Key Points
Question
Are medical and adult-use marijuana laws passed after 2010 associated with lower rates of opioid prescribing for Medicaid enrollees?
Findings
In this population-based, cross-sectional study using the all-capture Medicaid prescription data for 2011 to 2016, medical marijuana laws and adult-use marijuana laws were associated with lower opioid prescribing rates (5.88% and 6.38% lower, respectively).
Meaning
Medical and adult-use marijuana laws have the potential to lower opioid prescribing for Medicaid enrollees, a high-risk population for chronic pain, opioid use disorder, and opioid overdose, and marijuana liberalization may serve as a component of a comprehensive package to tackle the opioid epidemic.
Abstract
Importance
Overprescribing of opioids is considered a major driving force behind the opioid epidemic in the United States. Marijuana is one of the potential nonopioid alternatives that can relieve pain at a relatively lower risk of addiction and virtually no risk of overdose. Marijuana liberalization, including medical and adult-use marijuana laws, has made marijuana available to more Americans.
Objective
To examine the association of state implementation of medical and adult-use marijuana laws with opioid prescribing rates and spending among Medicaid enrollees.
Design, Setting, and Participants
This cross-sectional study used a quasi-experimental difference-in-differences design comparing opioid prescribing trends between states that started to implement medical and adult-use marijuana laws between 2011 and 2016 and the remaining states. This population-based study across the United States included all Medicaid fee-for-service and managed care enrollees, a high-risk population for chronic pain, opioid use disorder, and opioid overdose.
Exposures
State implementation of medical and adult-use marijuana laws from 2011 to 2016.
Main Outcomes and Measures
Opioid prescribing rate, measured as the number of opioid prescriptions covered by Medicaid on a quarterly, per-1000-Medicaid-enrollee basis.
Results
State implementation of medical marijuana laws was associated with a 5.88% lower rate of opioid prescribing (95% CI, −11.55% to approximately −0.21%). Moreover, the implementation of adult-use marijuana laws, which all occurred in states with existing medical marijuana laws, was associated with a 6.38% lower rate of opioid prescribing (95% CI, −12.20% to approximately −0.56%).
Conclusions and Relevance
The potential of marijuana liberalization to reduce the use and consequences of prescription opioids among Medicaid enrollees deserves consideration during the policy discussions about marijuana reform and the opioid epidemic.
This population-based, cross-sectional study examines the association of state implementation of medical and adult-use marijuana laws with opioid prescribing rates and spending among Medicaid enrollees.
Introduction
Overprescribing of opioids for pain management is considered a major driving force behind the opioid epidemic in the United States1,2 A concerted policy effort has been made during the past decade to regulate opioid-prescribing practices.3 As access to prescription opioids becomes increasingly restricted, there is growing concern that restrictions on prescription opioids may have pushed those already addicted to opioids to seek more dangerous drugs and sources.4
The potential unintended consequences of restricting access to prescription opioids has shifted some policy attention to the development and use of nonopioid alternatives.5,6 Marijuana is one of the potential alternative drugs that can provide relief from pain at a relatively lower risk of addiction and virtually no risk of overdose.7,8,9 The therapeutic value of marijuana has been one of the central rationales behind the marijuana liberalization policies in many states that now allow marijuana use for medical and adult-use purposes.10 On the one hand, proponents of these medical and adult-use marijuana laws tout marijuana liberalization as a potential solution to the excessive use of opioids.5,6,10 Some opponents, on the other hand, view marijuana as a “gateway” or “stepping stone” to opioids and worry that marijuana liberalization may exacerbate the opioid epidemic.6,11
Although both medical and adult-use marijuana laws, in principle, have made marijuana available to more Americans, the laws targeted different groups and may have different opioid-related consequences. In medical marijuana laws, states typically specify a list of conditions that are eligible for medical marijuana, and most states have included in the list generic terms such as “severe pain,” “chronic pain,” or “intractable pain unrelieved by standard medical treatment and medications.” Patients with eligible conditions are expected to obtain recommendation from qualified physicians and enroll in a patient registry. Patients are then issued identification cards that allow them or their caregivers to possess a certain amount of marijuana through home cultivation and licensed dispensaries (in some states these are called “compassionate centers”).10 As a result, medical marijuana laws may have affected pain management for only a selected group of patients with pain and with state-specified eligible conditions, sources of care from licensed marijuana physicians, and ready access to marijuana.
