Abstract
Importance
Among smokers with head and neck squamous cell carcinoma (HNSCC), there is ample evidence regarding the benefits of smoking cessation prior to treatment. Prior data indicates that increased attempts at cessation result in higher likelihood of cessation after diagnosis but the prediagnostic patterns of smoking cessation attempts among those smokers developing HNSCC has not been characterized. Data of this kind may direct cessation efforts toward increased efficacy.
Objective
To determine the frequency and character of tobacco cessation attempts and symptoms experienced prior to development of HNSCC, as well as to determine the correlation of these symptoms with number of cessation attempts and maximum quit days.
Design, Setting, and Participants
Cross-sectional study including 123 active smokers with HNSCC recruited from a tertiary medical center at an academic institution from February 2014 to May 2017.
Exposures
All included patients were active cigarette smokers prior to developing HNSCC.
Main Outcomes and Measures
Patients provided data indicating intensity of smoking, duration, number of cessation attempts, maximum number of days during which they successfully ceased smoking, and symptoms during cessation attempts. Principal component analysis was used to identify clustering of symptoms.
Results
In total, 123 patients were identified (97 men, 23 women, and 3 unspecified) from February 2014 to May 2017 as active smokers (mean [SD] age, 59.4 [9.0] years; median [interquartile range] age, 58.5 [54.8-66.0] years); patients had oral (n = 39 [32%]), oropharyngeal (n = 44 [36%]), laryngeal (n = 32 [26%]) or hypopharyngeal (n = 7 [6%]) tumors. Overall, 108 patients (88%) had made at least 1 prior attempt at cessation, and the mean number of lifetime cessation attempts was 6.6. Symptoms of cravings, restlessness, irritability, and anxiety were reported most frequently. Symptoms were clustered into 2 component groups: component group 1 (C1; increased appetite, cravings, depression) and component group 2 (C2; restlessness, irritability, insomnia, anxiety, and difficulty concentrating). Component group 2 correlated with quit attempts (Spearman correlation, 0.268 [95% CI, 0.07 to 0.45]), and C1 and C2 were not correlated with maximum quit days. Cessation attempts and maximum quit days positively correlated with each other.
Conclusions and Relevance
Our analysis shows that symptoms during cessation attempts tend to cluster and that most patients made 1 or more cessation attempts. Many patients successfully ceased before restarting. Our data suggest that patients experiencing C2 symptoms make more quit attempts; C1 symptoms may be more difficult to overcome because they are associated with fewer quit attempts. Future work will address whether amelioration of these symptoms may help smoking cessation among smokers with HNSCC.
This cross-sectional study of smokers with head and neck squamous cell carcinoma (HNSCC) examines tobacco cessation attempts and symptoms experienced prior to development of HNSCC, as well as the correlation of these symptoms with number of cessation attempts and maximum quit days.
Key Points
Question
At what rate is smoking cessation attempted by those who develop head and neck squamous cell carcinoma (HNSCC) and what symptoms are experienced?
Findings
In this cross-sectional study of 123 smokers who developed HNSCC, most patients (108) had attempted to quit smoking before developing the disease. During their quit attempts, patients developed symptoms that clustered into 2 groups; C1 (increased appetite, cravings, and depression) was associated with fewer smoking cessation attempts than C2 (restlessness, irritability, insomnia, anxiety, and difficulty concentrating).
Meaning
Our findings suggest that symptoms in C1 (increased appetite, cravings, and depression) might be more difficult for smokers to overcome in their smoking cessation attempts.
Introduction
Head and neck squamous cell carcinoma (HNSCC) represents a group of tumors that is strongly associated with tobacco use. While human papillomavirus has recently been identified as a frequent cause of oropharyngeal cancers, most head and neck cancers in the oral cavity, larynx, hypopharynx (any many in the oropharynx) are associated with tobacco use.1 While many smokers cease their tobacco use following a cancer diagnosis, complete tobacco cessation is far from given among patients with cancer, including those with HNSCC.2,3,4 For example, when considering smokers with HNSCC, 54% to 69% demonstrate cessation for some period around the time of diagnosis, while the remainder continue smoking.5,6,7 When considering smokers developing lung and/or head and neck cancer, a recent systematic review revealed that, while there is variability between studies, 9% to 55% of those developing these cancers will persistently smoke after diagnosis or relapse after temporarily quitting. Thus, patients who continue to smoke and those that relapse make up a significant fraction of smokers with HNSCC.
