Abstract
Almost 2.8 million men in the U.S. are living with prostate cancer (PC), accounting for 40% of all male cancer survivors. Men diagnosed with prostate cancer may experience chronic and debilitating treatment side effects, including sexual and urinary dysfunction, pain and fatigue. Side effects can be stressful and can also lead to poor psychosocial functioning. Prior trials reveal that group-based cognitive behavioral stress and selfmanagement (CBSM) is effective in reducing stress and mitigating some of these symptoms, yet little is known about the effects of culturally-translated CBSM among Spanish-speaking men with PC. This manuscript describes the rationale and study design of a multi-site, randomized controlled trial to determine whether participation in a culturally adapted cognitive behavioral stress management (C-CBSM) intervention leads to significantly greater reductions in symptom burden and improvements in healthrelated quality of life relative to participation in a non-culturally adapted cognitive behavioral stress management (CBSM) intervention. Participants (N=260) will be Spanish-speaking Hispanic/Latino men randomized to the standard, non-culturally adapted CBSM intervention (e.g., cognitive behavioral strategies, stress management, and health maintenance) or the culturally adapted C-CBSM intervention (e.g., content adapted to be compatible with Hispanic/Latino cultural patterns and belief systems, meanings, values and social context) for 10 weeks. Primary outcomes (i.e., diseasespecific symptom burden and health-related quality of life) will be assessed across time. We hypothesize that a culturally adapted C-CBSM intervention will be more efficacious in reducing symptom burden and improving health-related quality of life among Hispanic/Latino men when compared to a non-culturally adapted CBSM intervention.
Keywords: Hispanic, symptom burden, health-related quality of life, cognitivebehavioral, stress, culture
Introduction
Almost 2.8 million men in the U.S. are living with prostate cancer (PC), and approximately 80% of PC cases are diagnosed as non-metastatic with a 5-year relative survival rate of 100%.1 Despite high survival, treatment side effects, including sexual and urinary dysfunction, pain and fatigue are common and chronic. 2–4 Side effects also lead to poor psychosocial functioning, including mood disturbance, impaired intimacy and social functioning, and concerns about body image and masculinity 5. As PC occurs primarily in men 65 or older, age-related stressors (e.g., loss of independence, caregiving burden & comorbidities), can exacerbate compromises in health-related quality of life (HRQoL) 6.
Psychosocial interventions have shown to reduce symptom burden and improve HRQoL in cancer survivors 7,8. Cognitive behavioral stress management (CBSM), a group-based psychosocial intervention based on cognitive behavioral therapy (CBT) and stress- and self-management principles, has been shown to reduce symptom burden (e.g., sexual & urinary dysfunction) and improve HRQoL among men diagnosed with PC 9,10. In breast cancer survivors, stress management interventions that improve psychosocial adjustment impact physiological mechanisms (e.g., inflammatory cytokines) show beneficial effects on physical symptoms (e.g., fatigue, pain), HRQoL and disease activity 11–13. This research has primarily focused on non-Hispanic/Latino Whites (NHWs) PC survivors, with limited consideration of the influence of Hispanic/Latino (Hispanics hereafter) cultural processes.
Hispanics treated for PC report worse HRQoL relative to NHWs, controlling for differences in socioeconomic and disease related factors 14,15. Hispanic cancer survivors report greater supportive needs, including the need for stress management, coping, and connecting with other patients 16. Despite these disparities, few evidencebased treatments (EBTs) target Hispanics or address cultural processes.
Evidence suggests that Hispanic culture may impact health 17. Family interdependence (familism) is associated with seeking medical care and healthy behaviors, but can also compromise HRQoL among Hispanics who prioritize family needs above their own. Fatalistic beliefs that one lacks control over health can also prevent Hispanics from engaging in healthy behaviors. Further, the need to maintain harmonious social interactions (simpatía) can inhibit assertive and proactive health communication and behaviors. Few studies have addressed these sociocultural processes in cancer survivors and their implications for EBTs. Culturally adapted CBT interventions for depression have demonstrated superior effects relative to standard treatment 18–20. However, the few adapted EBTs for cancer survivors have focused solely on a involved a linguistic adaptation, ignoring the need to tailor content compatible with Hispanic culture by addressing cultural patterns, behaviors, frames of reference/world view, and belief systems, therefore limiting potential of therapeutic gains 21,22. Culturally adapted CBT that considers Hispanic cultural patterns may more effectively enable participants to prioritize their health, enhance communication with their provider and family, and reduce fatalistic and stigmatized views about cancer. Although non-culturally adapted CBT provides the same stress and self-management skills as the culturally adapted CBT (e.g., coping skills, relaxation training, enhancing social support), delivery of these CBT skills considering Hispanic culture (e.g., culturally informed exercises, acknowledgement of cultural patterns such as family interdependence and fatalistic views, etc.) may facilitate greater uptake of CBT-based skills.
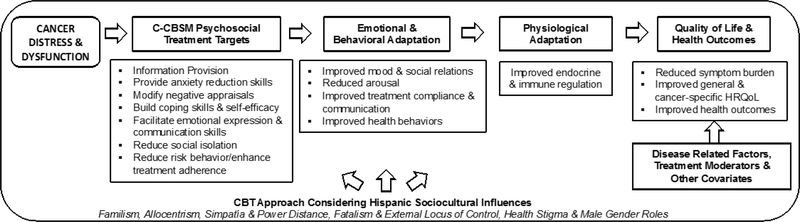
We describe a multi-site, randomized controlled behavioral clinical trial that evaluates CBT evidence-based skills grounded in the context of Hispanic sociocultural influences (Figure 1). The primary goal is to determine whether participation in the culturally adapted CBSM (C-CBSM) leads to significantly greater reductions in symptom burden relative to participation in the non-culturally adapted CBSM among Hispanics treated for localized PC with elevated symptom burden. A secondary goal is to determine whether C-CBSM related improvements in symptom burden and HRQoL are mediated by improvements in stress management, emotional adaptation, and the regulation of inflammation.
