Abstract
Background:
Patients with acetabular dysplasia often have abnormal femoral and acetabular version. The effect of combined femoral and acetabular version on clinical outcomes after periacetabular osteotomy for the treatment of acetabular dysplasia remains unclear. The purposes of the present study were (1) to evaluate the association of combined femoral and acetabular version with clinical outcome after periacetabular osteotomy and (2) to investigate the association of femoral version independently with clinical outcome after periacetabular osteotomy.
Methods:
We retrospectively reviewed the records for 92 consecutive patients (95 hips) who had undergone periacetabular osteotomy for the treatment of symptomatic acetabular dysplasia. The patient cohort comprised 85 females and 7 males with a mean age of 38.9 years at the time of surgery. The mean duration of follow-up was 4.8 years (range, 2.0 to 7.2 years). Femoral and acetabular version and the alpha angle were measured on postoperative computed tomography scans. Clinical outcomes included range of motion and the modified Harris hip score. Analysis of variance was used to investigate the effect of femoral version on clinical outcomes. Analysis of covariance was used to adjust for potential covariates.
Results:
Combined femoral and acetabular version after periacetabular osteotomy was slightly, but significantly, correlated with postoperative flexion (r = 0.222; p = 0.031) and internal rotation in flexion (r = 0.326; p = 0.001). Patients with mild femoral version (<15°) experienced significantly less postoperative internal rotation in flexion than those with severe femoral version (>35°); however, this difference was lost after adjustment for potential covariates. There were no differences among femoral version groups (mild, moderate, and severe) in terms of improvements in the clinical outcomes of pain, function, and activity.
Conclusions:
Combined femoral and acetabular version after periacetabular osteotomy was significantly correlated with postoperative range of motion. Abnormality of femoral version associated with acetabular dysplasia did not demonstrate any effect on the clinical outcomes of periacetabular osteotomy.
Level of Evidence:
Prognostic Level IV. See Instructions for Authors for a complete description of levels of evidence.
It is generally known that femoral and acetabular version are associated with hip pain, reduced range of motion, and the development of hip osteoarthritis1-3. Combined version is defined as the sum of femoral and acetabular version. It is unclear whether combined version affects the clinical outcomes of periacetabular osteotomy for the treatment of symptomatic acetabular dysplasia.
Patients with acetabular dysplasia often have proximal femoral abnormalities, including cam-type deformities and excessive femoral anteversion4-8. Femoral cam deformity can result in painful restricted range of motion after periacetabular osteotomy9,10. Although studies have investigated the effect of femoral version on the clinical outcomes of total hip arthroplasty11 and arthroscopic surgery for the treatment of femoroacetabular impingement12,13, there has been less focus on the effect of femoral version on the clinical outcomes of periacetabular osteotomy for the treatment of acetabular dysplasia.
The primary purpose of the present study was to investigate the association of the postoperative combined femoral and acetabular version with clinical outcomes after periacetabular osteotomy. The secondary purpose was to evaluate whether femoral version was independently associated with clinical outcomes following periacetabular osteotomy. Our primary hypothesis was that there would be an association between the combined femoral and acetabular version and clinical outcomes after periacetabular osteotomy. Our secondary hypothesis was that femoral version would be independently associated with the clinical outcomes following periacetabular osteotomy.
Materials and Methods
Patient Selection
This retrospective study was approved by our institutional review board. Between January 2009 and May 2012, a total of 151 consecutive patients (162 hips) underwent curved periacetabular osteotomy for the treatment of symptomatic acetabular dysplasia at our institution. The inclusion criterion was the availability of a postoperative pelvic computed tomography (CT) scan. Postoperative CT was performed for 143 patients (154 hips) for evaluation of the osteotomy line and postoperative acetabular coverage as well as the assessment of femoral version and the sphericity of the femoral head after concomitant femoral neck osteochondroplasty. The exclusion criteria were prior hip surgery (n = 4), Legg-Calvé-Perthes-like deformities (n = 7), <2 years of follow-up (n = 35), radiographic evidence of joint degeneration (n = 9), or incomplete data (n = 4) (Fig. 1).
Fig. 1.
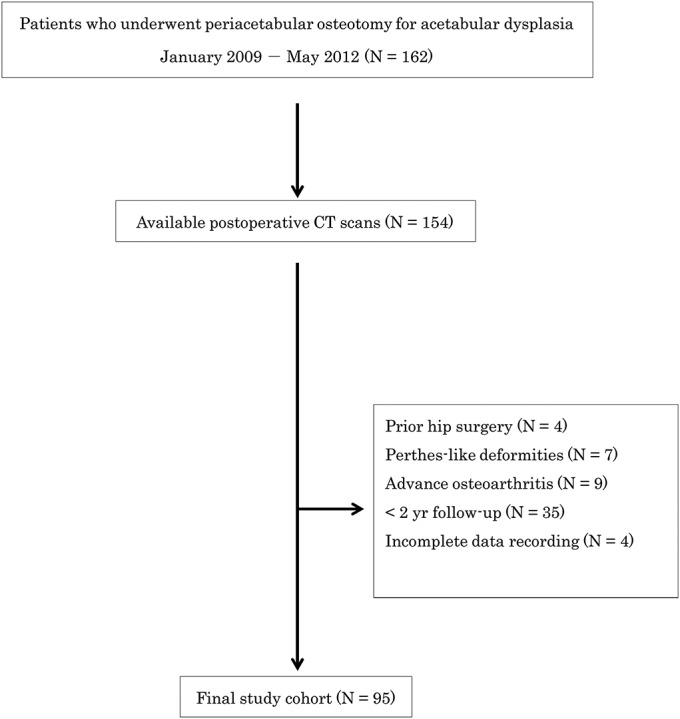
Flowchart for patient inclusion. The values in parentheses represent the number of hips.
