SUMMARY
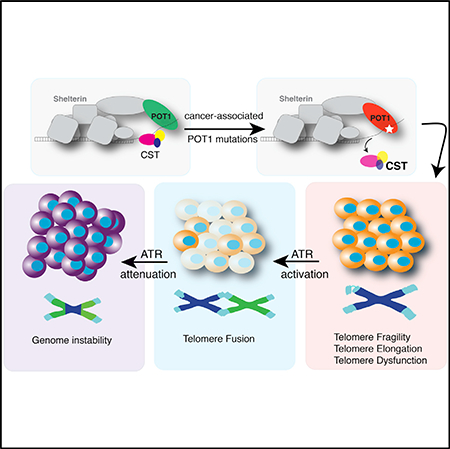
Genome sequencing studies have revealed a number of cancer-associated mutations in the telomerebinding factor POT1. Here, we show that when combined with p53 deficiency, depletion of murine POT1a in common lymphoid progenitor cells fosters genetic instability, accelerates the onset, and increases the severity of T cell lymphomas. In parallel, we examined human and mouse cells carrying POT1 mutations found in cutaneous T cell lymphoma (CTCL) patients. Inhibition of POT1 activates ATRdependent DNA damage signaling and induces telomere fragility, replication fork stalling, and telomere elongation. Our data suggest that these phenotypes are linked to impaired CST (CTC1-STN1-TEN1) function at telomeres. Lastly, we show that proliferation of cancer cells lacking POT1 is enabled by the attenuation of the ATR kinase pathway. These results uncover a role for defective telomere replication during tumorigenesis.
In Brief
Pinzaru et al. define a role for POT1 inactivation in the onset of thymic lymphomas. Inhibition of POT1 causes replication defects at telomeres resulting in telomere fragility, replication fork stalling, and genome instability. These results suggest a role of defective telemore replication during tumorigenesis
Graphical Abstract
INTRODUCTION
Telomere dysfunction has been proposed as a key event that causes transient genomic instability during cancer progression (Artandi et al., 2000). According to this model, progressive telomere shortening in preneoplastic cells results in telomere dysfunction and end-to-end chromosomal fusions. The resulting dicentric chromosomes undergo cycles of breakage-fusionbridge (BFB) and lead to gross chromosomal rearrangements. At this stage, reactivation of telomerase (or engagement of the alternative lengthening of telomeres [ALT] pathway) prevents further telomere dysfunction and allows cancer cells to proliferate indefinitely. This model has been validated in vivo using a mouse model in which telomerase activity can be experimentally re-activated (Ding et al., 2012). Additional evidence in support of this paradigm emerged from the analysis of telomere dynamics in human tumors (Chin et al., 2004; Gordon et al., 2003; Rudolph et al., 2001) and the detection of telomeric fusions in several types of cancers (Lin et al., 2010; Simpson et al., 2015).
Mutations affecting the telomere-binding protein protection of telomeres 1 (POT1) have been reported in chronic lymphocytic leukemia (CLL) (Quesada et al., 2011; Ramsay et al., 2013), familial melanoma (Robles-Espinoza et al., 2014; Shi et al., 2014), cardiac angiosarcoma (Calvete et al., 2015), glioma (Bainbridge et al., 2014), mantle cell lymphoma (Zhang et al., 2014), and parathyroid adenoma (Newey et al., 2012). Interestingly, analysis of the clonal evolution of CLL suggested that POT1 alterations arise during early leukemic development and are likely to contribute to disease progression (Landau et al., 2013). POT1 is a member of the six subunit shelterin complex that also comprises TRF1, TRF2, TPP1, TIN2, and RAP1 (de Lange, 2005). POT1 is anchored to telomeres by forming a heterodimer with TPP1, which is in turn tethered to the rest of the shelterin complex by TIN2 (Liu et al., 2004; Ye et al., 2004). POT1 binds single-stranded telomeric DNA (ssDNA) using two conserved oligonucleotide/oligosaccharide binding (OB) folds (Baumann and Cech, 2001; Lei et al., 2004), and has been proposed to counteract RPA binding (Flynn et al., 2011; Gong and de Lange, 2010). Depletion of POT1 in human cells elicits a DNA damage response (DDR) leading to the accumulation of telomere-dysfunction-induced foci (TIFs) and telomere fusions (Hockemeyer et al., 2005). Mice have two POT1 paralogs (POT1a and POT1b) that differ in their functions, with POT1a being most functionally related to human POT1. Depletion of POT1a leads to telomere dysfunction and results in embryonic lethality (Hockemeyer et al., 2006; Wu et al., 2006). In contrast, loss of POT1b leads to excessive elongation of the 3° overhang (Hockemeyer et al., 2006; Wu et al., 2006) and does not impair the viability of mice (Hockemeyer et al., 2006). Interestingly, conditional inactivation of POT1a in vivo induces different phenotypes depending on the cellular context. Depletion of POT1a in the nervous system leads to cellular attrition and disruption of neurogenesis (Lee et al., 2014). In contrast, POT1a depletion in the endometrium has no detectable consequences, but accelerates endometrial carcinogenesis in p53 null settings (Akbay et al., 2013). The POT1/TPP1 heterodimer also plays a key role in telomere length control (Nandakumar et al., 2012; Xin et al., 2007; Zhong et al., 2012; Lei et al., 2005; Loayza and De Lange, 2003).
The reported cancer-associated POT1 mutations cluster in the OB domains and disrupt the binding of POT1 to ssDNA in vitro (Quesada et al., 2011; Ramsay et al., 2013; Robles-Espinoza et al., 2014; Shi et al., 2014; Trigueros-Motos, 2014). Despite their prevalence among different cancer types, the mechanism by which POT1 mutations alter proper telomere function and influence tumor progression remains unclear. Limited functional analysis indicated that POT1 mutations promote excessive telomere elongation and an increase in telomere fragility (Ramsay et al., 2013; Robles-Espinoza et al., 2014). The telomere lengthening phenotype indicates that the mutations possibly act by extending cellular lifespan, which would enable further acquisition of cancer promoting mutations. However, the telomere fragility suggests that these mutations may induce telomere dysfunction leading to genome instability and tumor progression.
To elucidate the impact of POT1 inhibition in vivo, we conditionally deleted POT1a in lymphoid progenitor cells. The lymphatic system represents an ideal setting to address the consequences of POT1 inactivation, especially given the reported occurrence of somatic POT1 mutations in lymphoid tumors (Ramsay et al., 2013; Zhang et al., 2014). Our data demonstrate that POT1 inactivation synergistically cooperates with p53 loss to promote malignancy. Tumors derived from POT1 depleted cells display hallmarks of telomere dysfunction, including chromosome end-to-end fusions, telomere fragility, and gross chromosomal rearrangements. Similarly, expression of POT1 mutations (F62V and K90E) identified in cutaneous T cell lymphoma (CTCL) patients resulted in telomere fragility, chromosome fusions, ATR-dependent DNA damage activation, and replication fork stalling. Interestingly, our results indicate that POT1 inhibition leads to a concomitant impairment in CST function. Based on our data, we propose that inactivation of POT1 triggers telomere dysfunction due to defective telomere replication, ultimately leading to genome instability and enhanced tumorigenesis. Our data also suggest that growth of cancer cells carrying POT1 mutations is potentially achieved by a compensatory pathway that attenuates the ATR-dependent DDR pathway. Altogether, our data describe a unique mechanism by which defective telomere replication exacerbates tumor growth.
RESULTS
POT1a Inactivation in Common Lymphoid Progenitor Cells
The frequency of POT1 mutations in cancers of lymphoid origin prompted us to investigate the consequences of POT1 inhibition in common progenitor lymphoid (CLPs) cells. Given the close functional similarity between mouse POT1a and human POT1, we crossed POT1a conditional knockout mice (Hockemeyer et al., 2006) with the CLP cells specific CRE line hCD2iCRE (de Boer et al., 1988) and generated a cohort of POT1aF/FhCD2Cre (hereafter referred to as POT1Cd2) mice. The resulting mice were viable, but displayed a marked reduction in circulating mature B and T cells and fewer splenic B cells and CD4+CD8+ thymic T cells (Figures 1A and S1A–S1G and data not shown). To test whether this reduction was caused by the induction of a DDR, we crossed POT1aF/FhCD2Cre with mice harboring a conditional p53 allele (Marino et al., 2000) and generated animals in which both p53 and POT1a were depleted from CLP cells (Figure S1A). The resulting mice (3 weeks of age) had a partial rescue of CD4+CD8+ thymocyte development (Figures S1B and S1C) when compared to POT1Cd2 mice. In contrast, viability of B cells was not rescued by depletion of p53 (Figures S1E–S1G). Gene expression analysis indicates that the observed difference in viability is not due to differential expression levels of Pot1a and Pot1b in B and T cells (Figure S1H). Our data therefore show that upon POT1a depletion, B cells elicit a p53-independent cell death pathway, while T cells initiate a cell death response that is partially dependent on p53 activation.
