This cross-sectional epidemiologic study investigates whether urban residence is associated with greater odds for psychosis in low- and middle-income countries among respondents to the World Health Organization World Health Survey.
Key Points
Question
Is urban living associated with elevated odds for psychotic experiences or psychotic disorder in low- and middle-income countries?
Findings
In this cross-sectional epidemiological study of 42 countries and 215 682 participants, urban residence was not associated with increased odds of psychotic experiences or psychotic disorders.
Meaning
The association between urban living and psychosis, widely replicated in high-income countries, may not generalize to low- and middle-income countries, where 80% of the world’s population resides.
Abstract
Importance
Urban residence is one of the most well-established risk factors for psychotic disorder, but most evidence comes from a small group of high-income countries.
Objective
To determine whether urban living is associated with greater odds for psychosis in low- and middle-income countries (LMICs).
Design, Setting, and Participants
This international population-based study used cross-sectional survey data collected as part of the World Health Organization (WHO) World Health Survey from May 2, 2002, through December 31, 2004. Participants included nationally representative general population probability samples of adults (≥18 years) residing in 42 LMICs (N = 215 682). Data were analyzed from November 20 through December 5, 2017.
Exposures
Urban vs nonurban residence, determined by the WHO based on national data.
Main Outcomes and Measures
Psychotic experiences, assessed using the WHO Composite International Diagnostic Interview psychosis screen, and self-reported lifetime history of a diagnosis of a psychotic disorder.
Results
Among the 215 682 participants (50.8% women and 49.2% men; mean [SD] age, 37.9 [15.7] years), urban residence was not associated with psychotic experiences (odds ratio [OR], 0.99; 95% CI, 0.89-1.11) or psychotic disorder (OR, 0.89; 95% CI, 0.76-1.06). Results of all pooled analyses and meta-analyses of within-country effects approached a null effect, with an overall OR of 0.97 (95% CI, 0.87-1.07), OR for low-income countries of 0.98 (95% CI, 0.82-1.15), and OR for middle-income countries of 0.96 (95% CI, 0.84-1.09) for psychotic experiences and an overall OR of 0.92 (95% CI, 0.73-1.16), OR for low-income countries of 0.92 (95% CI, 0.66-1.27), and OR for middle-income countries of 0.92 (95% CI, 0.67-1.27) for psychotic disorder.
Conclusions and Relevance
Our results provide evidence that urbanicity, a well-established risk factor for psychosis, may not be associated with elevated odds for psychosis in developing countries. This finding may provide better understanding of the mechanisms by which urban living may contribute to psychosis risk in high-income countries, because urban-rural patterns of cannabis use, racial discrimination, and socioeconomic disparities may vary between developing and developed nations.
Introduction
Urbanicity is among the most well-established environmental risk factors for psychotic disorders, with nearly 8 decades of research reporting a positive association across various sampling approaches and definitions of urban exposure, time of exposure, onset of symptoms, and definition of illness.1,2,3 Meta-analysis4 has shown that the risk of developing schizophrenia is approximately 2.37 times greater in urban compared with rural settings and is associated with the level of density of the urban environment and population density in a dose-response fashion that suggests the possibility of a causal effect. Potential mechanisms that have been hypothesized include ethnic minority status, stress of urban living, greater urban prevalence of substance use, and toxic exposures that may be related to city dwelling.5 Although these mechanisms are plausible, studies have found that the association between urbanicity and psychosis is broadly robust to adjustment for these factors.6,7
Despite these well-replicated findings, most studies of urbanicity and psychosis have been conducted in high-income countries in Europe or North America or in Australia.4,6,8 The association between urbanicity and psychosis is understudied in low- and middle- income countries (LMICs), although LMICs are home to greater than 80% of the world’s population. Some factors that characterize urban-rural differences in high-income countries may not generalize to many LMICs, where urban living may indicate greater access to resources rather than greater exposure to social adversity.9,10 As such, the literature on urbanicity and psychosis has been less consistent in LMICs, finding significant associations in some countries (eg, Uganda11,12 and Nigeria13) but not others (eg, Mozambique14,15 and India16,17,18).
The World Health Organization’s (WHO) World Health Survey (WHS)19 presented a unique opportunity to examine the association between urbanicity and psychosis in LMICs in a large sample (N = 215 682). Using data from 42 LMICs, we tested whether urban environments in these countries were associated with elevated odds for (1) subthreshold psychotic experiences and (2) self-reported diagnoses of psychotic disorder.
Methods
World Health Survey
The WHS was a cross-sectional survey conducted in 70 countries from May 2, 2002, through December 31, 2004. Survey details are available from the WHO.19 All countries included in our analyses used multistage, random cluster sampling, stratified by sex, age, and residential area (rural or urban). All adults 18 years or older with a valid home address were assigned a nonzero chance of inclusion. Standard translation procedures were followed to ensure comparability across countries. Face-to-face and telephone interviews were conducted by trained interviewers. Individual level response rates were greater than 82%. Poststratification corrections were made to sampling weights to adjust for nonresponse and the population distribution reported by the United Nations Statistical Division. Data from 69 countries were publicly available. Twenty-seven countries were excluded from analysis (the list and rationale are given in eTable 1 in the Supplement). A total of 42 countries were included in the final sample of 215 682 respondents. According to the World Bank classification in 2003 (at the time of the survey), these countries corresponded to 17 low-income countries (86 437 respondents) and 25 middle-income countries (129 245 respondents). Ethical boards at each study site (listed in eTable 2 in the Supplement) approved the study with written informed consent being obtained from all participants after the nature of the procedure has been fully explained. Secondary analyses of these publicly available deidentified data were determined to be exempt from institutional ethical review (Office for Human Research Protections category 4 exemption), determined through consultation between us and the institutional review board of Fordham University.
