Abstract
Charcot arthropathy is an infrequent condition that primarily involves the foot and ankle; rarely, it has been reported to affect the knee. Risk factors for Charcot arthropathy are well described with diabetes being the most common cause. Idiopathic Charcot arthropathy without a secondary etiology is extremely rare, with only a few cases described involving the foot and shoulder. Clinically, idiopathic Charcot arthropathy presents a notable challenge because delayed diagnosis can lead to surgical complications and advancement of joint destruction. We report idiopathic Charcot arthropathy of the knee presenting as a bicondylar tibial plateau fracture successfully managed with total knee arthroplasty after failed open reduction internal fixation. We diagnosed the patient when the clinical/surgical presentation was indicative of Charcot arthropathy and after excluding all other diagnoses. This previously unreported case describes the complexity of idiopathic Charcot arthropathy with subsequent fractures and highlights the importance of patient history, presentation, and surgical intervention.
Charcot arthropathy is a relatively rare and poorly understood condition. In contrast to cases affecting the foot and ankle, Charcot arthropathy of the knee is an exceedingly rare condition, with <25 cases reported in the literature. Cases of Charcot arthropathy joints not associated with previously described risk factors are even rarer. Idiopathic Charcot arthropathy involving the midfoot1 and elbow2 have been described, and although acquired Charcot arthropathy of the knee secondary to spine surgery has been documented in case reports,3 in a review of the literature, no cases of idiopathic Charcot arthropathy affecting the knee were found. Given the rarity of Charcot arthropathy of the knee in general, treatment is still controversial, with the trend toward total knee arthroplasty (TKA).4 We report a case of idiopathic Charcot arthropathy affecting the knee presenting as a complicated bicondylar tibial plateau fracture managed with TKA after failed open reduction internal fixation (ORIF).
Case Report
A 62-year-old highly active white man presented to the orthopaedic office without ambulatory assistance because of left knee instability and mild pain after a minor misstep on uneven terrain while hiking more than 652 miles on the Appalachian Trail 3 weeks before. The patient had reported minor knee discomfort several days before his hike. The misstep resulted in an acute onset of increased knee pain and a new sensation of instability. The patient had no notable medical history, including diabetes, osteoarthritis, and neuropathy. He denied any history of knee/joint pain or instability before his hiking trip, denied tobacco use, and rarely used alcohol. Imaging performed at this time revealed a left bicondylar tibial plateau fracture (Figure 1). Given this, and his level of activity, we postulated that the fracture was a progression from stress fracture rather than Charcot arthropathy due to the patient's minimal pain, despite the severity of his injury on presentation. After discussing treatment options, the patient underwent ORIF with knee arthroscopy and uniplanar knee spanning external fixator placement. Knee arthroscopy relieved notable diffuse synovitis and medial and lateral meniscus tears with medial joint line instability that was indicated by probing of the cartilage, as well as lateral joint line depression (>2 mm). We also observed a large defect in the medial femoral condyle (1.5 cm × 1.5 cm) on the lateral aspect of the medial femoral condylar weight-bearing surface.
Figure 1.