Figure 1.
C-CBSM evidence-based skills are grounded in the context of sociocultural influences. These sociocultural influences are addressed in CBT skills provision exercises, didactics, homework assignments ingroup discussions. A diagnosis of prostate cancer and treatment-related symptom burden may cause distress and ongoing poor physical function. Culturally adapted cognitive behavioral stress and self-management is designed to facilitate emotional, behavioral, and physiological adaptation. Favorable adaptation may improve quality of life and health outcomes.
Materials and Methods
Hypotheses
Relative to the CBSM intervention, we hypothesize that the C-CBSM intervention will demonstrate significantly greater reductions in symptom burden and improvements in HRQoL from baseline to post-intervention assessments over a one-year period. We also hypothesized that specific targets of C-CBSM (e.g., cognitive restructuring, communication & coping skills, relaxation) provided considering the context of Hispanic culture (e.g., family interdependence, fatalistic attitudes), and physiological adaptation (e.g., reduced inflammation) will mediate the effects of C-CBSM on lower symptom burden and higher HRQoL.
Study Design
The study design was informed by the CONSORT guidelines 23. This is a randomized controlled trial (RCT) with a 2×4 repeated measures design with group assignment (C-CBSM vs. CBSM) as the between-group factor, and time as the withingroup factor. Participants complete in-person assessments at baseline (T1), immediately after a 10-week intervention with maximum of 30 days post intervention (T2), and 6- and 12 -months after the intervention +/− 30 days (T3 and T4, respectively). Participants will be randomized 1:1 by cluster randomization into groups (C-CBSM or CBSM) with stratification by PC treatment type (~50% surgery & ~50% radiotherapy) across conditions at each respective study site. All participants will be asked to participate in 10-weekly 90-minute in-person group-based sessions targeting CBTbased skills for stress- and self-management in one of two experimental conditions— 1) a linguistically translated (Spanish) and culturally adapted cognitive behavioral stress and self-management condition (C-CBSM) or 2) a linguistically translated standard version of CBSM (CBSM). Following the baseline visit (T1), participants are randomly assigned into either the C-CBSM intervention or the CBSM intervention. The lengths of both our interventions are based on our prior work documenting the efficacy of 10-week group-based programs in improving multiple psychosocial, physiological, and health outcomes. These interventions span across multiple chronic diseases, including breast cancer, HIV, cardiovascular disease, localized and advanced PC (including bilingual and Spanish monolingual Hispanics) 7,9,10. All assessments will be administered to consented participants as an in-person interview and all data will be collected and stored in REDcap database. Study staff will also be blinded to the participant cohort for all assessments. Participants will receive $75 for each in person assessment and blood draw, up to a total of $300 for completing study procedures. Additionally, participants can be reimbursed for transportation to attend the weekly program sessions up to $50 per visit. Participants will also be informed that their group sessions will be audio and video-recorded if all participants consent to monitor intervention fidelity. All procedures and questionnaires have been approved by the Institutional Review Boards at Northwestern University, Rush University Medical Center, and the University of Miami.
Participants
We will enroll a total of 260 participants of diverse Hispanic backgrounds from the Robert H. Lurie Comprehensive Cancer Center at Northwestern Memorial Hospital and the Sylvester Comprehensive Cancer Center of the University of Miami. Participants will meet the following inclusion criteria: 1) self-identified Hispanic/Latino adults, 2) Spanish-speaking (including bilingual English-Spanish speakers), 3) primary diagnosis of localized prostate cancer (stages I to IIIA), 4) have completed surgical or radiation treatment within 4–36 months of study enrollment, and 5) self-reported moderate to severe erectile and/or urinary dysfunction (as assessed by the Expanded Prostate Cancer Index Composite upon screening). Participants will be excluded for 1) prior inpatient psychiatric treatment for severe mental illness and active suicidality; 2) active alcohol or substance dependence; 3) history of other non-skin cancer; 4) scores of > 3 on the Short Portable Mental Status Questionnaire; and 5) acute or chronic immune system medical conditions, medications or conditions that impact immune and endocrine function (e.g., CFS, Lupus, Hepatitis C, or immunosuppressive treatment requiring conditions). 24
Intervention Content and Format
Both C-CBSM and CBSM are delivered face-to-face in a group setting with 4–8 participants lasting 90 minutes/session. In the first 30 minutes, participants are taught/discuss a new anxiety/stress reduction technique whereas the latter 60 minutes focus on stress- and self-management. Disease course, symptom burden, communication with intimate partner and/or family members and health care provider, impact of stress on physical and mental health and symptoms, and management of symptom burden and decrements in HRQoL are used for educational purposes and as catalysts for CBSM techniques. Participants describe general and disease specific stressors with an emphasis on symptoms and interpersonal disruption. Didactics integrate materials that target skills to improve multiple domains of HRQoL by providing coping, social support, anger management and other skills. In-session role-plays are conducted to practice skills provided. Participants receive a participant workbook with all the relaxation and stress management didactics, homework, self-monitoring tools and exercises in order to facilitate implementation of skills learned in the CBSM sessions in their own “real world” settings outside of the intervention (See Table 1).
