Key Points
Questions
Are there long-term health risks after having adenoids or tonsils removed in childhood?
Findings
In this population-based cohort study of almost 1.2 million children, removal of adenoids or tonsils in childhood was associated with significantly increased relative risk of later respiratory, allergic, and infectious diseases. Increases in long-term absolute disease risks were considerably larger than changes in risk for the disorders these surgeries aim to treat.
Meaning
The long-term risks of these surgeries deserve careful consideration.
This population-based cohort study examines the risk for respiratory, allergic, and infectious diseases following surgical removal of adenoids, tonsils, or both in children durring the first 9 years of life.
Abstract
Importance
Surgical removal of adenoids and tonsils to treat obstructed breathing or recurrent middle-ear infections remain common pediatric procedures; however, little is known about their long-term health consequences despite the fact that these lymphatic organs play important roles in the development and function of the immune system.
Objective
To estimate long-term disease risks associated with adenoidectomy, tonsillectomy, and adenotonsillectomy in childhood.
Design, Setting, and Participants
A population-based cohort study of up to 1 189 061 children born in Denmark between 1979 and 1999 and evaluated in linked national registers up to 2009, covering at least the first 10 and up to 30 years of their life, was carried out. Participants in the case and control groups were selected such that their health did not differ significantly prior to surgery.
Exposures
Participants were classified as exposed if adenoids or tonsils were removed within the first 9 years of life.
Main Outcomes and Measures
The incidence of disease (defined by International Classification of Diseases, Eighth Revision [ICD-8] and Tenth Revision [ICD-10] diagnoses) up to age 30 years was examined using stratified Cox proportional hazard regressions that adjusted for 18 covariates, including parental disease history, pregnancy complications, birth weight, Apgar score, sex, socioeconomic markers, and region of Denmark born.
Results
A total of up to 1 189 061 children were included in this study (48% female); 17 460 underwent adenoidectomy, 11 830 tonsillectomy, and 31 377 adenotonsillectomy; 1 157 684 were in the control group. Adenoidectomy and tonsillectomy were associated with a 2- to 3-fold increase in diseases of the upper respiratory tract (relative risk [RR], 1.99; 95% CI, 1.51-2.63 and RR, 2.72; 95% CI, 1.54-4.80; respectively). Smaller increases in risks for infectious and allergic diseases were also found: adenotonsillectomy was associated with a 17% increased risk of infectious diseases (RR, 1.17; 95% CI, 1.10-1.25) corresponding to an absolute risk increase of 2.14% because these diseases are relatively common (12%) in the population. In contrast, the long-term risks for conditions that these surgeries aim to treat often did not differ significantly and were sometimes lower or higher.
Conclusions and Relevance
In this study of almost 1.2 million children, of whom 17 460 had adenoidectomy, 11 830 tonsillectomy, and 31 377 adenotonsillectomy, surgeries were associated with increased long-term risks of respiratory, infectious, and allergic diseases. Although rigorous controls for confounding were used where such data were available, it is possible these effects could not be fully accounted for. Our results suggest it is important to consider long-term risks when making decisions to perform tonsillectomy or adenoidectomy.
Introduction
Adenoids and tonsils are commonly removed in childhood.1,2,3,4 Conventional wisdom suggests their absence has negligible long-term costs,3 but little support for this claim is available beyond estimates of short-term risks. Understanding the longer-term impact of these surgeries is critical because the adenoids and tonsils are parts of the immune system,3,5 have known roles in pathogen detection and defense,3,5 and are usually removed at ages when the development of the immune system is sensitive.6,7,8,9,10 Some single-disease studies have shown subtle short-term changes in risk after surgery,11,12,13,14 but no estimates of longer-term risk for a broad range of diseases are available. Here we analyze the long-term risks after surgery for 28 diseases in approximately 1.2 million individuals who were followed from birth up to age 30 years, depending on whether adenoidectomy, tonsillectomy, or adenotonsillectomy occurred during the first 9 years of life.
Current research suggests that tonsils and adenoids play specialized roles in immune system development and function.15 The tonsils protect against pathogens both directly3,5 and indirectly by stimulating other immune responses.3,5,16 The pharyngeal, palatine, and lingual tonsils form Waldeyer’s ring around the apex of the respiratory and digestive tract, providing early warnings for inhaled or ingested pathogens.3,5,16 Evidence now suggests that altering early life immune pathways (including dysbiosis)17 can have lasting effects on adult health, warranting concern that the long-term impact of removing adenoids and tonsils in childhood may not yet be fully appreciated.
Physicians often remove adenoids and tonsils to treat recurrent tonsillitis or middle ear infections. Research on consequences mostly relates to perioperative risks3,18 and short-term changes in the symptoms treated. That tonsils (particularly the adenoids) shrink with age, being largest in children and absent in adults,1 suggests that their absence might not affect adult health.3 However, their activity in early-life could still be critical for normal immune system development,3,5 especially given results on how perturbations to early growth and development alter risk of many adult diseases.19,20
Except for rhinosinusitis, ear and throat infections,21,22 and sleep apnea,23 there has been little work on consequences of removing the adenoids or tonsils in childhood. Evidence that adenoidectomy affects the risk of asthma is mixed.14 Tonsillectomy did not reduce the risk of respiratory diseases in adults, but it may increase inflammatory bowel disease risk,13 and improvements in sleep apnea of children may be less than hoped for.23 Surgery may change the risk of nonrespiratory diseases: tonsillectomy is associated with increased risks for certain cancer types11,24,25 and premature acute myocardial infarctions,12 although mechanistic explanations for these associations remain elusive. Reduction of mucosa-associated pathogens with tonsillectomy has been used to treat kidney disease26,27 although beneficial effects are not consistent.28 These single-disease studies make clear that a comprehensive assessment of long-term health risks is needed.
