Key Points
Question
Is teledermoscopy cost-effective for skin cancer referral and triage in Australia?
Findings
In this decision-analytic modeling study using deidentified Australian health system data, store-and-forward teledermoscopy skin cancer referral was estimated to cost A$54.64 per person more than usual care but enabled clinical resolution to be achieved a mean of 26 days earlier. The incremental cost per day saved to clinical resolution was A$2.10.
Meaning
Incorporating teledermoscopy as a referral method for skin cancer in Australia has the potential to benefit patients by providing earlier clinical resolution at additional cost to Medicare.
This study uses a decision-analytic model to assess the cost-effectiveness of teledermoscopy as a referral mechanism for skin cancer diagnosis and management in Australia.
Abstract
Importance
International literature has shown that teledermoscopy referral may be a viable method for skin cancer referral; however, no economic investigations have occurred in Australia.
Objective
To assess the cost-effectiveness of teledermoscopy as a referral mechanism for skin cancer diagnosis and management in Australia.
Design, Setting, and Participants
Cost-effectiveness analysis using a decision-analytic model of Australian primary care, informed by publicly available data.
Interventions
We compared the costs of teledermoscopy referral (electronic referral containing digital dermoscopic images) vs usual care (a written referral letter) for specialist dermatologist review of a suspected skin cancer.
Main Outcomes and Measures
Cost and time in days to clinical resolution, where clinical resolution was defined as diagnosis by a dermatologist or excision by a general practitioner. Probabilistic sensitivity analysis was performed to examine the uncertainty of the main results.
Results
Findings from the decision-analytic model showed that the mean time to clinical resolution was 9 days (range, 1-50 days) with teledermoscopy referral compared with 35 days (range, 0-138 days) with usual care alone (difference, 26 days; 95% credible interval [CrI], 13-38 days). The estimated mean cost difference between teledermoscopy referral (A$318.39) vs usual care (A$263.75) was A$54.64 (95% CrI, A$22.69-A$97.35) per person. The incremental cost per day saved to clinical resolution was A$2.10 (95% CrI, A$0.87-A$5.29).
Conclusions and Relevance
Using teledermoscopy for skin cancer referral and triage in Australia would cost A$54.64 extra per case on average but would result in clinical resolution 26 days sooner than usual care. Implementation recommendations depend on the preferences of the Australian health system decision makers for either lower cost or expedited clinical resolution. Further research around the clinical significance of expedited clinical resolution and its importance for patients could inform implementation recommendations for the Australian setting.
Introduction
Skin cancer presents a global health challenge. In Australia, melanoma accounts for more than 10% of all diagnosed and reported cancers, with an estimated 13 280 new cases diagnosed in 2016.1 The incidence of melanoma is increasing. Keratinocyte skin cancers (squamous and basal cell carcinomas) and other skin cancers are not nationally reported and occur between 10 and 20 times more often than melanoma.1
Teledermatology is the provision of dermatologic care at a distance using information and communications technology. Teledermatology often uses store-and-forward communication, in which digital images of a skin lesion are captured, typically in primary care, and subsequently forwarded to a dermatologist along with clinical information for review or management advice. In addition to the provision of virtual consultations, teledermatology can also be used to facilitate the triage of referrals for specialist care.2,3,4,5 When compared with a written referral for specialist care, the visual information included in a teledermatology referral provides extra information to assist with appropriate triage and patient management. Teledermatology referrals can result in earlier assessment and treatment6 and in reduced waiting times and waiting lists.7 When clinically indicated, some patients do not need to be seen by a dermatologist and instead can be managed by their general practitioners (GPs) often under advice from a dermatologist.8,9,10
Dermoscopy is a noninvasive diagnostic technique that links clinical dermatology and dermatopathology of pigmented and nonpigmented skin lesions by enabling the visualization of morphological features not seen by the naked eye.11 Teledermoscopy is a form of teledermatology that specifically involves the store-and-forwarding of digital dermoscopic images. When compared with other imaging techniques, teledermoscopy improves diagnostic accuracy.12,13 Teledermoscopy is not currently reimbursed under Medicare (Australia’s universal health scheme funded by the federal government).