A total of 92 patients (95 hips) with a minimum of 2 years of follow-up were included. The indication for curved periacetabular osteotomy was radiographic evidence of acetabular dysplasia with a lateral center-edge angle of Wiberg of <20° in patients with hip pain that interfered with daily activities. Patients showing improvement in femoral head coverage and joint congruity during abduction on anteroposterior pelvic radiographs were considered suitable for surgery. Hips with minimal or no osteoarthritic changes on radiographs at the time of surgery were included in this study.
Surgical Technique
Curved periacetabular osteotomy was developed for the treatment of acetabular dysplasia in 199514. For this procedure, the patient is placed in the supine position on a radiolucent table. Exposure of the osteotomy sites and osteotomy of the ischium are then performed in the same manner as for Bernese periacetabular osteotomy, and iliac and pubic osteotomies are performed in the same manner as for rotational acetabular osteotomy15. The acetabular fragment is rotated to achieve a horizontal weight-bearing acetabulum and medialization of the femoral head with use of intraoperative fluoroscopy. The acetabular fragment is then fixed with 2 or 3 poly-L-lactic acid screws (Fig. 2). To confirm the occurrence of postoperative anterior impingement, the anterior part of the capsule is palpated with the hip in flexion and internal rotation. When impingement is detected between the femoral head-neck junction and the anterior rim of the acetabulum, femoral head-neck osteochondroplasty is performed for the treatment of femoral cam deformity.
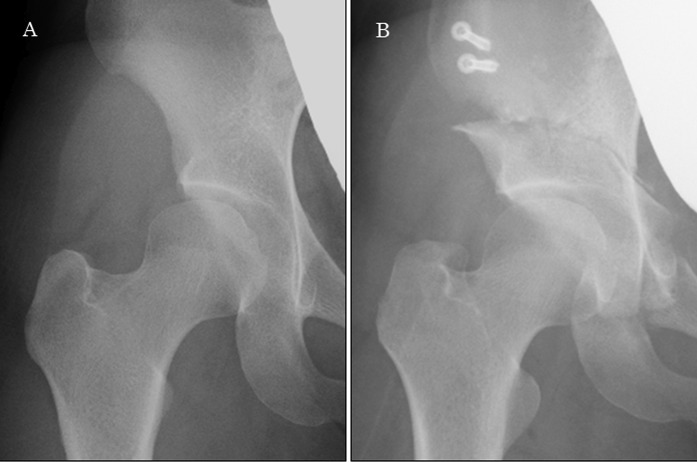
Fig. 2.
Preoperative (Fig. 2-A) and postoperative (Fig. 2-B) anteroposterior radiographs of the hip of a 35-year-old woman with symptomatic acetabular dysplasia who underwent curved periacetabular osteotomy.
Active motion exercises are initiated on the first postoperative day. Partial weight-bearing (10 kg) on 2 crutches or a walker is allowed on the third day, and full weight-bearing is allowed at 8 weeks.
Clinical Examination
Range of motion was measured with a goniometer at the time of the latest follow-up. The ranges of passive flexion, rotation (internal and external rotation) at 90° of flexion, and abduction in a neutral hip position were measured with the patient in the supine position with the pelvis stabilized. A previous study demonstrated that goniometric measurements of hip range of motion showed excellent interobserver and intraobserver reliabilities among multiple examiners16. Therefore, all range-of-motion measurements in the present study were performed by a single, trained examiner. The anterior impingement test was performed at the time of the latest follow-up. During this test, the hip was rotated internally as it was flexed passively to approximately 90° and adducted with the patient in the supine position. When a sudden sharp pain in the groin was elicited by this maneuver, the anterior impingement test was defined as positive17. The modified Harris hip score was used as part of the clinical assessment preoperatively and at the latest follow-up.
Imaging Technique
Radiographic evaluation was performed with use of supine anteroposterior pelvic and false-profile lateral radiographs. All radiographs were made according to previously published standardized techniques18. Radiographic parameters included measurements of the lateral center-edge angle, acetabular roof obliquity, Tönnis grade, and anterior center-edge angle (on false-profile lateral radiographs). The magnitude of the lateral center-edge angle was used to determine the severity of dysplasia. All measurements were made with use of digital calipers on the picture archiving and communication system.
Postoperative CT scans were made the week after periacetabular osteotomy. All patients received an explanation regarding the radiation exposure associated with CT, and all consented to our study protocol. All patients were placed in the supine position with the hip in a neutral position during CT scans. We used a 64-channel multidetector CT system (Aquilion TSX-101A/HA; Toshiba Medical Systems), and the scan protocol had a slice distance of 0.5 mm from the anterior superior iliac spines to below the knee. Multiplanar reconstruction images were made with use of a 3-dimensional (3D) workstation (Ziostation 2; Ziosoft).
Postoperative CT Measurements
With use of the 3D workstation, an initial correction for rotation in the coronal and axial planes was made by symmetrically aligning the pelvis. Acetabular version was determined in the axial plane by measuring the angle made by a line connecting the anterior and posterior edges of the acetabulum and a line perpendicular to the transverse line connecting the ischial spines19,20 (Fig. 3). Acetabular version measurements were made in 2 different transverse planes: (1) through the center of the femoral head and (2) more cranially, through the plane corresponding to the position 5 mm caudal to the acetabular roof. Acetabular version was defined as the mean version at the central and cranial positions in order to include global acetabular version rather than just a single axial slice. Femoral version was defined as the angle between the femoral neck axis and the posterior condylar axis of the femur in the axial plane2,21 (Fig. 4). The combined femoral and acetabular version was defined as the sum of the femoral and modified acetabular versions. The alpha angle was measured with use of the method of Nötzli et al.22 (Fig. 5). All radiographic measurements were performed by 2 examiners who were blinded to the clinical results and were repeated at least 4 weeks after the first measurements. Intraobserver reliability ranged from 0.70 to 0.99, and interobserver reliability ranged from 0.71 to 0.99.
