Abstract
Background:
Nonunion of long-bone fractures is difficult to treat, especially when the bones are osteoporotic or there is a large bone gap as a result of repeated failure of the metallic nails or implants. In such cases, the use of an autologous intramedullary fibular strut graft may be a viable treatment option.
Methods:
Twenty-two patients with a complex nonunion of the shaft of the femur, humerus, or tibia were managed with a free autologous fibular strut graft for intramedullary fixation with use of closed or open methods. All patients had evidence of moderate to severe local osteoporosis and had a bone gap ranging from 4 to 20 mm. Nineteen patients had had 1 to 4 prior operations. The mean age was 51.5 years. The duration of nonunion ranged from 9 months to 4 years.
Results:
The mean time to union was 17 weeks (range, 8 to 26 weeks), and the mean duration of follow-up was 4 years (range, 6 months to 17 years). All but 2 patients had healing at the time of the latest follow-up.
Conclusions:
The identification of a viable option for the treatment of difficult nonunion in osteoporotic bones has been a challenge. The insertion of a free autologous intramedullary fibular strut graft provided mechanical stability, and osteogenesis occurred inside the medullary canal of the host bone.
Level of Evidence:
Therapeutic Level IV. See Instructions for Authors for a complete description of levels of evidence.
Treatment of complex nonunion of the long bones is a challenge1-5. A variety of operative techniques, including those involving intramedullary nails and compression plates with bone grafts, have been tried, with variable results2-4. The concept of biological internal fixation for the treatment of nonunion is still developing, with emphasis on the biomechanics of stability, the biology of the blood supply, and the impact on clinical use3,5. Biological fixation has been advocated as a way to induce union by promoting osteogenesis3,6. The aim is to produce the best biological conditions for healing rather than to achieve absolute stability of fixation.
New technology provides potential benefits related to the surgical treatment of nonunion in osteoporotic bone5,7,8. With the increasing incidence of osteoporosis, the stabilization of fractures in patients with soft bones is a priority9-11. Osteopenia and severe soft-tissue damage with extensive skin scars increase the likelihood of repeated failure of metallic implants and/or persistent disuse osteoporosis, which can result in the widening of the medullary canal of long bones such as the femur, tibia, and humerus6,12-16.
A metallic nail or plate of any type may not provide adequate fixation in an ailing bone with severe osteopenia and a wide medullary canal. To achieve union of osteopenic bone, a stimulating factor in the form of an autologous bone graft may encourage the initiation of osteogenesis17-19.
In the present report, a simple biological technique is proposed in which a free fibular strut graft is used as a biological intramedullary nail for the treatment of complex nonunion.
Materials and Methods
Twenty-two patients with a complex nonunion of the humerus (8 patients), femur (9 patients), or tibia (5 patients) were managed with intramedullary fibular fixation between1992 and 2011. The study group included 15 male patients and 7 female patients ranging from 12 to 78 years of age. The mean time from fracture to treatment of nonunion was 17.5 months (range, 9 to 48 months). Ten patients (5 with a humeral nonunion and 5 with a femoral nonunion) were managed with a closed technique and 12 were managed with an open technique (Table I). All patients had evidence of moderate to severe local osteoporosis and had a bone gap ranging from 4 to 20 mm. The mean time to union was 17 weeks (range, 8 to 26 weeks), and the mean duration of follow-up was 4 years (range, 6 months to 17 years).
TABLE I.