Adult-use marijuana laws, which to date have been enacted only in states with existing medical marijuana systems, fundamentally restructured the distribution and possession of marijuana. Unlike the eligibility criteria and registry and/or renewal process under medical marijuana laws, adult-use marijuana laws permit all adults 21 years or older to use marijuana. Furthermore, marijuana supply channels have often been expanded through grow operations and retail dispensaries licensed and taxed by the states.10 Thus, adult-use marijuana laws enable individuals without eligibility or access to medical marijuana before such laws to use marijuana as self-medication for pain conditions. A potential repercussion of adult-use marijuana laws, however, is that the outright legalization/taxation message conveyed by the laws may encourage individuals to normalize the risky behaviors in general.12
Empirical studies on medical marijuana laws have indicated downstream policy effects on reducing opioid-related hospitalizations, opioid overdose deaths, and opioid-involved traffic fatalities.5,13,14 Furthermore, Bradford and Bradford15,16 found evidence that the implementation of medical marijuana laws reduced the number of prescriptions used to treat the conditions, including pain, which most states have deemed eligible for medical marijuana. However, the authors did not single out prescription opioids. The prescription opioids were aggregated with nonopioid analgesics and 9 other classes of drugs broadly classified as pain-related prescriptions (eg, antidepressants, muscle relaxants, respiratory inhalant products, functional bowel disorder agents).
Regarding adult-use marijuana laws, only 1 study to date has examined the policy effect on opioid-related health outcomes. Livingston and colleagues17 found an interrupted reversal of the upward trend in Colorado’s opioid overdose mortality when the state legalized adult-use marijuana use. No study to date has focused on the effect of medical and adult-use marijuana laws on opioid prescribing in particular.
We examined the opioid prescribing rates among Medicaid enrollees in the context of state marijuana liberalization policies between 2011 and 2016. During this period, an estimated one-third of opioid prescriptions were misused or abused, of which Medicaid shared a disproportionately large burden.18 In addition to opioid prescribing rates, we also studied Medicaid spending on prescription opioids, as well as the prescribing rates of, and spending on, nonopioid pain medications. As medical and adult-use marijuana laws continue to gather momentum in state legislatures, the study findings are informative for states’ implementation and iterations of marijuana reform as well as the nation’s fight against the opioid epidemic.
Methods
Data
This study was exempt from institutional review board review. The primary data source for this study was the State Drug Utilization Data from the Centers for Medicare and Medicaid Services (CMS).19 All states are required to report to CMS quarterly on the amount of all outpatient drug prescriptions covered by Medicaid fee-for-service and managed care in exchange for federal matching funds. We excluded a few observations from the study data owing to the inconsistency in state data reporting. The study sample includes 1059 state-quarter observations.