At present, there are no published economic evaluations for teledermoscopy services specific to the Australian health care system, and there are few international studies available.14 The implementation of new models of care requires information on their comparative cost-effectiveness. Therefore, the purpose of this study was to examine the cost-effectiveness of teledermoscopy as a referral mechanism for skin cancer diagnosis in Australia and determine its value for improving the management of skin cancer.
Methods
Overview
An ethics waiver was granted by the University of Queensland Human Ethics Research Office because the study used only previously collected, deidentified data. The cost-effectiveness of teledermoscopy referral for a suspected skin cancer was compared with usual care using a decision-analytic model. A teledermoscopy referral is an electronic referral to a dermatologist containing digital dermoscopic images and clinical information, whereas usual care is a written referral from a GP containing clinical information only.
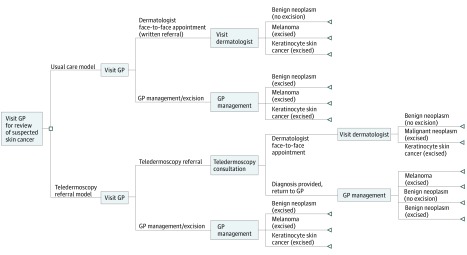
The decision-analytic model was developed in TreeAge Pro software, release 2.1 (2016). The model represented pathways of clinical management of suspected skin cancer in a general adult population. The model has 2 arms, 1 representing usual care for suspected skin cancer in Australia and 1 representing the teledermoscopy referral intervention (Figure 1).
Figure 1. Decision-Analytic Model Structure.
Decision-analytic model structure demonstrating the decision nodes and end points that were used in the model. GP indicates general practitioner.
The model end point was clinical resolution, defined as diagnosis by a dermatologist or excision of lesion by a GP. Diagnostic outcomes were melanoma, keratinocyte skin cancer (squamous cell carcinoma or basal cell carcinoma), and benign neoplasms (clinically and dermoscopically mimicking melanoma or a keratinocyte skin cancer). Costs were estimated from the perspective of the Australian Commonwealth Government (administrators of the Medical Benefits Scheme [MBS]), and included the costs of consultation, excision, and histopathologic analysis. Histopathologic confirmation of excised lesions is required before claiming items on the MBS to ensure correct itemization and payment for health care professionals.15
Comparative Treatments
In Australia, usual care for a patient begins with a visit to a GP. Suspicious skin lesions may be detected during routine skin checks or opportunistically when patients visit their GP for a different purpose. After examining the area of concern and performing a full skin check, the GP can perform a biopsy or excision for histopathologic analysis or refer the patient to a dermatologist for management. If referral is selected, the GP will write a referral letter and forward it to a nominated dermatologist or to the patient, who can submit to a dermatologist of their choice. When the patient has a consultation with the dermatologist, the dermatologist will undertake a full skin examination with or without a dermoscope, take dermoscopic images where appropriate, and if necessary perform a biopsy or excision. This process may occur across single or multiple visits with either the GP and/or dermatologist.
For teledermoscopy referral, rather than writing referrals, the GP captures and sends a teledermoscopy image with clinical notes to any participating dermatologist. Once reviewed by a dermatologist, the teledermoscopy information could either be used to advise the GP of management options (eg, to excise or monitor), or if necessary, schedule the patient for an in-person dermatologist consultation.
Model Inputs
Data estimates that informed the model were sourced systematically from literature searches and government databases. Probability data were sourced from international publications that had performed studies with similar usual care and teledermoscopy referral intervention (Table 1). The Australian Bettering the Evaluation and Care of Health (BEACH) report informed treatment estimates for proportion of occasions when GPs chose monitoring (no active treatment) for suspicious lesions, or rate of referral to a dermatologist (Table 1).17 The BEACH program runs out of the University of Sydney and collects data about the clinical activities of Australian GPs. Discounting of costs and benefits to the present day was not relevant to these analyses due to the 4-month time horizon.