Patient Characteristics
| Case | Sex, Age (yr) | Nonunion Site | No. of Prior Procedures | Duration of Nonunion (mo) | Operative Technique* | Time to Union (wk) | Complications | Notes |
| 1 | M, 12 | Tibia | 1 | 12 | Fibular strut graft | 20 | — | Severe osteoporosis with gap |
| 2 | M, 52 | Femur (middle) | 2 | 36 | Fibular strut graft + K wire | 14 | — | — |
| 3 | M, 56 | Femur (proximal) | 4 | 48 | Fibular strut graft + K wire | 13 | — | Nail plate applied twice before and removed each time |
| 4 | M, 62 | Humerus (middle) | 1 | 24 | Fibular strut graft | 8 | — | — |
| 5 | M, 33 | Humerus (middle) | 1 | 24 | Fibular strut graft + K wire | 10 | — | — |
| 6 | M, 44 | Femur (middle) | 2 | 16 | Fibular strut graft + K wire | 8 | Superficial infection | — |
| 7 | M, 59 | Humerus (proximal) | 0 | 9 | Fibular strut graft | 17 | — | Earlier conservative treatment had failed |
| 8 | F, 47 | Femur (middle) | 2 | 18 | Fibular strut graft + K wire | 12 | — | — |
| 9 | F, 39 | Tibia (middle) | 1 | 17 | Fibular strut graft + K wire | 16 | — | — |
| 10 | M, 46 | Femur (distal) | 1 | 16 | Fibular strut graft | 19 | — | Bilateral |
| 11 | M, 55 | Tibia (middle) | 1 | 15 | Fibular strut graft | 22 | — | — |
| 12 | M, 49 | Femur (proximal) | 1 | 13 | Fibular strut graft + K wire | 26 | — | — |
| 13 | F, 35 | Humerus (middle) | 3 | 18 | Fibular strut graft + K wire | Failed | Superficial infection failed | Needed plating and bone-grafting |
| 14 | M, 58 | Femur (middle) | 0 | 15 | Fibular strut graft with screws | 14 | — | Conservative treatment had failed |
| 15 | F, 35 | Humerus (middle) | 1 | 14 | Fibular strut graft | 18 | — | — |
| 16 | M, 72 | Femur (middle) | 2 | 18 | Fibular strut graft + K wire | 22 | — | — |
| 17 | M, 68 | Tibia (middle) | 1 | 11 | Fibular strut graft | 24 | Superficial infection | — |
| 18 | F, 78 | Humerus (middle) | 2 | 19 | Fibular strut graft | Failed | Failed | Needed plating and bone-grafting |
| 19 | F, 64 | Humerus (proximal) | 1 | 14 | Fibular strut graft + K wire | 20 | — | — |
| 20 | M, 53 | Femur (middle) | 1 | 9 | Fibular strut graft + K wire | 16 | — | — |
| 21 | M, 64 | Tibia (middle) | 0 | 9 | Fibular strut graft + K wire | 22 | — | Conservative treatment had failed |
| 22 | F, 54 | Humerus (distal) | 1 | 11 | Fibular strut graft | 14 | — | — |
K wire = Kirschner wire.
Radiographs were made in each case. All fractures were initially closed. Three patients had radial nerve palsy, and 5 had Sudeck atrophy of the hand. Twelve patients had had 1 prior procedure, 5 had had 2, 1 had had 3, and 1 had had 4; the remaining 3 patients had not had any prior operative procedures but still had a wide medullary canal (Table I). At the time of the first examination, all patients had pain and considerable disability. Four patients had obvious deformity in the arm (2 patients) or leg (2 patients) that could be corrected clinically. No additional cancellous grafting was attempted for any patient.
Surgical Technique
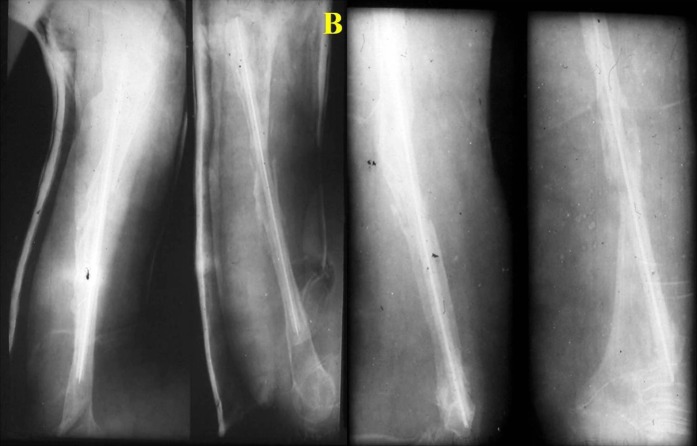
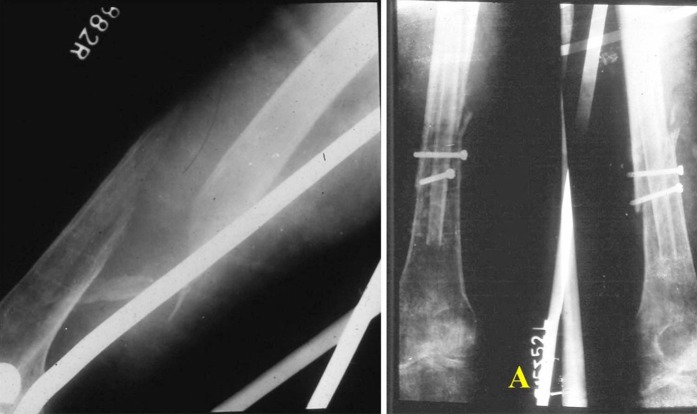
The basic principles are similar to those of metallic nail fixation. In cases in which the bone fragments are aligned, closed fibular fixation is recommended (Figs. 1-A, 1-B, and 1-C).