Naturally, there is great interest in effective measures for smoking cessation among patients with head and neck cancers. One of the most important reasons for this is that those who continue to smoke during and after treatment for head and neck cancer experience worsened outcomes with regard to cancer control and overall survival compared with those who quit prior to treatment.8,9,10,11 Prior work has shown that overall survival decreases by more than half among those who continue to smoke during and after treatment for HNSCC. One component of the poorer outcomes seen in those patients who continue to smoke after cancer treatment pertains to the development of second primary tumors. Patients with HNSCC who continue to smoke develop second primary tumors at significantly higher rates than those who quit.12 Additional work has shown that the relative risk of mortality among those who quit is 0.6 compared with those who continue to smoke.13
Prior studies7,14 examining patients with cancer found that smokers were more likely to successfully quit after diagnosis if they reported more cessation attempts in the prior year. While it is possible that many smokers who ultimately develop HNSCC have made attempts at tobacco cessation, patterns of prediagnostic tobacco cessation attempts are poorly studied to date. Furthermore, the symptoms experienced by patients with HNSCC when attempting cessation have not been previously studied. A better understanding of prior patterns and effects of cessation exhibited in this population has the potential to inform more appropriate strategies for assisting patients with HNSCC to quit smoking. This is especially needed given the high number of smokers who continue to smoke after a diagnosis of HNSCC.7 To better understand this group of smokers, we examined a cohort of cigarette smokers presenting with HNSCC to determine the frequency with which they attempted to quit over their lifetime, the symptoms they experienced during quit attempts, and which symptoms were most associated with their attempts at cessation.
Methods
Study Patients
This study was approved by the University of Minnesota institutional review board. Patients with HNSCC were identified and enrolled following informed consent during outpatient visits to the University of Minnesota Otolaryngology–Head and Neck Surgery Clinic with a new diagnosis of squamous cell carcinoma of the upper aerodigestive tract. This included tumors of the oral cavity, oropharynx, larynx, and hypopharynx. In some cases, cancers were first identified in our clinic, whereas in others, cancers were diagnosed at outside institutions and referred to our clinic for definitive management. Inclusion criteria included self-report of current daily smoking and having smoked at least 5 cigarettes per day for at least 5 years. A total of 123 smokers were eligible and enrolled in the study from February 2014 to May 2017.
Questionnaire
All patients completed questionnaires regarding their lifetime tobacco and alcohol use. The questionnaire is based on the Minnesota Nicotine Withdrawal Scale (MNWS).15 Data collected included cigarettes per day, duration of use, alcoholic drinks per day, alcoholic frequency, and tumor-related variables such as subsite and stage. In addition, patients answered questions regarding their prior smoking cessation attempts, length of quit periods, and symptoms experienced during prior attempts at cessation. Patients were asked if they experienced 1 or more of the following, which comprised 8-symptom variables for analysis: restlessness, cravings, irritability, insomnia, anxiety, difficulty concentrating, increased appetite, and depression. All data were stored using double data entry on a secure server at the University of Minnesota.
Statistical Analysis
Summary statistics were calculated for demographic variables and symptom analysis. Spearman correlations were performed to analyze the relationships between symptoms and 2 main variables of number of quit attempts and maximum quit days; 95% CIs were calculated by bootstrap in R version 3.4.0 for Windows (R Foundation).
Principal Components Analysis (PCA) was used as a data reduction method to find underlying patterns behind a set of variables. The PCA algorithm creates a set of artificial variables known as “components” from a weighted combination of the original variables in such a way that the components capture the most amount of the original variation in the data. The weights, or “loadings,” of the original variables can be thought of as their importance to that component. The main variables in a component can be thought as occurring together, or measuring a similar “construct.”16 We used the “scree plot” method to select the appropriate number of components. In this analysis, a Varimax rotated PCA (using the Psych package in R) was used for the 8 symptom variables to determine which symptoms are typically experienced together (ie, are present in the same component). As the symptom responses were binary (yes or no), polychoric correlations were used in the PCA. The weights were rotated through Varimax rotation to aid in the interpretability of the components. All analyses were conducted in R.
