municipal health policy memoranda seems to result from their commitment to institutional health-promoting goals for these health issues. Generally, developers are further away from processes of local collaboration.
Similarities and differences between RHS perspectives
The two RHS respondent groups involved in the concept mapping were not alike. This difference in compositions could have caused the differential appraisal of characteristics of successful implementation. However, in spite of the involvement of partner organizations and municipalities in the brainstorming sessions of RHS 1, these differences in results with RHS 2 were small. The characteristics as described by the two RHS's show strong resemblance in terms of mutual use and strengthening cooperation and coordination with other public health partners. One of the guidelines' fundamental premises, ‘integrated health policy’, seems to be appraised equally among all parties, including guideline developers. On the other hand, different emphases occur between the RHSs on targets for internal implementation. While RHS 1 shows a strong orientation on internal use of the guideline as the professional standard, RHS 2 considers advising municipalities to use the guideline as a priority manifestation of implementation success. This high rating on municipal commitment seems to indicate a high acceptance in RHS 2 toward the guideline, for policy advisors implicitly acknowledge its relevance as a health policy instrument for municipalities. In RHS 1, guideline acceptance is also rated as a priority, considering implementation targets of cluster 4 (fixed component in methods of RHS) and top 3-item 3 (RHS policy advisors use the guideline naturally).
RHS 1 stresses practical applicability of the guideline for RHS members, whereas RHS 2 primarily stressed the RHS advisory skills to support the use of the guideline by municipal policy officers. These different perspectives might be ascribed to different task orientations regarding municipal advisory in which RHS 1 seems to stress executive health promotion tasks and RHS 2 to policy advisory tasks. Different emphasis on executive or advisory skills appears to be relevant for determining customized implementation targets in the separate RHS organizations.
Similarities and differences between RHSs' and developers' perspectives
As RHSs, guideline developers perceive ‘local collaboration’ as an important indicator for implementation success. But above all, they point to the visibility of substantial elements of the guideline in local health policy. The developers' concept map does not address the process of the guidelines' implementation within the RHS organization and their interaction with municipalities. In contrast, the involved RHSs stress the presence of these process elements at all desired levels of their organization as important manifestations of implementation success.
Methodological considerations
The concept mapping process generally allows to represent all perspectives of relevant stakeholders in one map, which can create a broad sense of shared ownership and commitment with the final results of the map. However, we deliberately chose to compare perspectives of three separate concept maps to uncover differences in perceived characteristics of successful implementation between guideline developers and RHSs. Moreover, the RHS concept maps were meant as first step to develop tailored implementation strategies for the RHSs (beyond the scope of this study). The number of participants chosen by RHS 2 was limited and did not include external partners or municipalities. This brings us to methodological issues when it comes to internal and external validity of the concept map results.
Since the RHSs aimed for participant diversity, the concept mapping groups were formed using purposive sampling. This targeted sample ensured participant diversity of public health partners in RHS 1, and variety of disciplines in RHS 2, which is an important requirement for the concept mapping procedure (Trochim 1989, Kane and Trochim, 2007). Sampling for proportionality was therefore not the RHSs', nor the researchers' primary concern. The main objective was to find specific characteristics for tailoring an implementation strategy that could fit the contextual circumstances. This may have affected the outcomes, in a way that different definitions of successful implementation (between the 2 RHSs) would lead to different characteristics. In terms of research aimed at generic factors, this is a weakness. In terms of directions for customized implementation strategies, using targeted sampling can be a strength. It is clear that when successful implementation is defined differently, one will find other characteristics. Repeated concept maps could lead to more insight into both specific factors, and generic factors for implementation of the guideline.
We considered willingness to implement the guideline preconditional for participation in the concept mapping process. From this point, we wanted to observe how basic circumstances in both RHSs could lead to different choices in preparation and in the actual implementation of the guideline. Therefore, the concept mapping participants were determined in consultation with those responsible for implementation.