Table 1. Cost and Probability Estimates.
| Variable | Model Estimate | Sensitivity Values | Distribution Parameters | Source | |
|---|---|---|---|---|---|
| Minimum | Maximum | ||||
| Costs, A$ | |||||
| GP consultation fee | 37.05 | 37.05 (1 consult) | 111.15 (3 consults) | α = 6.10, λ = 0.16 | MBS item 2315 |
| Dermatologist consultation fee | 72.75 | 72.75 (1 consult) | 145.50 (2 consults) | α = 23.52, λ = 0.32 | MBS item 10415 |
| Dermatologist teledermatology consult | 72.75 | 36.38 (50%) | 109.12 (150%) | α = 23.52, λ = 0.32 | MSAC Application (refers to MBS item 104)15,16 |
| Histopathologic analysis | 107.12 | 107.12 (1 instance) | 214.24 (2 instances) | α = 28.69, λ = 0.27 | Weighted average of MBS items 72816-72818 and 7283015 |
| Benign neoplasm excision | 91.72 | 76.40 (lowest MBS cost) | 126.05 (highest MBS cost) | α = 84.13, λ = 0.92 | Weighted average of MBS items 31200-3121015 |
| Keratinocyte skin cancer excision | 157.36 | 155.85 (lowest MBS cost) | 299.25 (highest MBS cost) | α = 39.62, λ = 0.25 | Weighted average of MBS items 31255-3129015 |
| Melanoma skin cancer excision | 250.92 | 278.65 (lowest MBS cost) | 369.00 (highest MBS cost) | α = 279.83, λ = 1.12 | Weighted average of MBS items 31300-3133515 |
| Any skin cancer excision (keratinocyte or melanoma skin cancer) | 161.08 | 155.85 (lowest MBS cost) | 369.00 (highest MBS cost) | α = 21.18, λ = 0.13 | Weighted average of MBS items 31200-31210, 31255-31290, and 31300-3133515 |
| Probabilities | |||||
| GP refer to dermatologist (usual care) | 0.31 | 0.19 | 0.31 | α = 165.46, β = 368.29 | BEACH Report 2013-201417 |
| GP management condition without referral (usual care) | 0.7 | 0.4 | 0.7 | α = 9.51, β = 4.08 | BEACH Report 2013-20149 |
| GP refer to dermatologist via teledermatology | 0.64 | 0.15 | 0.85 | α = 9.60, β = 5.40 | Morton et al,18 2011 |
| Postteledermatology patient return to GP for management | 0.7 | 0.4 | 0.7 | α = 58.10, β = 24.90 | Snoswell et al,14 2016 |
| Postteledermatology patient attend in-person appointment with dermatologist | 0.2879 | 0.02 | 0.8 | α = 3.20, β = 7.93 | Moreno-Ramirez et al,4 2007 |
| GP excise melanoma skin cancer | 0.03 | 0.01 | 0.09 | α = 34.89, β = 1128.11 | English et al,19 2004 |
| GP excise keratinocyte skin cancer | 0.67 | 0.19 | 0.96 | α = 8.10, β = 3.99 | English et al,19 2004 |
| Dermatologist in-person excise melanoma skin cancer | 0.112 | 0.088 | 0.173 | α = 56.72, β = 449.71 | Taylor et al,20 2012 |
| Dermatologist in-person excise keratinocyte skin cancer | 0.247 | 0.1 | 0.8 | α = 18.13, β = 55.27 | Taylor et al,20 2012 |
| Postteledermatology GP consult and no action | 0.2 | 0.2 | 0.8 | α = 12.60, β = 50.4 | Massone et al,21 2014 |
| Postteledermatology GP consult and excise melanoma skin cancer | 0.01 | 0.01 | 0.09 | α = 3.95, β = 391.05 | Massone et al,21 2014 |
| Postteledermatology GP consult and excise keratinocyte skin cancer | 0.22 | 0.2 | 0.96 | α = 14.88, β = 52.76 | Massone et al,21 2014 |
| Outcomes, Time, d | |||||
| GP consult to GP excision without referral | 1 | 0 | 1 | No distribution | Same on both arms, therefore set to 1 |
| GP consult to final resolution (excision or dermatologist appointment) in usual care | 114 | 61 | 138 | No distribution | Lim et al,8,14 2012 |
| GP consult to final resolution (excision or dermatologist appointment) via teledermatology | 39 | 13 | 50 | No distribution | Lim et al,8,14 2012 |
| GP teledermatology referral to GP no action | 2 | 1 | 7 | No distribution | Lim et al,8,14 2012 |
Abbreviations: BEACH, Bettering the Evaluation and Care of Health; GP, general practitioner; MBS, Medical Benefits Scheme; MSAC, Medical Services Advisory Committee.