Results
Demographics
In total, 123 patients (smokers with HNSCC) were enrolled in the study. Demographic data are summarized in Table 1. The mean age of enrolled cases was 59 years, 97 patients (79%) were men, and 23 (21%) were women (3 patients did not disclose sex). Patients presented with squamous cell cancers of oral cavity (n = 39 [32%]), oropharynx (n = 44 [36%]), larynx (n = 32 [26%]), and hypopharynx (n = 7 [6%]).
Table 1. Demographic and Response Variable Summary.
| Demographic and Response Variables | Mean (SD) | Median (IQR) |
|---|---|---|
| Age, y | 59.4 (9.0) | 58.5 (54.8-66.0) |
| Sex, No. (%) | ||
| Male | 97 (78.9) | NA |
| Female | 23 (18.7) | NA |
| Not specified | 3 (2.0) | NA |
| Quit attempts, No. | 6.6 (10.0) | 4.0 (2.0-6.0) |
| Max quit days | 213.9 (524.5) | 25.5 (4.0-172.5) |
Abbreviation: NA, not applicable.
Tobacco Cessation
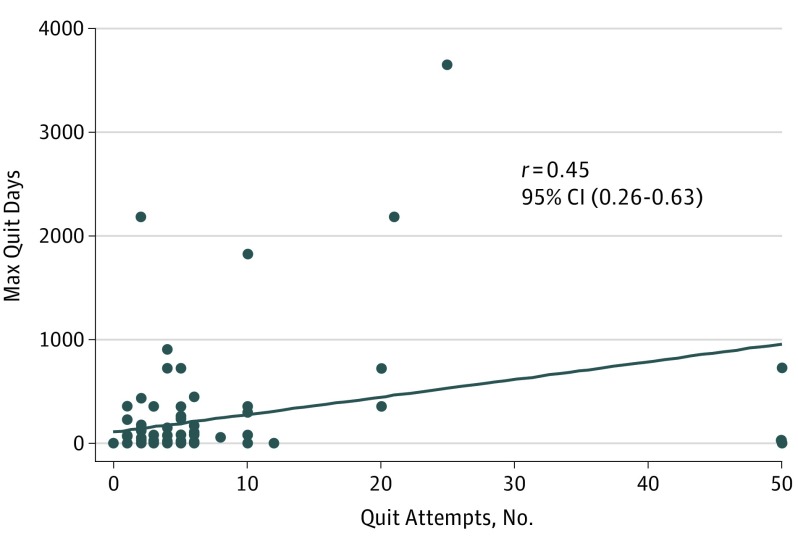
Patients smoked cigarettes at a mean rate of 15.6 cigarettes per day, and the mean duration of tobacco use was 29.1 years. The mean number of quit attempts prior to HNSCC diagnosis was 6.6, and the range was 0 to 50: 48 patients reported 0 to 3 attempts; 39, 4 to 9 attempts; and 22 cases, more than 10 attempts. Of those reporting 0 to 3 prior quit attempts (n = 48), 15 had no prior cessation attempts. Patients were queried regarding the maximum number of days they had previously successfully quit smoking (although all were smoking at time of enrollment). Of those who had successfully quit previously, the median (interquartile range [IQR]) duration was 25.5 (4.0-172.5) days. Fourteen patients were able to quit for 8 to 29 days; 22, 1 to 3 months; and 19, 4 to 12 months. Twelve patients quit for greater than 1 year, and 1 patient quit for 10 years before resuming smoking. Eighty-seven patients achieved at least 1 day of cessation. The relationship between number of cessation attempts and maximum quit days was analyzed via Spearman correlation. This revealed a strong positive association between these 2 variables (r = 0.45; 95% CI, 0.26-0.63) (Figure 1).