Variables
Exposure: Urban Residence
Urban residence was defined as a dichotomous variable based on the respondent’s place of residence at the time of the survey. Each country defined the categories of rural and urban and provided the definitions to the WHO to allow for stratified sampling and analytic comparison between countries. Although the specific criteria used by each country to define urban vs rural areas were not publicly released, the estimates of urbanicity for each country are consistent with contemporaneous (2003) urbanicity data used by the World Bank that are based on the United Nations world urbanization prospects report (eTable 3 in the Supplement).20 Six countries varied notably (>10%) from World Bank estimates of urbanicity, but study results were not meaningfully changed when these countries were excluded from analyses. To further validate the WHS measure of urbanicity, we examined whether WHS-defined urban areas had higher rates of known transnational indicators of urban living (eg, percentage of jobs in agriculture, household television ownership, and household electricity), confirming that households identified as urban in the WHS conformed to common validated characteristics of urban areas (eTables 4 and 5 in the Supplement).21
Outcomes: Psychotic Experiences and Psychotic Disorder
All participants were asked questions about psychotic symptoms that came from the WHO Composite International Diagnostic Interview (CIDI), version 3.0.22 The psychosis module of the CIDI has been reported to be highly consistent with clinician ratings in a clinical sample.23 Specifically, respondents were asked the following questions with answer options of yes or no: During the last 12 months, have you experienced (1) a feeling something strange and unexplainable was going on that other people would find hard to believe? (delusional mood); (2) a feeling that people were too interested in you or there was a plot to harm you? (delusions of reference and persecution); (3) a feeling that your thoughts were being directly interfered or controlled by another person or your mind was being taken over by strange forces? (delusions of control); or (4) an experience of seeing visions or hearing voices that others could not see or hear when you were not half asleep, dreaming, or under the influence of alcohol or drugs? (hallucinations). Individuals who endorsed at least 1 of these 4 symptoms were considered to have psychotic experiences.24
The secondary outcome of this study was a self-reported lifetime history of a psychotic disorder. Participants were asked whether they had ever received a diagnosis of schizophrenia or psychotic disorder with yes and no answer options. Hereafter, we refer to this condition as psychotic disorder for brevity.
Statistical Analysis
Data were analyzed from November 20 through December 5, 2017. The statistical analysis was accomplished in Stata software (release 14.1; StataCorp, LP).25 A descriptive analysis was conducted using unweighted numbers and weighted proportions. Countrywise age- and sex-adjusted prevalence estimates for psychotic experiences and psychotic disorder (overall and by urban residence) were calculated using the United Nations population pyramids for the year 2010 as the standard population.26 For analyses on psychotic experiences, individuals with psychotic disorder (n = 1996) were excluded because psychotic experiences, by definition, do not reach the clinical threshold for a psychosis diagnosis. Countrywise multivariable logistic regression models adjusted for age (continuous variable) and sex were constructed to assess the association between urban residence (exposure) and psychotic experiences or psychotic disorder (outcomes). Separate logistic regression models were used for each outcome, rather than multinomial regression, to avoid potentially inflating effect sizes for respondents with psychotic disorder by excluding respondents with psychotic experiences from the control group. The estimates for each country were combined into a random-effects meta-analysis. We calculated Higgins I2 statistics to assess the level of between-country heterogeneity that is not explained by sampling error. Heterogeneity of less than 40% is conventionally regarded as negligible.27