In this study, we estimated disease risk depending on whether adenoids, tonsils, or both were removed in the first 9 years of life. In contrast to previous single-disease, single-surgery studies of short-term risks, we:
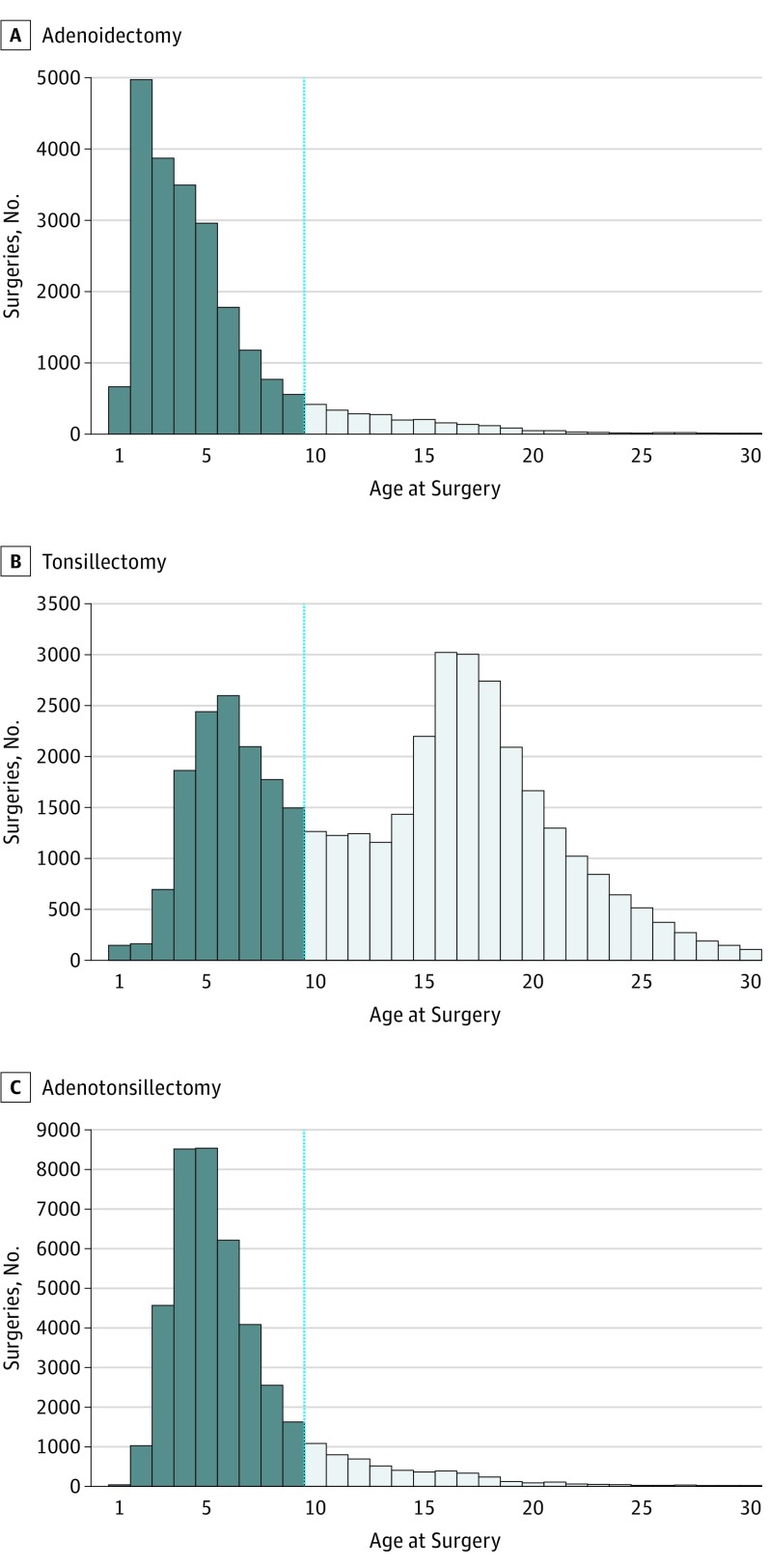
examined effects of all 3 surgeries at ages these are most commonly performed (both generally1,29 and in Denmark) (Figure 1) and most sensitive for immune development;
calculated long-term risks up to age 30 years for 28 diseases in 14 groups;
estimated relative and absolute risks and number of patients needed to treat (NNT) to obtain a first case of harm, to adjust for background rates of disease, and produce clinically applicable numbers;
compared long-term postsurgical absolute risks and benefits for diseases and conditions that these surgeries aim to treat; and
tested for general health differences between those in the case group and those in the control group within the first 9 years of life to establish that individuals who had surgery were not sicklier on average than the controls presurgery.
Figure 1. Age at Adenoidectomy, Tosillectomy, and Adenotonsillectomy for 1 753 100 Danes Born Between 1979 to 2009 and the Selected Surgery Observation Window of 9 Years.
This cut-off for inclusion as surgery cases (dark blue bars) was deemed optimal because the first decade of life is critical for normal immune system development, it represents most of the period in which these surgeries are usually performed, and maximized the number of years available for disease follow-up after surgery. For tonsillectomy this meant that we ignored a second peak at approximately 16 to 17 years because inclusion of these surgeries would have implied insufficient time for follow-up (to 30 years). Our study thus explores the impact of the 3 types of surgery when performed during childhood rather than adolescence. Individuals with these surgeries beyond the 9-year observation end point (dotted vertical line) were not included as either cases or controls. Individuals were also excluded if they had multiple surgeries at different ages, ie, some individuals underwent adenoidectomy followed by tonsillectomy years later or vice versa. Such cases were rare in the sample (<0.2%).
Methods
Study Sample Obtained From the Danish Health Registries
We used data from the Danish Birth Registry of approximately 1.2 million individuals born as singletons between 1979 and 1999 whose health was evaluated up to 2009. To match initial health of cases and controls, we only included those not diagnosed with the outcome diseases prior to surgery in the first 9 years of life (sample sizes presented in eTable 1 in the Supplement). The Danish electronic medical records collected from birth to death reliably sample health sequelae.30,31 Individuals who had surgery after age 9 years were not included; most operations occurred before then (Figure 1). Large sample sizes ensured high statistical power helping to avoid type-2 errors (false-negative resuts). Having access to entire medical histories from birth allowed us to match the health of cases and controls prior to surgery within the first 9 years of life. This reduced potential confounding from reverse causality so that Cox regression became the preferable approach vis-à-vis propensity analysis (eMethods in the Supplement). The many covariates reduced the potential for confounding from those sources. We included individuals with 1 to 21 years of follow-up after age 9 years and those with nonoutlying values for birth weights (1850-5400 g), gestation lengths (30-42 weeks), paternal ages (15-60 years), and maternal ages (15-46 years) at birth. We excluded individuals with missing covariate data and those born before 1979 because their early-life health records were incomplete (eMethods in the Supplement). The characteristics of the study population are shown in the Table.