Figure 1. Relationship Between Quit Attempts and Maximum Quit Days.
Spearman correlation between number of cessation attempts and maximum number of quit days.
Symptom Components
Patients were queried regarding 8 symptoms experienced during cessation attempts (Table 2). The symptom most commonly experienced was cravings, followed by restlessness, irritability, and anxiety. We examined the correlation between the symptoms experienced and the following variables: (1) total number of quit attempts, and (2) maximum number of quit days (Table 3).
Table 2. Prevalence of Symptoms Experienced by Subjects During Cessation Attempts.
| Symptoms (n = 123) | No. (%) | ||
|---|---|---|---|
| Yes | No | NA | |
| Cravings | 103 (83.7) | 9 (7.3) | 11 (8.9) |
| Restlessness | 64 (52.0) | 43 (35.0) | 16 (13.0) |
| Anxiety | 58 (47.2) | 50 (40.7) | 15 (12.2) |
| Irritability | 58 (47.2) | 50 (40.7) | 15 (12.2) |
| Difficulty concentrating | 30 (24.4) | 77 (62.6) | 16 (13.0) |
| Depression | 25 (20.3) | 82 (66.7) | 16 (13.0) |
| Increased appetite | 21 (17.1) | 84 (68.3) | 18 (14.6) |
| Insomnia | 14 (11.4) | 90 (73.2) | 19 (15.4) |
Abbreviation: NA, not applicable.
Table 3. Spearman Coefficients for Correlation Between C1 and C2.
| Variable | rs (95% CI) |
|---|---|
| Quit Attempts, No. (n = 98) | |
| C1a total | 0.137 (−0.07 to 0.33) |
| C2b total | 0.268 (0.06 to 0.45) |
| Total symptoms | 0.209 (0.00 to 0.42) |
| Maximum Quit Days (n = 89) | |
| C1a total | −0.047 (−0.26 to 0.17) |
| C2b total | 0.075 (−0.17 to 0.30) |
| Total symptoms | 0.024 (−0.22 to 0.24) |
Component group 1 (C1) included increased appetite, cravings, and depression.
Component group 2 (C2) included restlessness, irritability, insomnia, anxiety, and difficulty concentrating.
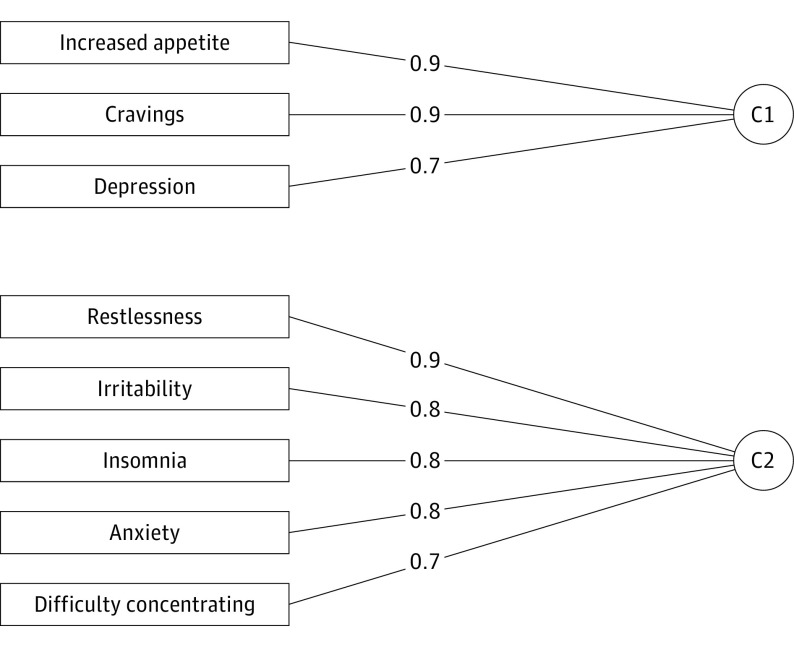
Principal Components Analysis revealed that symptoms clustered into 2 components. The symptom components, with related weights for each symptom, are depicted in Figure 2. The magnitude of the weight indicates how strongly the symptom is related to its component, with 1 being the strongest. Because all of the weights are positive, all of the symptoms are positively related to their corresponding component. The first component group (C1) of symptoms included cravings, depression, and increased appetite. The second component group (C2) included restlessness, irritability, insomnia, anxiety, and difficulty concentrating. Only C2 was significantly correlated with number of quit attempts although the Spearman correlation was only modestly positive at 0.268 (95% CI, 0.07 to 0.45). There was also a significant relationship between the total number of symptoms experienced and the number of quit attempts made (r = 0.209; 95% CI, −0.01 to 0.41). When examining individual reported symptoms, only irritability (r = 0.198; 95% CI, 0.01 to 0.38), feeling depressed (r = 0.206; 95% CI, −0.01 to 0.41), and increased appetite (r = 0.207; 95% CI, 0.02 to 0.37) were significantly correlated with number of quit attempts. None of the symptoms were significantly correlated with maximum number of quit days. The latter analysis was performed without use of the PCA analysis, but rather studied the correlation of the total symptoms experienced with the outcome variables.