Analyses using the overall sample and by country income level were conducted. Exploratory analyses tested associations between urbanicity and psychotic experiences separately between younger adults (ages 18-29 years) and the remainder of the sample (ages ≥30 years), given the particular significance of young adulthood in the etiology of psychosis.28,29 We did not use multilevel models because such analyses can produce biased estimates when used with complex study designs.30 The analytic approach of conducting meta-analyses with random effects based on countrywise estimates has been used in previous WHS publications.24,31 The percentage of missing values for each variable used in the analysis were 6.1% for psychotic disorder, 12.3% for psychotic experiences, 3.5% for age, 3.5% for sex, and 0.7% for urban residence. Cases with missing values were excluded in our complete case analysis of the data.
The sample weighting and the complex study design were taken into account in all analyses. Data on the clusters and strata in addition to the sampling weight were provided in the data set, and incorporation of these 3 elements with the Taylor linearization methods allowed for calculation of nationally representative estimates. Results from the logistic regression models are presented as odds ratios (ORs) with 95% CIs. The level of statistical significance was set at P < .05. Based on our a priori power analysis, we calculated a 99% chance (1 − β≥0.99) of detecting small effects (OR, ≥1.06 for psychotic experiences and 1.20 for psychotic disorder) in our 2-tailed logistic regression analyses (α = .05). We did not adjust the P value for multiple comparisons to avoid type II errors. Thus, significant countrywise estimates should be interpreted with caution because some may have occurred by chance.
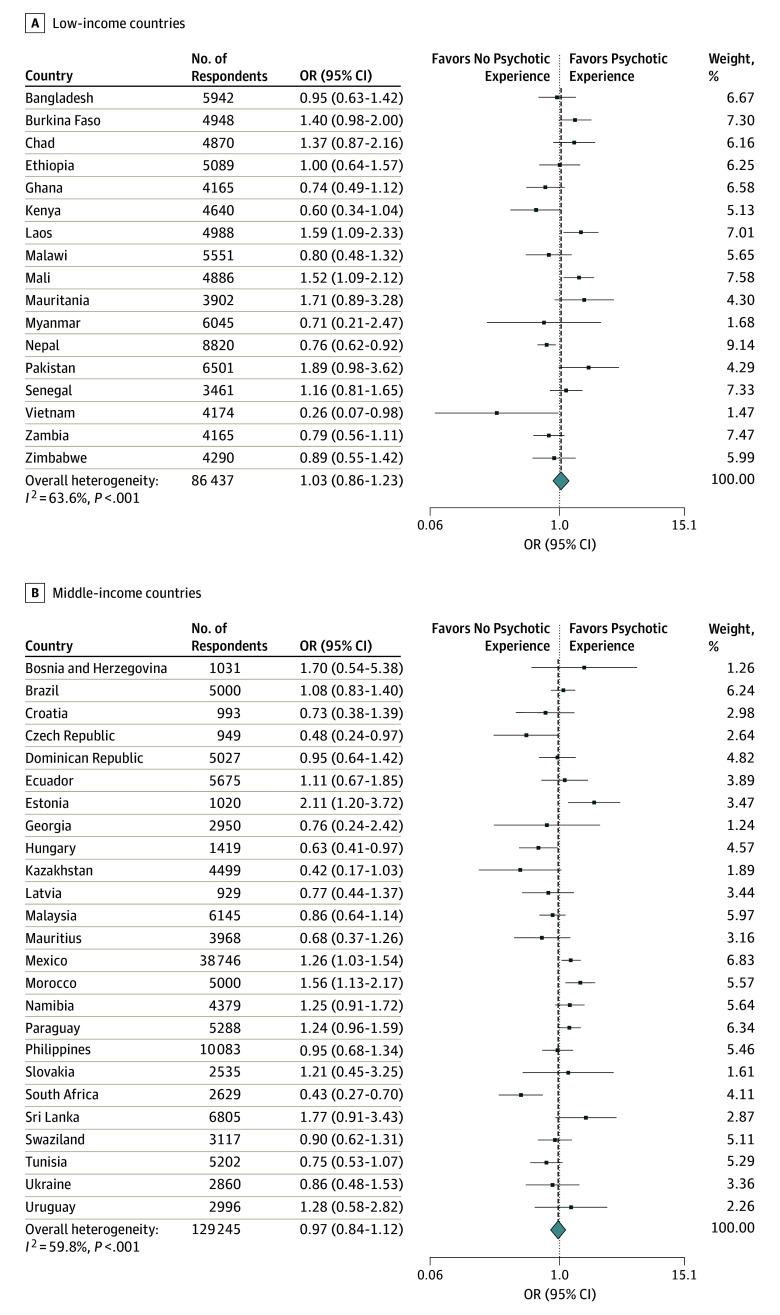
Results
The analytical sample consisted of 215 682 individuals with a mean (SD) age of 37.9 (15.7) years (50.8% women and 49.2% men). Overall, 46.2% were urban residents, but this proportion was higher in middle-income countries than in low-income countries (67.6% vs 28.7%). The prevalence of psychotic experiences was 13.0% (low-income countries, 10.2%; middle-income countries, 16.6%); of psychotic disorder, 0.9% (low-income countries, 1.0%; middle-income countries, 0.9%). The countrywise age- and sex-adjusted prevalence of psychotic experience and psychotic disorder (and by urban-rural residence) is shown in the Table. The countrywise associations between urban residence and psychotic experiences by country income level estimated by multivariable logistic regression are shown in Figure 1. At an individual country level, we found a significant positive association between urban residence and psychotic experiences in Laos (OR, 1.59; 95% CI, 1.09-2.33), Mali (OR, 1.52; 95% CI, 1.09-2.12), Estonia (OR, 2.11; 95% CI, 1.20-3.72), Mexico (OR, 1,26; 95% CI, 1.03-1.54), and Morocco (OR, 1.56; 95% CI, 1.13-2.17) and a significant negative association between urban residence and psychotic experiences in Nepal (OR, 0.76; 95% CI, 0.62-0.92), Vietnam (OR, 0.26; 95% CI, 0.07-0.98), Hungary (OR, 0.63; 95% CI, 0.41-0.97), and South Africa (OR, 0.43; 95% CI, 0.27-0.70). Overall, no significant association of urban residence with psychotic experiences was found in low-income countries (pooled OR, 1.03; 95% CI, 0.86-1.23) and middle-income countries (pooled OR, 0.97; 95% CI, 0.84-1.12). A moderate level of heterogeneity between countries was indicated (I2 = 61%; 95% CI, 45%-72%). The pooled OR for the association between urbanicity and psychotic experiences for all LMICs was 0.99 (95% CI, 0.89-1.11). Associations between urbanicity and psychotic experiences were nonsignificant when examined separately between younger adults (aged 18-29 years) and those 30 years or older (eFigures 1 and 2 in the Supplement). Multivariable logistic regression analysis pooling all countries and adjusting for age, sex, and country yielded a similar result of an overall OR of 0.97 (95% CI, 0.87-1.07), OR for low-income countries of 0.98 (95% CI, 0.82-1.15), and OR for middle-income countries of 0.96 (95% CI, 0.84-1.09).
Table. Age- and Sex-Adjusted Prevalence of Psychotic Disorder and Psychotic Experience.
| Countries | Unweighted No. of Respondents | Age- and Sex-Adjusted Weighted Prevalence, % (SE)a | |||||
|---|---|---|---|---|---|---|---|
| Psychotic Disorder | Psychotic Experience | ||||||