Each RHS wanted a support base within a specific group of stakeholders. RHS 1 invited external representatives next to its own staff members to gain their approval to work with the guideline, and to gain wider support for determining their own implementation targets. RHS 2 preferred to conduct a concept map with only participants of their own organization. To reach diversity of perspectives among participants of the concept maps, the selection of participants through purposive sampling ensured a spread representation of RHS disciplinary levels (management, policy officers, executive health promoters) in both RHSs. For the separate RHS purposes, to guide their own tailored and targeted implementation strategy, and with their own specific selection of stakeholders, internal validity of the concept maps is provided. However, due to RHSs' specific choices of stakeholders, external validity is not sufficiently provided, for the results are mainly useful for the specific local public health practices and have limited generalizability. Nevertheless, the RHS concept maps suggest external validity to some degree, since their different selections of participants still showed the same items. This indicates a possibility of tracing generic elements when the procedure would be repeated in another RHS context. In order to retrieve generic constituents, similar concept maps could be repeated and conducted with other RHSs, municipal representatives and similar stakeholders.
In a comparable study in a RHS context, Van Bon-Martens et al. (Van Bon-Martens et al., 2014) suggest that external validity of a concept map for theory development in evidence-based public health can be increased if concept maps on the same topic are held several times in several groups of stakeholders or regions. Different stakeholders (professionals, researchers, policy makers) crossing disciplinary borders, will add new statements and thereby contribute to the enrichment of the existing scientific evidence by adding new knowledge from theory and practice.
The three separate concept maps allowed us to compare RHSs' and developers' perspectives independently, since their generation phases of statements went along separate lines. There are differences in which the successive steps were completed in time between the three concept map procedures. Regarding the 4 hour session of RHS 2, participant burn out could be marked as limiting comparability of the maps. However, the generating phase took place at the start of each session and provided the separate statements in which the most important differences occurred. As intended, the comparison provided a better insight into characteristics of successfully achieved implementation as perceived by RHSs (users) and developers of the guideline. In this respect, the concept map method answered the initial research question of exploring similarities and differences in perceived characteristics. Therefore, a fair conclusion seems that concept mapping, when its outcome is based on local ownership of relevant stakeholders, can contribute to formulate targets for tailored implementation strategies by setting shared goals for a specific user group. Our choice for studying implementation goals in silos was motivated by deliberately giving space to possible differences. If the concept maps were conducted in mixed groups, specific context related characteristics might have been harder to detect. A concept map in a mixed group would have yielded more generic implementation characteristics for a shared conceptual framework among developers and user-groups. However, the concept maps were also used for their practical relevance, as a first step in the implementation process of the guideline. An important result of the individual concept maps was the recognition of the implementation characteristics for those who were directly involved.
From the perspectives of local ownership and direct involvement of relevant stakeholders, concepts based on actor network theory (ANT, as mentioned in the Introduction section) might provide a useful alternative in our search for implementation characteristics. ANT can be defined as a research method with a focus on the connections between both human and non-human entities (Dankert, 2015). In the ANT, the process of (knowledge) translation is explained as the structuring of reality, based on actors (people/organizations/things) and their interactions (Callon, 1986). The ANT focuses on how interactions of different actors arise and on the effects of these interactions. These interactions can be displayed in a network, in order to reconstruct who contacts who, who (or what) has influence and which actors are involved in the implementation of a best practice. As long as the players continue to see the value or necessity, the network endures and leads to results. Translation is the process in which actors re-interpret the mission and values of an improvement project and therefore play a key role in the development of working practices within an improvement theme, in this case the implementation of a guideline for local health policy (Maaijen and Stoopendaal, 2013).
Relevance of the results for implementation of the guideline in practice
The results of the concept maps can be discussed within RHSs in order to explicate expectations about their own implementation efforts. In the involved RHSs, these expectations might result from different task orientations regarding municipal advisory. To support the implementation, guideline developers could provide municipalities and RHSs with tools and sufficient indicators for monitoring progress in the implementation process. One might think of concrete methods for alignment of RHS goals with different municipal sectorial policies. Since RHS1 stresses the use of the guideline as a professional standard, for guideline developers, this would require in-depth understanding of RHS organizational structures concerning internal alignment issues between management and professional executives. For RHS 2, the guideline could provide indicators for monitoring progress in advisory methods that encourage guideline use by municipalities.
As mentioned by Gagliardi (Gagliardi and Brouwers, 2012), integration of guideline development and applicability information could strengthen implementation, for example by involving different types of experts (guideline users) in the guideline development and implementation processes. Involvement of practice can lead to inclusion of directions or tools for implementability in guidelines.