Figure 2. Clustering of Symptoms Experienced Together.
The principal component analysis of symptoms in patients resulted in clustering of symptoms most commonly experienced together. These were divided into component group 1 (C1), which included increased appetite, cravings, and depression, and component group 2 (C2), which included restlessness, irritability, anxiety, and difficulty concentrating. The coefficients represent the Varimax rotated weights.
Discussion
From the perspective of clinicians, tobacco cessation is a priority for every patient who smokes. At the time of a cancer diagnosis, many patients are able to find the strength and motivation to quit smoking while others continue to smoke during and after treatment. The ability to quit prior to cancer treatment has significant repercussions, with successful quitters achieving improved survival outcomes.8,9 The latter finding has been confirmed in a systematic review as well.11 Furthermore, a study of over 5600 patients with head and neck cancer in Ireland10 showed that current smokers had a significantly raised rate of death from cancer, and the use of radiotherapy or chemotherapy did not modify the effect of smoking. Thus, smoking status at diagnosis is an important factor in the outcomes of patients diagnosed with HNSCC. Given prior data indicating a greater likelihood of smoking cessation among patients with cancer who have made prior attempts, we examined a cohort of smokers diagnosed with HNSCC to better understand their history of tobacco cessation attempts. Through analysis of demographic and questionnaire data, we were able to analyze tobacco use history, prior attempts to quit, and levels of success previously achieved through maximum prior quit period. In addition, we analyzed a series of symptoms commonly experienced during cessation attempts to better identify which symptoms occurred together most often and which symptoms were most commonly reported in this group of smokers.
First, our results suggest that smokers who develop HNSCC generally have a history of multiple prior attempts at cessation. Only 14% of cases reported never having made an attempt to quit smoking in their lifetime. Furthermore, 57% reported making 4 or more attempts. Thus, while all of the patients in this study were smoking at the time of their HNSCC diagnosis, it was often after multiple unsuccessful efforts or short-lived periods of cessation. This is similar to figures in the general US population where in 2013, approximately two-thirds of all adult smokers reported attempting to quit in the past year.17 For the large proportion of patients who did attempt cessation, many were able to quit smoking for several weeks, months, or even years. Eighty four percent of patients achieved some duration of abstinence (1 day or greater), and it is notable that many were able to quit for one month or more. Despite this limited success, all patients eventually went back to smoking and continued until their diagnosis of HNSCC. The obstacles to tobacco cessation among cancer patients have been previously studied to some degree. Schnoll et al18 studied a group of 111 patients with cancer entering a smoking cessation program. They found that this group of patients most commonly had head and neck, rather than lung, cancer, and although they were highly addicted to nicotine, they were contemplating a change in tobacco use. Furthermore, most of these patients attempted to quit without formal treatment, but those who did seek treatment methods most commonly used the nicotine patch, nicotine, or bupropion. The authors identified the importance of self-motivation and self-efficacy in achieving successful abstinence such that smoking cessation treatments for patients with cancer should include pharmacotherapy, relapse prevention, and counseling.19 The social environment surrounding a smoker is also important in determining a smoker’s likelihood of cessation. A prior study of 295 smokers with HNSCC found that those consuming less alcohol, shorter lifetime smoking duration, those without spousal smoking, and those having few friends who smoked were more likely to quit after diagnosis.20 This data suggests that smoking cessation efforts must address the smoker while also paying close attention to factors in the smoker’s environment, which may make abstinence more difficult.