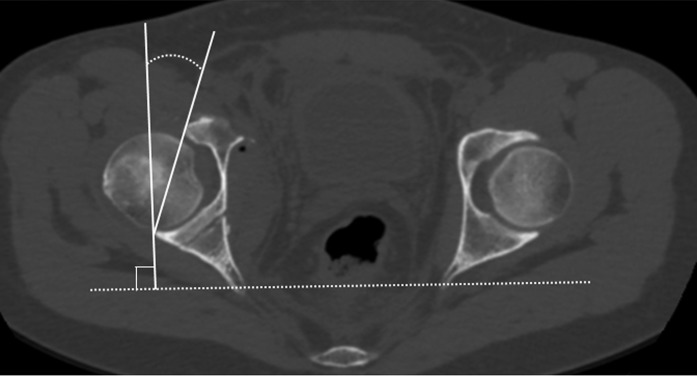
Fig. 3.
Acetabular version was determined in the axial plane by measuring the angle made by a line connecting the anterior and posterior edges of the acetabulum and a line perpendicular to the transverse line connecting the ischial spines.
Fig. 4.
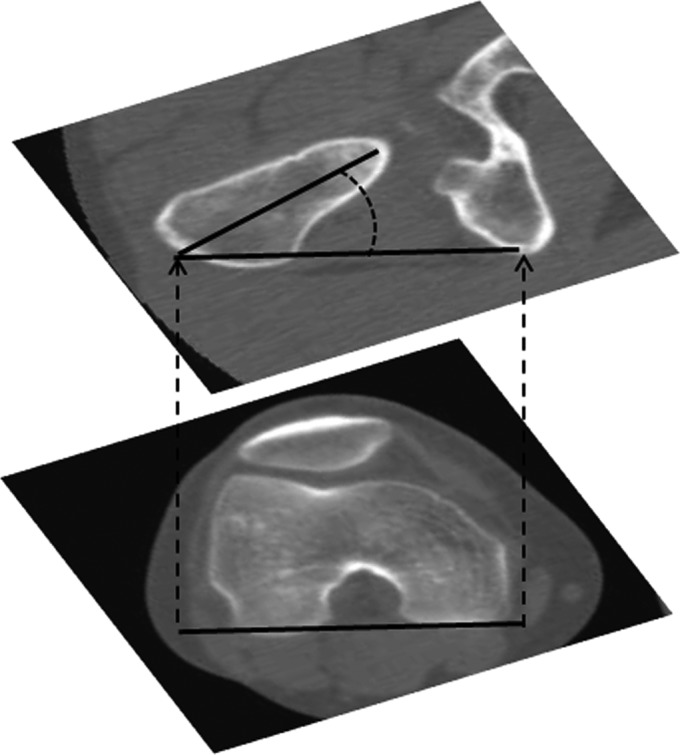
Femoral version was defined as the angle between the axis of the femoral neck and the posterior condylar axis of the femur in the axial plane.
Fig. 5.
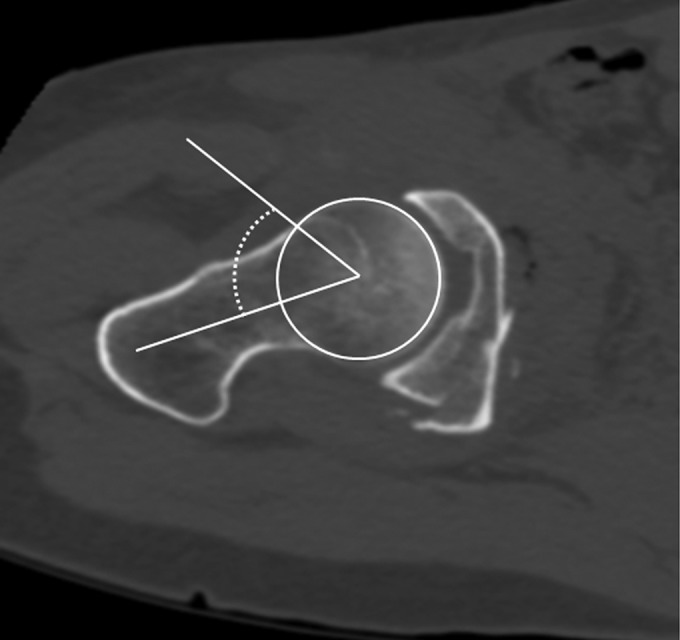
The alpha angle was defined as the angle between lines from the center of the femoral head through the middle of the femoral neck and through a point where the contour of the femoral head-neck junction exceeds the radius of the femoral head.
The severity of femoral anteversion was evaluated as a categorical predictor variable and was characterized as mild (<15°), moderate (15° to 35°), or severe (>35°). These ranges were chosen on the basis of a previous study involving 106 normal hips in Japanese adults in which the mean femoral version (and standard deviation) was found to be 23.6° ± 10.2° on 3D CT images23. For the present study, we then selected values that were approximately 1 standard deviation above and below this established mean (i.e., 15° and 35°) as the lower and upper values of the “moderate” category.