We used data from the first quarter of 2011 to the second quarter of 2016; 2011 is the first year in which state reporting of Medicaid managed care prescription data became mandatory and nearly complete under the Affordable Care Act (ACA) data collection requirements. The managed care data captures many high-risk low-income adult enrollees who recently gained Medicaid coverage under the expansion provisions of the ACA or the Section 1115 waiver. These low-income adults included in the recent expansion are shown to have disproportionately high risks for chronic pain, as well as opioid use disorder and overdose.20 Another reason behind our choice of the study window is that it minimizes the influence of some nationwide policies and guidelines that were in place before 2011 or were about to be announced in 2016. These major common changes include, but are not limited to, the 2010 OxyContin reformulation, the publication of 2 national guidelines for appropriate opioid prescribing in chronic pain management in 2009 and 2010, the Surgeon General’s warning letter about opioid crisis in 2016, and the Centers for Disease Control and Prevention (CDC) Guideline for Prescribing Opioids for Chronic Pain and the subsequent state laws aligned with the CDC guideline that limit the opioid prescribing duration.21,22,23,24,25
Measures
Our primary outcome of interest was the state-level opioid prescribing rate, defined as the number of opioid prescriptions that were primarily used for pain management and covered by Medicaid on a quarterly, per-1000-Medicaid-enrollee basis in each state. Each opioid product in the data was identified by a unique 11-digit, 3-segment National Drug Code (NDC) number. We classified opioid products into 2 categories based on the Controlled Substance Act scheduling: Schedule II opioids and Schedule III to V opioids. The Schedule II opioids are generally considered to have a higher addiction rate and overdose liability. Since October 2014, hydrocodone combination products have been rescheduled from Schedule III to Schedule II.26 Accordingly, we classified all hydrocodone combination products as Schedule II opioids throughout the entire study period. We excluded the opioid products that were primarily used for medication-assisted treatment of opioid use disorder and for conditions other than pain (eg, codeine-containing cough and cold medications). In addition to the main outcome of opioid prescribing rates, we also studied Medicaid spending on prescription opioids, as well as the prescribing rates of, and spending on, nonopioid pain medications. (See the Supplement for the detailed information on variable measurement.)
The key independent variables are an indicator for the implementation of medical marijuana laws and an indicator for the implementation of adult-use marijuana laws. The policy indicators were assigned a value of 1 for each full quarter subsequent to the effective date of the medical or adult-use marijuana law in a state, and a value of 0 for the premedical marijuana or pre–adult-use marijuana law quarters and for the comparison states. The medical marijuana law indicator captures the association between medical marijuana law implementation and opioid prescribing relative to no marijuana law. The adult-use marijuana law indicator captures the association between adult-use marijuana law implementation and opioid prescribing in the context of an existing medical marijuana law because no states without a medical marijuana law have adopted an adult-use marijuana law.
The 2 main policy indicators treat medical marijuana laws and adult-use marijuana laws as 2 homogeneous sets of laws between states and across time. Furthermore, we explored the heterogeneous policy effects using 12 separate indicators for 8 state medical marijuana laws and 4 state adult-use marijuana laws. The state-specific policy effects help provide further insights into the potential policy heterogeneity associated with differences in statutory language, enforcement experience, and policy environments across states.27 (See the Supplement for a summary of medical marijuana laws and adult-use marijuana laws.)
Statistical Analyses
We used a quasi-experimental difference-in-differences design, which is analogous to an adjusted pre-post trend difference analysis. In modeling this, we used a state and quarter fixed-effects approach that has commonly been used in multistate, multipolicy evaluations. This 2-way fixed-effects approach allows us to account for unobserved differences across states that were constant over time, as well as nation-wide secular trends that were correlated with prescription opioid use (eg, nationwide leveling off and gradual reduction in annual opioid prescribing rate, rising public awareness of the role of opioids in pain management and the role of buprenorphine in opioid use disorder treatment).28
All models were population-weighted and adjusted for state-level characteristics that varied over time and were correlated with prescription opioid use or the Medicaid system. Such covariates include overall physician supply, buprenorphine-waivered physician supply, general economic conditions, and concurrent state policies, such as prescription drug monitoring program adoption and mandates, pain clinic regulations, and Medicaid expansions. 95% Confidence intervals were derived from standard errors clustered by state to account for within-state serial correlation in a difference-in-differences design. We performed 2 sets of sensitivity analyses: first, we included group-specific linear trends at the US Census Division level to account for the unobserved US Census Division–wide confounding factors that evolve over time at a constant rate; second, we excluded the states with medical and adult-use marijuana laws in place before 2011 from the comparison states. Furthermore, we performed “parallel-trend assumption” tests by statistically and graphically comparing the prepolicy trends between medical marijuana states, adult-use marijuana states, and the comparison states. We also performed falsification tests by examining the policy effects on 3 classes of drugs prescribed for conditions that were unlikely to be affected by marijuana use or marijuana liberalization policies. These sensitivity analyses and statistically checks can be found in the Supplement.
