Abstract
This study evaluates the use of a comprehensive screening protocol for prostate, breast, colorectal, and pancreatic cancer and skin malignant abnormalities in male BRCA carriers.
Men with germline mutations in BRCA1 and BRCA2 genes have a higher risk of developing malignant abnormalities of the prostate, pancreas, breast, colon, and melanoma.1,2,3 Moreover, germline BRCA mutations are associated with higher stage, grade, and poor survival rates in patients with prostate cancer.4
In contrast to protocols for women, current screening protocols for men who are BRCA carriers are based on low-level evidence.5 Previous studies evaluating cancer screening in these men focused on prostate cancer rather than all BRCA-associated malignant diseases.6
In the current study, we report the use of a predefined comprehensive screening protocol for evaluating male BRCA carriers enrolled to a dedicated clinic.
Methods
Between February 2014 and February 2017 we evaluated 196 BRCA carriers. After obtaining approval from the institutional review board at Rabin Medical Center and written informed consent, we screened patients 40 years or older for prostate, breast, colorectal, pancreatic, and skin malignant abnormalities using a predefined protocol (Table).
Table. Screening Protocol for Male BRCA Mutation Carriers and Number of Previous and New Malignant Abnormalities Identified in a Cohort of 196 Mena.
| Organ | Screening Test | Frequency | Previous Malignant Abnormalities, No. | New Malignant Abnormalities, No. |
|---|---|---|---|---|
| Prostate | PSA | 1 Year | 4 | 9 |
| DRE | 1 Year | |||
| MRI | Performed at initial screening and before prostate biopsy in men aged 40 to 70 years | |||
| Breast | Clinical breast examination | 1 Year | 2 | 0 |
| Mammogram | Initial mammogram at age 40 years; frequency of subsequent testing determined by initial findings and patient age | |||
| Pancreas | CA-19-9 | 1 Year | 2 | 2 |
| Abdominal ultrasound | 1 Year | |||
| Colorectal | CEA | 1 Year | 2 | 0 |
| Colonoscopy | Every 5 years; screening is initiated at 45 years | |||
| Skin | Dermatologist examination | 1 Year; screening is initiated on enrollment disregarding patient age | 11 | 1 |
Abbreviations: DRE, digital rectal examination; MRI, magnetic resonance imaging; PSA, prostate-specific antigen.
The screening protocol for prostate and breast cancer is based on the National Comprehensive Cancer Network Genetic/Familial High-Risk Assessment: Breast and Ovarian (version 1.2014) with the addition of prostatic MRI. Screening for pancreatic, colorectal and skin cancer were based on specific society recommendations with the aim of minimizing the use of radiation and invasive studies; screening was initiated at age 40 years, except for where noted otherwise.
We report patient characteristics and prevalence of tumors identified prior to enrollment and initial screening. Standardized incidence ratios were calculated to compare cancer incidence in our cohort with the age-adjusted cancer incidence in the Israeli Jewish male population as reported in the Israeli-National Cancer Registry.
Results
A total of 117 (60%) BRCA1 and 79 (40%) BRCA2 carriers were included. Median age was 49 (interquartile range [IQR], 41-63) years. Common mutations were 185delAG in BRCA1 (87 of 117 [74%]) and 6174delIT in BRCA2 (67 of 79 [85%]).
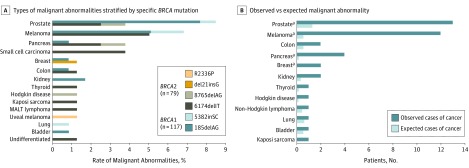
Thirty-four (17%) patients were diagnosed with 46 malignant abnormalities; 13 (28%) were identified during screening. Median age at first cancer diagnosis was 54 (IQR, 44-63) years. Seven patients had multiple malignant abnormalities, with a median of 3 per patient (range, 2-4). The most common malignant abnormality was prostatic adenocarcinoma identified in 10 (8.6%) BRCA1 carriers , and 3 (3.8%) BRCA2 carriers (Figure, A). Initial screening identified malignant abnormalities of the prostate (n = 9), pancreas (n = 2), and skin (n = 2), all treated with a curative intent.