Statistical Analysis
Statistical analyses were performed with use of SPSS software (version 23.0; IBM). The Spearman rank correlation coefficient was used to analyze the relationships between combined version after periacetabular osteotomy and clinical outcomes at the time of the latest follow-up. Demographic characteristics, radiographic and clinical parameters, and intraoperative procedures were compared among the 3 femoral version groups via analysis of variance (ANOVA) with Tukey-adjusted pairwise comparisons for continuous variables and via the chi-square test or Fisher exact test for categorical variables. Analysis of covariance (ANCOVA) was used to perform adjusted analyses for the relationship between femoral version group (mild, moderate, or severe) and clinical outcomes at the time of the latest follow-up while adjusting for demographic and postoperative radiographic variables (see Appendix). For all statistical analyses, the level of significance was set at p < 0.05.
Results
The study cohort comprised 95 hips in 92 patients (85 females, 7 males) with a mean age of 38.9 years and a mean duration of follow-up of 4.8 years (range, 2.0 to 7.2 years). Concomitant femoral neck osteochondroplasty in conjunction with periacetabular osteotomy was performed in 15 hips (16%). No patients underwent concomitant derotational femoral osteotomy for the treatment of abnormal femoral version. A positive anterior impingement sign was seen in 16 hips (17%) postoperatively, and 3 (19%) of these 16 hips had undergone concomitant femoral neck osteochondroplasty in conjunction with periacetabular osteotomy. On postoperative CT scans, the mean combined femoral and acetabular version was 46° ± 19° and the mean alpha angle was 41° ± 6° (Table I). In evaluations of combined version after periacetabular osteotomy, the combined version was slightly, but significantly, correlated with the ranges of flexion (r = 0.222; p = 0.031) and internal rotation in flexion (r = 0.326; p = 0.001) (Table II). There was no correlation between combined version and improvement in any modified Harris hip score category.
TABLE I.
Radiographic Variables Measured on Postoperative CT Scans
| Variable | Value* (°) |
| Acetabular version | |
| Cranial | 8 ± 14 |
| Central | 19 ± 9 |
| Femoral version | 32 ± 13 |
| Combined version† | 46 ± 19 |
| Alpha angle | 41 ± 6 |
The values are given as the mean and the standard deviation.
Combined version was defined as the sum of femoral and acetabular version.
TABLE II.
Correlation of Postoperative Combined Version with Clinical Outcomes*
| Variable | Spearman Rank Correlation Coefficient | P Value |
| Range of motion | ||
| Flexion | 0.222 | 0.031† |
| Abduction | −0.061 | 0.560 |
| Internal rotation in flexion | 0.326 | 0.001† |
| External rotation in flexion | −0.018 | 0.864 |
| Change in modified Harris hip score | ||
| Pain | −0.070 | 0.503 |
| Function | 0.043 | 0.679 |
| Activity | 0.132 | 0.202 |
| Overall | 0.027 | 0.801 |
Combined version was defined as the sum of femoral and acetabular version.
Significant (p < 0.05).
Femoral version was mild in 16 hips, moderate in 41, and severe in 38. There were no significant differences among the femoral version groups in terms of age or body mass index at the time of periacetabular osteotomy, sex, duration of follow-up, or preoperative modified Harris hip score (Table III). Patients with mild femoral version had more severe acetabular dysplasia preoperatively than those with moderate or severe femoral version (lateral center-edge angle: 15° ± 5° versus 10° ± 9° versus 10° ± 7°, respectively; ANOVA p = 0.026; Tukey-adjusted pairwise comparisons p < 0.05). The prevalence of concomitant femoral neck osteochondroplasty in conjunction with periacetabular osteotomy did not significantly differ among the femoral version groups (p = 0.095).
TABLE III.
Baseline Characteristics by Femoral Version Group
| Femoral Version Group* |
|||||
| Variable | Mild (N = 16) | Moderate (N = 41) | Severe (N = 38) | P Value† | Significant Pairwise Differences‡ |
| Age§ (yr) | 35 ± 11 | 40 ± 13 | 39 ± 14 | 0.403 | ― |
| Female sex | 88% | 90% | 97% | 0.154 | ― |
| Body mass index§ (kg/m2) | 22 ± 2 | 22 ± 3 | 22 ± 3 | 0.834 | ― |
| Duration of follow-up§ (mo) | 55 ± 15 | 58 ± 17 | 59 ± 15 | 0.749 | ― |
| Radiographic measurements§# | |||||
| LCEA (°) | 15 ± 5 | 10 ± 9 | 10 ± 7 | 0.026** | Moderate, severe < mild |
| ARO (°) | 17 ± 3 | 20 ± 7 | 18 ± 6 | 0.118 | ― |
| ACEA (°) | 12 ± 12 | 10 ± 15 | 16 ± 12 | 0.134 | ― |
| Modified Harris hip score§ | |||||
| Pain | 26 ± 6 | 26 ± 8 | 27 ± 6 | 0.591 | ― |
| Function | 30 ± 2 | 31 ± 3 | 30 ± 3 | 0.578 | ― |
| Activity | 12 ± 2 | 12 ± 2 | 12 ± 2 | 0.221 | ― |
| Overall | 77 ± 9 | 77 ± 10 | 78 ± 8 | 0.956 | ― |
| Concomitant procedure (no. of hips) | |||||
| Osteochondroplasty | 5 (31%) | 7 (17%) | 3 (8%) | 0.095 | ― |
Femoral version was classified as mild (<15°), moderate (15° to 35°), or severe (>35°).