| Overall | Urban Residence | Rural Residence | Overall | Urban Residence | Rural Residence | ||
| Low-income countries | |||||||
| Bangladesh | 5942 | 0.7 (0.2) | 1.0 (0.3) | 0.7 (0.2) | 13.1 (1.2) | 12.6 (1.7) | 13.2 (1.5) |
| Burkina Faso | 4948 | 1.3 (0.3) | 1.0 (0.5) | 1.3 (0.3) | 23.3 (1.9) | 26.9 (2.3) | 22.5 (2.3) |
| Chad | 4870 | 3.1 (0.4) | 3.4 (0.9) | 3.0 (0.4) | 16.3 (1.6) | 18.7 (2.6) | 15.4 (1.9) |
| Ethiopia | 5089 | 1.5 (0.2) | 2.3 (0.7) | 1.3 (0.2) | 16.6 (0.8) | 14.8 (2.7) | 16.9 (0.8) |
| Ghana | 4165 | 0.7 (0.1) | 0.9 (0.3) | 0.5 (0.1) | 4.9 (0.5) | 4.1 (0.6) | 5.5 (0.6) |
| Kenya | 4640 | 0.8 (0.2) | 0.9 (0.5) | 0.7 (0.2) | 17.9 (1.4) | 11.9 (2.8) | 19.9 (1.0) |
| Laos | 4988 | 0.4 (0.1) | 0.7 (0.3) | 0.3 (0.1) | 5.7 (0.5) | 7.7 (1.1) | 5.2 (0.5) |
| Malawi | 5551 | 1.2 (0.2) | 0.8 (0.5) | 1.3 (0.2) | 4.7 (0.6) | 5.0 (1.2) | 4.8 (0.6) |
| Mali | 4886 | 2.2 (0.4) | 1.2 (0.5) | 2.7 (0.5) | 14.1 (0.9) | 17.3 (2.2) | 12.5 (0.9) |
| Mauritania | 3902 | 2.6 (0.5) | 2.5 (0.7) | 3.0 (0.7) | 9.6 (1.2) | 11.3 (1.6) | 7.1 (1.9) |
| Myanmar | 6045 | 0.3 (0.1) | 0.4 (0.2) | 0.3 (0.2) | 2.6 (0.6) | 2.0 (1.1) | 2.9 (0.7) |
| Nepal | 8820 | 2.6 (0.2) | 1.9 (0.5) | 2.7 (0.2) | 45.1 (0.8) | 39.1 (2.6) | 46.2 (0.8) |
| Pakistan | 6501 | 1.1 (0.2) | 1.0 (0.3) | 1.1 (0.2) | 2.0 (0.3) | 2.9 (0.7) | 1.5 (0.3) |
| Senegal | 3461 | 1.4 (0.3) | 0.7 (0.2) | 2.0 (0.6) | 18.7 (1.4) | 19.9 (1.9) | 17.8 (2.0) |
| Vietnam | 4174 | 0.1 (0.03) | 0 (0) | 0.1 (0.04) | 0.7 (0.2) | 0.3 (0.2) | 0.8 (0.3) |
| Zambia | 4165 | 0.6 (0.1) | 0.9 (0.4) | 0.6 (0.1) | 10.6 (0.8) | 9.3 (1.3) | 11.4 (1.0) |
| Zimbabwe | 4290 | 1.1 (0.2) | 0.7 (0.4) | 1.3 (0.3) | 8.5 (0.8) | 8.3 (1.2) | 8.7 (1.1) |
| Middle-income countries | |||||||
| Bosnia and Herzegovina | 1031 | 0.1 (0.1) | 0.1 (0.1) | 0.1 (0.1) | 1.8 (0.5) | 2.4 (0.9) | 1.2 (0.5) |
| Brazil | 5000 | 1.7 (0.2) | 1.7 (0.2) | 1.6 (0.5) | 31.6 (0.9) | 31.7 (1.0) | 30.9 (2.6) |
| Croatia | 993 | 2.0 (0.5) | 1.7 (0.6) | 2.5 (1.1) | 7.3 (1.1) | 6.6 (1.4) | 9.2 (1.9) |
| Czech Republic | 949 | 0.4 (0.2) | 0.5 (0.3) | 0.1 (0.1) | 9.0 (1.5) | 7.1 (1.3) | 13.8 (3.6) |
| Dominican Republic | 5027 | 1.0 (0.2) | 0.7 (0.2) | 1.4 (0.5) | 21.5 (1.3) | 21.3 (1.7) | 22.1 (2.6) |
| Ecuador | 5675 | 0.9 (0.2) | 1.0 (0.3) | 0.9 (0.3) | 8.9 (1.0) | 9.1 (1.2) | 8.5 (1.7) |
| Estonia | 1020 | 1.5 (0.5) | 2.0 (0.6) | 0.2 (0.2) | 11.8 (1.2) | 14 (1.7) | 6.6 (1.6) |
| Georgia | 2950 | 0.5 (0.2) | 0.5 (0.3) | 0.5 (0.2) | 1.8 (0.5) | 1.5 (0.7) | 1.8 (0.5) |
| Hungary | 1419 | 2.4 (0.5) | 2.1 (0.7) | 3.1 (0.7) | 6.7 (0.7) | 5.6 (0.9) | 8.7 (1.2) |
| Kazakhstan | 4499 | 0.5 (0.1) | 0.3 (0.1) | 0.8 (0.3) | 3.0 (0.6) | 1.9 (0.6) | 4.5 (1.3) |
| Latvia | 929 | 0.8 (0.4) | 0.8 (0.5) | 0.7 (0.7) | 13.7 (1.7) | 12.8 (2.1) | 15.5 (2.9) |
| Malaysia | 6145 | 0.2 (0.1) | 0.2 (0.1) | 0.1 (0.1) | 7.1 (0.5) | 6.6 (0.6) | 7.8 (0.8) |
| Mauritius | 3968 | 0.6 (0.1) | 0.4 (0.1) | 0.8 (0.2) | 7.7 (1.0) | 6.3 (1.4) | 9.1 (1.5) |
| Mexico | 38 746 | 0.4 (0.04) | 0.4 (0.1) | 0.3 (0.1) | 8.7 (0.3) | 9.1 (0.4) | 7.5 (0.6) |
| Morocco | 5000 | 0.7 (0.2) | 0.7 (0.3) | 0.5 (0.2) | 17.6 (1.2) | 19.6 (1.8) | 14.5 (1.3) |
| Namibia | 4379 | 3.0 (0.4) | 3.3 (1.1) | 3.0 (0.5) | 10.9 (0.8) | 12.2 (1.4) | 10.1 (0.9) |
| Paraguay | 5288 | 0.5 (0.1) | 0.4 (0.1) | 0.5 (0.2) | 9.0 (0.5) | 9.6 (0.8) | 8.2 (0.6) |
| Philippines | 10 083 | 0.4 (0.1) | 0.3 (0.1) | 0.6 (0.1) | 8.9 (0.7) | 8.8 (0.9) | 9.1 (1.0) |
| Slovakia | 2535 | 0.3 (0.1) | 0.4 (0.2) | 0 (0) | 9.6 (1.7) | 10.4 (1.5) | 8.4 (3.3) |
| South Africa | 2629 | 1.2 (0.3) | 0.9 (0.3) | 1.6 (0.5) | 14.9 (1.6) | 10.4 (1.4) | 21.1 (3.2) |
| Sri Lanka | 6805 | 0.6 (0.2) | 0.8 (0.7) | 0.6 (0.1) | 2.2 (0.3) | 3.3 (0.8) | 1.9 (0.4) |
| Swaziland | 3117 | 6.2 (0.9) | 6.4 (1.2) | 6.4 (1.1) | 17.8 (1.3) | 17.1 (2.0) | 18.0 (1.5) |
| Tunisia | 5202 | 1.9 (0.3) | 1.7 (0.3) | 2.2 (0.5) | 14.7 (1.2) | 13.2 (1.6) | 17.4 (1.7) |
| Ukraine | 2860 | 0.6 (0.1) | 0.6 (0.2) | 0.5 (0.3) | 7.1 (0.9) | 6.7 (1.0) | 7.9 (1.9) |
| Uruguay | 2996 | 0.7 (0.1) | 0.8 (0.1) | 0.6 (0.4) | 5.5 (1.1) | 5.6 (1.2) | 4.2 (1.4) |
All age- and sex-adjusted weighted estimates were calculated using the United Nations population pyramids for 2010.26
Figure 1. Countrywise Association Between Urban Residence (Exposure) and Psychotic Experience (Outcome) by Country Income Level .