Figs. 1-A, 1B, and 1-C Radiographs of the femur in a 54-year-old man, illustrating the principles of the technique.
Fig. 1-A.

Anteroposterior radiographs showing a subtrochanteric nonunion after 4 surgical procedures, including 2 attempted applications (and subsequent removals) of plate and nail fixation.
Fig. 1-B.
Anteroposterior radiographs made 3 weeks after treatment with a fibular graft, showing signs of healing. At the time of the procedure, a Kirschner wire was passed through the fibular graft, and the graft was then inserted into the femur. Black and white arrows indicate the location of the fibular strut in the femur.
Fig. 1-C.

Radiographs made 11 weeks postoperatively, showing complete union.
First, the host site is prepared with a closed or open technique. The required autologous fibular strut (with a length of 10 to 20 cm) is removed, with the distal 8 to 9 cm of the fibula being left in place for ankle stability. If a long strut is required, the head of the fibula can also be taken after protecting the peroneal nerve. This fibular strut, or “biological nail,” is fashioned to fit the host medullary canal. The biological strut should be inserted into the host bone as early as possible to maximize its viability. If the surgeon thinks that the fibular strut should be strengthened, a Kirschner wire can be passed through the medullary canal of the fibular strut. Following procedures involving the femur or tibia, the extremity is supported with use of a Thomas splint. Following procedures involving the humerus, the arm is initially supported with a U-cast.
For closed insertion of the fibular strut into the humerus or femur, a 3-cm incision is made over the greater tuberosity or the greater trochanter. If required, the medullary canal is minimally reamed. An appropriately sized fibular strut is removed subperiosteally and is shaped to be driven first into the proximal fragment and then into the distal fragment after the fracture has been stabilized. In cases involving a relatively narrow medullary canal, the edges of the fibular graft are shaved before being inserted. The full length of the graft is inserted into the proximal fragment in a retrograde fashion and then is advanced into the distal fragment like a metallic nail to the extent that half of the strut is placed on either side of the fracture.
In the tibia, fixation can be attempted with an open method, with the nonunion site minimally exposed. The strut graft is passed on the proximal side and can be slowly inserted into the distal fragment after the nonunion is reduced. The lower limb is initially supported with a splint.
Advantages of the Technique
This technique is associated with several advantages. First, the technique is simple and is based on the principles of Kuntscher nailing. Second, the technique involves bone-in-bone fixation and is totally biological. As a result, the large contact area between the fibula and the endosteal surface of the host bone facilitates early union and strengthens the osteopenic host bone. Third, the autologous fibular strut also provides much-needed osteogenesis at the site of the nonunion and throughout the length of the graft in the parent bone. Fourth, no reaming is typically required. The triflanged fibula adequately engages both of the nonunion fragments, so no additional fixation is necessary. Once incorporated, the fibular strut does not require removal. Fifth, if it is considered necessary to strengthen the fibula, a Kirschner wire can be inserted into the fibula before the fibula is inserted into the parent bone. Sixth, the periosteum of the host bone is minimally disturbed.