Comparisons performed with ANOVA (for age, body mass index, duration of follow-up, radiographic parameters, and modified Harris hip score) or the chi-square test (for sex and concomitant procedures).
Pairwise comparisons performed with use of Tukey adjustment for multiple comparisons (p < 0.05).
The values are given as the mean and the standard deviation.
LCEA = lateral center-edge angle, ARO = acetabular roof obliquity, and ACEA = anterior center-edge angle.
Significant difference among groups.
In postoperative radiographic evaluations, the mild femoral version group had a greater lateral center-edge angle and smaller central and cranial acetabular version than the severe femoral version group (Table IV). The alpha angle was almost equivalent among femoral version groups. Radiographic progression of osteoarthritis at the latest follow-up was observed in 5 hips (5%), but the prevalence did not significantly differ among the femoral version groups (p = 0.979).
TABLE IV.
Postoperative Radiographic Variables by Femoral Version Group
| Femoral Version Group*† |
|||||
| Variable | Mild (N = 16) | Moderate (N = 41) | Severe (N = 38) | P Value‡ | Significant Pairwise Differences§ |
| Non-CT measurements# (°) | |||||
| LCEA | 35 ± 7 | 31 ± 7 | 29 ± 7 | 0.021** | Severe < mild |
| ARO | 3 ± 6 | 6 ± 6 | 5 ± 6 | 0.066 | ― |
| ACEA | 39 ± 11 | 30 ± 12 | 32 ± 13 | 0.061 | ― |
| CT measurements (°) | |||||
| Acetabular version | |||||
| Cranial | 0 ± 7 | 9 ± 15 | 10 ± 14 | 0.001** | Mild < moderate, severe |
| Central | 14 ± 7 | 19 ± 10 | 21 ± 9 | 0.031** | Mild < severe |
| Femoral version | 11 ± 4 | 28 ± 5 | 45 ± 7 | <0.001** | Mild < moderate < severe |
| Combined version | 18 ± 8 | 43 ± 12 | 60 ± 12 | <0.001** | Mild < moderate < severe |
| Alpha angle | 41 ± 5 | 42 ± 7 | 40 ± 3 | 0.434 | ― |
Femoral version was classified as mild (<15°), moderate (15° to 35°), or severe (>35°).
The values are given as the mean and the standard deviation.
Comparisons performed with ANOVA.
Pairwise comparisons performed with use of Tukey adjustment for multiple comparisons (p < 0.05).
LCEA = lateral center-edge angle, ARO = acetabular roof obliquity, and ACEA = anterior center-edge angle.
Significant difference among groups.
The mild femoral version group experienced less postoperative internal rotation in flexion than the severe femoral version group (28° ± 8° versus 35° ± 9°; ANOVA p = 0.030; Tukey-adjusted pairwise comparisons p = 0.023). However, this difference was lost after adjusting for preoperative severity of acetabular dysplasia and postoperative alpha angle and acetabular version (ANCOVA p = 0.162) (Table V, also see Appendix). There were no significant differences among the femoral version groups in terms of the remaining 3 range-of-motion parameters (flexion, abduction, and external rotation in flexion) either before or after adjustment for similar potential covariates. There were no differences among the femoral version groups in terms of improvement in any category of the modified Harris hip score, with or without adjustment for preoperative severity of acetabular dysplasia and modified Harris hip score and for postoperative alpha angle and acetabular version (Table VI). The number of patients with a positive anterior impingement sign at the latest follow-up did not significantly differ among the femoral version groups (p = 0.296).
TABLE V.
Postoperative Range of Motion by Femoral Version Group
| Femoral Version Group*† |
||||||
| Range of Motion | Mild (N = 16) | Moderate (N = 41) | Severe (N = 38) | Crude P Value‡ | Significant Pairwise Differences§ | Adjusted P Value# |
| Flexion (°) | 110 ± 13 | 115 ± 10 | 115 ± 9 | 0.223 | ― | 0.552 |
| Abduction (°) | 40 ± 6 | 39 ± 6 | 38 ± 7 | 0.339 | ― | 0.507 |
| Internal rotation in flexion (°) | 28 ± 8 | 32 ± 11 | 35 ± 9 | 0.030** | Mild < severe | 0.162 |
| External rotation in flexion (°) | 41 ± 6 | 41 ± 6 | 40 ± 9 | 0.780 | ― | 0.756 |
Femoral version was classified as mild (<15°), moderate (15° to 35°), or severe (>35°).
The values are given as the mean and the standard deviation.
Compared with use of ANOVA.
Pairwise comparisons performed with use of Tukey adjustment for multiple comparisons (p < 0.05).
ANCOVA adjusted for preoperative lateral center-edge angle, postoperative acetabular version, and postoperative alpha angle.
Significant difference among groups.
TABLE VI.
Change in Modified Harris Hip Score by Femoral Version Group
| Femoral Version Group*† |
|||||
| Change in Modified Harris Hip Score | Mild (N = 16) | Moderate (N = 41) | Severe (N = 38) | Crude P Value‡ | Adjusted P Value§ |
| Pain | 12 ± 9 | 15 ± 10 | 12 ± 8 | 0.336 | 0.748 |
| Function | 3 ± 3 | 2 ± 7 | 2 ± 3 | 0.828 | 0.430 |
| Activity | 1 ± 3 | 1 ± 3 | 2 ± 2 | 0.735 | 0.894 |
| Overall | 16 ± 12 | 18 ± 9 | 16 ± 9 | 0.661 | 0.404 |
Femoral version was classified as mild (<15°), moderate (15° to 35°), or severe (>35°).
The values are given as the mean and the standard deviation.
Compared with use of ANOVA.