Table. Characteristics of the Initial Study Sample (N = 1 753 100) for Surgery and Control Groupsa.
| Characteristic | No. (SD) | ||||
|---|---|---|---|---|---|
| Adenoidectomy | Tonsillectomy | Adenotonsillectomy | Control | Total | |
| Sample size, No. (%) | 22 637 (1.3) | 39 685 (2.3) | 42 384 (2.4) | 1 648 394 (94.0) | 1 753 100 |
| Paternal age mean (SD), y | 30.1 (5.8) | 29.7 (5.6) | 30.1 (5.7) | 31.3 (5.7) | 31.2 (5.7) |
| Maternal age mean (SD), y | 27.0 (4.9) | 26.8 (4.7) | 27.2 (4.8) | 28.5 (4.8) | 28.4 (4.9) |
| Gestation length, mean (SD), weeks | 39.4 (1.9) | 39.7 (1.6) | 39.6 (1.7) | 39.7 (1.6) | 40.0 (1.6) |
| Maternal bleeding, % (SD) | 9.6 (0.3) | 8.1 (0.2) | 9.0 (0.2) | 7.3 (0.2) | 7.4 (0.2) |
| Fetal oxygen deprivation, % (SD) | 0.13 (0.04) | 0.13 (0.04) | 0.09 (0.03) | 0.09 (0.03) | 0.09 (0.03) |
| Pregnancy edema, % (SD) | 1.44 (0.12) | 1.42 (0.12) | 1.08 (0.10) | 0.79 (0.09) | 0.82 (0.09) |
| Apgar score 1-10, mean (SD) | 9.8 (0.7) | 9.8 (0.5) | 9.8 (0.6) | 9.8 (0.6) | 9.8 (0.6) |
| Birth weight, mean (SD), grams | 3377 (597) | 3443 (537) | 3448 (574) | 3499 (541) | 3495 (543) |
| Preexisting hypertension (%) | 0.26 (0.05) | 0.15 (0.04) | 0.27 (0.05) | 0.33 (0.06) | 0.32 (0.06) |
| Preexisting diabetes, % (SD) | 0.40 (0.06) | 0.35 (0.06) | 0.50 (0.07) | 0.39 (0.06) | 0.39 (0.06) |
| Previous induced abortion (%) | 20.2 (0.4) | 19.5 (0.4) | 19.6 (0.4) | 18.2 (0.3) | 18.3 (0.3) |
| Previous spontaneous abortion, % (SD) | 16.3 (0.3) | 15.5 (0.3) | 15.6 (0.3) | 14.2 (0.3) | 14.3 (0.3) |
| Education, combined total years, mean (SD) | 24.4 (4.9) | 24.5 (4.6) | 24.4 (4.6) | 25.6 (4.7) | 25.5 (4.8) |
| Income, combined average, mean (SD), DKK | 381 030 (188 098) | 394 585 (163 759) | 361 933 (145 965) | 362 241 (172 797) | 363 188 (172 296) |
| Nationality (other than Danish) % (SD) | 5.58 (0.23) | 4.33 (0.2) | 7.69 (0.27) | 6.89 (0.25) | 6.83 (0.25) |
| Region in Denmark most lived in, % (SD) | |||||
| Hovedstaden | 29.1 (0.4) | 27.4 (0.4) | 23.6 (0.4) | 28.7 (0.4) | 28.5 (0.4) |
| Sjælland | 21.8 (0.4) | 18.6 (0.3) | 16.2 (0.3) | 14.5 (0.3) | 14.7 (0.3) |
| Syddanmark | 23.1 (0.4) | 19.7 (0.4) | 22.1 (0.4) | 22.4 (0.4) | 22.3 (0.4) |
| Midtjylland | 15.0 (0.3) | 23.3 (0.4) | 24.9 (0.4) | 23.7 (0.4) | 23.6 (0.4) |
| Nordjylland | 10.8 (0.3) | 10.7 (0.3) | 13.0 (0.3) | 10.5 (0.3) | 10.6 (0.3) |
| Birth year, mean (SD) | 1988 (8) | 1987 (6) | 1991 (7) | 1994 (8) | 1993 (8) |
| Birth season, month 1-12, mean (SD) | 6.4 (3.3) | 6.3 (3.3) | 6.4 (3.3) | 6.4 (3.3) | 6.4 (3.3) |
| Female sex, % (SD) | 40.7 (0.4) | 58.9 (0.4) | 44.5 (0.5) | 48.6 (0.5) | 48.7 (0.5) |
| Demographic parity, % (SD) | |||||
| First born | 46.2 (0.5) | 45.5 (0.5) | 47.9 (0.5) | 44.1 (0.5) | 44.3 (0.5) |
| Second born | 37.2 (0.4) | 38.2 (0.4) | 35.1 (0.4) | 37.3 (0.4) | 37.3 (0.4) |
| Third born | 12.0 (0.3) | 12.3 (0.3) | 12.6 (0.3) | 13.8 (0.3) | 13.7 (0.3) |
| Fourth (or higher born) | 4.33 (0.20) | 3.84 (0.19) | 4.33 (0.20) | 4.7 (0.21) | 4.67 (0.21) |
Numbers, means, percentages, and SDs are provided. This is the study sample before outlying values and exclusions were applied; for exact sample sizes used in Cox regression analyses for each disease group, see eTable 1 in the Supplement.
Covariate data were obtained from the Danish Birth Registry and others: Danish Patient Registry with nationwide hospital admission and ICD-8 and ICD-10 diagnosis data; Danish Psychiatric Registry with psychiatric diagnoses for inpatient admissions; and the Danish Civil Registration and Cause of Death Registries with dates of death, migration, socioeconomic, and other information. We combined individual-level information from different registries using unique deidentified personal identification numbers. Because data are collected for all Danish residents with a personal identification number assigned at birth (or on taking up residency), we are confident that we obtained complete health and socioeconomic histories of the approximately 1.2 million individuals in the analyses.
Defining Surgery Groups
Of the 3 main types of tonsils—pharyngeal (the adenoids), palatine (the tonsils), and lingual—we focused on surgery removing the first 2 (adenoidectomy, tonsillectomy), because lingual tonsils are not commonly removed, and on adenotonsillectomy, where both are removed in the same surgery.
Surgery codes are based on ICD operation classification codes from Statistics Denmark (up to 1996) and the Nordic Medico-Statistical Committee (NOMESCO) Classification of Surgical Procedures (NCSP) from 1996 onwards including: adenoidectomy, 2618, EMB30; tonsillectomy, 2614, EMB10; adenotonsillectomy, EMB20. Prior to 1996, when there was no code for adenotonsillectomy, we recorded this procedure when both codes (2618, 2614) had matching entry dates.
Selecting Disease Groups
We selected diseases thought to be affected by changes to immunity (infections, allergies) and other disorders examined in studies of short-term health impacts of these procedures (respiratory infections). We also included broader disease groups (all circulatory, nervous system, endocrine, and autoimmune diseases) because immune dysfunction or dysbiosis could affect many processes (eTable 2 in the Supplement). In Denmark, ICD-8 and ICD-10 codes were used before and after 1994, respectively. To reduce the likelihood of false-negative results, we did analyses of statistical power using R statistical software (version 3.4.1, R Foundation); this excluded some diseases with insufficient outcomes to adequately test the null hypothesis of no association between surgery and incident disease (eMethods in the Supplement).