Table 1.
C-CBSM & CBSM Weekly Relaxation Exercises & CBT Topics
| Weekly Sessions | Relaxation Exercise | CBT Topic |
|---|---|---|
| Session 1 | Progressive Muscle Relaxation (PMR) | Introduction; Prostate Cancer & My Body |
| Session 2 | PMR 4 & Diaphragmatic Breathing (DB) | Stress Awareness & Impact of Stress |
| Session 3 | Deep Breathing, PMR & Imagery | Sex and Sexuality After Treatment |
| Session 4 | PMR 4 & Imagery | Cognitive Distortions |
| Session 5 | Deep Breathing & Healing Light | Cognitive Restructuring |
| Session 6 | Meditation | Coping I |
| Session 7 | Color Meditation | Coping II |
| Session 8 | Mindfulness Meditation | Emotional Expression |
| Session 9 | Mindfulness Meditation | Communication |
| Session 10 | Mindfulness Meditation | Social Support |
Table 1 Demonstrates the content discussed in the weekly group sessions.
Standard Cognitive Behavioral Stress and Self-Management (CBSM).
The standard CBSM intervention was developed to promote stress management, health maintenance and self-management by providing relaxation training and CBT-based strategies to improve symptom management, interpersonal adjustment, and HRQoL, and reduce arousal and negative mood in men treated for PC. This English language, non-culturally adapted CBSM underwent forward and backward translation by Action Translation Services headquartered in Miami, FL with internal verification. All content in CBSM is linked to salient PC concerns and CBT-based skills provision to specifically target issues faced by PC survivors (see Table 2).
Table 2.
Sample CBSM Treatment Components Addressing Prostate Cancer
| Prostate Cancer Concern/Issue | CBSM Technique |
|---|---|
| Patient beliefs (e.g. cause, efficacy) | Information Provision, Cognitive Restructuring |
| Treatment side effects (e.g. sexual dysfunction) | Information Provision, Coping Skills, Relaxation Training, Communication Skills, Assertiveness Training, Emotional Expression |
| Doctor-patient relationship & communication | Assertiveness Training, Communication Skills |
| Recurrence and/or progression concerns | Information Provision, Coping Skills, Cognitive Restructuring |
| Spouse/Partner relations, Intimacy | Assertiveness Training, Communication Skills, Emotional Expression |
| Social isolation | Social Support, Group-Based Support, Coping |
| Health Behaviors | Self-Awareness, Self-Management, Information Provision |
Table 2 Provides the list of concerns salient to prostate cancer patients and the CBT-based skills used to target the concerns faced by prostate cancer patients
Culturally Adapted Cognitive Behavioral Stress and Self-Management (CCBSM).
We followed a systematic approach to culturally adapt CBSM that considered language, culture and context (e.g., symptom burden) to develop a linguistically and culturally adapted CBSM (C-CBSM) intervention compatible with our participants’ cultural patterns and belief systems, meanings, values and social context (see Table 3). Our goals were not to promote change in culturally held beliefs, but rather ensure that Hispanic values and context were grounded in each of our CBSM components designed to improve our outcomes. Our cultural adaptation was guided by previous studies and theoretical models 22,25,26. The cultural adaptation of CBSM occurred in four stages: (a) information gathering (e.g., review of the literature on cultural values, traditions, illness perceptions specific to Hispanics and cultural influences on core intervention components); (b) preliminary adaptation design (e.g., integrate input of key stakeholders and a community advisory board that had input from patients, health care providers and administrators in our Hispanic communities with 5 individuals from each city, forward/backward translation of language); (c) preliminary adaptation tests (e.g., train facilitators, pilot adapted intervention); and (d) adaptation refinement based on feedback from participants of a pilot trial of the intervention 7. The final step involves testing the adapted treatment in a full-scale RCT. Our C-CBSM intervention underwent all these preliminary stages that led to the current C-CBSM being evaluated in a full-scale RCT.
Table 3.