ANCOVA adjusted for preoperative lateral center-edge angle and modified Harris hip score and for postoperative acetabular version and alpha angle.
Minor complications were seen in association with 14 hips (15%), including lateral femoral cutaneous nerve dysesthesia (n = 6), delayed union of the pubis (n = 6), and inferior pubic ramus fracture (n = 2). Regarding reoperation, 3 patients underwent arthroscopy for labral treatment. Two patients who had untreated femoral head asphericity experienced groin pain postoperatively during internal rotation in flexion and underwent femoral neck osteochondroplasty at 3.7 and 5.3 years after periacetabular osteotomy. No patient underwent conversion to total hip arthroplasty during follow-up.
Discussion
Periacetabular osteotomy is commonly used for the treatment of symptomatic acetabular dysplasia, and clinical outcome studies have indicated that this procedure results in marked pain reduction and functional improvement14,24-29. However, various factors reportedly have been associated with the outcomes of periacetabular osteotomy9,30-33. To our knowledge, no previous study has evaluated the effect of femoral and acetabular version on clinical outcomes following periacetabular osteotomy. In the present study, we found that combined femoral and acetabular version after periacetabular osteotomy was significantly correlated with the postoperative ranges of flexion and internal rotation in flexion. However, the degree of femoral version was not independently associated with the clinical outcomes of periacetabular osteotomy when accounting for potential covariates in a general linear model.
Recognition of the interaction between femoral and acetabular morphology is important in clinical practice1-3. The concept of combined femoral and acetabular version has been previously reported in studies of pediatric patients with developmental hip dysplasia1, patients who have undergone total hip arthroplasty11, and, recently, patients who have undergone surgery for the treatment of femoroacetabular impingement13. In the present study, we noted significant associations between combined version and flexion as well as internal rotation in flexion in patients who had undergone periacetabular osteotomy. These findings indicate that it may be better to avoid postoperative acetabular retroversion, especially in patients with decreased femoral version. However, acetabular version should not be considered a preferential parameter in acetabular correction. Acetabular dysplasia presents with varying degrees of acetabular version associated with malalignment of the acetabulum. When performing periacetabular osteotomy for reorientation of the acetabulum, surgeons should pay attention to the interaction between femoral and acetabular version as well as the coverage of the acetabulum. For patients with acetabular dysplasia, it is most important that periacetabular osteotomy result in sufficient coverage of the acetabulum rather than increased acetabular version. Taken together, our results further emphasize the importance of recognizing this combined version, even in patients who undergo periacetabular osteotomy for the treatment of acetabular dysplasia.
Decreased femoral version is a distinct dynamic factor that should be considered in the evaluation of mechanical causes of hip pain34. A previous study demonstrated that the range of internal rotation in patients with decreased femoral version was significantly less than that in patients with normal version or increased femoral version both before and after arthroscopic femoral cam decompression (p < 0.05)12. In the present study, we also found a smaller range of internal rotation in hip flexion in the mild femoral version group after periacetabular osteotomy; however, this difference was lost after adjusting for potential covariates. Our results might be because the mild femoral version group had less acetabular version postoperatively than the severe femoral version group. Fabricant et al.13 noted that patients with decreased femoral version had smaller improvements in patient-reported outcomes after arthroscopic surgery for the treatment of femoroacetabular impingement. With the numbers available in the present study, we could not find any significant association between femoral version and clinical outcomes after periacetabular osteotomy. Conversely, excessive femoral anteversion generally can lead to painful restricted external rotation as a result of posterior impingement2,34. However, there were no differences in postoperative range of external rotation among the femoral version groups in the present study. Our results indicated that postoperative posterior impingement was less likely to occur in patients undergoing periacetabular osteotomy because the acetabulum was rotated anteriorly through periacetabular osteotomy. Future research is needed to determine the long-term effect of femoral version on several patient-reported outcomes after periacetabular osteotomy.
One advantage of the present study was the large cohort of patients who were evaluated with CT scans after periacetabular osteotomy. Using these postoperative CT scans, we measured postoperative femoral and acetabular version and alpha angle according to previously published methods2,19-22. In addition, because of the rigorous exclusion criteria in the present study, we could minimize the effect of degenerative change of the hip joint on the CT measurements. To our knowledge, this is the first study to investigate the associations of femoral and acetabular version with clinical outcomes following periacetabular osteotomy. However, the clinical outcomes of periacetabular osteotomy might be affected by further abnormal morphology. Future research is needed to identify such abnormal morphology.
The present study had several limitations. First, few patient-reported outcomes were evaluated. Although patient-reported outcomes are considered the gold standard when evaluating outcomes in a surgical population35, our study included only the modified Harris hip score for clinical scoring. Future research should investigate the effect of femoral and acetabular version on various patient-reported outcomes. Second, the present study lacked evaluation of preoperative acetabular version on CT scans and preoperative range of motion, both of which can affect clinical outcomes. Third, although labral tears are common in patients with acetabular dysplasia, we did not investigate labral pathology in the present study. Because labral pathology also affects clinical outcomes after periacetabular osteotomy36, there might be differences in clinical outcomes depending on the presence of labral tears. Last, there were no patients with femoral retroversion in the present study. A further large cohort study is warranted to investigate the effect of femoral retroversion on outcomes after periacetabular osteotomy.