Results
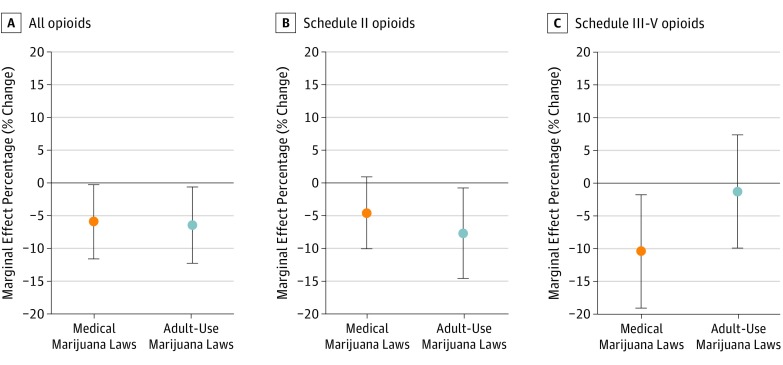
Figure 1 indicates that state implementation of medical and adult-use marijuana laws was associated with a lower Medicaid-covered opioid prescribing rate. Specifically, the implementation of medical marijuana laws was associated with a 5.88% lower rate of Medicaid-covered prescriptions for all opioids (95% CI, −11.55% to approximately −0.21%). Given that the annual rate of Medicaid-covered opioid prescriptions is on average 670.16 per 1000 enrollees in states without medical marijuana laws, the effect size of medical marijuana laws is equivalent to 39.41 fewer opioid prescriptions per 1000 enrollees per year. Moreover, when states with existing medical marijuana laws implemented adult-use marijuana laws, the implementation of adult-use marijuana laws was associated with an additional 6.38% lower opioid prescription rate (95% CI, −12.20% to approximately −0.56%). Using the annual average in states with medical marijuana laws but no adult-use marijuana laws (ie, 621.82 opioid prescriptions per 1000 enrollees), the effect size of adult-use marijuana laws can be translated to 39.67 fewer opioid prescriptions per 1000 enrollees per year. Furthermore, the estimated lower rate of opioid prescribing associated with adult-use marijuana laws was mainly concentrated in Schedule II opioids (−7.79%; 95% CI, −14.73% to approximately −0.85%), whereas the lower prescribing rate associated with medical marijuana laws was more pronounced in Schedule III to V opioids (−10.40%; 95% CI, −19.05% to approximately −1.74%).
Figure 1. Association Between Medical and Adult-Use Marijuana Laws and Medicaid-Covered Opioid Prescribing Rate.
Analysis of the CMS State Drug Utilization Data, 2011-2016.19 Opioid prescribing rate was measured by the number of Medicaid-covered prescriptions for opioids on a quarterly, per-1000-Medicaid-enrollees basis and was population-weighted. Error bars indicate 95% CIs clustered at the state level. Orange dots indicate prescribing rates under medical marijuana laws; gray dots, rates under adult-use marijuana laws.Rates and 95% CIs are also presented in eTables 3, 5, and 6 in the Supplement.