Associations are estimated with multivariable logistic regression adjusting for age and sex. The overall estimate and weights were calculated by random-effects meta-analysis. OR indicates odds ratio; diamond, heterogeneity.
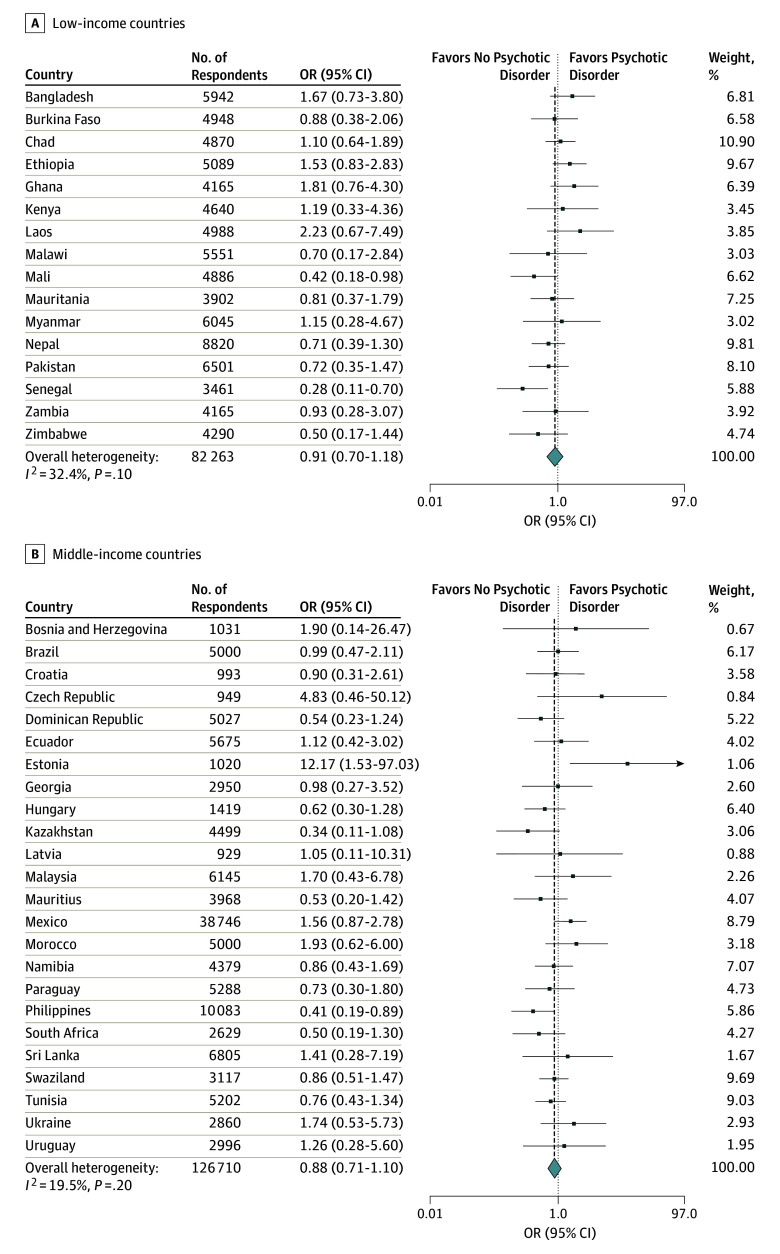
The countrywise associations between urban residence and psychotic disorder by country income level estimated by multivariable logistic regression are shown in Figure 2. Urban residents had significantly higher odds for psychotic disorder only in Estonia (OR, 12.17; 95% CI, 1.53-97.03), whereas significantly lower odds was observed in Mali (OR, 0.42; 95% CI, 0.18-0.98), Senegal (OR, 0.28; 95% CI, 0.11-0.70), and the Philippines (OR, 0.41; 95% CI, 0.19-0.89). A low level of heterogeneity was indicated among countries (I2 = 23%; 95% CI, 0%-48%). The pooled OR for the association between urbanicity and psychotic disorder for all LMICs was 0.89 (95% CI, 0.76-1.06). Multivariable logistic regression analysis pooling all countries and adjusting for age, sex, and country yielded similar results with an overall OR of 0.92 (95% CI, 0.73-1.16), OR for low-income countries of 0.92 (95% CI, 0.66-1.27), and OR for middle-income countries of 0.92 (95% CI, 0.67-1.27).
Figure 2. Countrywise Association Between Urban Residence (Exposure) and Psychotic Disorder (Outcome) by Country Income Level.
Associations are estimated with multivariable logistic regression adjusting for age and sex. Estimates for Vietnam and Slovakia could not be obtained because no individuals were found with psychotic disorder in one of the settings (ie, rural or urban). The overall estimate and weights were calculated by random-effects meta-analysis. OR indicates odds ratio; diamond, heterogeneity.
Discussion
Main Findings
The primary finding of this study was that urban living was not associated with subthreshold psychotic experiences or self-reported psychotic disorder in a large sample of adults from 42 LMICs. This finding was true for low-income countries and middle-income countries. In contrast, research to date, primarily in Western high-income countries,2,3,4 links urban living with psychosis. The large sample and limited adjustments in our analysis (age and sex only) indicate that our null findings are not attributable to a lack of statistical power or overspecification of our models because we had sufficient power to detect even small effects (power of 0.99 to detect an OR≥1.06 for psychotic experiences and OR≥1.20 for psychotic disorder). Furthermore, the high response rate of the WHS and our inclusion of only countries that used nationally representative probability samples reduces the likelihood that our null findings can be better explained by sampling error or other methodologic biases.