Existing literature suggests that there is a linear relationship between duration of cessation and likelihood of remaining abstinent.21 In the general population, only about 12% of those who quit for less than 1 month remain abstinent. This figure increases to 25% for those who are able to quit between 1 and 3 months and to greater than 50% for those who quit for 3 months or more. Our study population is not readily comparable to the general public because of our selection criteria mandating enrollment of active smokers. Still, it does illustrate the difference in quit rates between our study population and smokers in general. With regard to the previously reported association between number of quit attempts and later success in abstinence,7 our population is not easy to compare because, again, we selected for those who were actively smoking. Nevertheless, the strong correlation between number of quit attempts and maximum quit days in our study suggests that those who try to quit more often did have greater success in achieving tobacco-free periods.
Analysis of the symptoms experienced during cessation attempts revealed interesting patterns. The symptom of cravings for additional cigarettes was the most commonly reported symptom overall. Following cravings, the most commonly experienced symptoms were restlessness, irritability, and anxiety. For purposes of comparison, depression and anxiety have been previously reported to be present in nearly 19% of unsuccessful quitters,22 and that finding is nearly identical to the percentage of patients reporting depression during quit attempts in our sample (20%). Furthermore, it seems likely that depression and depressive episodes display a complex interaction with smoking. A study of over 73 000 respondents from the National Survey on Drug Use and Health revealed that persons with a self-reported lifetime history of depression, anxiety, anxiety with depression, or major depressive episode are more likely to be current smokers, smoke with higher intensity and frequency, have more dependence, and have lower success at quitting compared with those persons without a similar depressive history.23 Thus, it may be that depression is a result of smoking or unsuccessful quitting in some cases, while in other persons it may be the cause of persistent smoking or initiation in the first place.
The PCA allowed us to identify which symptoms occurred together most commonly. The first component of symptoms (ie, C1) included increased appetite, cravings, and depression. These symptoms were strongly correlated with each other and thus tended to occur in the same patients. The second component (ie, C2) was made up of restlessness, irritability, insomnia, anxiety, and difficulty concentrating. There is scant existing literature regarding the “clustering” of symptoms among smokers during cessation, but prior work using the MNWS has confirmed that symptoms tend to coalesce as a syndrome over time. As a result, although we have little ability to compare the PCA in this study with similar work performed in the past, there is prior evidence of symptom clustering as seen in our study. This finding informs efforts at addressing obstacles to tobacco cessation in smokers with HNSCC. For example, preexisting knowledge of C2 symptoms might allow clinicians to preemptively address depression in smokers who report significant problems with cravings. Similarly, smokers reporting some of the symptoms in C1 might be treated with a short course of antianxiety medications to address their anticipated symptom complex and assist their cessation attempt.
In addition to understanding which symptoms occurred together most commonly, we examined the relationship between symptoms and cessation-related variables. Each component was studied for correlation with the number of quit attempts and the maximum quit days reported. This analysis suggested that C2, but not C1, symptoms were positively correlated with the number of quit attempts reported. Also, C2 did not show a significant correlation with maximum number of quit days. In contrast, C1 symptoms were not correlated with quit attempts or maximum quit days. One possible interpretation of this result is that C1 symptoms were more bothersome to smokers trying to quit such that experiencing these symptoms made users less likely to achieve longer periods of abstinence. The same reasoning would suggest that C2 symptoms were more tolerable such that the users experiencing them were more likely to make additional quit attempts or that failing multiple attempts to quit leads to depression. Alternatively, this data could be interpreted to indicate that C2 symptoms were more difficult to overcome and thus resulted in a high number of unsuccessful attempts. Examining the correlation of all symptoms together with both number of quit attempts and maximum quit days shows significant correlation only with number of quit attempts. However, given the finding that C2 is correlated with number of quit attempts, it is safe to assume that the weight of these C2 symptoms is the main driver of this statistical finding. To more rigorously address the relationship between specific symptoms and their relationship to a smoker’s likelihood to make additional quit attempts and/or attain longer periods of abstinence, a prospective study would ideally be performed. Still, it is a step forward to begin to understand the relationship between symptoms experienced during smoking cessation and the level of success achieved in those who develop HNSCC.