Results
The results of the treatment were assessed on the basis of clinical and radiographic evidence of union, time to union, and the function of the extremity. All but 2 nonunions healed; the mean time to union was 17 weeks (range, 8 to 26 weeks). Two humeral nonunion had failed to unite and required plating and autologous bone-grafting. Both failures occurred in earlier in the study following procedures in which no Kirshner wire was inserted into the fibular graft.
In 3 cases (2 involving the humerus and 1 involving the femur), the fibula could be inserted in the distal fragment only for nearly 2 cm. However, a Kirschner wire was passed through the fibula down the whole length of the bone. Suitable splints were applied for a few days. In all 3 cases, union was achieved in 4 months. Complications included 1 case of transient radial nerve palsy and 2 cases of transient peroneal nerve palsy. All 3 patients improved subsequently. Three cases of superficial infection (1 each in the humerus, femur, and tibia) were treated successfully.
At the time of the latest follow-up, 2 patients had a slightly limited range of motion of the shoulder. The mean range of elbow flexion-extension was from 32° to 110°, and the mean range of forearm rotation was from 80° of pronation to 70° of supination. Seventeen of the 22 patients had returned to work. Fifteen patients had no pain, 5 patients had occasional pain that was relieved with analgesics, and the remaining 2 patients had pain and mobility at the nonunion site that were successfully treated with plate fixation and autologous cancellous bone.
Discussion
Open internal fixation may contribute to injury of the soft-tissue envelope. A high degree of skill and expertise is required to minimize the biological complications following traumatic and iatrogenic osteonecrosis13,20. Nonunion of the long bones is a difficult condition to treat and is fraught with complications21. After repeated implant failures, nonunions are resistant to treatment11,18. In such cases, the bone is often osteoporotic, with a large gap between the bone segments, and fixation is usually difficult to achieve6,12,15,22-25.
The advent of “biological internal fixation” is an important development in the surgical treatment of fractures and nonunions26. Ordinarily, a metallic nail acts as an internal splint and does not abolish motion completely, and the fracture heals through peripheral callus formation14. Even the best implants may not be adequate in severely osteoporotic fractured bone with wide medullary canals and a thin cortex11,16. Cementation has been advocated as a way to bridge the fracture gap and to fill areas of bone deficiency; however, it inhibits osteogenesis, and loosening is known to occur over time1,3,9. The use of a small fibular strut with compression plating has been reported to provide better fixation3,24.
In this technique, the fibula functions as a triflanged nail and engages the host bone firmly. In bones with a wide medullary canal, reaming is not necessary for the placement of the fibular strut21. Another advantage is that the periosteum of the host bone is undisturbed, as with closed internal fixation.
Reaming, if required, may assist in establishing contact between the endosteum of the host bone and the fresh autologous nail graft. The 3 borders of the fibula fix firmly to the inner cortices of the fractured fragments. In the present study, union was achieved even when there was damage to the soft tissue surrounding the bone gap and there was potential need for amputation (Figs. 2-A, 2-B, and 2-C). Evidently, the intramedullary graft sufficiently reduced the rotational and other undesirable movements that are sometimes observed in association with nonlocking intramedullary nails. Our technique has some of the advantages of both closed and open fixation. In cases in which the nonunion had occurred after the failure of a metallic nail, the fragments were in alignment and the fibular strut could be easily inserted into the same track of the parent bone as the metallic nail after minimal reaming with use of a closed method (Figs. 3-A through 3-E). With this technique, there is no need to use additional screws or a plate because the strong fibular strut can be hammered into the parent bone. If desired, a Kirschner wire can be inserted into the fibular graft, creating further support and anchorage to the repaired bone (Figs. 4-A and 4-B).