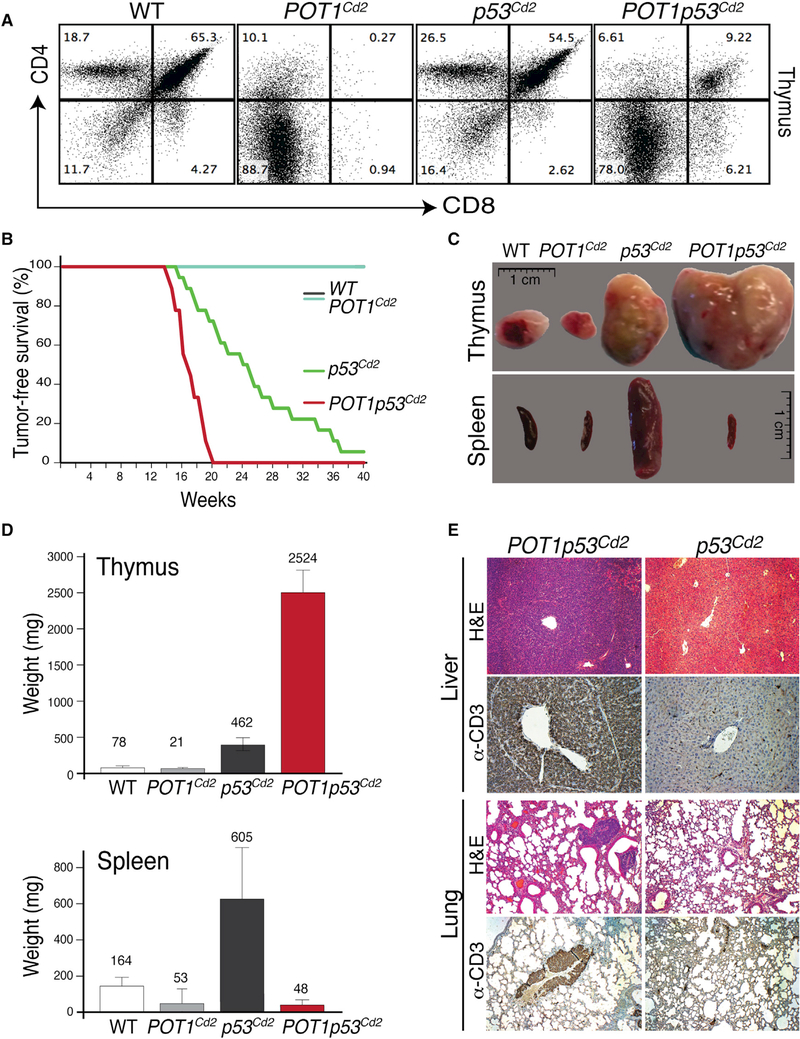
Figure 1. Conditional Deletion of POT1a and p53 in Mouse CLP Cells Leads to Aggressive Thymic Lymphomas.
(A) Flow cytometry analysis of CD4 (y axis) and CD8a (x axis) on thymocytes from mice of the indicated genotypes at approximately 16 weeks of age.
(B) Survival curve of mice of the indicated genotypes: POT1Cd2 (n = 20), p53Cd2 (n = 18), POT1p53Cd2 (n = 18), and Wild-Type (n = 25) (this cohort includes hCd2iCRE negative mice, as well as hCd2-iCRE positive not containing floxed alleles for POT1 or p53); survival curves of p53Cd2 and POT1p53Cd2 mice were compared using the log rank test (p < 0.01).
(C) Representative images of thymus and spleen from mice of the indicated genotypes.
(D)Quantification of thymus (top) and spleen size (bottom) from wild-type (WT), POT1Cd2, p53Cd2, and POT1p53Cd2 mice. The bars represent mean ± SD (n = 10 mice/genotype). The numbers within the graph indicate the mean value.
(E)Histological analysis of liver and lung tissues from p53Cd2 and POT1p53Cd2 mice that succumbed to tumor burden. The tissue sections were stained with H&E, as well as anti-CD3 antibody.
Somatic Inactivation of POT1a and p53 Predisposes Mice to Thymic Lymphomas
To evaluate the cooperation between POT1 and p53 inactivation during tumor progression, we monitored cohorts of POT1a+/+p53Flox/FloxhCD2Cre (p53Cd2), POT1aFlox/Floxp53+/+ hCD2Cre (POT1Cd2), and POT1aFlox/Floxp53Flox/FloxhCD2Cre (POT1p53Cd2) mice. None of the wild-type controls or the POT1Cd2 mice developed cancers (Figure 1B), whereas the majority of p53Cd2 mice presented with tumors by 20 weeks of age and displayed a median lifespan of 24 weeks. p53Cd2 mice developed both T cell lymphomas (14/18) as well as B cell lymphomas (4/18), and this is in agreement with the established role for p53 in the suppression of tumor formation in hematopoietic progenitors (Yin et al., 2011). Remarkably, POT1p53Cd2 mice had significantly shorter lifespans than the p53Cd2 mice, with a median age of 17 weeks (Figure 1B). This significant (log rank test p < 0.01) difference in tumor-free survival suggests that POT1 inactivation cooperates with p53 loss during tumor formation. Strikingly, all (18/18) POT1p53Cd2 mice developed thymic lymphomas and did not show signs of other malignancies (Figures 1C and 1D), suggesting that POT1 inactivation alters the distribution of T versus B cell lymphomas. Interestingly, the vast majority of thymic lymphomas in POT1p53Cd2 mice disseminated to both lymphoid and non-lymphoid tissues, such as liver, kidney, and lungs (Figure 1E). In contrast, only a small fraction (20%) of thymic lymphomas in p53Cd2 mice spread to other tissues (Figure 1E). The T cell origin of the metastasis was confirmed by staining for the T cell marker CD3 by immunohistochemistry (Figure 1E) and fluorescence-activated cell sorting (FACS) analysis (data not shown). In conclusion, our results show that POT1 inhibition cooperates with p53 inactivation during the development of invasive thymic lymphomas.
Increased Genome Instability in POT1p53Cd2 Mice
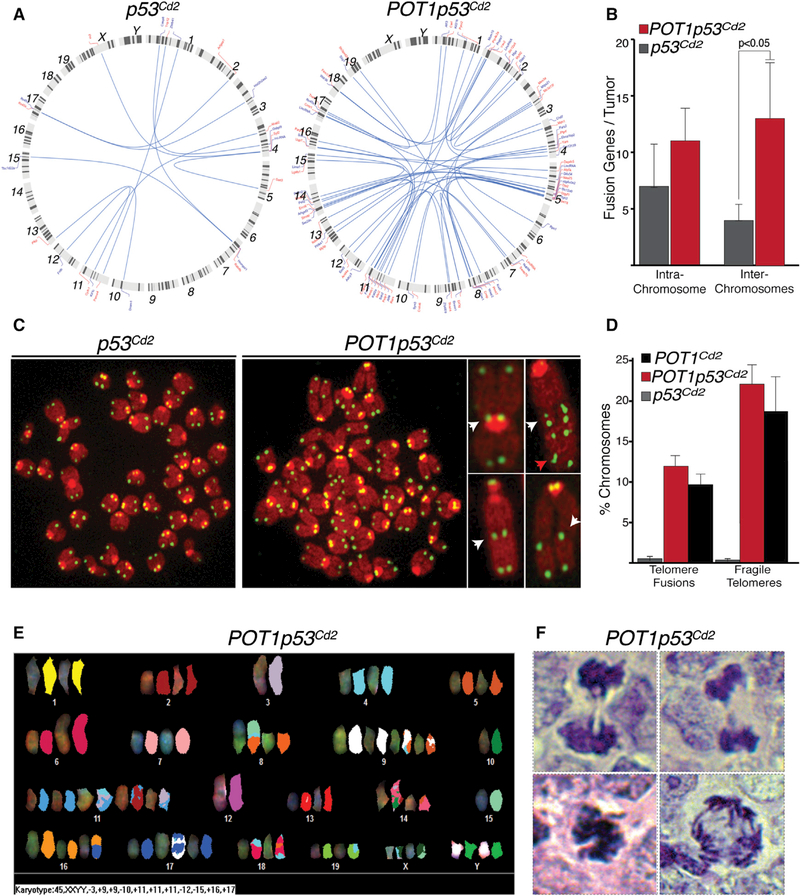
Next, we assessed whether the role of POT1 inactivation in tumor progression was correlated with increased genome instability. To this end, we performed a set of analyses to define the level of genomic instability observed in tumors derived from p53Cd2 and POT1p53Cd2 mice. First, we performed whole transcriptome analysis of tumors derived from p53Cd2 and POT1p53Cd2 mice. In tissues from POT1p53Cd2 tumors, we detected several transcripts derived from the fusion of genes located on distinct chromosomes (Figure 2A). On average, tumors from POT1p53Cd2 mice contained three times more gene fusion products compared to those derived from p53Cd2 mice, indicating a greater degree of genome instability (Figures 2B, S2A, and S2B). To further strengthen this observation, we collected metaphase spreads from freshly isolated p53Cd2 and POT1p53Cd2 thymic lymphomas. Telomeric fluorescence in situ hybridization (FISH) analysis revealed that tumor cells lacking POT1 show a significant increase in end-to-end chromosomal fusions (Figures 2C and 2D). Interestingly, telomeres derived from POT1p53Cd2 tumors show elevated levels of telomere fragility (Figures 2C and 2D), a phenotype indicative of replication-dependent defects at telomeres (Sfeir et al., 2009). To further characterize the level of chromosomal instability, we carried out spectral karyotyping (SKY) analysis on cells derived from p53Cd2 and POT1p53Cd2 tumors (Figure 2E) and noted that lymphomas from POT1p53Cd2 mice had elevated levels of chromosomal translocations relative to p53Cd2 mice (Figures 2E, S2D, and S2E). Lastly, POT1p53Cd2 tumors are characterized by the presence of aberrant mitotic figures (Figures 2F, S2F, and S2G), which were not detected in p53Cd2 tumors (Figures S2F and S2G). Collectively, these data show that the tumors derived from POT1p53Cd2 mice display increased levels of chromosome instability when compared to tumors derived from p53Cd2 mice, thereby establishing a role for POT1 inhibition in the onset of genome instability that promotes tumorigenesis.
Figure 2. Exacerbated Genome Instability in Tumors Derived from POT1p53Cd2 Mice.
(A)Circos plots illustrating the inter-chromosomal fusion transcripts detected by RNaseq analysis of p53Cd2 and POT1p53Cd2 thymic lymphomas. The connecting curves represent the chromosomal location of the genes involved in translocations. The chromosome number and name of the genes involved in translocation are indicated in the figure. Note that a complete list of translocations identified is also reported in Figure S2.
(B) Graph depicting the number of inter- and intra-chromosome fusions in tumors isolated from p53Cd2 and POT1p53Cd2 mice.