Potential Mechanisms and Their Variance Between High-Income Countries and LMICs
Combining the findings of this large study with the existing body of literature, which consists of mainly high-income country samples, suggests that the association between urban living and psychosis may be exclusive to high-income countries. Furthermore, a recent review of the literature in China (a middle-income country)32 showed a shift from having no association to a significant association between urbanicity and schizophrenia as the country underwent rapid urbanization in 2 decades. This discrepancy in findings between high-income countries and LMICs has important implications about urbanicity as a risk factor for psychosis, because understanding how urban-rural settings differ in high-income countries but not in LMICs can give us clues as to what urbanicity may be a proxy for in those settings. Speculatively, urban-rural disparities in economic deprivation and social isolation in high-income countries may not be present or may be less evident in LMICs. Affluent members of society tend to populate suburban areas in high-income countries, which differs from developing countries.3 Furthermore, familial and social cohesion may remain stronger in urban areas of developing countries.33 A recent English study,34 for example, demonstrated that the risk for psychosis is also elevated in nonurban areas with low social cohesion and high poverty (which are typically features of urban environments). In addition, high-income countries typically have relatively large immigrant and ethnic minority populations compared with LMICs (which may have more within-country migration), and these individuals typically reside in urban areas.35,36 This idea is consistent with past findings from high-income countries that show a reduced association between urbanicity and psychosis among racial/ethnic minorities who reside in areas of high within-group ethnic density.37,38 However, immigration factors and race/ethnicity may not explain discrepancies in urban effects between high-income countries and LMICs, because migration within a country and within areas with the same majority ethnic group carries similar mental health risks39; however, this has not specifically been examined in relation to psychosis, to our knowledge. Furthermore, LMICs are known to host most of the world’s refugees,40 particularly in urban areas, and these individuals may be at greater risk for psychosis.41
Another factor is that cannabis use is more common in cities compared with rural areas in high-income countries but is less prevalent overall in most LMICs.10 However, this difference may be offset by the availability of other potentially psychotogenic substances such as khat42; untangling these associations will require greater understanding of the urban-rural distribution of substances in LMICs as well as more conclusive data regarding which substances may be causally related to psychosis onset. Other possible factors include genetic selection effects, because individuals at genetic risk for schizophrenia have a greater tendency to cluster and remain in the same place in urban settings in some high-income countries (ie, the Netherlands, Dutch Belgium, and Sweden,43,44,45 but not consistently across age groups in Denmark46), although why a similar effect would not be present in LMICs is not clear. Urban-rural differences in stress reactivity and trauma exposure may also underlie the urbanicity effect,47 although evidence from cardiovascular risk research suggests that urban-rural differences in stress level appear to also generalize to LMICs.48 Finally, various other biological mechanisms have been proposed to explain the urban-rural difference in high-income countries, including greater ownership of cats in enclosed spaces, which can lead to toxoplasmosis infection,49 greater air pollution exposure (although this tends to be more rather than less pronounced in LMICs50), and less sun exposure and more vitamin D deficiency in high-income countries,51 all of which warrant further exploration in future studies.
Strengths and Limitations
Strengths of the present study include a large multinational sample that allowed sufficient statistical power to draw conclusions from null results. The null result was replicated across psychotic disorders and psychotic experiences, as well as across low-income countries and middle-income countries, with each replication consisting of a meta-analysis of data across 42 countries and thousands of individuals and yielding similar final effect sizes, all of which approached an OR of 1.00 (ie, a null effect). The inclusion of 42 LMICs allowed comparison of statistical effects across nations without publication bias, as may be present when comparing results across single-country studies.
A limitation of this study is that we could not directly compare LMICs with a globally representative range of high-income countries in the same data set. The association between urbanicity and psychosis may not be as consistent across all high-income countries, given that a large proportion of studies published to date have come from a few high-income countries.2,3,4 Of note, recent data from the multinational European Network of National Schizophrenia Networks Studying Gene-Environment Interactions52 found no urbanicity effect in data pooled across 5 high-income European countries and Brazil and found in their within-country analysis that urban living was only associated with greater incidence of psychosis in England and the Netherlands.
Because the data are cross-sectional, we were not able to differentially explore the effect of living in an urban environment at different life stages. The literature on urbanicity and psychosis from high-income countries benefits from greater availability of longitudinal data,4 and the discrepancy of findings may in part be explained by our use of psychosis prevalence rather than incidence data to study urbanicity as a risk factor. However, no data set exists, to our knowledge, that combines the broad LMIC representativeness of the WHS with a longitudinal survey design.
Psychotic experiences were assessed using the WHO CIDI screen, which does not attempt to exclude experiences that may be culturally appropriate. However, past studies24,31,53,54 have shown that psychotic experiences assessed using this measure are associated with clinical indicators across the entire range of LMICs included in this data set (eg, medical problems, sleep disturbances, and stress sensitivity), suggesting that they are indexing phenomena that are clinically meaningful (on average) and are not entirely driven by misclassification of culturally appropriate experiences.
The use of a single self-report item to identify cases of psychotic disorder was also a limitation although is consistent with prior psychiatric epidemiologic work. The overall prevalence of psychotic disorders in the countries included in the study was 0.9%, which is similar to previously reported figures in the general population.55 Furthermore, the results were consistent across diagnoses of psychotic disorder and psychotic experiences.
Conclusions
In the largest study to date, to our knowledge, of the association between urbanicity and psychosis in LMICs, we found that urban living was not associated with psychotic experiences or psychotic disorder. These findings contrast with the existing body of literature on this subject, which has been conducted primarily in high-income countries. This divergence suggests that the association between urbanicity and psychosis, rather than being a universal phenomenon, may be a feature of industrialized countries only. Further research is needed to clarify the causative factors underlying this differential relationship between LMICs and high-income countries.