Figure. Type and Rate of Malignant Abnormalities Identified in the Male BRCA Clinic.
A, Type and rate of malignant abnormalities stratified by mutation type in a prospectively screened cohort of male BRCA1 (n = 117, blue bars) and BRCA2 (n = 79, dark gray bars) mutation carriers enrolled to a male BRCA clinic. B, Observed and expected cases of malignant abnormalities in the study cohort. Expected number of malignant abnormalities were calculated by multiplying the number of patients entering a specific age interval with the corresponding age-adjusted cancer incidence rates for the general Israeli Jewish male population between 2003 and 2013 retrieved from the Israeli National Cancer Registry.
aP≤.003
Compared with the Jewish-Israeli male population, men with BRCA mutations had a significant increase in overall incidence of malignant disease (standardized incidence ratio, 8; 95% CI, 5.74-10.85; P < .001). BRCA mutations were associated with an elevated incidence of prostate, melanoma, pancreas, and breast cancers; however, the incidence of colon cancer was not higher (Figure, B).
Discussion
Current recommendations for the screening of BRCA-positive men include annual clinical breast examination starting at age 35 and yearly prostate cancer screening in BRCA2 carriers starting at age 45.5 We devised a screening protocol for male BRCA mutation carriers based on malignant abnormalities previously associated with this group of patients. Twenty-eight percent of malignant abnormalities were identified during screening, all of which were found at early stage and amenable to curative treatment.
In this study, overall cancer incidence among BRCA carriers was higher than that of the general population. Detection rates of prostate cancer were similar to those in the IMPACT study.6 The rate of prostate cancer among BRCA1 carriers was more than twice as high (8.6% vs 3.8%), likely owing to the high prevalence of the Jewish founder mutation 185delAG in this population. Melanoma was the second most common malignant abnormality, related to the high incidence of melanoma in the Israeli population.
We used abdominal ultrasound and CA19-9 testing to screen for pancreatic cancer and identified 2 cases of malignant disease, both received definitive local surgical treatment, emphasizing the profound clinical impact screening may have on patient outcome.
Limitations
Limitations of the study include initial screening ascertainment bias, and lack of control group to establish the benefit of screening.
Conclusion
Our initial findings suggest that in addition to screening for prostate and breast cancer, as recommended in current guidelines, there may be a role for screening for pancreatic cancer and melanoma, whereas screening for colon cancer may not be justified. Further long-term studies are needed to determine the effect of screening on mortality.
References
- 1.Ford D, Easton DF, Bishop DT, Narod SA, Goldgar DE; Breast Cancer Linkage Consortium . Risks of cancer in BRCA1-mutation carriers. Lancet. 1994;343(8899):692-695. [DOI] [PubMed] [Google Scholar]
- 2.Breast Cancer Linkage C; Breast Cancer Linkage Consortium . Cancer risks in BRCA2 mutation carriers. J Natl Cancer Inst. 1999;91(15):1310-1316. [DOI] [PubMed] [Google Scholar]
- 3.Liede A, Karlan BY, Narod SA. Cancer risks for male carriers of germline mutations in BRCA1 or BRCA2: a review of the literature. J Clin Oncol. 2004;22(4):735-742. [DOI] [PubMed] [Google Scholar]
- 4.Castro E, Goh C, Olmos D, et al. . Germline BRCA mutations are associated with higher risk of nodal involvement, distant metastasis, and poor survival outcomes in prostate cancer. J Clin Oncol. 2013;31(14):1748-1757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.National Comprehensive Cancer Network Genetic/Familial High-Risk Assessment: Breast and Ovarian (Version 1.2017). https://www.nccn.org/professionals/physician_gls/pdf/genetics_screening.pdf.
- 6.Bancroft EK, Page EC, Castro E, et al. ; IMPACT Collaborators . Targeted prostate cancer screening in BRCA1 and BRCA2 mutation carriers: results from the initial screening round of the IMPACT study. Eur Urol. 2014;66(3):489-499. [DOI] [PMC free article] [PubMed] [Google Scholar]