Cost data to inform the model were sourced from the Australian Department of Health MBS (Table 1). The dermatologist teledermoscopy consult fee was set to be the same as the dermatologist in-person consultation fee, A$72.75, aligning with the Medical Services Advisory Committee for asynchronous store-and-forward reimbursement.16 Costs for excision of melanoma, keratinocyte skin cancer, and benign neoplasm were informed by relevant MBS item codes (Table 1).22 Because there are multiple MBS item codes for each type of skin lesion, a single price per lesion type was calculated using a weighted average. Average weighted costs were calculated using MBS data from March 2013 to April 2014; this timeframe was selected to align with the BEACH report.15,17
The measure of benefit for this analysis was days to clinical resolution. Clinical resolution was defined as diagnosis by a dermatologist, or excision and histopathologic analysis by a GP. The time in days between a GP consultation and excision of a suspected skin cancer was set to 1 day and is the same in both arms of the model. All other time information was taken from a prospective cohort study performed in New Zealand with 300 participants in 2012.8 This study was selected because of the comparability of the New Zealand health system and skin cancer risk to Australia; existing alternatives were cohort studies from Spain or the United States.4,23
Analyses
The model performed an expected-values analysis by aggregating the probabilities and costs in the pathways to calculate the mean cost per person. The incremental cost-effectiveness ratio was calculated by dividing the difference in costs of the 2 options by the difference in days to clinical resolution (benefit). Cost inputs were in 2016 Australian dollars.
One-way sensitivity analysis was performed by separately varying all model inputs within plausible ranges of high and low values (from relevant sources or imputed (Table 1). Alternative probabilities were extracted from the published studies (Table 1). Frequencies of physician visits and pathology testing varied between 1 and 3 visits or tests, which in turn affected service costs (Table 1).
Probabilistic sensitivity analysis was undertaken by resampling the cost and probabilities (concurrently) within prespecified distributions (Table 1). Cost estimates and probabilities were randomly resampled according to γ and β distributions, respectively (Table 1). One thousand Monte Carlo simulations were run, resulting in a range of plausible costs and effects. These simulation data allowed for the estimation of a 95% credible interval (CrI) for model results to address the uncertainty in the model inputs. Each CrI was estimated by rank ordering the results sequentially and excluding the highest 2.5% and lowest 2.5% of values.
Results
Teledermoscopy referral had a mean cost of A$318.39 per case and took a mean of 9 days (range, 1-50 days) to clinical resolution, while usual care cost A$263.75 with 35 days (range, 0-138 days) to clinical resolution (Table 2). Therefore, teledermoscopy referral cost A$54.64 (95% CrI, A$22.69-A$97.35) more per case than usual care alone and was associated with a mean reduced time to clinical resolution of 26 (95% CrI, 13-38) days. This resulted in an incremental cost-effectiveness ratio of A$2.10 (95% CrI, A$0.87-A$5.29) per day saved to clinical resolution (Table 2).
Table 2. Incremental Cost-effectiveness Analysis.
| Group | Mean Cost, A$ | Mean Time to Clinical Resolution, d |
|---|---|---|
| Usual care | 263.75 | 35 |
| Usual care with teledermoscopy | 318.39 | 9 |
| Difference (95% CrI) | 54.64 (22.69-97.35) | 26 (13-38) |
| Incremental cost-effectiveness ratio per day saved to clinical resolution (95% CrI) | 2.10 (0.87-5.29) | |
Abbreviation: CrI, credible interval.
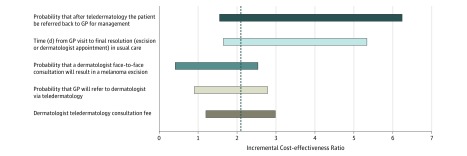
In 1-way sensitivity analyses, the most influential cost components were pathology testing (range of 1-2 tests), GP consultation fee (range of 1-3 appointments), and teledermoscopy dermatologist consultation fee (range of 50%-150%) (Figure 2). Influential probability components were the probability of a GP referring their patients via teledermoscopy, and the probability that after a teledermoscopy consultation the dermatologist would instruct the patient to return to their referring practitioner for diagnosis or treatment. As the number referred back to their GP decreased from 90% to 10%, the incremental cost-effectiveness ratio changed from A$1.55 to A$6.23 per day to clinical resolution. This was to be expected because the cost-effectiveness of teledermoscopy after implementation would depend on the uptake of referrals using teledermoscopy by GPs and the number of in-person dermatologist appointments avoided.