eTable 1. WHS Countries That Were Excluded From Data Analysis
eTable 2. Included Study Sites and Ethical Approving Bodies
eTable 3. Comparison Between WHS- and World Bank–Defined Urbanicity (2003 Data) for Each Country Included in the Study Sample
eTable 4. Indicators of Urbanicity by WHS-Defined Rural and Urban Setting in Low-Income Countries
eTable 5. Indicators of Urbanicity by WHS-Defined Rural and Urban Setting in Middle-Income Countries
eFigure 1. Countrywise Association Between Urban Residence (Exposure) and Psychotic Experience (Outcome) Among Individuals Aged 18-29 Years
eFigure 2. Countrywise Association Between Urban Residence (Exposure) and Psychotic Experience (Outcome) Among Individuals 30 or Older
References
- 1.Faris REL, Dunham HW. Mental Disorders in Urban Areas: An Ecological Study of Schizophrenia And Other Psychoses. Oxford, England: University of Chicago Press; 1939. [Google Scholar]
- 2.March D, Hatch SL, Morgan C, et al. Psychosis and place. Epidemiol Rev. 2008;30(1):84-100. [DOI] [PubMed] [Google Scholar]
- 3.Padhy SK, Sarkar S, Davuluri T, Patra BN. Urban living and psychosis—an overview. Asian J Psychiatr. 2014;12:17-22. [DOI] [PubMed] [Google Scholar]
- 4.Vassos E, Pedersen CB, Murray RM, Collier DA, Lewis CM. Meta-analysis of the association of urbanicity with schizophrenia. Schizophr Bull. 2012;38(6):1118-1123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McGrath J, Scott J. Urban birth and risk of schizophrenia: a worrying example of epidemiology where the data are stronger than the hypotheses. Epidemiol Psichiatr Soc. 2006;15(4):243-246. [PubMed] [Google Scholar]
- 6.Kelly BD, O’Callaghan E, Waddington JL, et al. Schizophrenia and the city: a review of literature and prospective study of psychosis and urbanicity in Ireland. Schizophr Res. 2010;116(1):75-89. [DOI] [PubMed] [Google Scholar]
- 7.van Os J, Kenis G, Rutten BPF. The environment and schizophrenia. Nature. 2010;468(7321):203-212. [DOI] [PubMed] [Google Scholar]
- 8.Scott J, Chant D, Andrews G, McGrath J. Psychotic-like experiences in the general community: the correlates of CIDI psychosis screen items in an Australian sample. Psychol Med. 2006;36(2):231-238. [DOI] [PubMed] [Google Scholar]
- 9.Boonstra N, Sterk B, Wunderink L, Sytema S, De Haan L, Wiersma D. Association of treatment delay, migration and urbanicity in psychosis. Eur Psychiatry. 2012;27(7):500-505. [DOI] [PubMed] [Google Scholar]
- 10.Whiteford HA, Ferrari AJ, Degenhardt L, Feigin V, Vos T. The global burden of mental, neurological and substance use disorders: an analysis from the Global Burden of Disease Study 2010. PLoS One. 2015;10(2):e0116820. doi: 10.1371/journal.pone.0116820 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Lundberg P, Cantor-Graae E, Kabakyenga J, Rukundo G, Ostergren PO. Prevalence of delusional ideation in a district in southwestern Uganda. Schizophr Res. 2004;71(1):27-34. [DOI] [PubMed] [Google Scholar]
- 12.Lundberg P, Cantor-Graae E, Rukundo G, Ashaba S, Ostergren PO. Urbanicity of place of birth and symptoms of psychosis, depression and anxiety in Uganda. Br J Psychiatry. 2009;195(2):156-162. [DOI] [PubMed] [Google Scholar]
- 13.Gureje O, Olowosegun O, Adebayo K, Stein DJ. The prevalence and profile of non-affective psychosis in the Nigerian Survey of Mental Health and Wellbeing. World Psychiatry. 2010;9(1):50-55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Patel V, Simbine AP, Soares IC, Weiss HA, Wheeler E. Prevalence of severe mental and neurological disorders in Mozambique: a population-based survey. Lancet. 2007;370(9592):1055-1060. [DOI] [PubMed] [Google Scholar]
- 15.Mlambo K. Does mental health matter? commentary on the provision of mental health services in Mozambique. Int Psychiatry. 2012;9(2):36-38. [PMC free article] [PubMed] [Google Scholar]
- 16.Ganguli HC. Epidemiological findings on prevalence of mental disorders in India. Indian J Psychiatry. 2000;42(1):14-20. [PMC free article] [PubMed] [Google Scholar]
- 17.Thara R, Padmavati R, Srinivasan TN. Focus on psychiatry in India. Br J Psychiatry. 2004;184:366-373. [DOI] [PubMed] [Google Scholar]
- 18.Jiloha RC, Kukreti P. Caregivers as the fulcrum of care for mentally ill in the community: the urban rural divide among caregivers and care giving facilities. Indian J Soc Psychiatry. 2016;32:35-39. [Google Scholar]
- 19.World Health Organization. WHO World Health Survey. http://www.who.int/healthinfo/survey/en/. Updated February 11, 2016. Accessed December 8, 2017.
- 20.United Nations Department of Economic and Social Affairs. World Urbanization Prospects, the 2014 Revision . https://esa.un.org/unpd/wup/. Updated January 2, 2018. Accessed February 12, 2018.
- 21.Novak NL, Allender S, Scarborough P, West D. The development and validation of an urbanicity scale in a multi-country study. BMC Public Health. 2012;12:530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kessler RC, Ustün TB. The World Mental Health (WMH) Survey Initiative version of the World Health Organization (WHO) Composite International Diagnostic Interview (CIDI). Int J Methods Psychiatr Res. 2004;13(2):93-121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Cooper L, Peters L, Andrews G. Validity of the Composite International Diagnostic Interview (CIDI) psychosis module in a psychiatric setting. J Psychiatr Res. 1998;32(6):361-368. [DOI] [PubMed] [Google Scholar]
- 24.DeVylder JE, Koyanagi A, Unick J, Oh H, Nam B, Stickley A. Stress sensitivity and psychotic experiences in 39 low- and middle-income countries. Schizophr Bull. 2016;42(6):1353-1362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.StataCorp . Stata Statistical Software: Release 14. College Station, TX: StataCorp LP; 2015. [Google Scholar]
- 26.United Nations DESA/Population Division . Population pyramid 2010. https://esa.un.org/wpp/Excel-Data/population.htm. Updated January 2, 2018. Accessed December 8, 2017.