In conclusion, we believe that ours is the first study to investigate the associations of femoral and acetabular version with clinical outcomes following periacetabular osteotomy. We found significant associations between combined femoral and acetabular version and hip range of motion in patients who underwent periacetabular osteotomy. Our results indicate that patients with decreased combined femoral and acetabular version after periacetabular osteotomy may experience restriction of range of motion. Surgeons performing periacetabular osteotomy should pay attention to postoperative acetabular retroversion as it may result in restriction of range of motion, especially for patients with decreased femoral version. Furthermore, we found that femoral version alone may not affect clinical outcomes after periacetabular osteotomy when adjusting for potential covariates such as the severity of acetabular dysplasia, alpha angle, and acetabular version. It may not be necessary to perform femoral derotational osteotomy routinely at the same time as periacetabular osteotomy unless major femoral retroversion is present. Further research regarding the impact of preoperative acetabular version and preoperative range of motion on the outcomes of periacetabular osteotomy needs to be conducted.
Appendix
A table showing general linear models for postoperative hip range of motion is available with the online version of this article as a data supplement at jbjs.org (http://links.lww.com/JBJSOA/A45).
Footnotes
Investigation performed at the Department of Orthopaedic Surgery, Fukuoka University, Fukuoka, Japan
Disclosure: There was no external funding for this study. The Disclosure of Potential Conflicts of Interest forms are provided with the online version of the article (http://links.lww.com/JBJSOA/A44).
References
- 1.McKibbin B. Anatomical factors in the stability of the hip joint in the newborn. J Bone Joint Surg Br. 1970. February;52(1):148-;59. [PubMed] [Google Scholar]
- 2.Tönnis D, Heinecke A. Acetabular and femoral anteversion: relationship with osteoarthritis of the hip. J Bone Joint Surg Am. 1999. December;81(12):1747-;70. [DOI] [PubMed] [Google Scholar]
- 3.Chadayammuri V, Garabekyan T, Bedi A, Pascual-Garrido C, Rhodes J, O’Hara J, Mei-Dan O. Passive hip range of motion predicts femoral torsion and acetabular version. J Bone Joint Surg Am. 2016. January 20;98(2):127-;34. [DOI] [PubMed] [Google Scholar]
- 4.Robertson DD, Essinger JR, Imura S, Kuroki Y, Sakamaki T, Shimizu T, Tanaka S. Femoral deformity in adults with developmental hip dysplasia. Clin Orthop Relat Res. 1996. June;327:196-;206. [DOI] [PubMed] [Google Scholar]
- 5.Noble PC, Kamaric E, Sugano N, Matsubara M, Harada Y, Ohzono K, Paravic V. Three-dimensional shape of the dysplastic femur: implications for THR. Clin Orthop Relat Res. 2003. December;417:27-;40. [PubMed] [Google Scholar]
- 6.Argenson JNA, Flecher X, Parratte S, Aubaniac JM. Anatomy of the dysplastic hip and consequences for total hip arthroplasty. Clin Orthop Relat Res. 2007. December;465:40-;5. [DOI] [PubMed] [Google Scholar]
- 7.Clohisy JC, Nunley RM, Carlisle JC, Schoenecker PL. Incidence and characteristics of femoral deformities in the dysplastic hip. Clin Orthop Relat Res. 2009. January;467(1):128-;34. Epub 2008 Nov 26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wells J, Nepple JJ, Crook K, Ross JR, Bedi A, Schoenecker P, Clohisy JC. Femoral morphology in the dysplastic hip: Three-dimensional characterizations with CT. Clin Orthop Relat Res. 2017. April;475(4):1045-;54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Albers CE, Steppacher SD, Ganz R, Tannast M, Siebenrock KA. Impingement adversely affects 10-year survivorship after periacetabular osteotomy for DDH. Clin Orthop Relat Res. 2013. May;471(5):1602-;14. Epub 2013 Jan 25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Steppacher SD, Zurmühle CA, Puls M, Siebenrock KA, Millis MB, Kim YJ, Tannast M. Periacetabular osteotomy restores the typically excessive range of motion in dysplastic hips with a spherical head. Clin Orthop Relat Res. 2015. April;473(4):1404-;16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoshimine F. The safe-zones for combined cup and neck anteversions that fulfill the essential range of motion and their optimum combination in total hip replacements. J Biomech. 2006;39(7):1315-;23. [DOI] [PubMed] [Google Scholar]
- 12.Kelly BT, Bedi A, Robertson CM, Dela Torre K, Giveans MR, Larson CM. Alterations in internal rotation and alpha angles are associated with arthroscopic cam decompression in the hip. Am J Sports Med. 2012. May;40(5):1107-;12. Epub 2012 Mar 5. [DOI] [PubMed] [Google Scholar]
- 13.Fabricant PD, Fields KG, Taylor SA, Magennis E, Bedi A, Kelly BT. The effect of femoral and acetabular version on clinical outcomes after arthroscopic femoroacetabular impingement surgery. J Bone Joint Surg Am. 2015. April 01;97(7):537-;43. [DOI] [PubMed] [Google Scholar]
- 14.Naito M, Shiramizu K, Akiyoshi Y, Ezoe M, Nakamura Y. Curved periacetabular osteotomy for treatment of dysplastic hip. Clin Orthop Relat Res. 2005. April;433:129-;35. [DOI] [PubMed] [Google Scholar]