(C) Representative metaphase spreads from thymic lymphomas with the indicated genotype. The telomeres are in green (peptide nucleic acid [PNA] probe) andthe chromosomes in red (DAPI). The highlighted chromosomes in the right images show examples of telomeres fusions (white arrow) and fragile telomeres (red arrow).
(D) Quantification of chromosome end-to-end fusions and fragile telomeres detected on metaphase spreads derived from primary thymocytes of the indicatedgenotypes. The bars represent mean values of three independent experiments with SDs.
(E) SKY analysis of tumor-derived thymocytes from POT1p53Cd2 mice displaying extensive chromosome rearrangements.
(F) Aberrant mitotic figures in thymic lymphoma sections from POT1p53Cd2 mice stained with H&E.
Somatic POT1 Mutations in CTCL
Next, we tested whether expression of cancer-associated POT1 mutations caused similar phenotypes to those detected upon POT1a inhibition in vivo. POT1 mutations were found in 10% of patients with CTCL by whole exome sequencing (Choi et al., 2015) (Figures 3A and S3A). We found two recurrent amino acid alterations (p.K90 and p.F62) that occurred in more than one cancer sample (Figure 3A). All cases with POT1 mutations had concomitant inactivating mutations in TP53 (Figure S3A). There were two CTCLs with p.F62 alterations (p.F62V and p.F62I). The p.K90E substitution was also identified in patients with CLL (Ramsay et al., 2013). We therefore focused on these two alleles (p.F62V and p.K90E) for further analysis. Of note, these two somatic mutations (p.F62V and p.K90E) were highly clonal (occurring in >95% of cancer cells), suggesting they occurred early in disease pathogenesis (data not shown).
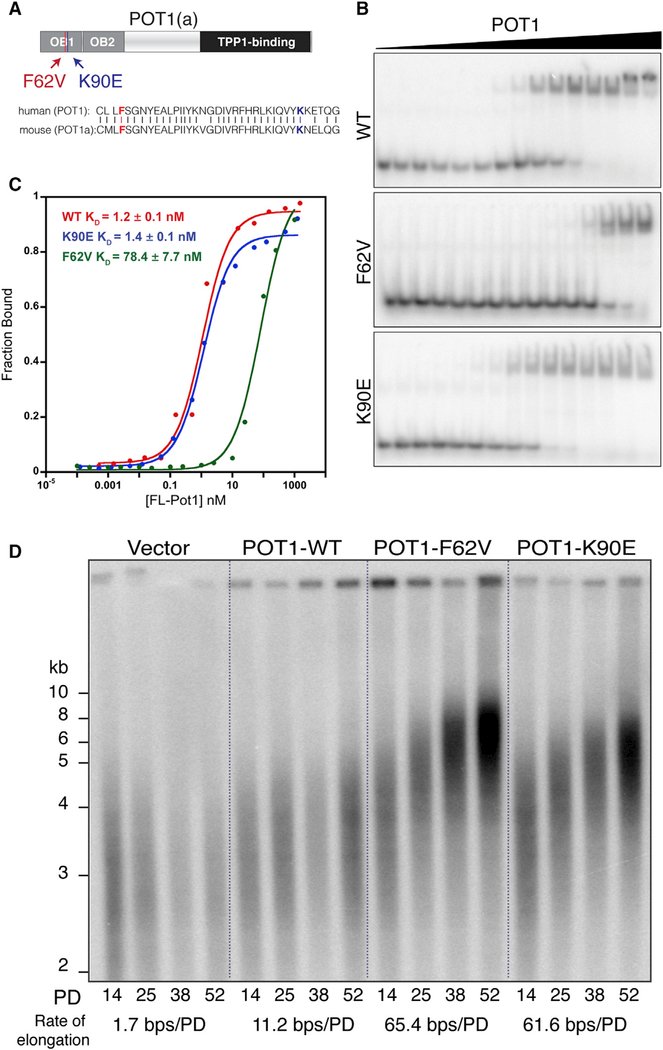
Figure 3. POT1 F62V and K90E Localize to the Telomeres and Induce Telomere Elongation.
(A) Schematic of the POT1/POT1a protein domains, highlighting the F62V and K90E mutations, which map to conserved residues in the OB fold of the protein.
(B) Representative EMSA to determine the DNAbinding affinity of purified WT and variant POT1 proteins to a radioactively end-labeled telomeric primer (5ˊ-TTAGGG)3.
(C) Data from (B) plotted as a function of fractionbound versus protein concentration. The mean KD values of three independent experiments are reported in the graph.
(D) Southern blot analysis to monitor telomerelength in HT1080 cells overexpressing WT and mutant POT1 proteins over several PDs. The median telomere length in each lane was calculated using the Telometric 1.2 software (Grant et al., 2001). The elongation rate for each condition was subsequently computed from the differences in median telomere length between lanes.
Characterization of POT1-F62V and POT1-K90E
To address the impact of F62V and K90E substitutions on the association of POT1 with ssDNA, we performed electrophoretic mobility shift assays (EMSA). Expression and purification of recombinant wild-type and mutant human POT1 was carried out using a baculovirus expression system (Figure S3B). The results indicate that the F62V substitution substantially diminishes the binding affinity of POT1 to a telomeric substrate comprising three TTAGGG repeats (Figures 3B and 3C). This result is in agreement with previous structural and biochemical analyses that denote the importance of this phenylalanine residue for ssDNA binding (Lei et al., 2004; Wu et al., 2006). Additionally, the significantly reduced ability of POT1-F62V to bind telomere DNA in vitro is consistent with limited analysis carried out on a handful of cancer-associated POT1 mutations thus far (Ramsay et al., 2013; Robles-Espinoza et al., 2014; Shi et al., 2014). As opposed to POT1-F62V, which was strongly impaired for DNA binding in vitro, the POT1-K90E mutant allele binds telomere DNA with similar affinity as POT1-WT (Figures 3B and 3C). The K90E substitution did not grossly alter the specificity of POT1 to telomere DNA, since no binding to a non-TTAGGG substrate was noted (data not shown). The striking difference in DNA binding affinity between the two mutations prompted us to investigate how they impact telomere maintenance and protection.
To elucidate the impact of the CTCL-associated mutations on telomere function at the cellular level, we pursued two complementary approaches. First, we generated heterologous cell lines in which Myc-tagged wild-type and mutant POT1 alleles (F62V and K90E) were overexpressed in human HT1080 fibrosarcoma cells and POT1a alleles were overexpressed in mouse embryonic fibroblasts (MEFs) (Figure S3C). In an independent approach, which allows us to investigate the mutations when expressed at endogenous levels, we used CRISPR/Cas9 gene targeting to manipulate the POT1 locus in human retinal pigment epithelium-1 (RPE-1) cells and the POT1a locus in mouse embryonic stem cells (mESCs) (Figures S3D–S3F).
The growth rate of HT1080 cells expressing POT1 mutations was similar to control cells (Figure S3G) and their cell cycle profile was unaffected (Figure S3H). Similarly, we generated several clonally derived cell lines carrying heterozygous and homozygous alleles of POT1a-K90E and POT1a-F62V, suggesting that the mutations do not grossly alter cellular survival. Indirect immunofluorescence (IF) and chromatin immunoprecipitation (ChIP) demonstrated that the mutant alleles are capable of localizing to telomere DNA (Figures S3I–S3K). These results are expected since POT1 recruitment to telomere DNA is mediated by an interaction with TPP1 (Liu et al., 2004; Ye et al., 2004), and the mutations lie in a region that does not interfere with POT1TPP1 binding (Figure 3A).
CTCL-Associated POT1 Mutations Promote Telomere Elongation
To determine whether POT1 mutations affect telomere length homeostasis and overhang processing, we cultured HT1080 cells overexpressing mutant POT1 alleles for increased population doublings (PDs) alongside cells expressing wild-type POT1 and control cells (Figure 3D). Telomere restriction fragment (TRF) analysis indicated that both mutations resulted in a significant and gradual increase in telomere length (Figures 3D, S3L, and S3M). In addition, expression of POT1-K90E and POT1F62V lead to a small reduction in overhang signal (Figures S3L and S3M), similar to the phenotype observed upon depleting POT1 from human cells (Hockemeyer et al., 2005) and following the deletion of POT1a from MEFs (Hockemeyer et al., 2006). Elongated telomeres were also observed in CRISPR/Cas9 targeted cells carrying mutant POT1 (Figures S3N and S3O). In conclusion, despite the significant difference in DNA binding affinities (Figures 3B and 3C), both POT1 mutations lead to a comparable telomere elongation. A similar telomere-lengthening phenotype was previously noted in patient-derived cells carrying analogous POT1 mutations (Ramsay et al., 2013; Robles-Espinoza et al., 2014; Shi et al., 2014; Trigueros-Motos, 2014). The observed telomere elongation is reminiscent of the phenotype observed after partial inhibition of DNA replication in human cells that have been treated with low levels of aphidicolin (Sfeir et al., 2009; Tong et al., 2015).