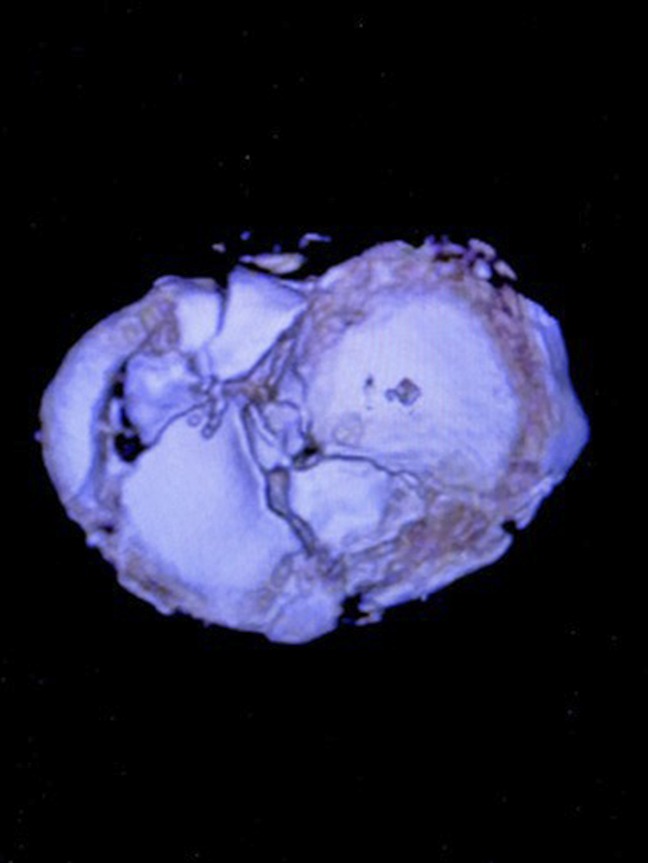
Axial three-dimensional CT reconstruction indicating bicondylar tibial plateau fracture with notable medial comminution and deficit.
After 2 months, the patient underwent removal of the external fixator and manipulation under anesthesia. Intraoperatively, the knee was stable through flexion, extension, and varus and valgus stress and exhibited near-normal range of motion.
The patient returned 7 months after the ORIF with continued pain and subsequent delayed tibial plateau union and fixation failure. He then underwent an iliac crest bone graft with revision ORIF of the tibial plateau fracture, medial joint line elevation, bone graft, and insertion of bone stimulator. Over the next 10 months, pain and failure of fixation progressed with advancement of osteoarthritis. Because of failure of fixation with continued nonunion of the tibial plateau, along with notable degenerative advancement, we elected to perform TKA. Intraoperatively, the knee showed extensive posteromedial bone loss from the subsided tibial plateau fracture with sclerotic bone and fibrous nonunion of the bicondylar tibial plateau fracture with continued diffuse synovitis (Figure 2). We removed the existing implants and completed successful TKA with augments (Figure 3). The patient had no further postoperative complications.
Figure 2.

Intraoperative photograph indicating synovitis and advancement of osteoarthritis.
Figure 3.

Postoperative AP radiograph after successful total knee arthroplasty.
Discussion
In most bicondylar tibial plateau fractures, primary or external fixation with delayed ORIF is the preferred treatment because surgical complications remain relatively low, with implant failure and nonunion reported at 0.4% and 0.7%, respectively.5 In highly active individuals without a history of osteoarthritis, stress fractures have been implicated as a cause of bicondylar tibial plateau fractures,6 which is consistent with the demographics of the patient reported in this study. However, because of the patient's presentation and treatment course, a stress fracture as the etiology of his bicondylar tibial plateau fracture was less consistent than idiopathic Charcot arthropathy of the knee. Ambulation despite a bicondylar tibial plateau fracture, significant synovitis, delayed union or nonunion, extensive rapid progression of osteoarthritis, and repeated surgical complications necessitating TKA are considered to be more consistent with Charcot arthropathy. The pathophysiology of Charcot arthropathy is not fully understood. Autonomic dysfunction and repetitive microtrauma due to decreased nociception are believed to contribute to the development of Charcot arthropathy.1 The risk factors have been well described. Diabetes mellitus has been extensively demonstrated as the most common risk factor for Charcot arthropathy. Other factors include tertiary syphilis, leprosy, alcoholism, syringomyelia, lacunar infarcts, and hereditary cerebral and cerebellar atrophy. The presentation of Charcot arthropathy remains similar, with distinct presentation in the affected joints. Pain of varying degrees and instability are common presenting symptoms of Charcot arthropathy. The degree of pain does not correlate with the degree of joint destruction.7 Patients often present with varying degrees of joint effusion, erythema, and local temperature change depending on the stage of presentation.