Limitations
The main limitation of our study relates to the self-reporting of data that was analyzed. It is well established that self-report may be subject to error owing to memory lapse or, in the case of smokers with a cancer diagnosis, shame or embarrassment may lead smokers to report inaccurately. Still, most of the data regarding questionnaire falsification that is presumably owing to shame relates to questions of how much and/or how long one smoked.24 In contrast, our study was focused on questions pertaining to past attempts at cessation and the symptoms experienced during those symptoms. While inaccurate self-report is still possible in our study, we submit that it may be less pervasive in a study of this type. Another limitation is that the scale used to identify patient symptoms (ie, MNWS) does not include severity of symptoms. Therefore, those with “mild” or “severe” symptoms are treated equally in our analysis.
Conclusions
We have examined the experience of smokers attempting cessation prior to developing HNSCC. We found that most patients had made at least 1 attempt to quit smoking in their lifetime, and many had made multiple attempts. In addition, a significant portion of patients had achieved cessation for 1 month or more before ultimately returning to smoke again. Furthermore, we found that cravings, followed by restlessness, irritability, and anxiety, were the most commonly reported symptoms during cessation attempts in this group. Lastly, from our correlation analysis, we may infer and hypothesize that symptoms in C1 were more difficult to overcome such that smokers experiencing them were less likely to have greater quit attempts and longer durations of abstinence. The new hypothesis generated by our data will be a focus of future study.
References
- 1.Marur S, D’Souza G, Westra WH, Forastiere AA. HPV-associated head and neck cancer: a virus-related cancer epidemic. Lancet Oncol. 2010;11(8):781-789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Blanchard CM, Denniston MM, Baker F, et al. Do adults change their lifestyle behaviors after a cancer diagnosis? Am J Health Behav. 2003;27(3):246-256. [DOI] [PubMed] [Google Scholar]
- 3.Gritz ER, Nisenbaum R, Elashoff RE, Holmes EC. Smoking behavior following diagnosis in patients with stage I non-small cell lung cancer. Cancer Causes Control. 1991;2(2):105-112. [DOI] [PubMed] [Google Scholar]
- 4.Tao L, Wang R, Gao YT, Yuan JM. Impact of postdiagnosis smoking on long-term survival of cancer patients: the Shanghai cohort study. Cancer Epidemiol Biomarkers Prev. 2013;22(12):2404-2411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Duffy SA, Terrell JE, Valenstein M, Ronis DL, Copeland LA, Connors M. Effect of smoking, alcohol, and depression on the quality of life of head and neck cancer patients. Gen Hosp Psychiatry. 2002;24(3):140-147. [DOI] [PubMed] [Google Scholar]
- 6.Vander Ark W, DiNardo LJ, Oliver DS. Factors affecting smoking cessation in patients with head and neck cancer. Laryngoscope. 1997;107(7):888-892. [DOI] [PubMed] [Google Scholar]
- 7.Chan Y, Irish JC, Wood SJ, et al. Smoking cessation in patients diagnosed with head and neck cancer. J Otolaryngol. 2004;33(2):75-81. [DOI] [PubMed] [Google Scholar]
- 8.Chen AM, Chen LM, Vaughan A, et al. Tobacco smoking during radiation therapy for head-and-neck cancer is associated with unfavorable outcome. Int J Radiat Oncol Biol Phys. 2011;79(2):414-419. [DOI] [PubMed] [Google Scholar]