POT1 Mutations Activate an ATRDependent DDR and Induce Telomere Fragility
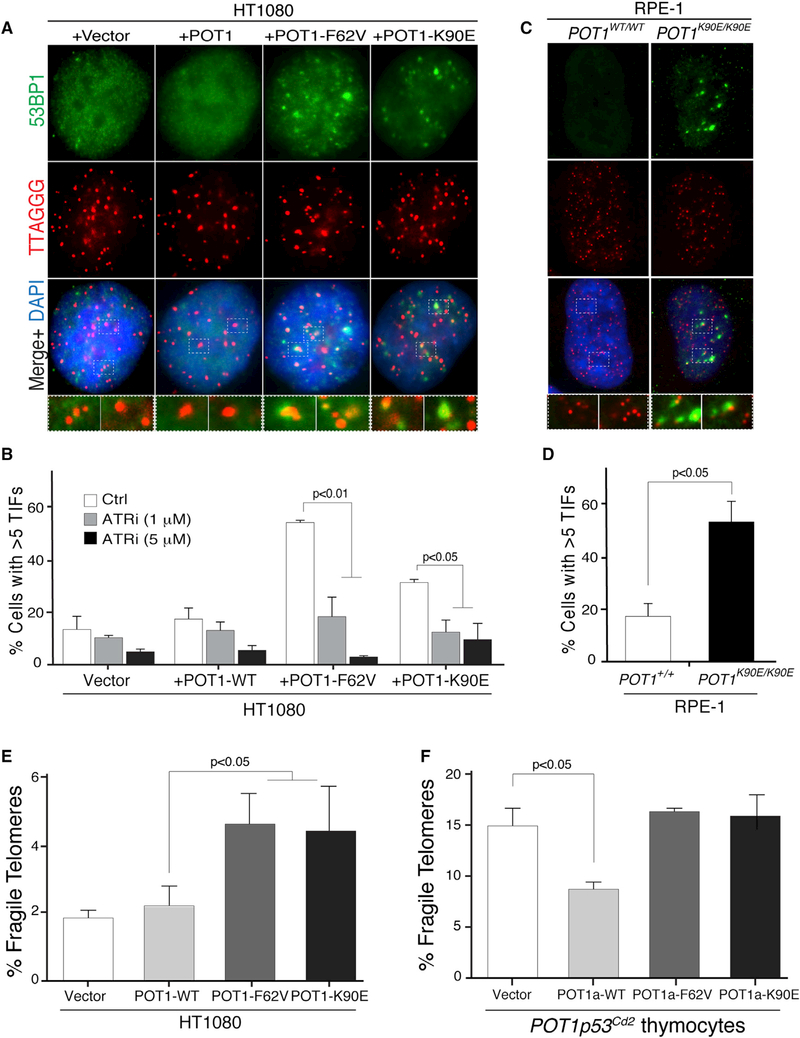
We next asked whether CTCL-associated mutations impair the protective function of POT1 at telomeres. Using IF-FISH (IF for 53BP1 coupled with FISH for telomeres), we found that cells (HT1080 and MEFs) expressing F62V and K90E mutants have frequent TIFs (Takai et al., 2003) (Figures 4A, 4B, and S4A). We also observed a significant increase in the TIF response in human and mouse cells carrying homozygous alleles for F62V and K90E (Figures 4C, 4D, and S4B). Notably, the expression of these CTCL-associated POT1 mutations induced an ATR-dependent DDR, as seen by the significant abrogation of TIFs in HT1080 cells treated with an ATR inhibitor (Figure 4B), led to the accumulation of RPA foci at telomere DNA (Figure S4C), and induced chromosome end-to-end fusions (Figures S4F and S4G). In addition, chromosome analysis revealed that POT1 mutations increased the incidence of fragile telomeres (Figures 4E and S4D), similarly to what was observed in thymic lymphomas derived from POT1p53Cd2 mice (Figure 2D). Complementation of POT1p53Cd2 thymocytes confirmed that POT1a mutant alleles are unable to suppress telomere fragility. Indeed, re-expression of a wild-type POT1a allele reduced the frequency of fragile telomeres, however, both mutants failed to rescue the telomere fragility caused by POT1a depletion (Figures 4F and S4E). Altogether, our data indicate that expression of cancer associated POT1 alleles inhibit the function of a key shelterin component, potentially leading to replication stress and telomere dysfunction.
Figure 4. POT1 Mutations Elicit an ATR Response and Lead to Telomere Fragility.
(A)IF-FISH staining for the DNA damage factor 53BP1 (green) at telomere DNA (red) in HT1080 cells overexpressing Myc-tagged WT POT1, as well as POT1-F62Vand POT1-K90E.
(B) Quantification of TIFs in HT1080 cells in the absence (white bars) and in the presence of ATR inhibitor (gray bars 1 mM ATRi and black bars 5 μM ATRi) for 6 hr. The bars represent the mean of three independent experiments (n = 100 nuclei per sample) ±SD (p value derived using student’s t test) (two-tailed).
(C) CRISPR/Cas9 gene targeting was used to create single base substitutions to the POT1 locus in RPE-1 cells and to generate clonally derived cells with the K90E mutation. IF-FISH was used to denote the TIFs response in cells expressing mutant POT1.
POT1 Inhibition Induces Replication Fork Stalling at Telomeres
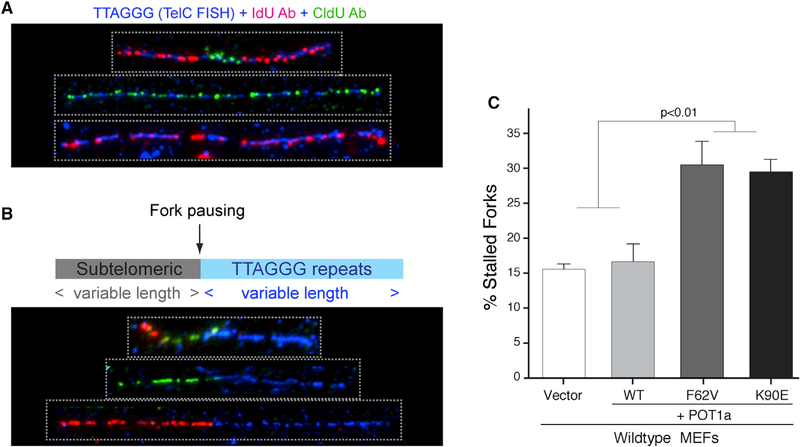
To address the impact of POT1 mutations on telomere replication in a direct manner, we performed single-molecule analysis of replicated DNA (SMARD) (Norio and Schildkraut, 2001) and examined the progression of replication forks through telomere DNA at single-molecule level. Analysis of CldU and IdU labeled molecules, including ones which carry a subtelomeric DNA segment, revealed several cases of labeling patterns indicative of replication fork stalling before or within the telomeric DNA (Figures 5A, 5B, and S5). The partially labeled telomere molecules were significantly enriched in cells expressing F62V and K90E when compared to cells expressing wild-type POT1a (Figure 5C). Thus, inhibiting POT1 function appears to challenge normal progression of the replication fork as it copies telomere DNA.
Figure 5. POT1 Mutations Lead to Replication Fork Stalling at Telomere DNA.
(A) SMARD analysis of telomeric DNA from MEFs overexpressing WT and mutant POT1a. The telomeric DNA molecules of variable lengths were identified bytelomeric FISH (TelC; blue) with incorporated IdU and CldU detected with fluorescent antibodies (red and green, respectively). The molecules are representative of a normal replication profile.
(B) Representative molecules that exhibit stalled replication forks at the junction between subtelomeres and telomeres.
(C) Quantification of stalled replication forks in MEFs overexpressing WT and mutant POT1a. The average of two independent experiments ±SEM is shown.
(D) Quantification of TIFs for cells with the indicated genotype. There were >2 independently isolated clones that were analyzed for each genotype. The barsrepresent the mean of three independent experiments (n = 100 nuclei per sample) ±SD (p value derived using student’s t test) (two-tailed).
(E) Quantification of fragile telomeres on metaphase spreads from HT1080 cells expressing WT and POT1 variants. The mean of at least three independent experiments ±SD (n > 4,000 total analyzed telomeres) (p value derived using student’s t test) (two-tailed) are shown.
(F) Quantification of fragile telomeres on metaphase spreads from tumor-derived POT1p53Cd2 thymocytes overexpressing WT and POT1a mutants. The mean of three independent experiments ±SD (p value derived using student’s t test) (two-tailed) are shown.
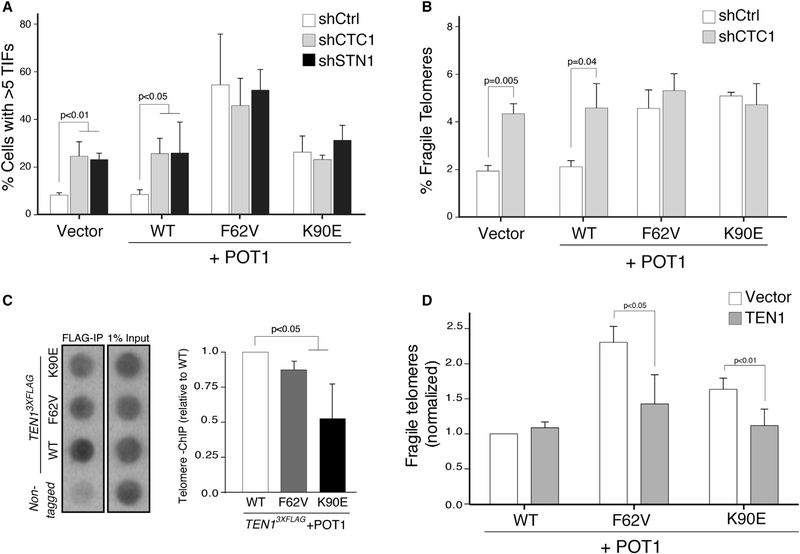
POT1 Inhibition and the Impairment of CST Function at Telomeres
The telomere phenotypes caused by expression of the POT1F62V and POT1-K90E alleles are reminiscent of the telomere aberrations caused by depletion of the CST complex. Indeed, inhibition of CST leads to ATR activation, telomere fragility, and significant lengthening of telomeres (Chen et al., 2012, 2013; Gu et al., 2012; Kasbek et al., 2013; Stewart et al., 2012). We therefore wondered whether POT1 acts in the same pathway as the CST complex to promote efficient telomere replication. To test this hypothesis, we treated HT1080 cells overexpressing wild-type or mutant POT1 with small hairpin (sh)RNAs against CTC1 and STN1, independently. The TIFs response elicited by the two POT1 mutants was not further enhanced following the depletion of CST factors (Figures 6A and S6A–S6C). Moreover, the percentage of fragile telomeres caused by the mutations did not significantly increase when CTC1 was inhibited (Figures 6B, S6A, and S6B). These results suggest that POT1 mutants act in the same pathway as CST inhibition to alter telomere replication.