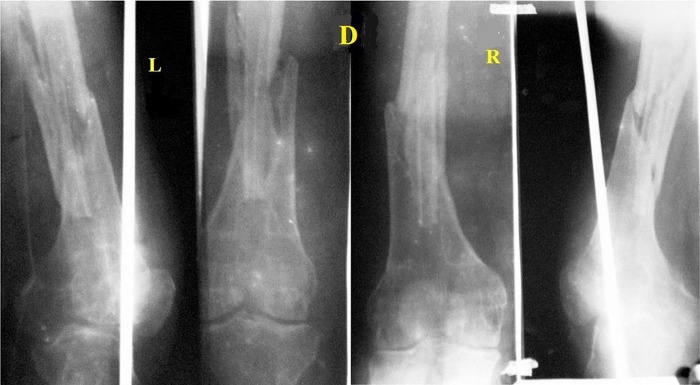
Figs. 2-A, 2-B, and 2-C A 12-year-old boy who was managed with an autologous fibular strut graft for the treatment of a complete circumferential injury of the distal aspect of the lower limb.
Fig. 2-A.

Preoperative photographs.
Fig. 2-B.
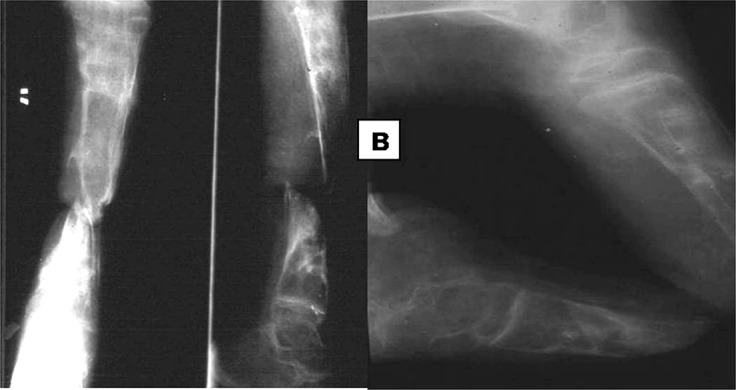
Anteroposterior (left and middle panels) and lateral (right panel) radiographs showing gap nonunion with severe osteoporosis.
Fig. 2-C.
Anteroposterior and lateral radiographs (left) and clinical photographs (right), made 18 months after the insertion of the fibular strut. Before surgery a full-thickness skin graft had been attempted. The clinical photographs show that the patient had an equinus deformity, which compensated for the limb-shortening on the involved side. The patient was satisfied with the results of treatment and refused any further surgical intervention.
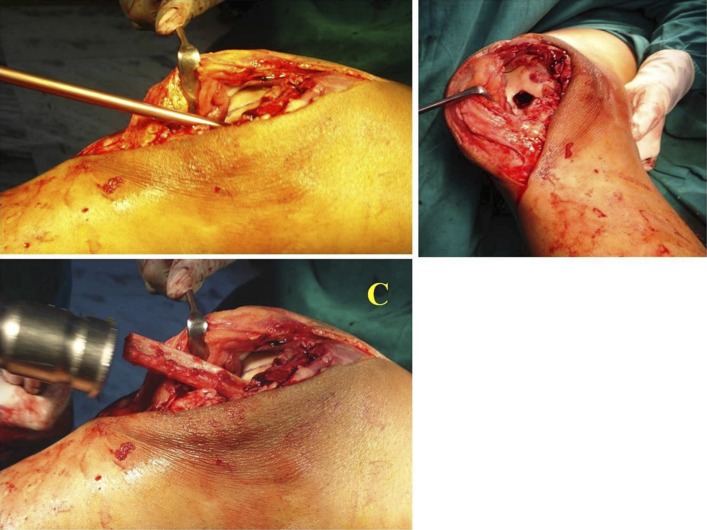
Figs. 3-A through 3-E A 45-year-old man with bilateral symmetrical fractures of the distal third of the femur. Figs. 3-A and 3-B Radiographs made after treatment with interlocking nails. The fractures have not yet united and the nails are projecting into the joint. The patient was subsequently managed with removal of the nails and the insertion of an autologous fibular strut graft.
Fig. 3-A.

Fig. 3-B.

Fig. 3-C.
Intraoperative photographs showing the host site and insertion of the strut graft.
Fig. 3-D.
Fig. 3-E.
Radiographs made 10 weeks after placement of the fibular struts at the fracture site.