Covariates
To account for possibly confounding effects on the prevalence of outcome diseases, we included these covariates in Cox regressions: binary variables for maternal preexisting conditions (eTable 2 in the Supplement) including hypertension (primary or secondary hypertension, hypertensive heart, or renal disease), diabetes (types 1 and 2, malnutrition-related, other or unspecified), previous spontaneous or induced abortions; maternal pregnancy-related variables including gestation length (in weeks) and variables indicating maternal bleeding (hemorrhage, placenta praevia), fetal oxygen deprivation (hypoxia, asphyxia), and pregnancy edema. Parental variables included a binary code for whether either parent had ever been diagnosed within the same disease group as their child (accounting for familial transmission), education (total years summed for both parents), and average income (summed 1979-2009 across both parents). Birth-related variables included birth weight (in grams), season (calendar month, 1-12) and cohort (3-yearly between 1979-1999 accounting for putative changes in diagnostic criteria over time), and Apgar score of 1 to 10 (maximally 2 points for each category) given to newborns at 5 minutes of life ranging from poor to excellent health. Other child-related variables included sex (male, female), nationality (Danish national, immigrant), parity (first, second, third, fourth or higher born), and the region in Denmark (Hovedstaden/Copenhagen, Sjælland, Syddanmark, Midtjylland, or Nordjylland) that individuals had resided in most, accounting for possible regional differences in diagnoses. Accurate data on parental and/or patient smoking status (a potentially important confounder) were not available (ie, only available from 1993 onwards and assessed in a small percentage of parents).
Statistical Design and Analysis
We used Cox regressions to estimate relative risk for the 28 diseases up to age 30 (with age as timescale), depending on whether surgery occurred within the first 9 years of life. Cox regression model assumptions were confirmed and proportional hazards ensured by stratifying for sex, birth cohort, birth season and demographic parity while also accounting for 18 further covariates. To reduce chances of type-1 errors, Cox regression P values were Bonferroni corrected for the 78 analyses performed (Bonferroni-corrected α P value <.05/78 = 0.000641). To provide clinically useful results, absolute risks and number of patients needed to treat (NNT) before causing benefit or harm to one of them were calculated from relative risks and disease prevalence within the first 30 years of life (eMethods in the Supplement).
Each of the 3 surgeries was compared with controls (no surgeries during the study period) after ensuring they were otherwise of comparable health (see Testing for Biases in General Health Before Surgery section). Fewer than 0.2% of individuals in the original sample underwent more than 1 surgery at different times, indicating no need to test for interaction effects between surgeries and later disease risks.
Estimating Risks for Nonimmune Diseases and Conditions That Surgeries Aim to Treat
To weigh potential disease risks against benefits of surgery, we calculated relative risks, absolute risks, and NNTs for the conditions that these surgeries treat using the same samples and statistical setup described herein. Conditions included obstructive sleep apnea, sleep disorders, abnormal breathing, (chronic) sinusitis, otitis media, and (chronic) tonsillitis (eTable 2 in the Supplement). As a control, we tested whether surgeries were associated with diseases unrelated to the immune system, estimating risk for osteoarthritis, cardiac arrhythmias, heart failure, acid-peptic disease and alcoholic hepatitis (eTable 2 in the Supplement) using the same sample and statistical setup described herein. Results (eTable 3 in the Supplement) showed that surgery was not associated with these non–immune diseases up to age 30 years.
Testing for Biases in General Health Before Surgery
With complete medical records from birth, we tested whether general health of cases and controls was different presurgery. The null hypotheses tested were that there was no difference in general health between cases and controls for: (1) age at any disease diagnosis, or (2) age at first diagnosis for diseases recorded before surgery. Neither null hypothesis was rejected, suggesting that cases were no less healthy than controls presurgery in the first 9 years of life. Power analyses confirmed sufficient sample sizes and power to compare general health of those in the case with those in the control groups (eMethods in the Supplement).
Results
Association of Surgery With Risk of Respiratory Disease
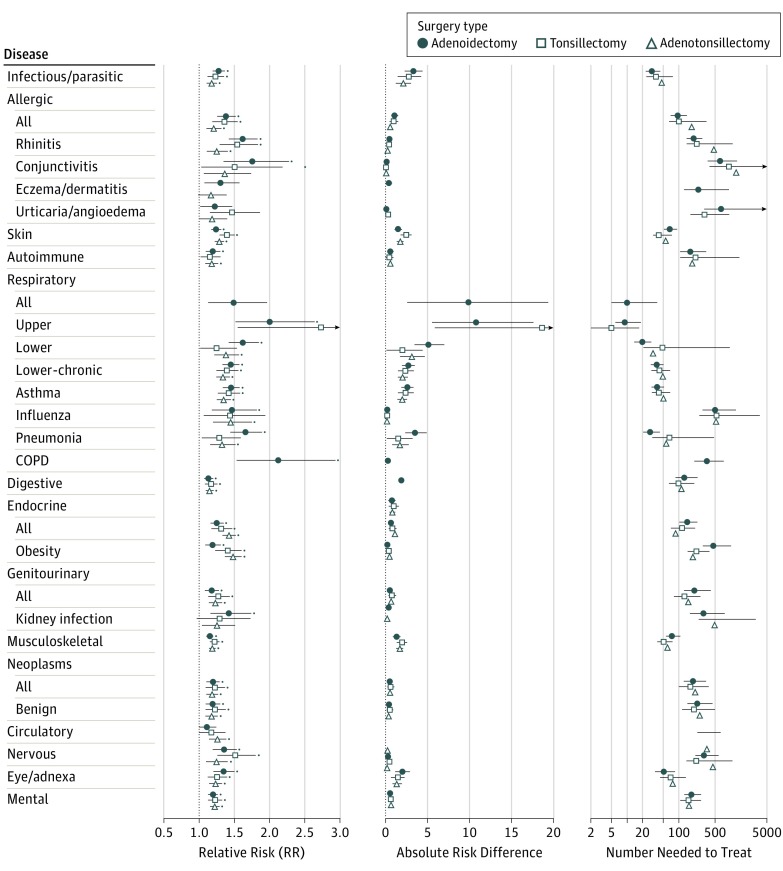
Up to 1 189 061 children were analyzed in this study (48% female); 17 460 underwent adenoidectomy, 11 830 tonsillectomy, and 31 377 adenotonsillectomy; 1 157 684 were in the control group (eTable 1 in the Supplement). Tonsillectomy was associated with nearly tripled relative risk of diseases of the upper respiratory tract (RR = 2.72; 95% CI, 1.54-4.80) (Figure 2) (eTables 4 and 5 in the Supplement) with a substantial increase in absolute risk (absolute risk difference [ARD], 18.61%) (eTable 4 in the Supplement) and a small number needed to treat (NNT-harm, 5) (eTable 4 in the Supplement), suggesting that only about 5 tonsillectomies would need to be performed for an additional upper respiratory tract disease to be associated with one of those patients. The degree to which tonsillectomy is associated with this disease in the overall population later in life may therefore be considerable.