Prevalent Hispanic Sociocultural Processes/Themes, Implications for CBT Approaches & C-CBSM Cultural Adaptations
| Cultural Factors | Cultural Process | Psychosocial Implication | C-CBSM Framed by Hispanic Cultural Factor | |
|---|---|---|---|---|
| C-CBSM Content | Implication for Participants | |||
| Familism | Strong attachment /interdependence with nuclear & extended family | • Over-reliance on family networks for support • Therapeutic gains must benefit & extend to family network • Risk of limited support if family network is limited or conflicted |
• Identifying efficacious sources of tangible & emotional support within the extended family • Identifying efficacious sources outside the family system • Gains extend to family system |
• Importance of self-care to maintain a strong family • Greater attention to expanding available efficacious social networks beyond family systems |
| Allocentrism | Needs of the group placed over the needs of the individual | • Preference of interpersonal relationships with nurturing, intimate and respectful “in-group” members • Collectivistic view— benefits must also benefit the group |
• Social support skills provision with direct benefits to in-group • Cognitive restructuring of how individual benefits derived from stress and self-management benefit the group |
• Identifying and optimizing ingroup sources of support • How self- care/manageme nt enhances ability to nurture and derive benefit from ingroup relations |
| Simpatía & Power Distance | Nonconfrontational interactions & conformity / powerful others as authority figures to respect | • Non-assertive communication style to maintain harmony • Avoid interpersonal conflict • Authority figures (e.g., health care providers) not questioned • Information seeking/questioning perceived as inappropriate/disrespect ful |
• Communication skills training with spouse/partner/family/hea lth care provider • Assertiveness skills, distinction between assertive vs. confrontational styles • Adaptive emotional expression of positive and negative emotions |
• Normalized assertive communication • Demystifying powerful figures/others • Communicating needs and emotions is appropriate • Managing family conflict caused by assertive communication |
| Fatalism & External Locus of Control | Destiny is beyond one’s control | • Limited outcome expectancies as external forces supersede selfmanagement and determination • Very little one can do to change the future • Limited motivation |
• More psychoeducation on disease etiology and course • Cognitive restructuring of fatalistic attitudes • Building coping skills/resources and selfefficacy to impact favorable outcomes |
• More attention to controllability and modifying outcome expectancies • Greater information on linkage between behavior, behavior change and outcomes |
| Health Stigma | Self-blame / health conditions perceived as punishment | • Shame and embarrassment • Stigmatized health condition with limited options for improvement |
• More psychoeducation on disease etiology and course • Cognitive restructuring of illness perceptions |
• Tailored and more detailed health information of PC • Normalcy and commonality of chronic diseases |
| Male Gender Roles | Strong masculine pride and identity | • Less treatment compliance • Sexual dysfunction as a major threat to identity |
•Cognitive restructuring to address multiple aspects of a masculine role • Expanding intimacy behaviors |
• Attention to how benefits to selfsupport masculine role • Normalization of alternative intimate behaviors |
Table 3 Demonstrates the process in which certain cultural factors are targeted to be culturally adapted
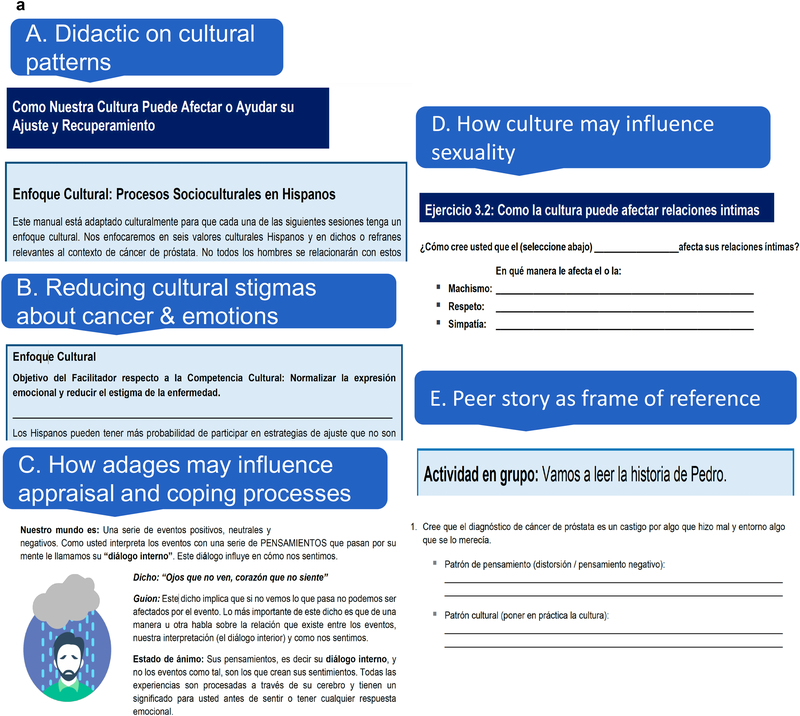
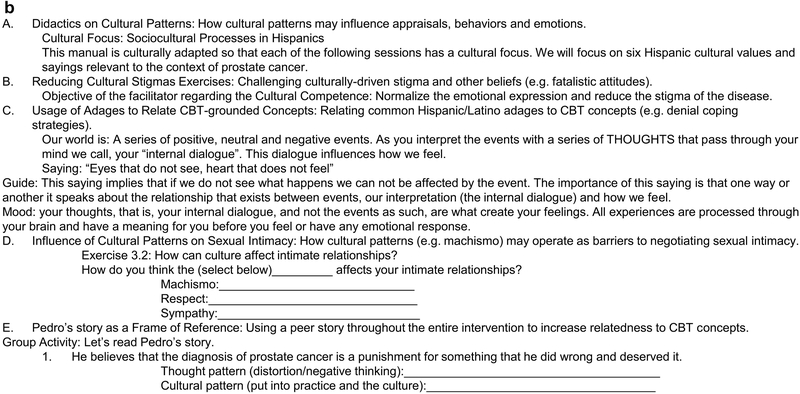
The C-CBSM intervention addresses social-cultural processes and biases with the goal of facilitating participants’ interpretation of CBSM skills practiced during the group sessions. For instance, participants are asked to consider an example of a fictitious character who struggles with intimacy with his partner and exhibits evasive behaviors due to a “machismo” or a strong masculine pride and identity. Participants then discuss how to use CBSM skills in order to evaluate this particular social cultural bias and expand alternative intimate behaviors. Examples of the cultural tailored material from our facilitator manual are depicted in Figure 2a and Figure 2b.
Figure 2.
a. Excerpts of how the culturally adapted intervention delivers intervention techniques
Cultural Awareness & Sensitivity Training
The group sessions will be led by facilitators who are fluent in Spanish and have graduate-level training in mental health. The facilitators will not be matched on ethnicity or sex. In order to avoid contamination, facilitators will not cross over condition. We will provide a 5-day training seminar on cultural sensitivity and awareness for all personnel involved in recruitment and assessment, and the interventionists leading the C-CBSM condition only. To reduce contamination, interventionists in the standard CBSM condition do not undergo this training and will not have access to C-CBSM intervention materials (e.g., facilitator manual). All CBSM and C-CBSM sessions will be audiorecorded and reviewed weekly by a licensed clinical psychologist for fidelity and feedback to the facilitators. To maximize participant accrual, retention and comfort with all procedures, emphasis will be on Hispanic PC survivors and involve thorough training on multicultural awareness that incorporate cultural attentiveness and sensitivity including cultural awareness (commonly held beliefs & practices by a culture), appreciation (respecting cultural differences specific to the delivery therapeutic techniques; e.g., collectivistic & familial frames of reference), and respect 27,28.