Figure 2. One-way Sensitivity Analysis for Model Inputs Expressed in Incremental Cost-effectiveness Ratio Values (Cost per Days to Clinical Resolution).
Output for a 1-way sensitivity analysis expressed as an incremental cost-effectiveness ratio in the form of a tornado diagram. GP indicates general practitioner. The dashed line at $2.10 indicates the mean incremental per day saved to clinical resolution.
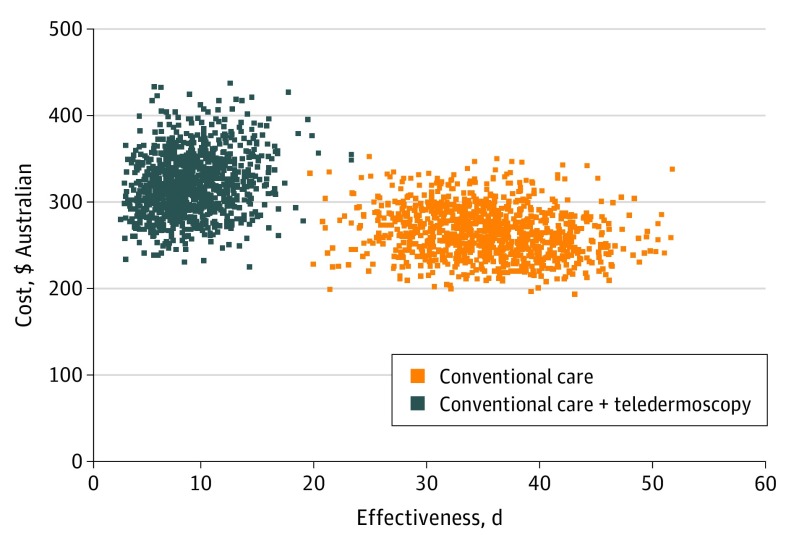
Results from the probabilistic sensitivity analyses showed costs ranging from A$22.69 to A$97.35 per person, and for time to clinical resolution from 13 to 38 days. This variation in estimates meant that the overall incremental cost-effectiveness ratio was estimated between A$0.87 and A$5.29 per day saved to resolution (Table 2). Figure 3 shows a clear separation between the cost-effectiveness ratios of teledermoscopy and usual care; teledermoscopy had a higher cost with faster clinical resolution than usual care within the modeled conditions.
Figure 3. Probabilistic Sensitivity Analysis Simulation for Cost-effectiveness (Cost per Days to Clinical Resolution).
Scatterplot output from the probabilistic sensitivity analysis simulation demonstrates a clear divide between the estimates for usual care and teledermoscopy care.
Discussion
Teledermoscopy referral has the potential to increase the efficiency of a dermoscopic case of care, reduce the rate of unnecessary biopsies, and reduce inappropriate referral for specialist consultations. To our knowledge, this is the first study to evaluate the economic impact of teledermoscopy referral for the management of suspected skin cancers in the Australian context. Under the modeled conditions, it was found that teledermoscopy referral would on average cost an additional A$54.64 per case compared with usual care but would reduce time to clinical resolution by 26 days. Although using teledermoscopy referral can increase the overall cost of treatment, the extra A$54.64 per case may be a justifiable cost for the Australian government for expedited diagnosis and treatment.
Consistent with our findings, studies in other countries have demonstrated that teledermoscopy services were of comparable or higher cost vs usual care with positive benefits.10,14,24,25,26 Internationally, teledermoscopy referral systems have been successfully piloted with benefits similar to those demonstrated by this model.8,9,10 These studies showed that when used as a referral method, teledermoscopy meant that 39% to 88% of patients did not have to attend an in-person consultation with their dermatologist and were able to be managed by their GP.14,26 Each patient referred to a dermatologist for a teledermoscopy consultation that resulted in GP management (rather than requiring an in-person dermatologist consultation) increased the cost-effectiveness of teledermoscopy referral because dermatologists attract a higher attendance fee than GPs (Figure 2). In addition, accurate dermatologist diagnosis via teledermoscopy has the potential to avoid erroneously excising benign neoplasms, preventing excision and histopathology costs. Teledermoscopy referral can optimize triage for in-person dermatologist appointments, due to the visual information about the condition,10,24,25 thereby ensuring that dermatologist appointments are available for urgent cases when required.14
In Australia, the government routinely reimburses real-time telehealth services (eg, video consultations) at a higher rate than in-person services. This measure is to incentivize telehealth use and occurs because practitioners are entitled to claim their standard attendance fee plus a telehealth item fee, which is generally equal to 50% of their attendance fees. The Australasian College of Dermatologists’ application to the Commonwealth’s Department of Health to fund teledermoscopy under Medicare proposed an equal reimbursement for store-and-forward teledermatology compared with in-person care; however, the application was not endorsed by the Medical Services Advisory Committee.16 Reducing the consultation fee for teledermoscopy (modeled in this study as equal to the in-person dermatologist reimbursement fee) increases the cost-effectiveness of the teledermoscopy service.