CONCLUSION
Results of the concept maps show different orientations about successfully achieved implementation by participants from two RHSs and guideline developers. These differences are assumed to originate from participants' various reasons for the use of the instrument. In developing a strategy for adoption of the guideline by different user groups, the question, ‘What's in it for me?’, needs to be met more specifically for several organizations and employees. The results of a concept map indicate possible targets for supporting adoption and implementation processes within organizations by developing additional practical implementation tools, including methods of tracing users' individual purpose of use. Without the concept maps, the different characteristics had not been found. An implementation strategy aiming at internal adoption of the guideline by RHS professionals and managers would be appropriate for one organization (in this case, RHS 1), but would be a blunder for another.
With regard to the two main questions of this study, the concept map method was suitable for improved understanding of perceived characteristics of implementation success by RHSs and developers. A key observation from this study is the discrepancy between what is considered crucial for implementation among guideline developers (actual visibility of guidelines' thematic content) and what targeted users intend to do with the guideline, which is to align policy processes between RHS, partners, and municipalities. Attention to these policy processes seems particularly important for the distribution of the guidelines' content. Policy processes, as we understand from Greenhalgh, rarely follow a linear development and can be characterized as incremental processes, due to their participatory nature and contextual conditions that tend to challenge guideline implementation efforts. When developing the guideline, developers should take into account application purposes of different users that pursue different implementation goals. Subsequently, the provision of implementation strategies should be tailored to these differences. The developers' awareness of differences and similarities in implementation goals in practice can be achieved through improved dialogue between guideline developers and intended users, in this case, the RHSs. The purpose of the concept maps in this study was to contextualize the implementation processes by revealing different policy contexts and by showing directions for tailoring the processes. The individual RHS organizations have an important role in this process, because tailoring implementation from within the organization finds an immediate shape. Although the concept maps of both RHSs show different results, and do not reach a generic implementation strategy, their own emphasis on the individual policy context seems functional and important for implementation.
In conclusion, the concept map results concerning the various perceived characteristics of successful implementation lead to an important recommendation for public health practice. In order to reach better guidance and support base for an implementation strategy, every time and in each organizational setting all relevant stakeholders should jointly explicit their implementation goals. To uncover different user groups' and developers' latent expectations and implementation goals, methods to achieve this explicit formulation, e.g. concept mapping, could be added to the guideline. In guideline implementation research, evidence in the development and use of applicability information is still not extensive and most developers who disseminated guidelines online and in scientific journals lack the resources for developing targeted implementation activities (Gagliardi and Brouwers, 2012; Gagliardi et al., 2014). From our results, we found that concept mapping could serve as a specific, and feasible tool for enhancing implementability of guidelines and for facilitating integration of research, policy and practice. However, there are other tools for this purpose. With regard to concept mapping, further studies would yet have to test the supposed benefits of this method for adequate knowledge translation in public health policy development. Examining the significance of ‘diversity’ in definitions of successful implementation among intended users of policy guidelines, could contribute to developing better tailoring tools for knowledge-based action in local public health.
AUTHORS’ CONTRIBUTIONS
T.J.M.K. contributed to the design, execution and data analyses of the study and wrote the manuscript. M.J.H.v.B.-M. also contributed to the design, data collection and analyses. I.A.M.v.d.G. and H.A.M.v.O. contributed to the analysis and T.G.W.M.P., I.A.M.v.d.G., M.J.H.v.B.-M., and H.A.M.v.O. revised and commented on the manuscript. All authors read and approved the final manuscript.
ACKNOWLEDGMENTS
We thank all participants from Regional Health Services, municipalities, local health organizations, representatives of national health institutes and the National Institute for Public Health and the Environment for their collaboration and contributions to the concept maps. We thank Regional Health Service GGD Hart voor Brabant for providing the necessary conditions to carry out the research project. We thank the Netherlands Organization for Health Research and Development (ZonMw) for financially supporting this project. This study was not subject to the Dutch Medical Research Involving Human Subjects Act and therefore medic ethical assessment was not compulsory.
Funding
This work was supported by a grant from the Netherlands Organization for Health Research and Development (ZonMw, grant number 201000001).