Data Collection
Sociodemographic, Medical, and Disease Characteristics
Participants will self-report medical information such as time since diagnosis and cancer treatment(s), stage of cancer, as well as information on prior or current psychiatric diagnoses. All medical and disease information will be verified via medical chart review. Medical comorbidities will be assessed with the Charlson Comorbidity Index 29. We will also collect age, education, income, race, Hispanic ancestry, employment status, relationship status, nativity, years in the US and years of US education. Sociodemographic, medical and disease information will be obtained at study baseline and during the 3, 6, and 12-month post-intervention assessments. All assessments will be done in person by a Spansih-speaking member of the research team.
Primary Outcomes: Symptom Burden and Health Related Quality of Life (HRQoL)
Symptom burden will be assessed as an interview with study staff using the EPIC-Short Form Sexual Summary (EPIC-S) score and the EPIC-Short Form urinary domain score 30–34. HRQoL will be measured with two questionnaires, the Functional Assessment of Cancer Therapy-Prostate and the Patient-Reported Outcomes Measurement Information System (PROMIS) short forms for pain and fatigue 35–39. The FACT assesses physical well-being, emotional well-being, social/family well-being, and functional well-being. The FACT-P and PROMIS measures have been used to assess functioning (e.g., nausea, pain, fatigue, life engagement, work and/or daily activities) in cancer survivors and are available in Spanish 37
Secondary Outcomes: Stress Management Skills, and Emotional & Physiologic Adaptation
We hypothesize that C-CBSM’s greater impact on symptom burden and HRQoL will be mediated by its effect on stress management skills, emotional adaptation, and the regulation of inflammation. C-CBSM intervention targets including stress awareness, cognitive appraisals, relaxation skills, coping and communication skills, and interpersonal skills will be assessed using the Measure of Current States (MOCS) 40. This instrument was designed to specifically evaluate efficacy of CBSM. For distress, we will administer the Memorial Anxiety Scale for Prostate Cancer patients (MAX-PC). The MAX-PC is an 18-item scale that detects symptoms of anxiety in PC patients. It evaluates three aspects of PC specific anxiety on 3 subscales: anxiety related to PC in general (PC anxiety subscale), anxiety specifically centered around prostate specific antigen (PSA) testing (PSA anxiety subscale) and fears of cancer recurrence (fear of recurrence subscale). The MAX-PC demonstrated high internal reliability and is well validated in PC patient samples41.
Because inflammation underlies much of the symptom burden in PC treatment 42, a secondary aim is to examine whether C-CSBM dampens cytokine release and proinflammatory gene expression. Accordingly, blood is being collected to measure biomarkers of low-grade, systemic inflammation, and to assess leukocyte cytokine release following microbial stimulation. A licensed phlebotomist within the study medical centers of each site will conduct blood draws. Blood draws will occur at study baseline and during all three follow-up assessments. For systemic biomarker, 5-ml of blood are drawn before the assessment interviews into BD Serum-Separator Tubes and serum harvested via manufacturer’s instructions. Aliquots are frozen at −80° C until the study ends. Serum is assayed in a single batch for C-reactive protein (CRP) and interleukin-6 (IL-6)-widely utilized markers of inflammation. Assays are conducted with commercially available Quantikine immunoassays (R&D Systems). To model leukocyte cytokine responses, we culture whole blood ex vivo with microbial ligands that engage toll-like receptors (TLRs), and monitor production of inflammatory cytokines43. (The ligands are endotoxin, which simulates bacterial activation via TLR4, and R848, which simulates viral activation via TLR7/TLR8). Plates are incubated for 6 hours under standard conditions, after which supernatants are harvested and frozen at −80°C. Thawed samples are assayed in single batch by electrochemiluminescence on a SECTOR Imager 2400A, using multiplex kits from Meso Scale Discovery. We will measure four cytokines implicated in symptom burden and HRQoL: IL-1 β, IL-6, IL-10 and TNF-α and standardized values will be averaged into an unweighted linear composite reflecting the magnitude of inflammatory response. One aliquot of stored blood will also be assayed for genome-wide transcriptional profiling by mRNA sequencing. Briefly, RNA samples will be tested for suitable mass and integrity, converted to cDNA (Lexogen QuantSeq 3’ FWD), and sequenced on an Illumina HiSeq4000 instrument. Sequence reads will be mapped to the human genome to quantify transcript abundance, and log2-transformed normalized abundance values will be analyzed by linear statistical models to quantify intervention effects on gene expression after control for covariates. Bioinformatics analyses will test for intervention-induced reductions in expression of an a priori-defined set of pro-inflammatory genes44 as well as promoter sequence-based indications of reduced activity of pro-inflammatory transcription factors NF-κB and AP-1.
Analyses
Descriptive statistics will be computed to ensure values are within expected ranges and to eliminate any errors. We will compute estimates of internal consistency (Chronbach’s α) for all scales and composite scores. If reliability is <.70, we will evaluate the internal consistency of the measure and delete items or subscales as needed.