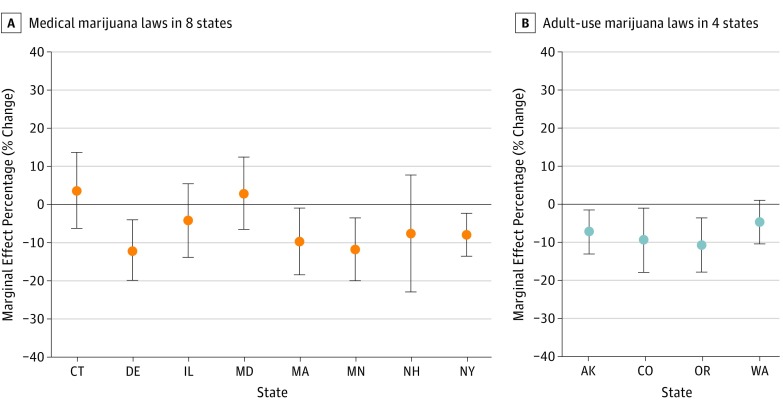
The state-specific policy effects presented in Figure 2 reveal a more nuanced picture. Among the 8 states that started to implement medical marijuana laws during the study period, Delaware, Massachusetts, Minnesota, and New Hampshire had significant lower opioid prescribing rates, whereas the plausible differences in opioid prescribing rates in Illinois and New Hampshire were not precisely estimated. Connecticut and Maryland, however, did not have clinically meaningful or statistically discernable changes in opioid prescribing rates associated with the implementation of medical marijuana laws.
Figure 2. State-Specific Association Between Medical and Adult-Use Marijuana Laws and Medicaid-Covered Opioid Prescribing Rate.
Analysis of the CMS State Drug Utilization Data, 2011-2016.19 Opioid prescribing rate was measured by the number of Medicaid-covered prescriptions for opioids on a quarterly, per-1000-Medicaid-enrollees basis and was population-weighted. Error bars indicate 95% CIs clustered at the state level. Dots indicate prescribing rates. Rates and 95% CIs are also presented in eTable 4 in the Supplement. AK indicates Alaska; CO, Colorado; CT, Connecticut; DE, Delaware; IL, Illinois; MA, Massachusetts; MD, Maryland; MN, Minnesota; NH, New Hampshire; NY, New York; OR, Oregon; WA, Washington.
Regarding the adult-use marijuana states, 3 of the 4 states (ie, Alaska, Colorado, and Oregon) had significantly lower opioid prescribing rates associated with the implementation of adult-use marijuana laws, whereas the change in Washington was relatively moderate.
Furthermore, the implementation of adult-use marijuana laws was associated with a 9.78% lower Medicaid spending on prescription opioids (95% CI, −18.29% to approximately −1.26%), equivalent to an annual saving of $1815 Medicaid spending per 1000 enrollees (Table). The implementation of medical and adult-use marijuana laws was also associated with a lower rate of Medicaid-covered prescriptions for nonopioid pain medications of 8.36% (95% CI, −13.67% to approximately −3.05%) and 8.69% (95% CI, −15.50% to approximately −1.89%), respectively (Table).
Table. Association Between Medical and Adult-Use Marijuana Laws and Medicaid-Covered Prescribing Rate of and Spending on Pain Medicationsa.
| Medication Type | Prescriptions, No. | Cost, $ | ||
|---|---|---|---|---|
| Relative Change, % (95% CI) | Absolute Annual Effect Size per 1000 Enrollees | Relative Change, % (95% CI) | Absolute Annual Effect Size per 1000 Enrollees | |
| All opioid pain medications | ||||
| Medical marijuana laws | −5.88 (−11.55 to −0.21) | −39.41 | −2.87 (−8.16 to 2.42) | … |
| Adult-use marijuana laws | −6.38 (−12.20 to −0.56) | −39.67 | −9.78 (−18.29 to −1.26) | −1815.5 |
| Schedule II opioids | ||||
| Medical marijuana laws | −4.69 (−10.05 to 0.67) | −24.56 | −2.11 (−9.45 to 5.12) | … |
| Adult-use marijuana laws | −7.79 (−14.73 to −0.85) | −36.48 | −11.93 (−21.26 to −2.60) | −1916.4 |
| Schedule III-V opioids | ||||
| Medical marijuana laws | −10.40 (−19.05 to −1.74) | −15.14 | −14.27 (−32.20 to 3.75) | … |
| Adult-use marijuana laws | −1.36 (−12.93 to 10.21) | … | 0.39 (−8.55 to 9.33) | … |
| Nonopioid pain medications | ||||
| Medical marijuana laws | −8.36 (−13.67 to −3.05) | −105.36 | −3.92 (−9.28 to 1.44) | … |
| Adult-use marijuana laws | −8.69 (−15.50 to −1.89) | −95.65 | −9.85 (−21.85 to 2.15) | … |
Abbreviation: ellipses, not significant at the .05 level.