- 9.Sitas F, Weber MF, Egger S, Yap S, Chiew M, O’Connell D. Smoking cessation after cancer. J Clin Oncol. 2014;32(32):3593-3595. [DOI] [PubMed] [Google Scholar]
- 10.Sharp L, McDevitt J, Carsin AE, Brown C, Comber H. Smoking at diagnosis is an independent prognostic factor for cancer-specific survival in head and neck cancer: findings from a large, population-based study. Cancer Epidemiol Biomarkers Prev. 2014;23(11):2579-2590. [DOI] [PubMed] [Google Scholar]
- 11.van Imhoff LC, Kranenburg GG, Macco S, et al. Prognostic value of continued smoking on survival and recurrence rates in patients with head and neck cancer: a systematic review. Head Neck. 2016;38(suppl 1):E2214-E2220. [DOI] [PubMed] [Google Scholar]
- 12.Khuri FR, Kim ES, Lee JJ, et al. The impact of smoking status, disease stage, and index tumor site on second primary tumor incidence and tumor recurrence in the head and neck retinoid chemoprevention trial. Cancer Epidemiol Biomarkers Prev. 2001;10(8):823-829. [PubMed] [Google Scholar]
- 13.Stevens MH, Gardner JW, Parkin JL, Johnson LP. Head and neck cancer survival and life-style change. Arch Otolaryngol. 1983;109(11):746-749. [DOI] [PubMed] [Google Scholar]
- 14.Wakefield M, Olver I, Whitford H, Rosenfeld E. Motivational interviewing as a smoking cessation intervention for patients with cancer: randomized controlled trial. Nurs Res. 2004;53(6):396-405. [DOI] [PubMed] [Google Scholar]
- 15.Hughes JR, Hatsukami D. Signs and symptoms of tobacco withdrawal. Arch Gen Psychiatry. 1986;43(3):289-294. [DOI] [PubMed] [Google Scholar]
- 16.Jolliffe I. Principal Component Analysis. 2nd ed New York, NY: Springer; 2002. [Google Scholar]
- 17.Lavinghouze SR, Malarcher A, Jama A, Neff L, Debrot K, Whalen L. Trends in quit attempts among adult cigarette smokers—United States, 2001-2013. MMWR Morb Mortal Wkly Rep. 2015;64(40):1129-1135. [DOI] [PubMed] [Google Scholar]
- 18.Schnoll RA, Rothman RL, Newman H, et al. Characteristics of cancer patients entering a smoking cessation program and correlates of quit motivation: implications for the development of tobacco control programs for cancer patients. Psychooncology. 2004;13(5):346-358. [DOI] [PubMed] [Google Scholar]
- 19.Schnoll RA, Malstrom M, James C, et al. Correlates of tobacco use among smokers and recent quitters diagnosed with cancer. Patient Educ Couns. 2002;46(2):137-145. [DOI] [PubMed] [Google Scholar]
- 20.Kashigar A, Habbous S, Eng L, et al. Social environment, secondary smoking exposure, and smoking cessation among head and neck cancer patients. Cancer. 2013;119(15):2701-2709. [DOI] [PubMed] [Google Scholar]
- 21.Gilpin EA, Pierce JP, Farkas AJ. Duration of smoking abstinence and success in quitting. J Natl Cancer Inst. 1997;89(8):572-576. [DOI] [PubMed] [Google Scholar]
- 22.McClave AK, Dube SR, Strine TW, Kroenke K, Caraballo RS, Mokdad AH. Associations between smoking cessation and anxiety and depression among U.S. adults. Addict Behav. 2009;34(6-7):491-497. [DOI] [PubMed] [Google Scholar]
- 23.Trosclair A, Dube SR. Smoking among adults reporting lifetime depression, anxiety, anxiety with depression, and major depressive episode, United States, 2005-2006. Addict Behav. 2010;35(5):438-443. [DOI] [PubMed] [Google Scholar]
- 24.Warren GW, Arnold SM, Valentino JP, et al. Accuracy of self-reported tobacco assessments in a head and neck cancer treatment population. Radiother Oncol. 2012;103(1):45-48. [DOI] [PMC free article] [PubMed] [Google Scholar]