Figure 2. Risk of Disease up to Age 30 Years After Removal of Tonsils and Adenoids in the First 9 Years of Life.
Abbreviation: COPD, chronic obstructive pulmonary disorder. Relative risks (RR) and 95% CIs are the exponents from Cox regressions that capture risk of each disease up to age 30 years depending on whether surgery was performed. The RR P values significant after Bonferroni corrections for 78 tests are shown by a blue point above the upper confidence interval for each disease. The RR values are presented only for analyses with sufficient power for hypothesis testing (see methods). Absolute risk differences (ARD) and 95% CIs were estimated as ARD = 100 × CR × (1-RR), where CR (control risk) is the risk of the disease in the control sample and RR is the relative risk of disease in individuals post-surgery relative to the disease risk in the control sample that did not undergo surgery. Numbers needed to treat (NNT) and 95% CIs were estimated as NNT = 100/ARD. The NNT values above or below zero indicate harm or benefit associated with surgery, respectively, with values closer to 0 indicating harm occurring more often to patients. For example, for risk of asthma after adenoidectomy (ie, RR = 1.45; 95% CI, 1.33-1.57), the event rate in the control group (or control risk, CR) for asthma up to age 30 years in our dataset was 5.8%, ARD = |100 × 0.058 x (1−1.45)| = 2.6 and NNT = 100/2.6 = 38. Relative risk of asthma was 1.45 and thus 45% higher after adenoidectomy compared with controls (no surgery), which translates to an absolute risk difference of 2.6% or 2.6 more cases of asthma per 100 treated patients. In other words, approximately 38 adenoidectomies would need to be performed for an additional asthma diagnosis to be associated with one of those patients in the first 30 years of life. Note: urinary tract infections were not included in the kidney infection group.
Adenoidectomy was associated with more than doubled relative risk of chronic obstructive pulmonary disorder ([COPD]; RR = 2.11; 95% CI, 1.53-2.92) (Figure 2) (eTables 4 and 6 in the Supplement) and nearly doubled relative risk of upper respiratory tract diseases (RR = 1.99; 95% CI, 1.51-2.63) and conjunctivitis (RR = 1.75; 95% CI, 1.35-2.26). This corresponds to a substantial increase in absolute risk for upper respiratory tract diseases (ARD = 10.7%; 95% CI, 5.49-17.56) (eTable 4 in the Supplement), but small increases for COPD (ARD = 0.29%; 95% CI, 0.13-0.48) and conjunctivitis (ARD = 0.16%; 95% CI, 0.07-0.26), consistent with the NNT values (NNT-harm: diseases of upper respiratory tract = 9; COPD = 349; conjunctivitis = 624) (eTable 4 in the Supplement). Although relative risk increases were similar for these diseases, the large differences in absolute risk reflect the prevalence of these disorders in the population. Diseases of the upper respiratory tract occur 40 to 50 times more frequently (in 10.7% of those in the control group aged ≤30 years) than do COPD (0.25%) and conjunctivitis (0.21%).
Other Significant Effects on Long-term Disease Risks
For some diseases, even modest increases in relative risk (RR, 1.17-1.65) resulted in relatively large increases in absolute risk (2%-9%) and low NNTs (NNT-harm <50) because of the high prevalence of these diseases in the population (control risk, 5%-20%) (eTable 4 in the Supplement). These were mainly respiratory diseases (groups: all, lower, lower-chronic, asthma, pneumonia), infectious/parasitic diseases (all), skin diseases (all), musculoskeletal (all), and eye/adnexa (all). For example, adenotonsillectomy was significantly associated with 17% increased relative risk of infectious diseases (RR = 1.17; 95% CI, 1.10-1.25) (eTables 4 and 7 in the Supplement). However, because infectious diseases are relatively common (12%) (eTable 4 in the Supplement), the absolute risk increase of 2.14% was lower, but still suggested approximately 47 adenotonsillectomies would need to be performed for an extra infectious disease to be associated with one of those patients (eTable 4 in the Supplement).
When all 28 disease groups were considered, there were small but significant increases in relative risk for 78% of them after Bonferroni correction. The negative health consequences of these surgeries within the first 30 years of life thus appear to be consistent, affecting a range of tissues and organ systems. This highlights the importance of adenoids and tonsils for normal immune system development and suggests that their early-life removal may slightly but significantly perturb many processes important for later-life health.
Later-Life Risk of Conditions That Surgeries Directly Aimed to Treat Were Mixed
Risks for conditions that surgeries aimed to treat were mixed (eTable 8 in the Supplement). Surgery was associated with significantly reduced long-term relative risk for 7 of 21 conditions (33% of our disease-specific analyses), with no changes for 9 (43%) other conditions and significant increases for 5 (24%).
For example, adenoidectomy was associated with significantly reduced relative risk for sleep disorders (RR = 0.30; 95% CI, 0.15-0.60; ARD = −0.083%; 95% CI, −0.10 to −0.05), and all surgeries were associated with significantly reduced risk for tonsillitis and chronic tonsillitis (ie, RR = 0.09-0.54; ARD, −0.29% to −2.10%). For abnormal breathing, there was no significant change in relative risk up to 30 years of age after any surgery and no change in relative risk for sinusitis after adenoidectomy or tonsillectomy. Conditions where relative risk significantly increased included otitis media, which showed a 2- to 5-fold increase postsurgery (RR, 2.06-4.84; ARD, 5.3%-19.4%), and sinusitis, which increased significantly after adenotonsillectomy (RR = 1.68; 95% CI, 1.32-2.14; ARD = 0.11%; 95% CI, 0.05-0.19) (eDiscussion in the Supplement).
Thus, short-term health benefits of these surgeries for some conditions may not continue up to age 30 years. Indeed, apart from the consistently reduced risk for tonsillitis (after any surgeries) and sleep disorders (after adenoidectomy), longer-term risks for abnormal breathing, sinusitis, chronic sinusitis, and otitis media were either significantly higher after surgery or not significantly different.