Analyses will be intent-to-treat analyses and linear mixed models will be used to test the study hypothesis including those with missing data at time points by using full information maximum likelihood (FIML) estimation 45,46. A linear mixed model will include fixed effects for the experimental group (C-CBSM vs. CBSM) and observation time, and random effect for person with a compound symmetry covariance structure for the repeated residuals within person. The linear mixed model will be analyzed for each outcome and intervention target (e.g., EPIC, PROMIS, FACT-P, MOCS, MAX-PC, inflammation). To address any potential effects of the interventionist, we will adjust for potential interventionist effects when testing our hypotheses. A group by time interaction and posthoc tests on this model effect will indicate whether and how the time course of the outcomes differ between the groups. We will test mediation using Latent Growth Modeling (LGM), where individual change trajectory (in each outcome of interest) is characterized by an intercept and a slope factor. The overall pattern of change (e.g., linear, quadratic, etc.) for the whole group can be specified by a particular set of coefficients associated with the slope factor. First, we will specify a growth curve model for all participants with an intercept factor representing our outcome of interest at baseline, and the slope factor reflecting the change trajectory in our outcome measure from baseline to our last time-point. For example, to test that increased stress management skills (e.g., MOCS) in the C-CBSM group accounts for reductions in symptom burden (e.g., EPIC-S), we will first test a LGM model without the stress management skills (the mediator), and then test the model with change in stress management skills from baseline to our last follow-up time-point. In the model without the stress management skills, we expect that group assignment is not related to baseline symptom burden, but that group assignment will be related to a greater negative change (i.e., reduction) in symptom burden scores. In the next step, we will add stress management skills and expect that after adding this mediator in the model, the path between group assignment and symptom burden slope will become nonsignificant, while the path between the mediator and symptom burden slope is significant thus suggesting mediation 47,48.
Power is based on the effect size defined as the group difference in the mean change divided by the standard deviation of the change. Power calculations are based on effects found within our pilot study 7. With 100 participants per study condition, there is 80% power to detect an effect size of 0.40 assuming a two-tailed test and a Type I error rate of 5% in our primary outcomes. Since multiple tests look at change in various post-intervention time points, using a Type I error rate of 1% results in a detectable effect size of 0.49. The sample size of at least 100 per arm has sufficient power to detect differences even after adjusting for the analysis of change from baseline to postintervention time points. We anticipate that we will be able to detect small changes in all of our outcomes. As an example, PROMIS measures were scaled to the general population with a standard deviation of 10. Therefore, an assumed effect size of .40 would translate to four t-score points, which is less than half a standard deviation change in the PROMIS scales.
Data Management
All research data will be organized and managed using Research Electronic Data Capture (REDCap) hosted at Northwestern University. REDCap is a research management tool which enables a secure study website accessible to all IRB approved research team members regardless of study site 39. REDCap will be used to administer the screening, sociodemographics, baseline and follow-up questionnaires, and to organize medical record review data. Once collected, all research data will be imported into SPSS for cleaning and analysis.
Discussion
The goal of this randomized controlled trial is to evaluate the incremental efficacy of a culturally adapted cognitive behavioral stress and self-management intervention (CCBSM) in reducing the symptom burden and improving the HRQoL in Hispanic, Spanish-speaking men treated for localized prostate cancer, relative to a standard, nonculturally adapted intervention (CBSM). We also evaluate the extent to which incremental effects of C-CBSM on symptom burden and HRQoL are mediated by improvements in targets of C-CBSM (e.g., stress management) emotional adaptation (e.g., anxiety) and inflammatory regulation. Given the HRQoL disparities among Hispanic PC survivors and the influence of Hispanic culture and sociocultural processes (e.g., allocentrism, familism, fatalism, simpatia) on health among Hispanics, this study represents an importance advancement in the literature 10,17. In particular, the cultural adaptation in this study went beyond linguistic translation to Spanish and incorporated intervention content compatible with our Hispanic cultural and sociocultural patterns, belief systems, meanings, values, and social context into the C-CBSM intervention.
The primary limitation of this study protocol is the interventions (both C-CBSM and CBSM) require in-person sessions which requires men to travel to medical centers in order to participate. If the C-CBSM intervention demonstrates superior efficacy to the standard, non-culturally adapted CBSM intervention, future studies should consider expanding the reach of patients by offering a web-based or eHealth version of the CCBSM intervention. Furthermore, because the focus of this study is cancer survivorship post-active treatment, men undergoing active treatment such as radiotherapy or active surveillance (AS) will not be enrolled in the current study. Future studies should consider establishing the efficacy of a C-CBSM program among Hispanic men in active treatment or AS for PC.
To our knowledge, this is the first study to examine the effects of a culturally adapted CBT-based intervention on symptom burden and HRQoL in Hispanic PC survivors relative to a standard, non-culturally adapted intervention. In light of the very high 5-year survival rates among men with localized PC, it is imperative that researchers continue to improve the efficacy of tailored psychosocial interventions that aim to improve to reduce chronic and debilitating treatment side effects (e.g., sexual and urinary dysfunction, pain and fatigue) and improve overall functioning among men with PC, particularly minority men like Hispanics 1.
Acknowledgments
Funding: This work was supported by the National Cancer Institute [grant number R01 CA206456–01A1]
This study was funded in part by NCI Grant # RO1CA206456.
Footnotes
Publisher's Disclaimer: This is a PDF file of an unedited manuscript that has been accepted for publication. As a service to our customers we are providing this early version of the manuscript. The manuscript will undergo copyediting, typesetting, and review of the resulting proof before it is published in its final citable form. Please note that during the production process errors may be discovered which could affect the content, and all legal disclaimers that apply to the journal pertain.