Figure 6. F62V and K90E Mutations Impact CST Function at Telomeres.
(A) Quantification of TIFs in HT1080 cells overexpressing WT and mutant POT1 and treated with shRNA against CTC1 (gray bars), STN1 (black bars), or control (white bars). The mean of three independent experiments (n > 100 nuclei per sample) ±SD (p value derived using student’s t test) (two-tailed) are shown.
(B) Quantification of fragile telomeres on metaphase spreads from HT1080 cells with the indicated treatments. The mean of three independent experiments ±SD (n > 2,500 total analyzed telomeres) (p value derived using student’s t test) (two-tailed) are shown.
(C) Telomere-ChIP from S phase synchronized TEN13XFLAG HeLa 1.3 cells expressing WT and mutant POT1. The telomeric DNA was blotted and detected with a telomere specific probe. The graph represents the % of input quantification of the telomere ChIP. The values were normalized to the control sample expressing WT POT1. The mean of five experiments ±SD (p value derived using student’s t test) (two-tailed, unequal variance) are shown.
(D) Quantification of fragile telomeres on metaphase spreads from HT1080 cells overexpressing WT and mutant POT1 in the absence (white bars) or presenceof overexpressed TEN1 (gray bars). The values were normalized to WT samples with no exogenous CST proteins. The mean of three independent experiments (n > 4,500 total analyzed telomeres) ±SD (p value derived using student’s t test) (two-tailed) are shown.
In recent years, it has become evident that the association of CST with telomeres is modulated by the interaction with the POT1/TPP1 heterodimer (Chen et al., 2012; Wan et al., 2009; Wu et al., 2012). We therefore set out to test whether the POT1 mutations destabilize the association between CST and the shelterin complex. To address this possibility, we transiently co-expressed FLAG-CST, HA-TPP1, and wild-type or mutant Myc-POT1. IP with anti-FLAG antibodies followed by western blot analysis for HA and Myc suggested that the K90E and F62V substitution in POT1 do not impact the interaction between CST and the TPP1/POT1 complex (Figures S6D and S6E). Intriguingly, however, pull-down experiments showed a small, but significant, reduction in the interaction between FLAGSTN1 and HA-TEN1 in the presence of Myc-POT1-K90E or Myc-POT1-F62V (Figures S6F and S6G). In summary, the coIP analyses suggest that alterations in the OB fold domain of POT1 are unlikely to compromise the direct interaction between the TPP1/POT1 heterodimer and the CST complex, yet both substitutions subtly destabilize CST complex assembly, potentially altering its function at telomeres. To address the impact of POT1 mutations on the telomeric-localization of CST in a direct manner, we generated knockin cells where endogenous TEN1 was tagged with three FLAG epitoptes and performed ChIP using FLAG antibodies. As evident by the results from the ChIP analysis, a small reduction in TEN1 localization at telomeres resulted when POT1-F62V and POT1-K90E were expressed (Figures 6C and S6H–S6J). Furthermore, overexpression of TEN1 and STN1 was capable of partially complementing the phenotypes associated with the POT1 mutations, indicated by the repression of telomere fragility in HT1080 cells expressing K90E and F62V (Figures 6D and S6K–S6M). Taken together, our data highlight a previously unanticipated functional interaction between POT1 and CST to ensure faithful telomere replication.
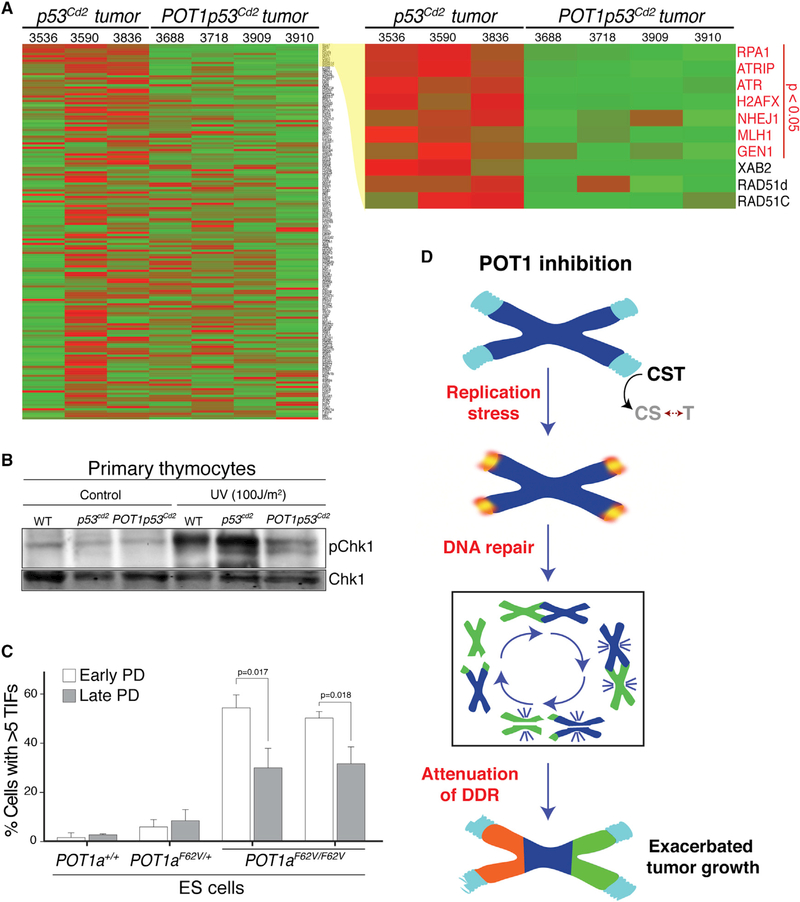
Attenuation of the ATR DDR Pathway in POT1p53Cd2 Tumors
So far, our data demonstrate that the development and progression of POT1-deficient tumors (Figure 1B) and the proliferation of POT1 mutant cells (Figures 4 and S3G) take place despite robust telomere dysfunction. To gain insight into the specific pathways that enable cellular growth in settings where POT1 is inactivated, we analyzed the transcription profile of thymic lymphomas derived from p53Cd2 and POT1p53Cd2 mice. Our goal was to identify potential differences in gene expression between tumors developing in the context of p53 deficiency alone and the aggressive malignancy resulting from the additional loss of POT1. RNA-sequencing (seq) analysis of seven tumors derived from p53Cd2 and POT1p53Cd2 mice identified 400 genes that are differentially expressed between the genotypes (Figures 7A and S7A). Interestingly, when we selectively examined the expression of known DDR genes and ranked them based on differential expression, we noted a significant reduction of DNA damage genes, most notably genes in the ATR pathway such as RPA1, ATR, and ATRIP (Figures 7A and S7A). Quantitative (q)PCR analysis confirmed that tumors derived from POT1p53Cd2 mice have lower expression of ATR and RPA1 when compared to thymic lymphomas derived from p53Cd2 mice (Figure S7B). Notably, we did not detect a significant difference in proliferation indexes between tumors derived from p53Cd2 and POT1p53Cd2 mice (Figures S2F and S2G), excluding that alterations in these genes is caused by cell cycle defects. These results suggest that in POT1 deficient tumors, a reduced level of expression of key ATR signaling factors allows cells to evade cell cycle checkpoints. To corroborate this finding, we assessed whether tumor cells derived from POT1p53Cd2 mice showed any defect in the activation of ATR signaling. Our data indicate that cells isolated from POT1p53Cd2 mice when challenged with UV irradiation had a severe impairment in the activation (phosphorylation) of the checkpoint kinase CHK1 (Figure 7B), a key downstream target of the ATR kinase. Finally, to test whether attenuation of the DDR in response to POT1 inhibition occurs in other cell types, we used mouse ES cells in which the endogenous POT1 gene was mutated to the F62V allele (Figures S3E and S4B). Using these cells, we could assess the long-term TIF response to POT1 inhibition in an isogenic setting. Consistent with our in vivo data, we found that when cultured for 50 passages (late PD), POT1-F62V ES cells downregulate the DDR and accumulate less TIFs in comparison to the same clones analyzed shortly after gene targeting (early PD) (Figure 7C).
Figure 7. Attenuation of the DNA Damage Response following POT1 Inhibition.
(A) RNA-seq analysis of three p53Cd2 and four independent POT1p53Cd2 thymic lymphomas.
(B) Western blot analysis of phosphorylated-Chk1 (pCHK1) and CHK1. The lysates prepared from primary thymocytes isolated from mice of the indicated genotypes were treated with UV (100 J/m2) and harvested 90 min after.
(C) Bar graph displaying percentage of TIF positive heterozygous (F62V/+) and homozygous (F62V/F62V) mouse ES cells, comparing levels of TIFs in early (whitebars) and late passage (gray bars) cells. The mean of three independent experiments (n > 100 nuclei per sample) ±SD are shown.
(D) Model depicting the proposed mechanism by which POT1 mutations shape tumor progression. POT1 inhibition impairs the function of CST at telomerespossibly by destabilizing the interaction between STN1 and TEN1. This then induces replication-dependent telomere defects (telomere fragility, ATR-dependent signaling, telomere elongation, and chromosome end-to-end fusions), which in turn triggers chromosomal instability. Ultimately, attenuation of the DDR enables the proliferation of cancer cells, leading to more aggressive tumors.
DISCUSSION
The experiments described here define a previously unrecognized mechanism for telomere-driven genomic instability in cancer cells. In addition to the classical view of telomeredys function due to telomere attrition, our findings highlight telomere replication stress as an additional pathway that leads to genomic rearrangements and fuels cancer progression. POT1 mutations have been previously documented in a number of cancers, including CLL, mantle cell lymphoma, melanoma, and glioma (Bainbridge et al., 2014; Quesada et al., 2011; Ramsay et al., 2013; Robles-Espinoza et al., 2014; Zhang et al., 2014). Here, we provide the first experimental evidence that POT1 inactivation contributes to cancer progression in the lymphatic system. We also identified two recurrent cancer-associated mutations in CTCL and elucidated the mechanistic basis for their potential tumor promoting activity.