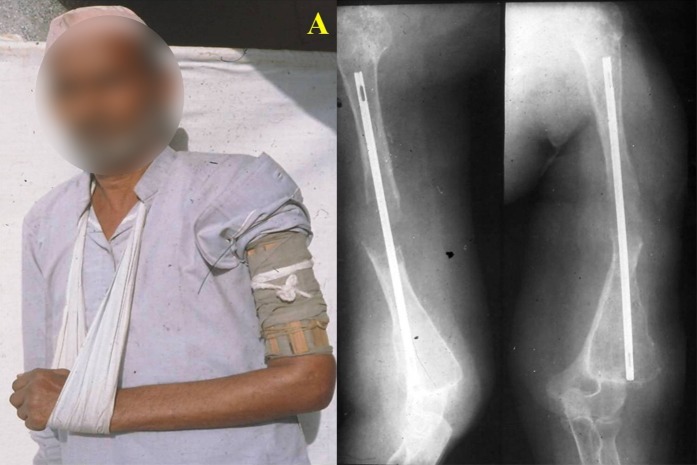
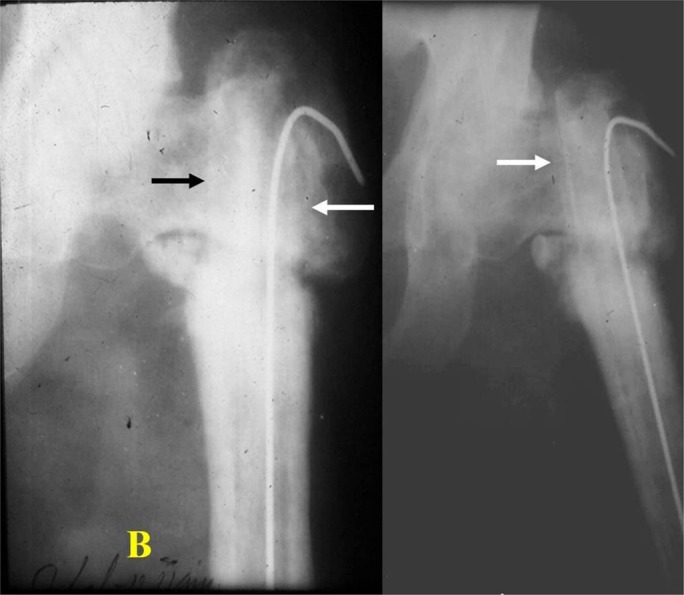
Fig. 4-A.
Clinical photograph and radiographs of a 64-year-old man with a humeral fracture who initially received local treatment and was subsequently treated with use of a Kuntscher nail. The radiographs show a loose Kuntscher nail and gross osteoporosis.
Fig. 4-B.
Immediate postoperative (left) and follow-up (right) radiographs made after the patient was managed with a fibular strut graft and a long Kirschner wire for the treatment of nonunion of the osteoporotic humeral shaft. The follow-up radiographs, made at 11 weeks, show union at the fracture site.
Free fibular grafts are known to be at risk for necrosis resulting in absorption and non-incorporation to the host bone2,22. The fibular struts were inserted immediately after removal from the donor site in order to encourage the retention of viable properties7,17,19,27. It has been reported that if the autologous bone graft is fixed to the recipient bone immediately after it is retrieved, the osteogenic cells on and in the graft survive17,24. Immediate fixation of the graft at the recipient site allows the cells in and over the graft to draw oxygenation and nutrition from the blood, thereby preserving their osteogenic properties18,23,28. Moreover, with this type of intramedullary fixation, the fibular strut is in contact with the viable parent bone throughout the length of the graft, with intact osteogenic potentials.
The large contact area between the fibular strut graft and the host bone encourages union. With a firmly fixed autologous graft, compression may not be necessary. However, in cases involving a very wide medullary canal and a thin cortex, screws can be utilized to achieve 4-cortex fixation (Figs. 5-A and 5-B). These minor modifications to the basic technique can be employed when necessary.
Figs. 5-A and 5-B A 59-year-old man was managed with an autologous fibular strut graft for the treatment of an oblique fracture of the distal third of the femur with severe osteoporosis.