- 27.Higgins JP, Thompson SG. Quantifying heterogeneity in a meta-analysis. Stat Med. 2002;21(11):1539-1558. [DOI] [PubMed] [Google Scholar]
- 28.McGrath JJ, Saha S, Al-Hamzawi AO, et al. Age of onset and lifetime projected risk of psychotic experiences: cross-national data from the World Mental Health Survey. Schizophr Bull. 2016;42(4):933-941. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Thompson JL, Pogue-Geile MF, Grace AA. Developmental pathology, dopamine, and stress: a model for the age of onset of schizophrenia symptoms. Schizophr Bull. 2004;30(4):875-900. [DOI] [PubMed] [Google Scholar]
- 30.Rabe-Hesketh S, Skrondal A. Multilevel modelling of complex survey data. J R Stat Soc. 2006;169:805-827. [Google Scholar]
- 31.Koyanagi A, Stickley A, Haro JM. Psychotic symptoms and smoking in 44 countries. Acta Psychiatr Scand. 2016;133(6):497-505. [DOI] [PubMed] [Google Scholar]
- 32.Chan KY, Zhao FF, Meng S, et al. Urbanization and the prevalence of schizophrenia in China between 1990 and 2010. World Psychiatry. 2015;14(2):251-252. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Avasthi A. Preserve and strengthen family to promote mental health. Indian J Psychiatry. 2010;52(2):113-126. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Richardson L, Hameed Y, Perez J, Jones PB, Kirkbride JB. Association of environment with the risk of developing psychotic disorders in rural populations: findings from the social epidemiology of psychoses in East Anglia study. JAMA. 2018;75(1):75-83. doi: 10.1001/jamapsychiatry.2017.3582 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Card D. How immigration affects US cities. In: Inman RP, ed. Making Cities Work: Prospects and Policies for Urban America. Princeton, NJ: Princeton University Press; 2009:158-200. [Google Scholar]
- 36.World Bank. Net migration. https://data.worldbank.org/indicator/SM.POP.NETM. Accessed March 11, 2017.
- 37.Schofield P, Ashworth M, Jones R. Ethnic isolation and psychosis: re-examining the ethnic density effect. Psychol Med. 2011;41(6):1263-1269. [DOI] [PubMed] [Google Scholar]
- 38.Das-Munshi J, Bécares L, Boydell JE, et al. Ethnic density as a buffer for psychotic experiences: findings from a national survey (EMPIRIC). Br J Psychiatry. 2012;201(4):282-290. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Siriwardhana C, Stewart R. Forced migration and mental health: prolonged internal displacement, return migration and resilience. Int Health. 2013;5(1):19-23. [DOI] [PubMed] [Google Scholar]
- 40.UN Refugee Agency . Mid-year trends 2016. http://www.unhcr.org/statistics/unhcrstats/58aa8f247/mid-year-trends-june-2016.html. 2016. Accessed January 17, 2018.
- 41.Anderson KK, Cheng J, Susser E, McKenzie KJ, Kurdyak P. Incidence of psychotic disorders among first-generation immigrants and refugees in Ontario. CMAJ. 2015;187(9):E279-E286. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Adorjan K, Odenwald M, Widmann M, et al. Khat use and occurrence of psychotic symptoms in the general male population in Southwestern Ethiopia: evidence for sensitization by traumatic experiences. World Psychiatry. 2017;16(3):323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Grech A, van Os J; GROUP Investigators . Evidence that the urban environment moderates the level of familial clustering of positive psychotic symptoms. Schizophr Bull. 2017;43(2):325-331. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sariaslan A, Fazel S, D’Onofrio BM, et al. Schizophrenia and subsequent neighborhood deprivation: revisiting the social drift hypothesis using population, twin and molecular genetic data. Transl Psychiatry. 2016;6:e796. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Sariaslan A, Larsson H, D’Onofrio B, Långström N, Fazel S, Lichtenstein P. Does population density and neighborhood deprivation predict schizophrenia? a nationwide Swedish family-based study of 2.4 million individuals. Schizophr Bull. 2015;41(2):494-502. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Paksarian D, Trabjerg BB, Merikangas KR, et al. The role of genetic liability in the association of urbanicity at birth and during upbringing with schizophrenia in Denmark. Psychol Med. 2018;48(2):305-314. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Steinheuser V, Ackermann K, Schönfeld P, Schwabe L. Stress and the city: impact of urban upbringing on the (re)activity of the hypothalamus-pituitary-adrenal axis. Psychosom Med. 2014;76(9):678-685. [DOI] [PubMed] [Google Scholar]
- 48.Hernández AV, Pasupuleti V, Deshpande A, Bernabé-Ortiz A, Miranda JJ. Effect of rural-to-urban within-country migration on cardiovascular risk factors in low- and middle-income countries: a systematic review. Heart. 2012;98(3):185-194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Torrey EF, Yolken RH. The urban risk and migration risk factors for schizophrenia: are cats the answer? Schizophr Res. 2014;159(2-3):299-302. [DOI] [PubMed] [Google Scholar]
- 50.Gordon SB, Bruce NG, Grigg J, et al. Respiratory risks from household air pollution in low and middle income countries. Lancet Respir Med. 2014;2(10):823-860. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Belvederi Murri M, Respino M, Masotti M, et al. Vitamin D and psychosis: mini meta-analysis. Schizophr Res. 2013;150(1):235-239. [DOI] [PubMed] [Google Scholar]
- 52.Jongsma HE, Gayer-Anderson C, Lasalvia A, et al. ; European Network of National Schizophrenia Networks Studying Gene-Environment Interactions Work Package 2 (EU-GEI WP2) Group . Treated incidence of psychotic disorders in the multinational EU-GEI study. JAMA Psychiatry. 2018;75(1):36-46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 53.Moreno C, Nuevo R, Chatterji S, Verdes E, Arango C, Ayuso-Mateos JL. Psychotic symptoms are associated with physical health problems independently of a mental disorder diagnosis: results from the WHO World Health Survey. World Psychiatry. 2013;12(3):251-257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Nuevo R, Chatterji S, Verdes E, Naidoo N, Arango C, Ayuso-Mateos JL. The continuum of psychotic symptoms in the general population: a cross-national study. Schizophr Bull. 2012;38(3):475-485. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.McGrath J, Saha S, Chant D, Welham J. Schizophrenia: a concise overview of incidence, prevalence, and mortality. Epidemiol Rev. 2008;30:67-76. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. WHS Countries That Were Excluded From Data Analysis
eTable 2. Included Study Sites and Ethical Approving Bodies
eTable 3. Comparison Between WHS- and World Bank–Defined Urbanicity (2003 Data) for Each Country Included in the Study Sample
eTable 4. Indicators of Urbanicity by WHS-Defined Rural and Urban Setting in Low-Income Countries
eTable 5. Indicators of Urbanicity by WHS-Defined Rural and Urban Setting in Middle-Income Countries
eFigure 1. Countrywise Association Between Urban Residence (Exposure) and Psychotic Experience (Outcome) Among Individuals Aged 18-29 Years
eFigure 2. Countrywise Association Between Urban Residence (Exposure) and Psychotic Experience (Outcome) Among Individuals 30 or Older