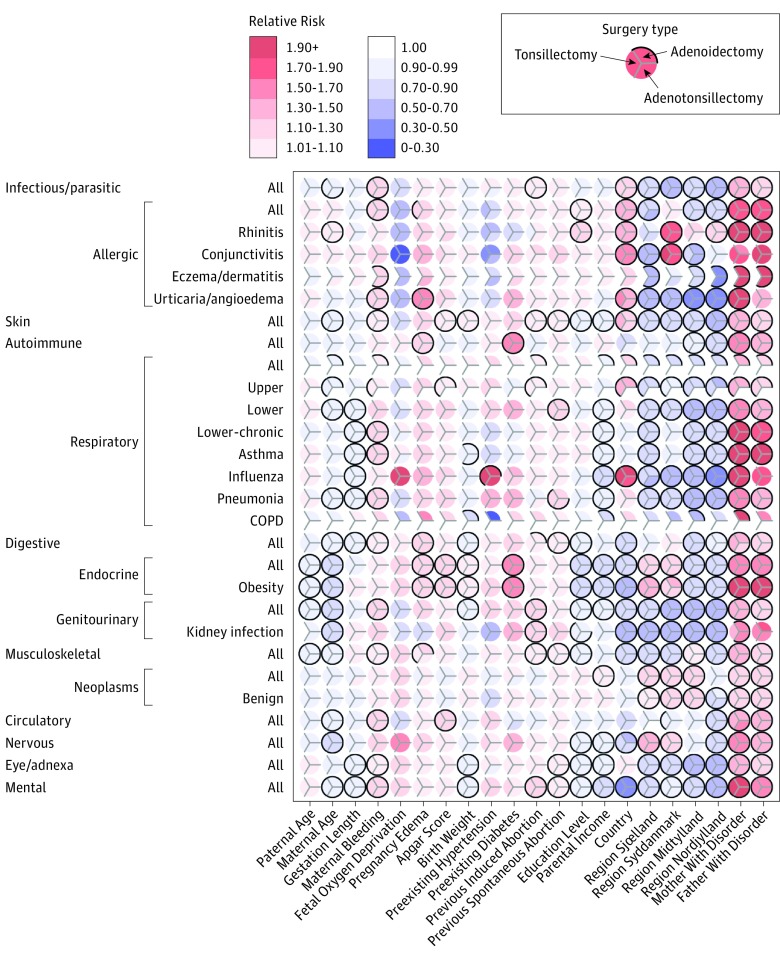
Risk Patterns for Covariates
The many associations between disease risk and covariates highlight the complexity of the factors affecting diseases (Figure 3) (eTables 5-7 in the Supplement). Consider those significantly associated with upper respiratory tract diseases (Figure 3) and their largest increases in relative (RR, 1.99-2.72) and absolute risks (ARD, 10.77%-18.61%) after adenoidectomy and tonsillectomy (Figure 2). Risks for these diseases slightly but significantly decreased for offspring born to older mothers (RR = 0.96; 95% CI, 0.95-0.98; both surgeries), slightly increased (tonsillectomies) when maternal bleeding occurred during pregnancy (RR = 1.07; 95% CI, 1.03-1.12), increased (both analyses) with Apgar score (RR = 1.09; 95% CI, 1.04-1.13, both surgeries), increased (both analyses) when mothers had a previous induced abortion (RR = 1.09; 95% CI, 1.06-1.12; both surgeries), increased in immigrants relative to Danish nationals (RR = 1.40; 95% CI, 1.33-1.47; both surgeries), decreased in those living anywhere in Denmark other than Copenhagen (RR, 0.69-0.93), and increased when fathers or mothers had a history of the same disease (RR, 1.29-1.38). Parental history of disease was significantly associated with prevalence in children for almost all diseases (RR, 1.10-3.71).
Figure 3. Disease Risk Patterns for Covariates.
Relative risk magnitude and direction correspond to red (increased relative risk) and purple (decreased relative risk) colors derived from Cox regressions capturing the risk of diseases (vertical axis) within the first 30 years of life depending on 21 covariates (horizontal axis). Within each circle there are 3 divisions corresponding to surgery type. A black border indicates whether risk for that particular disease-covariate combination was significant after Bonferroni correction for 78 tests; a complete black border surrounding a circle indicates that risks were significant for all 3 surgeries. Disease risks for the covariate region most lived in Denmark are relative to Hovedstaden (Copenhagen region). Note: Urinary tract infections were not included in the kidney infection group.
Parental education, income, and country of origin had many significant effects, but risk direction varied depending on the disease considered and were generally modest, consistent with free health care for all residents in Denmark. For example, mental disorders were less frequent in Danish nationals than immigrants (RR, 0.48-0.49), but influenza risk was higher in Danes (RR, 1.89-2.06). Endocrine and mental diseases were associated with many covariates suggesting complex causation. We discuss other associations with covariates in the eResults in the Supplement.
Discussion
We estimated relative risks, absolute risks, and number needed to treat to gain a balanced view of how adenoidectomy and tonsillectomy performed between birth and 9 years were associated with disease up to age 30 years in Denmark. Disease risks typically increased after surgery and for some disorders relative risks translated into substantial changes in absolute risk; for these, low NNT values suggested that only a few surgeries would need to be performed for an extra case of disease to be associated with one of those patients.
Although otorhinolaryngologists are sensitive to short-term consequences of procedures for the symptoms that they treat,18,32,33,34 they have had no evidence to evaluate the full range of long-term risks. Using the Danish public health data allowed us to control for many medical, socioeconomic, and statistical confounders so that credible estimates of long-term risks of surgery could be made. We found that tonsillectomy was associated with a nearly tripled risk of upper respiratory tract diseases, and that adenoidectomy was associated with doubled risk of COPD and upper respiratory tract diseases and nearly doubled risk of conjunctivitis. Large increases in absolute risk for upper respiratory tract diseases also occurred. Smaller elevated risks for a broad range of other diseases translated into detectable increases in absolute disease risks with high prevalence in the population (infectious/parasitic, skin, musculoskeletal, and eye/adnexa diseases). These findings add to previous research on single diseases that showed increased risks of breast cancer11 and premature acute myocardial infarctions12 associated with these surgeries. In contrast, the long-term benefits of surgery were generally minor and provided a neutral spectrum of sometimes decreasing and sometimes increasing risk for the conditions they aimed to treat.
Our results raise the important issue of when the benefits of operating outweigh overall short- and long-term morbidity risks. For much of the past century these operations were common, but they have declined recently35,36 with the emergence of alternative treatments for infections in ear, oral, and nasal cavities, coinciding with heightened appreciation of the short-term risks of surgery.37 The long-term risk associations presented herein add a new perspective to these considerations. They suggest that revived discussion may be timely, because these surgical procedures remain among the most common medical interventions in childhood.3,4 It is important to note that the cumulative long-term impact of surgery depends on the prevalence of specific conditions in the population because these trends are not straightforward to extrapolate from relative risks. Thus, the potential impacts of tonsillectomy and adenoidectomy on the absolute risk of upper respiratory tract diseases were substantial because these conditions were prevalent, whereas those of adenoidectomy on the absolute risks of COPD and conjunctivitis were small because those diseases have low prevalence.