To effectively implement teledermoscopy services at the substitution rates that achieve desirable cost-effectiveness, a streamlined dermoscopic image capture process for general practice would be essential.7,27 Capturing dermoscopic images and completing a digital referral form could increase general practice appointment time by as much as 11:32 minutes (range, 7:02-26:44 minutes)28; this may serve as a disincentive to GPs in the Australian fee-for-service model. Using support staff could reduce this barrier to implementation: once the GP has identified the lesions of interest, they could capture the images and complete some of the digital referral.7,26
Further research around the clinical significance of expedited clinical resolution and its importance for patients could inform implementation recommendations for the Australian setting. The same goes for research into what consumers are willing to pay for teledermoscopy given its ability to reduce the time to clinical resolution. If teledermoscopy remains unfunded by the government, then patients may be willing to self-fund the service in a private capacity to reduce their travel and receive a faster specialist opinion.
Limitations
The model examined costs from the perspective of the Australian Commonwealth Government in community outpatient settings. The results are therefore only applicable to the Australian health care setting. This model was not applicable to patients treated through alternate clinical pathways, including those who receive inpatient treatment in a hospital. Due to limited data regarding teledermoscopy in Australia, probability data were sourced from select international clinical trials that demonstrated similar clinical pathways to Australia. Due to the comparatively high rate of skin cancer in Australia, the use of international probability data may underestimate skin cancer incidence and the impact of teledermoscopy. Sensitivity analysis was used to examine the impact of variations in probabilities. The model does not distinguish between GPs who are working in GP clinics and those working in skin cancer clinics; referral and excision rates for the later may vary from those presented.29
Although few previous economic models have examined the cost-effectiveness of teledermoscopy service provision, there are several randomized clinical trials and observational trials that have collected cost information alongside their clinical data.14,30 One strength of this study is that actual cost data were used to inform our model for all items except the teledermoscopy fee.
Several costs were excluded from the model, for example, those associated with hospital treatments or referrals managed in a hospital, biopsies, and the costs incurred by patients (co-payments and other out-of-pocket expenses). Patient-incurred costs are likely to be substantial for patients who need to travel from rural areas to access metropolitan dermatologists in the usual care scenario. Australia has travel subsidy and reimbursement schemes for eligible patients; however, they are only available to patients in the public hospital system, not those accessing care through community-based medical practices as described in this model. Therefore, if teledermoscopy as described in this model was examined from a societal perspective, it would likely have superior cost-effectiveness to usual care.
Not excising benign lesions that would otherwise be removed may be an optimal outcome for teledermoscopy. The change in excision rates for benign neoplasm as a measure of effectiveness assumes that optimal clinical resolution would be to leave benign neoplasms intact. However, patients often request benign lesions be excised for cosmetic, discomfort, or other reasons; therefore, the costs for benign lesion excision may have been underestimated.31,32
Time in days to clinical resolution was taken from a New Zealand study as the best available source. This is relevant to the Australian context because New Zealand also has a high incidence of skin cancers and a similar health system to the Australia.18 The use of international values may have the potential to underestimate or overestimate the time components in this model. However, the New Zealand values used to populate the model fall within the range of time in days to clinical resolution shown by other international studies. These other studies examining teledermoscopy referral reported 13 to 50 days when using teledermoscopy referral, and 61 to 138 days for usual care.8,9,10,33
Conclusions
Teledermoscopy for skin cancer referral and triage in Australia will increase the cost per case but reduce time to clinical resolution, when compared with usual care. Implementation recommendations depend on the preferences of the Australian health system decision makers for either lower cost or expedited clinical resolution.