Analysis of the Centers for Medicare and Medicaid State Drug Utilization Data, 2011-2016.19 The opioid prescribing rate was measured by the number of Medicaid-covered prescriptions for opioids and nonopioid pain medications on a quarterly, per-1000-Medicaid-enrollees basis and were population-weighted; the nominal spending values between 2011 and 2016 were converted to real values based on national monthly Consumer Price Index.
Results from sensitivity analyses were consistent with the main findings. Moreover, the “parallel-trend assumption” tests and falsification tests lent weight to the validity of the methods (Supplement).
Discussion
This study provides some of the first empirical evidence that the implementation of medical and adult-use marijuana laws from 2011 to 2016 was associated with lower Medicaid-covered opioid prescribing rates and spending. The study findings are consistent with those of Bradford and Bradford,15,16 who found reductions in broad category of pain prescriptions covered by Medicaid associated with medical marijuana laws. Our focus on opioids specifically is important in the context of the current epidemic. Furthermore, we also found that implementation of adult-use marijuana laws was associated with even lower rates of opioid prescribing, which previously had not been investigated.
Most opioid use disorder and overdose cases occurred in patients with legitimate prescriptions from health care professionals for pain management.29 Marijuana liberalization, therefore, may have benefited these patients by providing them with legal protection and access to marijuana as an alternative relief from their pain conditions.7,8 According to the 2017 Yahoo News/Marist Poll,30 83% of Americans supported legalizing marijuana for medical purpose. The widespread public support will bring medical marijuana laws to more and more states for years to come, which may help decrease the use of prescription opioids in pain management and the adverse consequences, such as opioid use disorder and overdose. Furthermore, emerging evidence suggests that marijuana may help ease opioid withdrawal symptoms.31 Thus, marijuana liberalization potentially reduced prescription opioid use on 2 fronts, serving as a substitute for opioid pain medications, and as a complement to opioid use disorder treatment.
When exploring the policy heterogeneity across states, we identified 2 states, Connecticut and Maryland, where the medical marijuana laws had much less effect on opioid prescribing. There are some possible explanations for these 2 notable exceptions. First, Connecticut did not list any pain conditions as eligible conditions for medical marijuana during the study period (included only “complex regional pain syndrome,” a very uncommon chronic pain condition, as one of the extended eligible conditions in late 2016). Second, Maryland, despite the law going into effect in June 2014, did not have an operational medical marijuana system in place until late 2016 owing to multiple legal disputes and bureaucratic challenges.
Furthermore, the association between adult-use marijuana laws and lower prescription opioid rate and spending are worth noting. Because states with adult-use marijuana laws all had medical marijuana laws in place before the implementation of adult-use marijuana laws, the further reductions in opioid prescribing associated with the newly implemented adult-use marijuana laws suggest that there were individuals beyond the reach of medical marijuana laws who may also benefit from using marijuana in lieu of opioids. Our finding that the lower opioid prescribing rates associated with adult-use marijuana laws were pronounced in Schedule II opioids, further suggest that reaching these individuals may have greater potential to reduce the adverse consequences, such as opioid use disorder and overdose. The 2017 Gallup Poll shows a record high 64% of Americans in favor of adult-use marijuana laws.32 Four of the 5 ballot initiatives for adult-use marijuana were passed on the 2016 Election Day alone.10 In 2018, more states with existing medical marijuana laws may vote on adult-use marijuana bills. The potential of adult-use marijuana laws to reduce the use and consequences of addictive opioids deserves consideration, especially in states that have been hit hard by the opioid epidemic. As for the states currently reluctant to consider the outright legalization of adult-use marijuana and those still debating medical marijuana, policy efforts can still be made in legislation and implementation process to extend the availability of marijuana to more people who may benefit from the therapeutic value of marijuana.