In the current case, we diagnosed a Charcot arthropathy knee as a diagnosis of exclusion. We ruled out other diagnoses based on a lack of evidence of septic or microcrystalline arthritis, or any additional neurologic deficits or symptoms suggesting a CNS lesion. The patient's presentation of minimal pain and new complaints of instability is consistent with a previously reported case of Charcot arthropathy of the knee with fractures of the tibial plateau in a diabetic patient.8 Furthermore, the diffuse synovitis seen is also consistent with the appearance of Charcot arthropathy of the knee reported previously.9 High complication rates with ORIF and arthrodesis in patients with Charcot arthropathy have also been described.8
Charcot arthropathy affecting the knee is a rare condition, even in those with predisposing factors to Charcot arthropathy joints. Cases of idiopathic Charcot arthropathy joints are seldom seen; however, early diagnosis can be crucial to successful management. The current case indicates that even with notable confounding factors, and with careful consideration of the patient's presentation and medical history, Charcot arthropathy may have several key identifiers allowing for detection early in the disease course. In healthy, highly active adults, idiopathic Charcot arthropathy can markedly increase the risk for debilitating injuries. In patients presenting with an unusually high tolerance to pain and notable joint involvement, neurogenic arthropathy should be considered despite a lack of established risk factors. Furthermore, this case indicates that in instances of idiopathic Charcot arthropathy of the knee with a bicondylar tibial plateau fracture, ORIF may have an increased chance of failure; as with the current convention for Charcot arthropathy knees of other etiologies, TKA is becoming a preferred treatment.10
Footnotes
None of the following authors or any immediate family member has received anything of value from or has stock or stock options held in a commercial company or institution related directly or indirectly to the subject of this article: Dr. L. F. Hanson, Mr. C. G. Hanson, and Mr. Barner.
References
- 1.Bariteau J, Tenenbaum S, Rabinovich A, Brodsky J: Charcot arthropathy of the foot and ankle in patients with idiopathic neuropathy. Foot Ankle Int 2014;35:996-1001. [DOI] [PubMed] [Google Scholar]
- 2.Blanford AT, Keane SP, McCarty DJ, Albers JW: Idiopathic Charcot joint of the elbow. Arthritis Rheum 1978;21:723-726. [DOI] [PubMed] [Google Scholar]
- 3.Hayashi S, Okada T, Horita K: Bilateral TKA for Charcot arthropathy associated with multiple levels of spinal canal stenosis: A case report and review of literature. J Orthop 2017;14;77-80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zeng M, Xie J, Hu Y: Total knee arthroplasty in patients with Charcot joints. Knee Surg Sports Traumatol Arthrosc 2016;24:2672-2677. [DOI] [PubMed] [Google Scholar]
- 5.Kugelman D, Qatu A, Haglin J, Leucht P, Konda S, Egol K: Complications and unplanned outcomes following operative treatment of tibial plateau fractures. Injury 2017;48:2221-2229. [DOI] [PubMed] [Google Scholar]
- 6.An V, van den Broek M, Oussedik S: Subchondral insufficiency fracture in the lateral compartment of the knee in a 64-year-old Marathon runner. Knee Surg Relat Res 2017;29:325-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Babazadeh S, Stoney J, Lim K, Choomg P: Arthroplasty of a Charcot knee. Orthop Rev (Pavia) 2010;2:e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Goetti P, Gallusser N, Borens O: Bilateral diabetic knee neuroarthropathy in a forty-year-old patient. Case Rep Orthop 2016;2016:1-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kucera T, Urban K, Sponer P: Charcot arthropathy of the knee: A case-based review. Clin Rheumatol 2011;30:425-428. [DOI] [PubMed] [Google Scholar]
- 10.Zeng M, Xie J, Hu Y: Total knee arthroplasty in patients with Charcot joints. Knee Surg Sports Traumatol Arthrosc 2016;24:2672-2677. [DOI] [PubMed] [Google Scholar]