References
- 1.Skin Cancer in Australia. Canberra, Australia: Australian Institute of Health and Welfare; 2016. [Google Scholar]
- 2.Börve A, Dahlén Gyllencreutz J, Terstappen K, et al. . Smartphone teledermoscopy referrals: a novel process for improved triage of skin cancer patients. Acta Derm Venereol. 2015;95(2):186-190. [DOI] [PubMed] [Google Scholar]
- 3.Congalton AT, Oakley AM, Rademaker M, Bramley D, Martin RC. Successful melanoma triage by a virtual lesion clinic (teledermatoscopy). J Eur Acad Dermatol Venereol. 2015;29(12):2423-2428. [DOI] [PubMed] [Google Scholar]
- 4.Moreno-Ramirez D, Ferrandiz L, Nieto-Garcia A, et al. . Store-and-forward teledermatology in skin cancer triage: experience and evaluation of 2009 teleconsultations. Arch Dermatol. 2007;143(4):479-484. [DOI] [PubMed] [Google Scholar]
- 5.Tan E, Yung A, Jameson M, Oakley A, Rademaker M. Successful triage of patients referred to a skin lesion clinic using teledermoscopy (IMAGE IT trial). Br J Dermatol. 2010;162(4):803-811. [DOI] [PubMed] [Google Scholar]
- 6.Finnane A, Dallest K, Janda M, Soyer HP. Teledermatology for the diagnosis and management of skin cancer: a systematic review. JAMA Dermatol. 2017;153(3):319-327. [DOI] [PubMed] [Google Scholar]
- 7.Caffery LJ, Farjian M, Smith AC. Telehealth interventions for reducing waiting lists and waiting times for specialist outpatient services: a scoping review. J Telemed Telecare. 2016;22(8):504-512. [DOI] [PubMed] [Google Scholar]
- 8.Lim D, Oakley AM, Rademaker M. Better, sooner, more convenient: a successful teledermoscopy service. Australas J Dermatol. 2012;53(1):22-25. [DOI] [PubMed] [Google Scholar]
- 9.Moreno-Ramirez D, Ferrandiz L, Ruiz-de-Casas A, et al. . Economic evaluation of a store-and-forward teledermatology system for skin cancer patients. J Telemed Telecare. 2009;15(1):40-45. [DOI] [PubMed] [Google Scholar]
- 10.Whited JD, Datta S, Hall RP, et al. . An economic analysis of a store and forward teledermatology consult system. Telemed J E Health. 2003;9(4):351-360. [DOI] [PubMed] [Google Scholar]
- 11.Argenziano G, Soyer HP. Dermoscopy of pigmented skin lesions—a valuable tool for early diagnosis of melanoma. Lancet Oncol. 2001;2(7):443-449. [DOI] [PubMed] [Google Scholar]
- 12.Bashshur RL, Shannon GW, Tejasvi T, Kvedar JC, Gates M. The empirical foundations of teledermatology: a review of the research evidence. Telemed J E Health. 2015;21(12):953-979. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Rosendahl C. Dermatoscopy in general practice. Br J Dermatol. 2016;175(4):673-674. [DOI] [PubMed] [Google Scholar]
- 14.Snoswell C, Finnane A, Janda M, Soyer HP, Whitty JA. Cost-effectiveness of store-and-forward teledermatology: a systematic review. JAMA Dermatol. 2016;152(6):702-708. [DOI] [PubMed] [Google Scholar]
- 15.Medicare Benefits Schedule Book. Canberra, Australia: Department of Health; 2016. [Google Scholar]
- 16.Australian Government Medical Services Advisory Committee Application No. 1360.1 – specialist dermatology services delivered by asynchronous store and forward technology. 2017. http://www.health.gov.au/internet/msac/publishing.nsf/Content/21799DF1CF99AC93CA25801000123C0D/$File/1360.1-FinalPSD-accessible.pdf. Accessed November 20, 2015.