Limitations
This study is subject to the following limitations. First, the aggregate nature of the study data did not allow us to identify opioid prescriptions for individual Medicaid enrollees or individual patients treated for pain. Thus, we cannot distinguish between changes on the extensive margin (ie, the number of individuals with any opioid prescription) and the changes on the intensive margin (ie, the number of prescriptions to those already been prescribed opioids). Another limitation of this state-level study lies in that inferences about individual-level mechanisms can only be deduced from the inference for states to which the individuals belong. Second, the data lack the necessary information to adjust our measures of prescription counts for the variations in dosage and strength or to convert the prescription counts into more standardized values, such as morphine milligram equivalents. Third, the geographic proximity and cultural similarity between states with medical or adult-use marijuana laws and those without such laws suggests that the laws were not likely to be “randomly assigned” to states. Thus, as with any observational study, we cannot definitively establish causality between marijuana liberalization and opioid prescribing.
Conclusions
These findings suggest that medical and adult-use marijuana laws have the potential to reduce opioid prescribing for Medicaid enrollees, a segment of population with disproportionately high risk for chronic pain, opioid use disorder, and opioid overdose.20 Nonetheless, marijuana liberalization alone cannot solve the opioid epidemic. As with other policies evaluated in the previous literature, marijuana liberalization is but one potential aspect of a comprehensive package to tackle the epidemic.33
eTable 1. Descriptive Statistics of Study Variables Weighted by State Population
eTable 2. Effective Dates & Dispensary Status of Medical Marijuana Laws & Adult-Use Marijuana Laws between 2011 and 2016
eMethods. Variable Measurement & Model Specifications
eTable 3. Estimated Effect of Medical Marijuana Laws & Adult-Use Marijuana Laws on Medicaid-Covered Prescription Rate of & Spending on All Opioid Pain Medications
eTable 4. Estimated State-Specific Effects of Medical Marijuana Laws & Adult-Use Marijuana Laws on Medicaid-Covered Prescription Rate of & Spending on All Opioid Pain Medications
eTable 5. Estimated Effect of Medical Marijuana Laws & Adult-Use Marijuana Laws on Medicaid-Covered Prescription Rate of & Spending on Schedule II Opioid Pain Medications
eTable 6. Estimated Effect of Medical Marijuana Laws & Adult-Use Marijuana Laws on Medicaid-Covered Prescription for & Spending on Schedule III-V Opioid Pain Medications
eTable 7. Estimated Effect of Medical Marijuana Laws & Adult-Use Marijuana Laws on Medicaid-Covered Prescription Rate of & Spending on Non-Opioid Pain Medications
eTable 8. Tests for Pre-Policy Trend Differences of Medicaid-Covered Prescription for & Spending on Opioid and Non-Opioid Pain Medications between Medical Marijuana States & Comparison States, & between Adult-Use Marijuana States & Comparison States
eFigure. Trend Comparisons of Medicaid-Covered Prescription for & Spending on Opioid and Non-Opioid Pain Medications between Medical Marijuana States, Adult-Use Marijuana States & Comparison States
eTable 9. Sensitivity Analyses of Effects of Medical Marijuana Laws & Adult-Use Marijuana Laws on Medicaid-Covered Opioid Pain Medication Prescribing Rate
eTable 10. Falsification Analyses of Effects of Medical Marijuana Laws & Adult-Use Marijuana Laws on Medicaid-Covered Prescribing Rates of Blood Thinning Agents, Influenza Antiviral Drugs, and Antibiotics
References
- 1.Bohnert AS, Valenstein M, Bair MJ, et al. . Association between opioid prescribing patterns and opioid overdose-related deaths. JAMA. 2011;305(13):1315-1321. [DOI] [PubMed] [Google Scholar]
- 2.Volkow ND. America’s addiction to opioids: heroin and prescription drug abuse. Washington, DC: Senate Caucus on International Narcotics Control. May 14, 2014. https://www.drugcaucus.senate.gov/sites/default/files/Volkow%20Testimony.pdf. Accessed July 12, 2017.