Apart from the specific cases above, our results suggest a more general association between removal of immune organs in the upper respiratory tract during childhood and increased risk of infectious/parasitic diseases later in life. Given that tonsils and adenoids are part of the lymphatic system and play a key role both in the normal development of the immune system and in pathogen screening during childhood and early-life,3 it is not surprising that their removal may impair pathogen detection and increase risk of later respiratory and infectious diseases. However, the associations between these surgeries and diseases of the skin, eyes, and musculoskeletal system are not likely to be directly linked to removal of the tonsils or adenoids and need further investigation. The growing body of research on developmental origins of disease19,38 has convincingly demonstrated that even small perturbations to fetal and childhood growth and development can have lifelong consequences for general health.
Limitations
Our study did not address risks of diseases in those older than 30 years, the limit of our sample, and even though records of the entire population of Denmark were available, we did not have large enough samples for rarer diseases to obtain reliable risk estimates. A strength of our study is its large coverage of a relatively homogeneous population with equal access to health care irrespective of socioeconomic status, but this may mean that some results will not generalize to other populations. Although many controls were employed to minimize confounding and reverse causation between surgery and disease risk, it is possible that we could not completely remove these effects. Because this study is the first to assess long-term risks associated with these surgeries, we could not compare our results with other studies. We therefore recommend additional studies to validate our findings. We could not include parental smoking data in our analyses as a potential confounding effect, which is a limitation for assessing offspring respiratory disease risk.39 However, we note that our parental education covariate is correlated with smoking, and should thus have partially covered risks of exposure to parental smoking during childhood.40,41 The socioeconomic variables that we were able to include were also quantitative and available without missing values, whereas smoking scores are often self-reported and of more dubious quality.42
Conclusions
To our knowledge, this is the first study to estimate long-term disease associations with early-life tonsillectomies and adenoidectomies for a broad range of diseases. Risks were significant for many diseases and large for some. We showed that absolute risks and the number of patients needed to treat before enhanced health risks later in life become apparent were more consistent and widespread than the immediate population-wide benefits of childhood surgery for subsequent health within the first 30 years of life. The associations that we uncovered in the Danish population appear to warrant renewed evaluation of potential alternatives to surgery.
eTable 1. Sample sizes (main analysis)
eTable 2. ICD-8 and ICD-10 codes (all analyses)
eTable 3. Relative risks for non-immune diseases
eTable 4. Risks (relative, absolute, NNT) for disease outcomes
eTable 5. Full Cox regression results (tonsillectomy)
eTable 6. Full Cox regression results (adenoidectomy)
eTable 7. Full Cox regression results (adenotonsillectomy)
eTable 8. Risks (relative, absolute, NNT) for conditions surgeries treat
eMethods
eResults
References
- 1.Casselbrant ML. What is wrong in chronic adenoiditis/tonsillitis anatomical considerations. Int J Pediatr Otorhinolaryngol. 1999;49(suppl 1):S133-S135. [DOI] [PubMed] [Google Scholar]
- 2.Kvaerner KJ, Nafstad P, Jaakkola JJ. Otolaryngological surgery and upper respiratory tract infections in children: an epidemiological study. Ann Otol Rhinol Laryngol. 2002;111(11):1034-1039. [DOI] [PubMed] [Google Scholar]
- 3.Ramos SD, Mukerji S, Pine HS. Tonsillectomy and adenoidectomy. Pediatr Clin North Am. 2013;60(4):793-807. [DOI] [PubMed] [Google Scholar]
- 4.Baugh RF, Archer SM, Mitchell RB, et al. ; American Academy of Otolaryngology-Head and Neck Surgery Foundation . Clinical practice guideline: tonsillectomy in children. Otolaryngol Head Neck Surg. 2011;144(1)(suppl):S1-S30. [DOI] [PubMed] [Google Scholar]
- 5.Brandtzaeg P. Immunology of tonsils and adenoids: everything the ENT surgeon needs to know. Int J Pediatr Otorhinolaryngol. 2003;67(suppl 1):S69-S76. [DOI] [PubMed] [Google Scholar]
- 6.Dowling DJ, Levy O. Ontogeny of early life immunity. Trends Immunol. 2014;35(7):299-310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Goenka A, Kollmann TR. Development of immunity in early life. J Infect. 2015;71(suppl 1):S112-S120. [DOI] [PubMed] [Google Scholar]
- 8.Sharma AA, Jen R, Butler A, Lavoie PM. The developing human preterm neonatal immune system: a case for more research in this area. Clin Immunol. 2012;145(1):61-68. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Simon AK, Hollander GA, McMichael A. Evolution of the immune system in humans from infancy to old age. Proc Biol Sci. 2015;282(1821):20143085. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.West LJ. Defining critical windows in the development of the human immune system. Hum Exp Toxicol. 2002;21(9-10):499-505. [DOI] [PubMed] [Google Scholar]
- 11.Brasky TM, Bonner MR, Dorn J, et al. . Tonsillectomy and breast cancer risk in the Western New York Diet Study. Cancer Causes Control. 2009;20(3):369-374. [DOI] [PubMed] [Google Scholar]
- 12.Janszky I, Mukamal KJ, Dalman C, Hammar N, Ahnve S. Childhood appendectomy, tonsillectomy, and risk for premature acute myocardial infarction—a nationwide population-based cohort study. Eur Heart J. 2011;32(18):2290-2296. [DOI] [PubMed] [Google Scholar]
- 13.Johansson E, Hultcrantz E. Tonsillectomy—clinical consequences twenty years after surgery? Int J Pediatr Otorhinolaryngol. 2003;67(9):981-988. [DOI] [PubMed] [Google Scholar]
- 14.Mattila PS, Hammarén-Malmi S, Pelkonen AS, et al. . Effect of adenoidectomy on respiratory function: a randomised prospective study. Arch Dis Child. 2009;94(5):366-370. [DOI] [PubMed] [Google Scholar]
- 15.Layton TB. What can we do to diminish the number of tonsil operations. Lancet. 1934;223(5760):117-119. [Google Scholar]