REFERENCES
- Armstrong R., Waters E., Dobbins M., Anderson L., Moore L., Petticrew M.. et al. (2013) Knowledge translation strategies to improve the use of evidence in public health decision making in local government: intervention design and implementation plan. Implementation Science, 8, 1.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Best A., Holmes B. (2010) Systems thinking, knowledge and action: towards better models and methods. Evidence & Policy: A Journal of Research, Debate and Practice, 6, 145–159. [Google Scholar]
- Boeije H. (2006) Analyseren in kwalitatief onderzoek. (Analysis of Qualitative Research). Boom onderwijs.
- Bon-Martens V. M., Van de Goor L., Holsappel J., Kuunders T., Jacobs-van der Bruggen M., Brake T.. et al. (2014) Concept mapping as a promising method to bring practice into science. Public Health, 128, 504–514. [DOI] [PubMed] [Google Scholar]
- Bon-Martens V. M., Achterberg P., Van de Goor L., Oers H. V. (2011) Towards quality criteria for regional public health reporting: concept mapping with Dutch experts. European Journal of Public Health, 22, 337–342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cabana M., Rand C., Powe N., Wu A., Wilson M., Abboud P. A.. et al. (1999) Why don't physicians follow clinical practice guidelines? A framework for improvement. Journal of the American Medical Association, 282, 1458–1465. [DOI] [PubMed] [Google Scholar]
- Callon M. (1986). Some elements of a sociology of translation: domestication of the scallops and the fishermen of St. Brieuc Bay In Law J. E. (ed.), Power, Action, and Belief: A New Sociology of Knowledge. Routledge, London. [Google Scholar]
- Dankert R. (2015). Using Actor-Network Theory (ANT) doing research. http://ritskedankert.nl/using-actor-network-theory-ant-doing-research/ (last accessed 13 July 2016).
- Damanpour F. (1991) Organizational innovation: a meta-analysis of effects of determinants and moderators. The Academy of Management Journal, 34, 555–590. [Google Scholar]
- Dobbins M., Hanna S. E., Ciliska D., Manske S., Cameron R., Mercer S. L.. et al. (2009) A randomized controlled trial evaluating the impact of knowledge translation and exchange strategies. Implementation Science, 4, 1.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dobbins M., Traynor R. (2015) Engaging public health decision makers in partnership research. Implementation Science, 10, 1.25567289 [Google Scholar]
- Dutch Public Health and Preventive Measures Act. (2003). (Wet Publieke Gezondheid, WPG).
- Fleuren M., Wiefferink K., Paulussen T. (2010) Checklist for determinants of innovations in health care organizations. (Checklist determinanten van innovaties in gezondheidszorgorganisaties). Tijdschrift Voor Gezondheidswetenschappen (Journal of Health Sciences), 88, 51–54. [Google Scholar]
- Forsner T., Åberg Wistedt A., Brommels M., Janszky I., Ponce de Leon A., Forsell Y. (2010) Supported local implementation of clinical guidelines in psychiatry: a two-year follow-up. Implementation Science, 5, 4.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fullan M. (2007) The New Meaning of Educational Change, 4th edition Routledge, London, p. 11. [Google Scholar]
- Gagliardi A. R., Brouwers M. C. (2012) Integrating guideline development and implementation: analysis of guideline development manual instructions for generating implementation advice. Implementation Science, 7, 7.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gagliardi A. R., Brouwers M. C., Bhattacharyya O. K. (2014) A framework of the desirable features of guideline implementation tools (GItools): Delphi survey and assessment of GItools. Implementation Science, 9, 2.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glasgow, R. E., Vinson, C., Chambers, D., Khoury, M. J., Kaplan, R. M. and Hunter, C. (2012) National Institutes of Health approaches to dissemination and implementation science: current and future directions. American Journal of Public Health, 102, 1274–1281. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Greenhalgh T., Robert G., Macfarlane F., Bate P., Kyriakidou O. (2004) Diffusion of innovations in service organizations: systematic review and recommendations. Milbank Quarterly, 82, 581–629. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Grol R., Grimshaw J. (2003) From best evidence to best practice: effective implementation of change in patients’ care. Research into practice. The Lancet, 362, 1228–1229. [DOI] [PubMed] [Google Scholar]
- Grol R., Wensing M., Eccles M. (2009) Planning and executing an implementation process. In Improving Patient Care. The Implementation of Change in Clinical Practice, Elsevier, Edinburgh, Scotland, pp. 44–52.