References
- 1.Howlader N NA, Krapcho M, Miller D, Bishop K, Kosary CL, Yu M, Ruhl J, Tatalovich Z, Mariotto A, Lewis DR, Chen HS, Feuer EJ, Cronin KA (eds). SEER Cancer Stat Facts: Prostate Cancer SEER Cancer Statistics Review, National Cancer Institute; Bethesda, MD: 1975–2014;http://seer.cancer.gov/statfacts/html/prost.html. [Google Scholar]
- 2.Davis KM, Kelly SP, Luta G, Tomko C, Miller AB, Taylor KL. The Association of Long-term Treatment-related Side Effects With Cancer-specific and General Quality of Life Among Prostate Cancer Survivors. Urology. 2014;84(2):300–306. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Selli C, Bjartell A, Burgos J, et al. Burden of Illness in Prostate Cancer Patients with a Low-to-Moderate Risk of Progression: A One-Year, Pan-European Observational Study. Prostate Cancer. 2014;2014:472949. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Skolarus TA, Wolf A, Erb NL, et al. American Cancer Society prostate cancer survivorship care guidelines. CA: a cancer journal for clinicians. 2014;64(4):225–249. [DOI] [PubMed] [Google Scholar]
- 5.Paterson C, Robertson A, Smith A, Nabi G. Identifying the unmet supportive care needs of men living with and beyond prostate cancer: A systematic review. Eur J Oncol Nurs 2015;19(4):405–418. [DOI] [PubMed] [Google Scholar]
- 6.Aldwin CM, Park CL, Spiro A. Handbook of health psychology and aging. Guilford Press; 2007. [Google Scholar]
- 7.Penedo FJ, Traeger L, Dahn J, et al. Cognitive behavioral stress management intervention improves quality of life in Spanish monolingual hispanic men treated for localized prostate cancer: results of a randomized controlled trial. Int J Behav Med 2007;14(3):164–172. [DOI] [PubMed] [Google Scholar]
- 8.Stanton AL. Psychosocial concerns and interventions for cancer survivors. Journal of Clinical Oncology. 2006;24(32):5132–5137. [DOI] [PubMed] [Google Scholar]
- 9.Penedo FJ, Molton I, Dahn JR, et al. A randomized clinical trial of group-based cognitive-behavioral stress management in localized prostate cancer: Development of stress management skills improves quality of life and benefit finding. Annals of Behavioral Medicine. 2006;31(3):261–270. [DOI] [PubMed] [Google Scholar]
- 10.Yanez B, McGinty HL, Buitrago D, Ramirez AG, Penedo FJ. Cancer Outcomes in Hispanics/Latinos in the United States: An Integrative Review and Conceptual Model of Determinants of Health. J Lat Psychol 2016;4(2):114–129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Antoni MH. Psychosocial intervention effects on adaptation, disease course and biobehavioral processes in cancer. Brain, behavior, and immunity. 2013;30:S88–S98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Antoni MH, Lechner S, Diaz A, et al. Cognitive behavioral stress management effects on psychosocial and physiological adaptation in women undergoing treatment for breast cancer. Brain, behavior, and immunity. 2009;23(5):580–591. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Antoni MH, Lutgendorf SK, Blomberg B, et al. Cognitive-behavioral stress management reverses anxiety-related leukocyte transcriptional dynamics. Biological psychiatry. 2012;71(4):366–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Lubeck DP, Kim H, Grossfeld C, et al. Health related quality of life differences between black and white men with prostate cancer: Data from the cancer of the prostate strategic urologic research endeavor. Journal of Urology. 2001;166(6):2281–2285. [PubMed] [Google Scholar]
- 15.Penedo FJ, Dahn JR, Shen BJ, Schneiderman N, Antoni MH. Ethnicity and determinants of quality of life after prostate cancer treatment. Urology. 2006;67(5):1022–1027. [DOI] [PubMed] [Google Scholar]
- 16.Moadel AB, Morgan C, Dutcher J. Psychosocial needs assessment among an underserved, ethnically diverse cancer patient population. Cancer. 2007;109(S2):446–454. [DOI] [PubMed] [Google Scholar]
- 17.Gallo LC, Penedo FJ, Espinosa de los Monteros K, Arguelles W Resiliency in the face of disadvantage: do Hispanic cultural characteristics protect health outcomes? J Pers 2009;77(6):1707–1746. [DOI] [PubMed] [Google Scholar]
- 18.Kohn LP, Oden T, Muñoz RF, Robinson A, Leavitt D. Brief report: Adapted cognitive behavioral group therapy for depressed low-income African American women. Community mental health journal. 2002;38(6):497–504. [DOI] [PubMed] [Google Scholar]
- 19.Miranda J, Azocar F, Organista KC, Dwyer E, Areane P. Treatment of depression among impoverished primary care patients from ethnic minority groups. Psychiatric services. 2003;54(2):219–225. [DOI] [PubMed] [Google Scholar]
- 20.Miranda J, Duan N, Sherbourne C, et al. Improving care for minorities: can quality improvement interventions improve care and outcomes for depressed minorities? Results of a randomized, controlled trial. Health services research. 2003;38(2):613–630. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.American Psychological Association Guidelines for Providers of Psychological Services to Ethnic, Linguistic and Culturally Diverse Populations. 2018;http://www.apa.org/pi/oema/resources/policy/provider-guidelines.aspx.