- 16.Kato A, Hulse KE, Tan BK, Schleimer RP. B-lymphocyte lineage cells and the respiratory system. J Allergy Clin Immunol. 2013;131(4):933-957. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Donaldson GP, Lee SM, Mazmanian SK. Gut biogeography of the bacterial microbiota. Nat Rev Microbiol. 2016;14(1):20-32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Subramanyam R, Varughese A, Willging JP, Sadhasivam S. Future of pediatric tonsillectomy and perioperative outcomes. Int J Pediatr Otorhinolaryngol. 2013;77(2):194-199. [DOI] [PubMed] [Google Scholar]
- 19.Gluckman PD, Hanson MA. Developmental origins of health and disease. Cambridge, England: Cambridge University Press; 2006. [Google Scholar]
- 20.Hanson MA, Gluckman PD. Developmental origins of health and disease: new insights. Basic Clin Pharmacol Toxicol. 2008;102(2):90-93. [DOI] [PubMed] [Google Scholar]
- 21.Brietzke SE, Brigger MT. Adenoidectomy outcomes in pediatric rhinosinusitis: a meta-analysis. Int J Pediatr Otorhinolaryngol. 2008;72(10):1541-1545. [DOI] [PubMed] [Google Scholar]
- 22.Buskens E, van Staaij B, van den Akker J, Hoes AW, Schilder AG. Adenotonsillectomy or watchful waiting in patients with mild to moderate symptoms of throat infections or adenotonsillar hypertrophy: a randomized comparison of costs and effects. Arch Otolaryngol Head Neck Surg. 2007;133(11):1083-1088. [DOI] [PubMed] [Google Scholar]
- 23.Friedman M, Wilson M, Lin HC, Chang HW. Updated systematic review of tonsillectomy and adenoidectomy for treatment of pediatric obstructive sleep apnea/hypopnea syndrome. Otolaryngol Head Neck Surg. 2009;140(6):800-808. [DOI] [PubMed] [Google Scholar]
- 24.Vestergaard H, Westergaard T, Wohlfahrt J, Hjalgrim H, Melbye M. Tonsillitis, tonsillectomy and Hodgkin’s lymphoma. Int J Cancer. 2010;127(3):633-637. [DOI] [PubMed] [Google Scholar]
- 25.Sun LM, Chen HJ, Li TC, Sung FC, Kao CH. A nationwide population-based cohort study on tonsillectomy and subsequent cancer incidence. Laryngoscope. 2015;125(1):134-139. [DOI] [PubMed] [Google Scholar]
- 26.Maeda I, Hayashi T, Sato KK, et al. . Tonsillectomy has beneficial effects on remission and progression of IgA nephropathy independent of steroid therapy. Nephrol Dial Transplant. 2012;27(7):2806-2813. [DOI] [PubMed] [Google Scholar]
- 27.Liu LL, Wang LN, Jiang Y, et al. . Tonsillectomy for IgA nephropathy: a meta-analysis. Am J Kidney Dis. 2015;65(1):80-87. [DOI] [PubMed] [Google Scholar]
- 28.Feehally J, Coppo R, Troyanov S, et al. ; VALIGA study of ERA-EDTA Immunonephrology Working Group . Tonsillectomy in a European cohort of 1,147 patients with IgA nephropathy. Nephron. 2016;132(1):15-24. [DOI] [PubMed] [Google Scholar]
- 29.Erickson BK, Larson DR, St Sauver JL, Meverden RA, Orvidas LJ. Changes in incidence and indications of tonsillectomy and adenotonsillectomy, 1970-2005. Otolaryngol Head Neck Surg. 2009;140(6):894-901. [DOI] [PubMed] [Google Scholar]
- 30.Schmidt M, Schmidt SA, Sandegaard JL, Ehrenstein V, Pedersen L, Sørensen HT. The Danish National Patient Registry: a review of content, data quality, and research potential. Clin Epidemiol. 2015;7:449-490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Thygesen LC, Daasnes C, Thaulow I, Brønnum-Hansen H. Introduction to Danish (nationwide) registers on health and social issues: structure, access, legislation, and archiving. Scand J Public Health. 2011;39(7)(suppl):12-16. [DOI] [PubMed] [Google Scholar]
- 32.Brietzke SE, Gallagher D. The effectiveness of tonsillectomy and adenoidectomy in the treatment of pediatric obstructive sleep apnea/hypopnea syndrome: a meta-analysis. Otolaryngol Head Neck Surg. 2006;134(6):979-984. [DOI] [PubMed] [Google Scholar]
- 33.Paradise JL, Bluestone CD, Rogers KD, et al. . Efficacy of adenoidectomy for recurrent otitis media in children previously treated with tympanostomy-tube placement. Results of parallel randomized and nonrandomized trials. JAMA. 1990;263(15):2066-2073. [PubMed] [Google Scholar]
- 34.van den Aardweg MT, Boonacker CW, Rovers MM, Hoes AW, Schilder AG. Effectiveness of adenoidectomy in children with recurrent upper respiratory tract infections: open randomised controlled trial. BMJ. 2011;343:d5154. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Curtin JM. The history of tonsil and adenoid surgery. Otolaryngol Clin North Am. 1987;20(2):415-419. [PubMed] [Google Scholar]
- 36.Grob GN. The rise and decline of tonsillectomy in twentieth-century America. J Hist Med Allied Sci. 2007;62(4):383-421. [DOI] [PubMed] [Google Scholar]
- 37.Randall DA, Hoffer ME. Complications of tonsillectomy and adenoidectomy. Otolaryngol Head Neck Surg. 1998;118(1):61-68. [DOI] [PubMed] [Google Scholar]
- 38.Wadhwa PD, Buss C, Entringer S, Swanson JM. Developmental origins of health and disease: brief history of the approach and current focus on epigenetic mechanisms. Semin Reprod Med. 2009;27(5):358-368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pattenden S, Antova T, Neuberger M, et al. . Parental smoking and children’s respiratory health: independent effects of prenatal and postnatal exposure. Tob Control. 2006;15(4):294-301. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Osler M, Gerdes LU, Davidsen M, et al. . Socioeconomic status and trends in risk factors for cardiovascular diseases in the Danish MONICA population, 1982-1992. J Epidemiol Community Health. 2000;54(2):108-113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Gilman SE, Martin LT, Abrams DB, et al. . Educational attainment and cigarette smoking: a causal association? Int J Epidemiol. 2008;37(3):615-624. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Newell SA, Girgis A, Sanson-Fisher RW, Savolainen NJ. The accuracy of self-reported health behaviors and risk factors relating to cancer and cardiovascular disease in the general population: a critical review. Am J Prev Med. 1999;17(3):211-229. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Sample sizes (main analysis)
eTable 2. ICD-8 and ICD-10 codes (all analyses)
eTable 3. Relative risks for non-immune diseases
eTable 4. Risks (relative, absolute, NNT) for disease outcomes
eTable 5. Full Cox regression results (tonsillectomy)
eTable 6. Full Cox regression results (adenoidectomy)
eTable 7. Full Cox regression results (adenotonsillectomy)
eTable 8. Risks (relative, absolute, NNT) for conditions surgeries treat
eMethods
eResults