POT1 Inhibition in Lymphoid Cells Promotes Tumor Progression
Germline deletion of POT1a is lethal in mice, a phenotype that cannot be rescued by p53 inactivation (Hockemeyer et al., 2006). Conditional inactivation of POT1 in vivo yields different phenotypes depending on tissue and cell type. Depletion of POT1a in neural stem cells results in impaired neurogenesis, a phenotype that can be rescued by p53 inactivation without promoting tumor formation (Lee et al., 2014). In striking contrast, depletion of POT1a in the endometrial epithelium had no detectable consequences on cell survival, but when combined with p53 inactivation resulted in accelerated tumor formation (Akbay et al., 2013). Mutations in human POT1 have not been associated with neurological defects nor with endometrial cancers, thus the implication of these findings for human health remains to be established. Here, we show that inactivation of POT1 in the lymphatic system accelerates the development of T cell lymphomas, which genetically mimics leukemic CTCL and have widespread genomic instability (Choi et al., 2015). While we cannot exclude that the compromised immune surveillance associated with POT1 deficiency is potentially contributing to tumor formation, we propose that POT1 inactivation in preneoplastic cells fosters genomic instability which enables cancer cells to acquire additional mutations to support unlimited growth and aggressive behavior (Figure 7D). In agreement with this hypothesis, we found that POT1a inactivation in mice results in telomere dysfunction (telomere fragility and telomere fusions) and genomic instability (chromosomal translocations), leading to the formation of lethal thymic lymphomas that invade surrounding tissues. Similarly, in CLL patients, POT1 mutations are associated with the more aggressive type of cancers (Ramsay et al., 2013).
Interestingly, our data indicate that depletion of POT1a shifts the tumor spectrum toward T cell lymphomas. While p53 depletion in CLP cells results in both T cell and B cell lymphomas, mice lacking p53 and POT1a primarily develop T cell lymphomas. A possible explanation for this finding is that T cell lymphomas in POT1p53cd2 mice are highly aggressive leading to accelerated lethality and precluding the development of the less aggressive B cell lymphomas. In agreement with this hypothesis, other mouse models that exacerbate p53 tumorigenesis also show a shift toward aggressive thymic lymphomas (Takahashi et al., 2007). Alternatively, it is possible that B cells are inherently less resistant to telomere dysfunction. In that regards, novel mouse models aimed at targeting POT1a and p53 depletion only in B cells will be required to fully address the latter possibility.
Shelterin Mutations: An Independent Pathway to Induce Genomic Instability in Tumors
Mutations in the shelterin subunits TIN2 (Walne et al., 2008) and TPP1 (Guo et al., 2014) have been previously identified in patients with critically short telomeres affected by bone marrow failure and dyskeratosis congenita. The increased risk of cancer associated with these mutations is linked to telomere attrition. So far, mutations in POT1 have not been found in short-telomeres syndromes. Instead, POT1 is the first subunit of the shelterin complex to show recurrent mutations in various types of cancers. The mechanism linking POT1 mutations with tumor development has been speculative. Our results show that POT1 mutations stimulate telomere elongation and telomere dysfunction, indicating that the compromised function of the shelterin complex can lead to tumorigenesis independent of the classic telomere erosion mechanism. Our findings raise the question of whether mutations in other shelterin subunits (or their accessory factors) might contribute to tumor progression, particularly mutations affecting telomere replication. In agreement with this hypothesis, recent experiments have shown that reduced TRF1 levels in mice can increase lymphoid tumor formation (Hartmann et al., 2016), and deletion of TRF1 in p53 null keratinocytes leads to squamous cell carcinomas (Martínez et al., 2009). TRF1 has been shown to play a crucial role in telomere replication (Martínez et al., 2009; Sfeir et al., 2009), suggesting that mice with reduced levels of TRF1 could display defective telomere replication. In addition, mice carrying mutations in RTEL1, a helicase that acts downstream of TRF1 in assisting telomere replication, display accelerated tumorigenesis when analyzed in the context of p53 deficiency (Vannier et al., 2013). It remains to be determined whether TRF1, RTEL1, and other telomere binding proteins are mutated in human cancers. Notably, SNPs in CTC1 and STN1 have been recently identified as risk factors in gliomas (Walsh et al., 2015).
A New Role for POT1 in Suppressing Telomere Defects Induced by Replication Stress
The highly repetitive and G-rich nature of telomere DNA makes it especially prone to forming G-quadruplex-like structures that can impede replicative polymerases as they duplicate telomere DNA (Parkinson et al., 2002). Telomeres evolved special ways to prevent replication fork stalling and assist fork restart. The shelterin subunit, TRF1, recruits unwinding helicases, including RTEL1 and BLM to resolve secondary structures and allow fork progression (Sfeir et al., 2009; Vannier et al., 2012, 2013; Zimmermann et al., 2014). In addition, the hetero-trimeric CST complex has been shown to assist in telomere duplication by enabling replication fork restart, independent of TRF1 activity (Stewart et al., 2012).
Our results highlight a previously unrecognized role for POT1 during telomere replication and suggest that this function is potentially linked to the CST complex. How the two complexes cooperate to ensure proper telomere duplication is far from being understood. A direct interaction between CST and TPP1/POT1 was previously reported, whereby TPP1 binds to STN1 in human cells (Chen et al., 2012, 2013), and POT1b recruits mouse STN1 during C-strand fill-in synthesis (Wu et al., 2012). This suggests that the interaction between the two complexes is multi-faceted and likely to be subject to different levels of regulation. Here, we identify two CTCL-associated mutations in the first OB fold domain of POT1 (F62V and K90E) that display very different binding affinities to telomere DNA in vitro, but lead to similar telomere phenotypes in vivo. We find that the two mutations do not impact the association between POT1/TPP1 and the CST complex. Instead, both F62V and K90E substitutions slightly affect CST complex assembly and impact its association with telomeres.
Structural Insight into the Deleterious Effect of F62V and K90E on the POT1-CST Interaction
To gain insight into how the cancer-associated POT1 mutations F62V and K90E could affect the function of the CST complex at telomeres, we analyzed the structural implication of these mutations.The crystal structure of human POT1 incomplex with ssDNA reveals that a single, continuous nucleoprotein molecular surface is formed by the side-by-side packing of the K90 residue and ssDNA, while F62 makesa strong geometrically constrained binding interaction with ssDNA (Figure S7C). Mutation of either of these sites is predicted to disrupt this surface, but only mutation atF62would also abolish DNA binding.This model is in a greement with the in vitro DNA binding assays (Figures3B and 3C).We speculate that this nucleoprotein surface serves as a scaffold for the assembly of the CST complex and either of the semutations would affect CST assembly. According to this model, the F62 residue of POT1 interacts directly with the ssDNA, while the K90 residue would be potentially involved in the interaction with CST. An alternative model based on structural analysis predicts that the K90E substitution might alter the conformation of ssDNA in the POT1ssDNA complex, which, in turn, might affect the CST complex assembly. Undoubtedly, future biochemical and structural experiments are required to further define the dynamic interplay between the TPP1-POT1 complexes and the CST complex at telomeric DNA. It is worth noting that recent work from Arabidopsis thaliana highlighted an interaction between the OB fold domain of POT1 and STN1 (Renfrew et al., 2014). In addition, expression of STN1 mutants that interfere with proper CST complex assembly leads to elongated telomeres and increased telomere fragility (Bryan et al., 2013), phenotypes that closely resemble those observed upon POT1 inhibition.
Attenuation of DDR Signaling as a Tumor Promoting Mechanism
The discovery of shelterin mutations in tumors raises the question of how tumor cells are able to proliferate despite high levels of telomere dysfunction and the resulting activation of a DDR. In the case of telomere erosion, re-activation of telomerase, or engagement in the ALT pathway, enables cancer cells to suppress telomere dysfunction and proliferate indefinitely. Our results indicate that attenuation of the ATR-dependent DDR represents one mechanism that allows tumor cells to bypass the proliferation defect imposed by POT1 inhibition (Hockemeyer et al., 2005, 2006). At a first glance, the impairment of the ATR-pathway in POT1-mutated tumors might seem counterintuitive especially that increased ATR signaling by activated oncogenes allows tumor cells to cope with replicative stress (Lecona and Ferná ndez-Capetillo, 2014). However, attenuation of the ATR pathway, perhaps in later stages of carcinogenesis or in the context of other replicative-stressors, could potentially allow tumor cells harboring replication defects to evade checkpoint activation and cell cycle arrest. Consistent with this idea, ATR or Chk1 heterozygous mice show increased incidence of tumors (Brown and Baltimore, 2000; Liu et al., 2000; Tho et al., 2012). In addition, somatic mutations in ATR and Chk1 have been found in human tumors with microsatellite instability (Vassileva et al., 2002). This observation is of interest given that complete suppression of ATR is lethal and that inhibitors of this pathway have been developed for clinical applications. It is tempting to speculate that inhibition of the ATR pathway in tumors with an attenuated ATR signaling might represent a valid treatment strategy. In effect, slight perturbation in the levels of ATR signaling might result in excessive inhibition of this essential signaling pathway, leading to selective cell death of cancer cells. On the other hand, one could imagine that treatments that reactivate the ATR pathway in cancer cells with attenuated ATR signaling might selectively kill such cancer cells without affecting healthy surrounding cells.