- 22.Sue S, Zane N, Nagayama Hall GC, Berger LK. The case for cultural competency in psychotherapeutic interventions. Annu Rev Psychol 2009;60:525–548. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: Updated guidelines for reporting parallel group randomised trials. J Pharmacol Pharmacother. 2010;1(2):100–107. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Pfeiffer E A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. J Am Geriatr Soc 1975;23(10):433–441. [DOI] [PubMed] [Google Scholar]
- 25.Barrera M, Castro FG, Strycker LA, Toobert DJ. Cultural Adaptations of Behavioral Health Interventions: A Progress Report. Journal of Consulting and Clinical Psychology. 2013;81(2):196–205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bernal G, Rodriguez MMD. Advances in Latino Family Research: Cultural Adaptations of Evidence-Based Interventions. Family Process. 2009;48(2):169–178. [DOI] [PubMed] [Google Scholar]
- 27.Cross T, Bazron B, Dennis K, & Isaacs M National Center for Cultural Competence: Definitions of Cultural Competence. Curricula Enhancement Module Series. 2004;https://nccc.georgetown.edu/curricula/culturalcompetence.html.
- 28.Hays PA. Integrating Evidence-Based Practice, Cognitive-Behavior Therapy, and Multicultural Therapy: Ten Steps for Culturally Competent Practice. Professional Psychology-Research and Practice. 2009;40(4):354–360. [Google Scholar]
- 29.Charlson M, Szatrowski TP, Peterson J, Gold J. Validation of a combined comorbidity index. J Clin Epidemiol 1994;47(11):1245–1251. [DOI] [PubMed] [Google Scholar]
- 30.Ellison JS, He C, Wood DP. Stratification of postprostatectomy urinary function using expanded prostate cancer index composite. Urology. 2013;81(1):56–60. [DOI] [PubMed] [Google Scholar]
- 31.Ferrer M, Garin O, Pera J, et al. [Evaluation of the quality of life of patients with localizad prostate cancer: validation of the Spanish version of the EPIC]. Med Clin (Barc) 2009;132(4):128–135. [DOI] [PubMed] [Google Scholar]
- 32.Wei JT, Dunn RL, Litwin MS, Sandler HM, Sanda MG. Development and validation of the expanded prostate cancer index composite (EPIC) for comprehensive assessment of health-related quality of life in men with prostate cancer. Urology. 2000;56(6):899–905. [DOI] [PubMed] [Google Scholar]
- 33.Wheat JC, Hedgepeth RC, He C, Zhang L, Wood DP Jr. Clinical interpretation of the Expanded Prostate Cancer Index Composite-Short Form sexual summary score. J Urol 2009;182(6):2844–2849. [DOI] [PubMed] [Google Scholar]
- 34.Sanda MG, Dunn RL, Michalski J, et al. Quality of life and satisfaction with outcome among prostate-cancer survivors. New England Journal of Medicine. 2008;358(12):1250–1261. [DOI] [PubMed] [Google Scholar]
- 35.Cella DF, Tulsky DS, Gray G, et al. The Functional Assessment of Cancer-Therapy Scale - Development and Validation of the General Measure. Journal of Clinical Oncology. 1993;11(3):570–579. [DOI] [PubMed] [Google Scholar]
- 36.NIH PROMIS Instrument Development and Validation Scientific Standards Version 2.0 2013;http://www.healthmeasures.net/images/PROMIS/PROMISStandards_Vers2.0_Final.pdf.
- 37.Available Translations PROMIS measures are available in languages other than English. 2018;http://www.healthmeasures.net/explore-measurement-systems/promis/intro-topromis/available-translations
- 38.Cella D, Hernandez L, Bonomi AE, et al. Spanish language translation and initial validation of the functional assessment of cancer therapy quality-of-life instrument. Medical care. 1998;36(9):1407–1418. [DOI] [PubMed] [Google Scholar]
- 39.Harris PA, Taylor R, Thielke R, Payne J, Gonzalez N, Conde JG. Research electronic data capture (REDCap)--a metadata-driven methodology and workflow process for providing translational research informatics support. J Biomed Inform. 2009;42(2):377–381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Carver CS. Measure of Current Status. 2006; http://www.psy.miami.edu/faculty/ccarver/sclMOCS.html.
- 41.Dale W, Bilir P, Han M, Meltzer D. The role of anxiety in prostate carcinoma. Cancer. 2005;104(3):467–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Bower JE. Cancer-related fatigue: links with inflammation in cancer patients and survivors. Brain Behav Immun 2007;21(7):863–871. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Miller GE, Chen E, Fok AK, et al. Low early-life social class leaves a biological residue manifested by decreased glucocorticoid and increased proinflammatory signaling. Proceedings of the National Academy of Sciences. 2009;106(34):14716–14721. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Fredrickson BL, Grewen KM, Coffey KA, et al. A functional genomic perspective on human well-being. Proceedings of the National Academy of Sciences. 2013;110(33):13684–13689. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Schafer JL, Graham JW. Missing data: our view of the state of the art. Psychological methods. 2002;7(2):147. [PubMed] [Google Scholar]
- 46.Gupta SK. Intention-to-treat concept: a review. Perspectives in clinical research. 2011;2(3):109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.De Stavola BL, Daniel RM, Ploubidis GB, Micali N. Mediation analysis with intermediate confounding: structural equation modeling viewed through the causal inference lens. American journal of epidemiology. 2014;181(1):64–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.MacKinnon DP, Valente MJ. Mediation from multilevel to structural equation modeling. Annals of Nutrition and Metabolism. 2014;65(2–3):198–204. [DOI] [PMC free article] [PubMed] [Google Scholar]