Fig. 5-A.
Preoperative and immediate postoperative radiographs. During the procedure, an autologous fibular graft was inserted at the fracture site; however, because the medullary canal was very wide, the fibular strut was a loose fit. The site was fixed with 2 cortical screws to achieve 4-cortex fixation.
Fig. 5-B.
Radiographs demonstrating fracture healing at 10 weeks.
In the present study, 20 of 22 nonunions healed after treatment with a biological intramedullary nail, without additional intervention. Bone healing occurred with adequate mechanical stability and a continuous process of osteogenesis7. This technique is most appropriate for the treatment of established nonunions, especially when the bone is osteopenic and when previous fixation methods have failed (Figs. 4-A and 4-B). The host bone length was maintained, early mobilization was possible, and union occurred.
Note
The author thanks all of his assistants over the span of 5 decades, which was the period for the preparation of this study. The author also thanks Mr. Mohit Kumar for his secretarial assistance.
Footnotes
Investigation performed at Mirpur Institute of Medical Sciences, Rewari, Haryana, India
Disclosure: There was no external funding for this study. The Disclosure of Potential Conflicts of Interest form is provided with the online version of the article (http://links.lww.com/JBJSOA/A48).
References
- 1.Trotter DH, Dobozi W. Nonunion of the humerus: rigid fixation, bone grafting, and adjunctive bone cement. Clin Orthop Relat Res. 1986. March;(204):162-8. [PubMed] [Google Scholar]
- 2.Rosen H. The treatment of nonunions and pseudarthroses of the humeral shaft. Orthop Clin North Am. 1990. October;21(4):725-42. [PubMed] [Google Scholar]
- 3.Wright TW, Miller GJ, Vander Griend RA, Wheeler D, Dell PC. Reconstruction of the humerus with an intramedullary fibular graft. A clinical and biomechanical study. J Bone Joint Surg Br. 1993. September;75(5):804-7. [DOI] [PubMed] [Google Scholar]
- 4.Lynch JR, Taitsman LA, Barei DP, Nork SE. Femoral nonunion: risk factors and treatment options. J Am Acad Orthop Surg. 2008. February;16(2):88-97. [DOI] [PubMed] [Google Scholar]
- 5.Somford MP, van den Bekerom MPJ, Kloen P. Operative treatment for femoral shaft nonunions, a systematic review of the literature. Strategies Trauma Limb Reconstr. 2013. August;8(2):77-88. Epub 2013 Jul 27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Jupiter JB. Complex non-union of the humeral diaphysis. Treatment with a medial approach, an anterior plate, and a vascularized fibular graft. J Bone Joint Surg Am. 1990. June;72(5):701-7. [PubMed] [Google Scholar]
- 7.Cannada LK. Viable bone and circulatory factors required for survival of bone grafts [table of contents.]. Orthop Clin North Am. 2010. January;41(1):5-13. [DOI] [PubMed] [Google Scholar]
- 8.Maheshwari P, Maheshwari P. Non-union distal femur fracture: causes and management options. Trauma Int. 2016. Jan-Apr;2(1):28-33. [Google Scholar]
- 9.Cameron HU, Jacob R, Macnab I, Pilliar RM. Use of polymethylmethacrylate to enhance screw fixation in bone. J Bone Joint Surg Am. 1975. July;57(5):655-6. [PubMed] [Google Scholar]
- 10.Epps CH, Jr, Grant RE. Fractures of the shaft of the humerus. In: Rockwood CA. Jr, Green DP, Bucholz RW, editors. Rockwood and Green’s fractures in adults. 3rd ed Philadelphia: J.B. Lippincott; 1991. p 843-69. [Google Scholar]
- 11.Li XK, Wang HQ, Wei YY, Wu ZX; LiXK. Treatment of nonunions of humeral fractures with interlocking intramedullary nailing. Chin J Traumatol. 2008. December;11(6):335-40. [DOI] [PubMed] [Google Scholar]