- 15.Ninomiya S, Tagawa H. Rotational acetabular osteotomy for the dysplastic hip. J Bone Joint Surg Am. 1984. March;66(3):430-;6. [PubMed] [Google Scholar]
- 16.Prather H, Harris-Hayes M, Hunt DM, Steger-May K, Mathew V, Clohisy JC. Reliability and agreement of hip range of motion and provocative physical examination tests in asymptomatic volunteers. PM R. 2010. October;2(10):888-;95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Klaue K, Durnin CW, Ganz R. The acetabular rim syndrome. A clinical presentation of dysplasia of the hip. J Bone Joint Surg Br. 1991. May;73(3):423-;9. [DOI] [PubMed] [Google Scholar]
- 18.Clohisy JC, Carlisle JC, Beaulé PE, Kim YJ, Trousdale RT, Sierra RJ, Leunig M, Schoenecker PL, Millis MB. A systematic approach to the plain radiographic evaluation of the young adult hip. J Bone Joint Surg Am. 2008. November;90(Suppl 4):47-;66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dandachli W, Ul Islam S, Tippett R, Hall-Craggs MA, Witt JD. Analysis of acetabular version in the native hip: comparison between 2D axial CT and 3D CT measurements. Skeletal Radiol. 2011. July;40(7):877-;83. Epub 2010 Dec 22. [DOI] [PubMed] [Google Scholar]
- 20.Dolan MM, Heyworth BE, Bedi A, Duke G, Kelly BT. CT reveals a high incidence of osseous abnormalities in hips with labral tears. Clin Orthop Relat Res. 2011. March;469(3):831-;8. Epub 2010 Oct 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Sugano N, Noble PC, Kamaric E. A comparison of alternative methods of measuring femoral anteversion. J Comput Assist Tomogr. 1998. Jul-Aug;22(4):610-;4. [DOI] [PubMed] [Google Scholar]
- 22.Nötzli HP, Wyss TF, Stoecklin CH, Schmid MR, Treiber K, Hodler J. The contour of the femoral head-neck junction as a predictor for the risk of anterior impingement. J Bone Joint Surg Br. 2002. May;84(4):556-;60. [DOI] [PubMed] [Google Scholar]
- 23.Nakahara I, Takao M, Sakai T, Nishii T, Yoshikawa H, Sugano N. Gender differences in 3D morphology and bony impingement of human hips. J Orthop Res. 2011. March;29(3):333-;9. Epub 2010 Oct 11. [DOI] [PubMed] [Google Scholar]
- 24.Ganz R, Klaue K, Vinh TS, Mast JW. A new periacetabular osteotomy for the treatment of hip dysplasias. Technique and preliminary results. Clin Orthop Relat Res. 1988. July;232:26-;36. [PubMed] [Google Scholar]
- 25.Matta JM, Stover MD, Siebenrock K. Periacetabular osteotomy through the Smith-Petersen approach. Clin Orthop Relat Res. 1999. June;363:21-;32. [PubMed] [Google Scholar]
- 26.Murphy SB, Millis MB, Hall JE. Surgical correction of acetabular dysplasia in the adult. A Boston experience. Clin Orthop Relat Res. 1999. June;363:38-;44. [PubMed] [Google Scholar]
- 27.Hussell JG, Mast JW, Mayo KA, Howie DW, Ganz R. A comparison of different surgical approaches for the periacetabular osteotomy. Clin Orthop Relat Res. 1999. June;363:64-;72. [PubMed] [Google Scholar]
- 28.Clohisy JC, Schutz AL, St John L, Schoenecker PL, Wright RW. Periacetabular osteotomy: a systematic literature review. Clin Orthop Relat Res. 2009. August;467(8):2041-;52. Epub 2009 Apr 21. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Clohisy JC, Ackerman J, Baca G, Baty J, Beaulé PE, Kim YJ, Millis MB, Podeszwa DA, Schoenecker PL, Sierra RJ, Sink EL, Sucato DJ, Trousdale RT, Zaltz I, on behalf of the ANCHOR Study Group. Patient-reported outcomes of periacetabular osteotomy from the prospective ANCHOR cohort study. J Bone Joint Surg Am. 2017. January 04;99(1):33-;41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Steppacher SD, Tannast M, Ganz R, Siebenrock KA. Mean 20-year followup of Bernese periacetabular osteotomy. Clin Orthop Relat Res. 2008. July;466(7):1633-;44. Epub 2008 May 1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Matheney T, Kim YJ, Zurakowski D, Matero C, Millis M. Intermediate to long-term results following the Bernese periacetabular osteotomy and predictors of clinical outcome. J Bone Joint Surg Am. 2009. September;91(9):2113-;23. [DOI] [PubMed] [Google Scholar]
- 32.Troelsen A, Elmengaard B, Søballe K. Medium-term outcome of periacetabular osteotomy and predictors of conversion to total hip replacement. J Bone Joint Surg Am. 2009. September;91(9):2169-;79. [DOI] [PubMed] [Google Scholar]
- 33.Beaulé PE, Dowding C, Parker G, Ryu JJ. What factors predict improvements in outcomes scores and reoperations after the Bernese periacetabular osteotomy? Clin Orthop Relat Res. 2015. February;473(2):615-;22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Bedi A, Dolan M, Leunig M, Kelly BT. Static and dynamic mechanical causes of hip pain. Arthroscopy. 2011. February;27(2):235-;51. Epub 2010 Oct 29. [DOI] [PubMed] [Google Scholar]
- 35.Kemp JL, Collins NJ, Roos EM, Crossley KM. Psychometric properties of patient-reported outcome measures for hip arthroscopic surgery. Am J Sports Med. 2013. September;41(9):2065-;73. Epub 2013 Jul 8. [DOI] [PubMed] [Google Scholar]
- 36.Ricciardi BF, Mayer SW, Fields KG, Wentzel C, Kelly BT, Sink EL. Patient characteristics and early functional outcomes of combined arthroscopic labral refixation and periacetabular osteotomy for symptomatic acetabular dysplasia. Am J Sports Med. 2016. October;44(10):2518-;25. Epub 2016 Jul 14. [DOI] [PubMed] [Google Scholar]