Abstract
This diagnostic study compares the training efficacy of a novel web-based application to the publicly available Internet Curriculum For Melanoma Early Detection Skin Education Series to determine if intuitive visual diagnosis training is superior to a traditional rule-based algorithm in the diagnosis of melanomas.
The ABCD rule has long been the primary framework for teaching clinicians and patients to differentiate melanomas from benign lesions. However, it remains unclear that such rule-based methods are a substitute for pattern-recognition skills in the diagnosis of skin lesions.1,2 Dermatologists develop an innate sense of how melanomas appear after examining thousands of malignant and benign lesions. In contrast, most medical students are relatively disadvantaged by the paucity of their dermatology exposure. Thus, limited experience is the primary barrier to the development of pattern-recognition and intuition as a reliable tool for melanoma diagnosis in nonexperts.3 To remedy this problem, we developed a novel web-based application to mimic the training of a dermatologist by teaching medical students intuitive melanoma diagnosis in a highly condensed period of time.
Our application, Skinder, teaches intuitive visual diagnosis of melanoma by quickly presenting the learner with thousands of benign and malignant skin lesions. The user makes a rapid binary decision, by swiping right for benign or left for malignant, and receives instant feedback on accuracy. With this application, the learner can amass a mental repository of diagnostic experience in a short amount of time. To determine if intuitive visual diagnosis training is superior to a traditional rule-based algorithm, we compared our web-based application with the publicly available Internet Curriculum For Melanoma Early Detection (INFORMED) Skin Education Series.
Methods
This randomized diagnostic study was conducted on 36 medical students at a single institution. The study was approved by the West Virginia University institutional review board. All participants were financially compensated and provided written informed consent. Medical students, without a formal clinical dermatology rotation, were randomized into either the rule-based or application group. Each participant took a 32 image pretest where they were asked to determine if each lesion was a melanoma or a benign skin lesion. Participants were then given an hour of observed training time devoted to their assigned learning modality. Immediately following training, participants took a postassessment consisting of the same 32 images in randomized order to evaluate improvement. The pretest and posttest means of the 2 groups were compared using a simple t test. Participants also completed an exit questionnaire.
Results
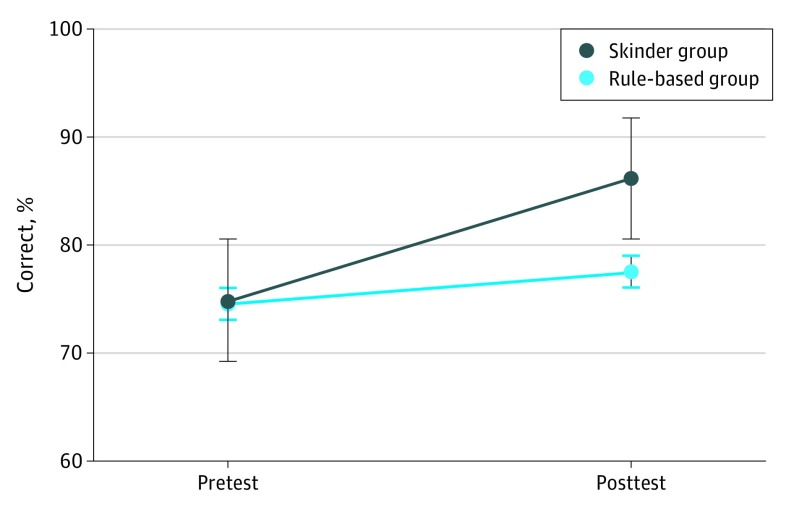
The pretest mean for the application group was 75% correct, compared with 74.7% correct for the INFORMED group. The posttest mean for the application group was 86.3% correct, compared with 77.5% correct for the INFORMED group. The posttest mean difference between the 2 groups represents a statistically significant improvement for the web-based application group (absolute difference, 9%; P = .003) (Figure). During the 60-minute training session, application users estimated that Skinder held their attention for 34.3 minutes, which is less than the 45.6 minutes estimated by INFORMED trainees. Overall, Skinder users believed they were more likely than INFORMED users to access their learning modality again if given the opportunity (Table).
Figure. Mean Percent Correct on Preassessments and Postassessments for Application and Rule-Based Groups.
This figure shows a statistically significant improvement in postassessment outcomes for users of Skinder (absolute difference, 9%; P = .003).
Table. Composite Results of Poststudy Questionnairea.
| Variable | Training | |
|---|---|---|
| Application | Rule-Based | |
| My learning modality held my attention. | 3.9 | 3.8 |
| I would recommend my learning modality to a colleague. | 3.9 | 3.9 |
| During the 60 minutes of allotted training, how long do you estimate your attention was held, in minutes? | 34.3 | 45.6 |
| If given the opportunity, how likely are you to use your learning modality in the future? | 3.6 | 3.4 |
| I think this type of training should be included in the medical curriculum. | 3.8 | 4.0 |
Evaluated using 1-5 point scale with 1 indicating “strongly disagree” and 5 indicating “strongly agree.”
Discussion
This study reinforces the importance of visual pattern recognition in clinical diagnosis4,5 and supports the premise that intuitive diagnosis is superior to rule-based algorithms. Despite its small sample size, this study supports that Skinder is a more effective learning tool for accurate diagnosis of melanoma than traditional rule-based methods. Future studies will expand the sample size as well as investigate the use of the application beyond medical students to include primary care physicians, nurses, and patients with the goal of early recognition of skin malignant abnormalities.
References
- 1.Aldridge RB, Zanotto M, Ballerini L, Fisher RB, Rees JL. Novice identification of melanoma: not quite as straightforward as the ABCDs. Acta Derm Venereol. 2011;91(2):125-130. doi: 10.2340/00015555-1070 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Girardi S, Gaudy C, Gouvernet J, Teston J, Richard MA, Grob JJ. Superiority of a cognitive education with photographs over ABCD criteria in the education of the general population to the early detection of melanoma: a randomized study. Int J Cancer. 2006;118(9):2276-2280. [DOI] [PubMed] [Google Scholar]
- 3.Aldridge RB, Maxwell SS, Rees JL. Dermatology undergraduate skin cancer training: a disconnect between recommendations, clinical exposure and competence. BMC Med Educ. 2012;12:27. doi: 10.1186/1472-6920-12-27 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.McWhirter JE, Hoffman-Goetz L. Visual images for patient skin self-examination and melanoma detection: a systematic review of published studies. J Am Acad Dermatol. 2013;69(1):47-55. Published online March 6, 2013. doi: 10.1016/j.jaad.2013.01.031 [DOI] [PubMed] [Google Scholar]
- 5.Aldridge RB, Glodzik D, Ballerini L, Fisher RB, Rees JL. Utility of non-rule-based visual matching as a strategy to allow novices to achieve skin lesion diagnosis. Acta Derm Venereol. 2011;91(3):279-283. doi: 10.2340/00015555-1049 [DOI] [PMC free article] [PubMed] [Google Scholar]