- 12.Ring D, Jupiter JB, Sanders RA, Quintero J, Santoro VM, Ganz R, Marti RK. Complex nonunion of fractures of the femoral shaft treated by wave-plate osteosynthesis. J Bone Joint Surg Br. 1997. March;79(2):289-94. [DOI] [PubMed] [Google Scholar]
- 13.Mukhopadhaya J, Shivapuri S. Functional outcome after open reduction and internal fixation for symptomatic delayed union and nonunion after fracture clavicle: A series of 31 cases. Indian J Orthop. 2007. July;41(3):209-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Vidyadhara S, Vamsi K, Rao SK, Gnanadoss JJ, Pandian S. Use of intramedullary fibular strut graft: a novel adjunct to plating in the treatment of osteoporotic humeral shaft nonunion. Int Orthop. 2009. Aug; 33(4):1009-14. Epub 2008 Jun 18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Tarr RR, Wiss DA. The mechanics and biology of intramedullary fracture fixation. Clin Orthop Relat Res. 1986. November;(212):10-7. [PubMed] [Google Scholar]
- 16.Esterhai JL, Jr, Brighton CT, Heppenstall RB, Thrower A, EsterhaiJLJr Nonunion of the humerus. Clinical, roentgenographic, scintigraphic, and response characteristics to treatment with constant direct current stimulation of osteogenesis. Clin Orthop Relat Res. 1986. October;(211):228-34. [PubMed] [Google Scholar]
- 17.Healy WL, White GM, Mick CA, Brooker AF, Jr, Weiland AJ. Nonunion of the humeral shaft. Clin Orthop Relat Res. 1987. June;(219):206-13. [PubMed] [Google Scholar]
- 18.Ray RD. Vascularization of bone grafts and implants. Clin Orthop Relat Res. 1972. September;87(87):43-8. [PubMed] [Google Scholar]
- 19.Schuh R, Panotopoulos J, Puchner SE, Willegger M, Hobusch GM, Windhager R, Funovics PT. Vascularised or non-vascularised autologous fibular grafting for the reconstruction of a diaphyseal bone defect after resection of a musculoskeletal tumour. Bone Joint J. 2014. September;96-B(9):1258-63. [DOI] [PubMed] [Google Scholar]
- 20.Yadav SS. Radical resection of bone tumours and reconstruction by autologous bone grafting. Indian J Orthop. 1980;14(2):150-4. [Google Scholar]
- 21.Yadav SS. Observations on enbloc resection and reconstruction of malignant bone tumours. Indian J Cancer. 1981. September;18(3):206-10. [PubMed] [Google Scholar]
- 22.Yadav SS. Dual-fibular grafting for massive bone gaps in the lower extremity. J Bone Joint Surg Am. 1990. April;72(4):486-94. [PubMed] [Google Scholar]
- 23.Marino JT, Ziran BH. Use of solid and cancellous autologous bone graft for fractures and nonunions. Orthop Clin North Am. 2010. January;41(1):15-26. [DOI] [PubMed] [Google Scholar]
- 24.Livani B, Belangero W, Medina G, Pimenta C, Zogaib R, Mongon M. Anterior plating as a surgical alternative in the treatment of humeral shaft non-union. Int Orthop. 2010. October;34(7):1025-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Trader JE, Johnson RP, Kalbfleisch JH. Bone-mineral content, surface hardness, and mechanical fixation in the human radius. A correlative study. J Bone Joint Surg Am. 1979. December;61(8):1217-20. [PubMed] [Google Scholar]
- 26.Brown CR, Boden SD. Fracture repair and bone grafting. In: Fischgrund JS, editor. Orthopaedic knowledge update 9. Rosemont: AAOS; 2008. p 13-22. [Google Scholar]
- 27.Khan SN, Cammisa FP, Jr, Sandhu HS, Diwan AD, Girardi FP, Lane JM. The biology of bone grafting. J Am Acad Orthop Surg. 2005. Jan-Feb;13(1):77-86. [PubMed] [Google Scholar]
- 28.Yadav SS. Bridging of large skeletal defects by twin fibular grafts supported by L-plate fixation. Orthopaedics (Int Ed). 1995;3(3):213-21. [Google Scholar]