EXPERIMENTAL PROCEDURES
Detailed experimental procedures are provided in Supplemental Information. All animal studies were conducted in accordance with the NIH guidelines and approved by Institutional Animal Cancer and Use Committee. Cell culture techniques, CRISPR targeting, and RNA-seq analysis was performed using standard protocols. Telomere analysis, including telomere length measurement, TIF assay, telomere FISH on metaphase chromosomes, ChIP, and telomere SMARD were performed as previously described (Sfeir et al., 2009). Protein purification and EMSA are explained in detail in the Supplemental Information.
Supplementary Material
Highlights.
CTCL-associated POT1 mutations lead to telomere replication defects
POT1 mutations compromise the function of the CST complex at telomeres
Inactivation of POT1a promotes genomic instability and enhances tumorigenesis
Attenuation of ATR signaling in POT1a/p53 double knockout tumors
ACKNOWLEDGMENTS
We thank Titia de Lange, Joachim Lingner, Changchung Xiao, and Jerold Chun for providing critical reagents for this study. We thank Lauren Pitt, Markos Al-Far, and Angela Hin for technical assistance. We are grateful to Elena Federzoni and Bruce Torbett for support with the characterization of thymic lymphomas and Jonathan Hart and Andrew Routh for help in analyzing the RNA-seq data. We thank Susan Schwab, Shaheen Kabir, and members of the E.L-D. and A.S. labs for commenting on the manuscript. This work was supported by grants from the NIH for E.L.-D. (AG038677), A.S. (CA195767), and D.S.W. (GM059414). A.M.P. was supported by a NYSTEM institutional training grant (C026880). A.B. was supported by a CIRM scholarship, and R.A.H. was supported by the Ruth L. Kirschstein National Research Service Award (GM100532). Additional support was provided by the V-Foundation to A.S., by a Pew-Stewart Scholars Award to A.S., by a Pew Scholars Award to E.L.-D., and by the Novartis Advanced Discovery Institute to E.L.-D.
Footnotes
ACCESSION NUMBERS
The accession number for the RNA-seq data reported in this paper is NCBI: PRJNA316433.
SUPPLEMENTAL INFORMATION
Supplemental Information includes Supplemental Experimental Procedures and seven figures and can be found with this article online at http://dx.doi.org/10.1016/j.celrep.2016.05.008.
REFERENCES
- Akbay EA, Peñ a CG, Ruder D, Michel JA, Nakada Y, Pathak S, Multani AS, Chang S, and Castrillon DH (2013). Cooperation between p53 and the telomere-protecting shelterin component Pot1a in endometrial carcinogenesis. Oncogene 32, 2211–2219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Artandi SE, Chang S, Lee SL, Alson S, Gottlieb GJ, Chin L, and DePinho RA (2000). Telomere dysfunction promotes non-reciprocal translocations and epithelial cancers in mice. Nature 406, 641–645. [DOI] [PubMed] [Google Scholar]
- Bainbridge MN, Armstrong GN, Gramatges MM, Bertuch AA, Jhangiani SN, Doddapaneni H, Lewis L, Tombrello J, Tsavachidis S, Liu Y, et al. ; Gliogene Consortium (2014). Germline mutations in shelterin complex genes are associated with familial glioma. J. Natl. Cancer Inst 107, 384. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Baumann P, and Cech TR (2001). Pot1, the putative telomere end-binding protein in fission yeast and humans. Science 292, 1171–1175. [DOI] [PubMed] [Google Scholar]
- Brown EJ, and Baltimore D (2000). ATR disruption leads to chromosomal fragmentation and early embryonic lethality. Genes Dev. 14, 397–402. [PMC free article] [PubMed] [Google Scholar]
- Bryan C, Rice C, Harkisheimer M, Schultz DC, and Skordalakes E (2013). Structure of the human telomeric Stn1-Ten1 capping complex. PLoS ONE 8, e66756. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calvete O, Martínez P, Garcia-Pavia P, Benitez-Buelga C, Paumard-Herná ndez B, Fernandez V, Dominguez F, Salas C, Romero-Laorden N, Garcia-Donas J, et al. (2015). A mutation in the POT1 gene is responsible for cardiac angiosarcoma in TP53-negative Li-Fraumeni-like families. Nat. Commun 6, 8383. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chen LY, Redon S, and Lingner J (2012). The human CST complex is a terminator of telomerase activity. Nature 488, 540–544. [DOI] [PubMed] [Google Scholar]
- Chen LY, Majerská J, and Lingner J (2013). Molecular basis of telomere syndrome caused by CTC1 mutations. Genes Dev. 27, 2099–2108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chin K, de Solorzano CO, Knowles D, Jones A, Chou W, Rodriguez EG, Kuo WL, Ljung BM, Chew K, Myambo K, et al. (2004). In situ analyses of genome instability in breast cancer. Nat. Genet 36, 984–988. [DOI] [PubMed] [Google Scholar]
- Choi J, Goh G, Walradt T, Hong BS, Bunick CG, Chen K, Bjornson RD, Maman Y, Wang T, Tordoff J, et al. (2015). Genomic landscape of cutaneous T cell lymphoma. Nat. Genet 47, 1011–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Boer D, Cremers F, Teertstra R, Smits L, Hille J, Smeekens S, and Weisbeek P (1988). In vivo import of plastocyanin and a fusion protein into developmentally different plastids of transgenic plants. EMBO J. 7, 2631–2635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- de Lange T (2005). Shelterin: the protein complex that shapes and safeguards human telomeres. Genes Dev. 19, 2100–2110. [DOI] [PubMed] [Google Scholar]
- Ding Z, Wu CJ, Jaskelioff M, Ivanova E, Kost-Alimova M, Protopopov A, Chu GC, Wang G, Lu X, Labrot ES, et al. (2012). Telomerase reactivation following telomere dysfunction yields murine prostate tumors with bone metastases. Cell 148, 896–907. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Flynn RL, Centore RC, O’Sullivan RJ, Rai R, Tse A, Songyang Z, Chang S, Karlseder J, and Zou L (2011). TERRA and hnRNPA1 orchestrate an RPA-to-POT1 switch on telomeric single-stranded DNA. Nature 471, 532–536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gong Y, and de Lange T (2010). A Shld1-controlled POT1a provides support for repression of ATR signaling at telomeres through RPA exclusion. Mol. Cell 40, 377–387. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gordon KE, Ireland H, Roberts M, Steeghs K, McCaul JA, MacDonald DG, and Parkinson EK (2003). High levels of telomere dysfunction bestow a selective disadvantage during the progression of human oral squamous cell carcinoma. Cancer Res. 63, 458–467. [PubMed] [Google Scholar]
- Grant JD, Broccoli D, Muquit M, Manion FJ, Tisdall J, and Ochs MF (2001). Telometric: A tool providing simplified, reproducible measurements of telomeric DNA from constant field agarose gels. BioTechniques 31, 1314–1316. [DOI] [PubMed] [Google Scholar]
- Gu P, Min JN, Wang Y, Huang C, Peng T, Chai W, and Chang S (2012). CTC1 deletion results in defective telomere replication, leading to catastrophic telomere loss and stem cell exhaustion. EMBO J. 31, 2309–2321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo Y, Kartawinata M, Li J, Pickett HA, Teo J, Kilo T, Barbaro PM, Keating B, Chen Y, Tian L, et al. (2014). Inherited bone marrow failure associated with germline mutation of ACD, the gene encoding telomere protein TPP1. Blood 124, 2767–2774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hartmann K, Illing A, Leithauser F, Baisantry A, Quintanilla-Fend L, and Rudolph KL (2016). Gene dosage reductions of Trf1 and/or Tin2 induce telomere DNA damage and lymphoma formation in aging mice. Leukemia 30, 749–753. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hockemeyer D, Sfeir AJ, Shay JW, Wright WE, and de Lange T (2005). POT1 protects telomeres from a transient DNA damage response and determines how human chromosomes end. EMBO J. 24, 2667–2678. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hockemeyer D, Daniels JP, Takai H, and de Lange T (2006). Recent expansion of the telomeric complex in rodents: Two distinct POT1 proteins protect mouse telomeres. Cell 126, 63–77. [DOI] [PubMed] [Google Scholar]
- Kasbek C, Wang F, and Price CM (2013). Human TEN1 maintains telomere integrity and functions in genome-wide replication restart. J. Biol. Chem 288, 30139–30150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Landau DA, Carter SL, Stojanov P, McKenna A, Stevenson K, Lawrence MS, Sougnez C, Stewart C, Sivachenko A, Wang L, et al. (2013). Evolution and impact of subclonal mutations in chronic lymphocytic leukemia. Cell 152, 714–726. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lecona E, and Ferná ndez-Capetillo O (2014). Replication stress and cancer: it takes two to tango. Exp. Cell Res. 329, 26–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lee Y, Brown EJ, Chang S, and McKinnon PJ (2014). Pot1a prevents telomere dysfunction and ATM-dependent neuronal loss. J. Neurosci. 34, 7836–7844. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lei M, Podell ER, and Cech TR (2004). Structure of human POT1 bound to telomeric single-stranded DNA provides a model for chromosome end-protection. Nat. Struct. Mol. Biol 11, 1223–1229. [DOI] [PubMed] [Google Scholar]
- Lei M, Zaug AJ, Podell ER, and Cech TR (2005). Switching human telomerase on and off with hPOT1 protein in vitro. J. Biol. Chem 280, 20449–20456. [DOI] [PubMed] [Google Scholar]
- Lin TT, Letsolo BT, Jones RE, Rowson J, Pratt G, Hewamana S, Fegan C, Pepper C, and Baird DM (2010). Telomere dysfunction and fusion during the progression of chronic lymphocytic leukemia: evidence for a telomere crisis. Blood 116, 1899–1907. [DOI] [PubMed] [Google Scholar]