- Harris, J. R. (2012) A framework for disseminating evidence-based health promotion practices. Preventing Chronic Disease, 9, 6–7. [PMC free article] [PubMed] [Google Scholar]
- Jansen M., De Leeuw E., Hoeijmakers M., De Vries N. (2012) Working at the nexus between public health policy, practice and research. Dynamics of knowledge sharing in the Netherlands. Health Research Policy and Systems, 10, 33. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kane, M. and Trochim, W. M. (2007) Concept mapping for planning and evaluation. Sage Publications, Thousand Oaks, CA, pp. 1–200. [Google Scholar]
- LaRocca R., Yost J., Dobbins M., Ciliska D., Butt M. (2012) The effectiveness of knowledge translation strategies used in public health: a systematic review. BMC Public Health, 12, 751. [DOI] [PMC free article] [PubMed] [Google Scholar]
- De Leeuw E., McNess A., Stagnitti K., Crisp B. (2007). Acting at the Nexus: Integration of Research, Policy and Practice. Deakin University.
- De Leeuw E., McNess A., Crisp B., Stagnitti K. (2008). Theoretical reflections on the nexus between research, policy and practice. Critical Public Health, 18, 5–20.
- Maaijen M., Stoopendaal A. (2013) Actor Netwerk Theorie: een filosofie én een methode toegepast in onderzoek over best practices in de langdurige zorg. (Actor Network Theory: applying philosophy and a method in research for best practices in long-term care. KWALON. Tijdschrift Voor Kwalitatief Onderzoek in Nederland, 18, 35–42. [Google Scholar]
- Matland, R. E. (1995) Synthesizing the implementation literature: The ambiguity-conflict model of policy implementation. Journal of Public Administration Research and Theory, 5, 145–174.
- Ministry of Health, Welfare and Sport. (2003) Longer healthy living 2004-2007. A matter of healthy behavior (VWS, Langer gezond leven. Ook een kwestie van gezond gedrag) The Hague.
- Moulding N., Silagy C., Weller D. (1999) A framework for effective management of change in clinical practice: dissemination and implementation of clinical practice guidelines. Quality in Health Care, 8, 177–183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- National Institute for Public Health and the Environment, Centre for Healthy Living (Rijks Instituut voor Volksgezondheid en Milieu, RIVM. (2010) Healthy Community Guideline, revised edition (Handreiking Gezonde Gemeente), Bilthoven.
- National Institute for Public Health and the Environment (RIVM). (2008) Evaluation of local health guides (Evaluatie handleidingen lokaal gezondheidsbeleid), Bilthoven.
- National Institute for Public Health and the Environment, Centre for Healthy Living (RIVM). (2012) webpage Loketgezondleven.nl: ‘Working on an integrated policy: There is no fixed recipe for an integrated policy. The right approach depends on local options.’ Bilthoven. https://www.loketgezondleven.nl/gezonde-gemeente/gezondheidsbeleid-maken/integraal-beleid/ (last accessed 6 November, 2015).
- Paulussen T., Wiefferink K., Mesters I. (2007) Invoering van effectief gebleken interventies. (Introduction of proved effective interventions) In: Brug A., Lechner (eds), Gezondheidsvoorlichting en gedragsverandering (Health education and behavior change), Assen Van Gorcum, Assen, The Netherlands, pp. 16. [Google Scholar]
- Rogers E. M. (2003) Diffusion of Innovations, 5th edition.Free Press, New York. [Google Scholar]
- Severens P. (1995) Manual for Concept Mapping using Ariadne (Handboek Concept Mapping met Ariadne). Nederlands Centrum Geestelijke Volksgezondheid/Talcott BV Utrecht, pp. 5–6.
- Trochim W. (1989) An introduction to concept mapping for planning and evaluation. In Trochim, W. (ed.), A Special Issue of Evaluation and Program Planning, 12: 1–16.
- Watt S., Sword W., Krueger P. (2005) Implementation of a health care policy: an analysis of barriers and facilitators to practice change. BMC Health Services Research, 5, 53.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiner B. (2009) A theory of organizational readiness for change. Implementation Science, 4, 67.. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Weiss D., Lillefjell M., Magnus E. (2016) Facilitators for the development and implementation of health promoting policy and programs—a scoping review at the local community level. BMC Public Health, 16, 1.. [DOI] [PMC free article] [PubMed] [Google Scholar]