- 17.Britt H, Miller GC, Henderson J, et al. . General Practice Activity in Australia 2013-2014. BEACH: Bettering the Evaluation and Care of Health. Sydney, Australia: Sydney University Press; 2014. [Google Scholar]
- 18.Morton CA, Downie F, Auld S, et al. . Community photo-triage for skin cancer referrals: an aid to service delivery. Clin Exp Dermatol. 2011;36(3):248-254. [DOI] [PubMed] [Google Scholar]
- 19.English DR, Del Mar C, Burton RC. Factors influencing the number needed to excise: excision rates of pigmented lesions by general practitioners. Med J Aust. 2004;180(1):16-19. [DOI] [PubMed] [Google Scholar]
- 20.Taylor R. Sensitivity and Specificity of Malignant Melanoma, Squamous Cell Carcinoma, and Basal Cell Carcinoma in a General Dermatological Practice [BA thesis]. Waco, TX: Baylor University; 2012.
- 21.Massone C, Maak D, Hofmann-Wellenhof R, Soyer HP, Frühauf J. Teledermatology for skin cancer prevention: an experience on 690 Austrian patients. J Eur Acad Dermatol Venereol. 2014;28(8):1103-1108. [DOI] [PubMed] [Google Scholar]
- 22.Gordon L, Youl PH, Elwood M, et al. . Diagnosis and management costs of suspicious skin lesions from a population-based melanoma screening programme. J Med Screen. 2007;14(2):98-102. [DOI] [PubMed] [Google Scholar]
- 23.Whited JD, Hall RP, Foy ME, et al. . Teledermatology’s impact on time to intervention among referrals to a dermatology consult service. Telemed J E Health. 2002;8(3):313-321. [DOI] [PubMed] [Google Scholar]
- 24.Datta SK, Warshaw EM, Edison KE, et al. . Cost and utility analysis of a store-and-forward teledermatology referral system: a randomized clinical trial. JAMA Dermatol. 2015;151(12):1323-1329. [DOI] [PubMed] [Google Scholar]
- 25.Pak HS, Datta SK, Triplett CA, Lindquist JH, Grambow SC, Whited JD. Cost minimization analysis of a store-and-forward teledermatology consult system. Telemed J E Health. 2009;15(2):160-165. [DOI] [PubMed] [Google Scholar]
- 26.Ferrándiz L, Ojeda-Vila T, Corrales A, et al. . Internet-based skin cancer screening using clinical images alone or in conjunction with dermoscopic images: a randomized teledermoscopy trial. J Am Acad Dermatol. 2017;76(4):676-682. [DOI] [PubMed] [Google Scholar]
- 27.Landow SM, Mateus A, Korgavkar K, Nightingale D, Weinstock MA. Teledermatology: key factors associated with reducing face-to-face dermatology visits. J Am Acad Dermatol. 2014;71(3):570-576. [DOI] [PubMed] [Google Scholar]
- 28.Berghout RM, Eminović N, de Keizer NF, Birnie E. Evaluation of general practitioner’s time investment during a store-and-forward teledermatology consultation. Int J Med Inform. 2007;76(suppl 3):S384-S391. [DOI] [PubMed] [Google Scholar]
- 29.Rosendahl C, Williams G, Eley D, et al. . The impact of subspecialization and dermatoscopy use on accuracy of melanoma diagnosis among primary care doctors in Australia. J Am Acad Dermatol. 2012;67(5):846-852. [DOI] [PubMed] [Google Scholar]
- 30.Eminović N, Dijkgraaf MG, Berghout RM, Prins AH, Bindels PJ, de Keizer NF. A cost minimisation analysis in teledermatology: model-based approach. BMC Health Serv Res. 2010;10:251. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Marks R, Jolley D, McCormack C, Dorevitch AP. Who removes pigmented skin lesions? a study of the ratio of melanoma to other benign pigmented tumors removed by different categories of physicians in Australia in 1989 and 1994. J Am Acad Dermatol. 1997;36(5, pt 1):721-726. [DOI] [PubMed] [Google Scholar]
- 32.Baade PD, Youl PH, Janda M, Whiteman DC, Del Mar CB, Aitken JF. Factors associated with the number of lesions excised for each skin cancer: a study of primary care physicians in Queensland, Australia. Arch Dermatol. 2008;144(11):1468-1476. [DOI] [PubMed] [Google Scholar]
- 33.Ferrándiz L, Moreno-Ramírez D, Ruiz-de-Casas A, et al. . An economic analysis of presurgical teledermatology in patients with nonmelanoma skin cancer [in Spanish]. Actas Dermosifiliogr. 2008;99(10):795-802. [PubMed] [Google Scholar]