- Liu Q, Guntuku S, Cui XS, Matsuoka S, Cortez D, Tamai K, Luo G, Carattini-Rivera S, DeMayo F, Bradley A, et al. (2000). Chk1 is an essential kinase that is regulated by Atr and required for the G(2)/M DNA damage checkpoint. Genes Dev. 14, 1448–1459. [PMC free article] [PubMed] [Google Scholar]
- Liu D, Safari A, O’Connor MS, Chan DW, Laegeler A, Qin J, and Songyang Z (2004). PTOP interacts with POT1 and regulates its localization to telomeres. Nat. Cell Biol 6, 673–680. [DOI] [PubMed] [Google Scholar]
- Loayza D, and De Lange T (2003). POT1 as a terminal transducer of TRF1 telomere length control. Nature 423, 1013–1018. [DOI] [PubMed] [Google Scholar]
- Marino S, Vooijs M, van Der Gulden H, Jonkers J, and Berns A (2000). Induction of medulloblastomas in p53-null mutant mice by somatic inactivation of Rb in the external granular layer cells of the cerebellum. Genes Dev. 14, 994–1004. [PMC free article] [PubMed] [Google Scholar]
- Martínez P, Thanasoula M, Muñ oz P, Liao C, Tejera A, McNees C, Flores JM, Fernandez-Capetillo O, Tarsounas M, and Blasco MA (2009). Increased telomere fragility and fusions resulting from TRF1 deficiency lead to degenerative pathologies and increased cancer in mice. Genes Dev. 23, 2060–2075. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nandakumar J, Bell CF, Weidenfeld I, Zaug AJ, Leinwand LA, and Cech TR (2012). The TEL patch of telomere protein TPP1 mediates telomerase recruitment and processivity. Nature 492, 285–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Newey PJ, Nesbit MA, Rimmer AJ, Attar M, Head RT, Christie PT, Gorvin CM, Stechman M, Gregory L, Mihai R, et al. (2012). Whole-exome sequencing studies of nonhereditary (sporadic) parathyroid adenomas. J. Clin. Endocrinol. Metab 97, E1995–E2005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Norio P, and Schildkraut CL (2001). Visualization of DNA replication on individual Epstein-Barr virus episomes. Science 294, 2361–2364. [DOI] [PubMed] [Google Scholar]
- Parkinson GN, Lee MP, and Neidle S (2002). Crystal structure of parallel quadruplexes from human telomeric DNA. Nature 417, 876–880. [DOI] [PubMed] [Google Scholar]
- Quesada V, Conde L, Villamor N, Ordóñez GR, Jares P, Bassaganyas L, Ramsay AJ, Bea S, Pinyol M, Martínez-Trillos A, et al. (2011). Exome sequencing identifies recurrent mutations of the splicing factor SF3B1 gene in chronic lymphocytic leukemia. Nat. Genet 44, 47–52. [DOI] [PubMed] [Google Scholar]
- Ramsay AJ, Quesada V, Foronda M, Conde L, Martínez-Trillos A, Villamor N, Rodríguez D, Kwarciak A, Garabaya C, Gallardo M, et al. (2013). POT1 mutations cause telomere dysfunction in chronic lymphocytic leukemia. Nat. Genet 45, 526–530. [DOI] [PubMed] [Google Scholar]
- Renfrew KB, Song X, Lee JR, Arora A, and Shippen DE (2014). POT1a and components of CST engage telomerase and regulate its activity in Arabidopsis. PLoS Genet. 10, e1004738. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Robles-Espinoza CD, Harland M, Ramsay AJ, Aoude LG, Quesada V, Ding Z, Pooley KA, Pritchard AL, Tiffen JC, Petljak M, et al. (2014). POT1 loss-of-function variants predispose to familial melanoma. Nat. Genet 46, 478–481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rudolph KL, Millard M, Bosenberg MW, and DePinho RA (2001). Telomere dysfunction and evolution of intestinal carcinoma in mice and humans. Nat. Genet 28, 155–159. [DOI] [PubMed] [Google Scholar]
- Sfeir A, Kosiyatrakul ST, Hockemeyer D, MacRae SL, Karlseder J, Schildkraut CL, and de Lange T (2009). Mammalian telomeres resemble fragile sites and require TRF1 for efficient replication. Cell 138, 90–103. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Shi J, Yang XR, Ballew B, Rotunno M, Calista D, Fargnoli MC, Ghiorzo P, Bressac-de Paillerets B, Nagore E, Avril MF, et al. ; NCI DCEG Cancer Sequencing Working Group; NCI DCEG Cancer Genomics Research Laboratory; French Familial Melanoma Study Group (2014). Rare missense variants in POT1 predispose to familial cutaneous malignant melanoma. Nat. Genet 46, 482–486. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simpson K, Jones RE, Grimstead JW, Hills R, Pepper C, and Baird DM (2015). Telomere fusion threshold identifies a poor prognostic subset of breast cancer patients. Mol. Oncol 9, 1186–1193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stewart JA, Wang F, Chaiken MF, Kasbek C, Chastain PD, 2nd, Wright WE, and Price CM (2012). Human CST promotes telomere duplex replication and general replication restart after fork stalling. EMBO J. 31, 3537–3549. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Takahashi K, Akiyama H, Shimazaki K, Uchida C, Akiyama-Okunuki H, Tomita M, Fukumoto M, and Uchida T (2007). Ablation of a peptidyl prolyl isomerase Pin1 from p53-null mice accelerated thymic hyperplasia by increasing the level of the intracellular form of Notch1. Oncogene 26, 3835–3845. [DOI] [PubMed] [Google Scholar]
- Takai H, Smogorzewska A, and de Lange T (2003). DNA damage foci at dysfunctional telomeres. Curr. Biol 13, 1549–1556. [DOI] [PubMed] [Google Scholar]
- Tho LM, Libertini S, Rampling R, Sansom O, and Gillespie DA (2012). Chk1 is essential for chemical carcinogen-induced mouse skin tumorigenesis.Oncogene 31, 1366–1375. [DOI] [PubMed] [Google Scholar]
- Tong AS, Stern JL, Sfeir A, Kartawinata M, de Lange T, Zhu XD, and Bryan TM (2015). ATM and ATR signaling regulate the recruitment of human telomerase to telomeres. Cell Rep. 13, 1633–1646. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Trigueros-Motos L (2014). Mutations in POT1 predispose to familial cutaneous malignant melanoma. Clin. Genet 86, 217–218. [DOI] [PubMed] [Google Scholar]
- Vannier JB, Pavicic-Kaltenbrunner V, Petalcorin MI, Ding H, and Boulton SJ (2012). RTEL1 dismantles T loops and counteracts telomeric G4-DNA to maintain telomere integrity. Cell 149, 795–806. [DOI] [PubMed] [Google Scholar]
- Vannier JB, Sandhu S, Petalcorin MI, Wu X, Nabi Z, Ding H, and Boulton SJ (2013). RTEL1 is a replisome-associated helicase that promotes telomere and genome-wide replication. Science 342, 239–242. [DOI] [PubMed] [Google Scholar]
- Vassileva V, Millar A, Briollais L, Chapman W, and Bapat B (2002). Genes involved in DNA repair are mutational targets in endometrial cancers with microsatellite instability. Cancer Res. 62, 4095–4099. [PubMed] [Google Scholar]
- Walne AJ, Vulliamy T, Beswick R, Kirwan M, and Dokal I (2008). TINF2 mutations result in very short telomeres: analysis of a large cohort of patients with dyskeratosis congenita and related bone marrow failure syndromes. Blood 112, 3594–3600. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Walsh KM, Codd V, Rice T, Nelson CP, Smirnov IV, McCoy LS, Hansen HM, Elhauge E, Ojha J, Francis SS, et al. ; ENGAGE Consortium Telomere Group (2015). Longer genotypically-estimated leukocyte telomere length is associated with increased adult glioma risk. Oncotarget 6, 42468–42477. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wan M, Qin J, Songyang Z, and Liu D (2009). OB fold-containing protein 1 (OBFC1), a human homolog of yeast Stn1, associates with TPP1 and is implicated in telomere length regulation. J. Biol. Chem 284, 26725–26731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wu L, Multani AS, He H, Cosme-Blanco W, Deng Y, Deng JM, Bachilo O, Pathak S, Tahara H, Bailey SM, et al. (2006). Pot1 deficiency initiates DNA damage checkpoint activation and aberrant homologous recombination at telomeres. Cell 126, 49–62. [DOI] [PubMed] [Google Scholar]
- Wu P, Takai H, and de Lange T (2012). Telomeric 3° overhangs derive from resection by Exo1 and Apollo and fill-in by POT1b-associated CST. Cell 150, 39–52. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Xin H, Liu D, Wan M, Safari A, Kim H, Sun W, O’Connor MS, and Songyang Z (2007). TPP1 is a homologue of ciliate TEBP-beta and interacts with POT1 to recruit telomerase. Nature 445, 559–562. [DOI] [PubMed] [Google Scholar]
- Ye JZ, Hockemeyer D, Krutchinsky AN, Loayza D, Hooper SM, Chait BT, and de Lange T (2004). POT1-interacting protein PIP1: a telomere length regulator that recruits POT1 to the TIN2/TRF1 complex. Genes Dev. 18, 1649–1654. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yin B, Yang-Iott KS, Chao LH, and Bassing CH (2011). Cellular contextdependent effects of H2ax and p53 deletion on the development of thymic lymphoma. Blood 117, 175–185. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhang J, Jima D, Moffitt AB, Liu Q, Czader M, Hsi ED, Fedoriw Y, Dunphy CH, Richards KL, Gill JI, et al. (2014). The genomic landscape of mantle cell lymphoma is related to the epigenetically determined chromatin state of normal B cells. Blood 123, 2988–2996. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zhong FL, Batista LF, Freund A, Pech MF, Venteicher AS, and Artandi SE (2012). TPP1 OB-fold domain controls telomere maintenance by recruiting telomerase to chromosome ends. Cell 150, 481–494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zimmermann M, Kibe T, Kabir S, and de Lange T (2014). TRF1 negotiates TTAGGG repeat-associated replication problems by recruiting the BLM helicase and the TPP1/POT1 repressor of ATR signaling. Genes Dev. 28, 2477–2491. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.