- 3.Dowell D, Zhang K, Noonan RK, Hockenberry JM. Mandatory provider review and pain clinic laws reduce the amounts of opioids prescribed and overdose death rates. Health Aff (Millwood). 2016;35(10):1876-1883. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Cicero TJ, Ellis MS, Surratt HL, Kurtz SP. The changing face of heroin use in the United States: a retrospective analysis of the past 50 years. JAMA Psychiatry. 2014;71(7):821-826. [DOI] [PubMed] [Google Scholar]
- 5.Bachhuber MA, Saloner B, Cunningham CO, Barry CL. Medical cannabis laws and opioid analgesic overdose mortality in the United States, 1999-2010. JAMA Intern Med. 2014;174(10):1668-1673. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Wilkinson ST, Yarnell S, Radhakrishnan R, Ball SA, D’Souza DC. Marijuana legalization: impact on physicians and public health. Annu Rev Med. 2016;67:453-466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lynch ME, Campbell F. Cannabinoids for treatment of chronic non-cancer pain; a systematic review of randomized trials. Br J Clin Pharmacol. 2011;72(5):735-744. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Hill KP. Medical marijuana for treatment of chronic pain and other medical and psychiatric problems: a clinical review. JAMA. 2015;313(24):2474-2483. [DOI] [PubMed] [Google Scholar]
- 9.National Academies of Sciences, Engineering, and Medicine The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. Washington, DC: National Academies Press; 2017. [PubMed] [Google Scholar]
- 10.National Conference of State Legislation (NCSL). Deep Dive: Marijuana. Denver, CO: National Conference of State Legislation. 2016. http://www.ncsl.org/bookstore/state-legislatures-magazine/marijuana-deep-dive.aspx. Accessed July 12, 2017.
- 11.Lynskey MT, Heath AC, Bucholz KK, et al. . Escalation of drug use in early-onset cannabis users vs co-twin controls. JAMA. 2003;289(4):427-433. [DOI] [PubMed] [Google Scholar]
- 12.Hathaway AD, Comeau NC, Erickson PG. Cannabis normalization and stigma: contemporary practices of moral regulation. Criminol Crim Justice. 2011;11(5):451-469. doi.org/ 10.1177/1748895811415345 [DOI] [Google Scholar]
- 13.Shi Y. Medical marijuana policies and hospitalizations related to marijuana and opioid pain reliever. Drug Alcohol Depend. 2017;173:144-150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kim JH, Santaella-Tenorio J, Mauro C, et al. . State medical marijuana laws and the prevalence of opioids detected among fatally injured drivers. Am J Public Health. 2016;106(11):2032-2037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bradford AC, Bradford WD. Medical marijuana laws reduce prescription medication use in Medicare part D. Health Aff (Millwood). 2016;35(7):1230-1236. [DOI] [PubMed] [Google Scholar]
- 16.Bradford AC, Bradford WD. Medical marijuana laws may be associated with a decline in the number of prescriptions for Medicaid enrollees. Health Aff (Millwood). 2017;36(5):945-951. [DOI] [PubMed] [Google Scholar]
- 17.Livingston MD, Barnett TE, Delcher C, Wagenaar AC. Recreational cannabis legalization and opioid-related deaths in Colorado, 2000-2015. Am J Public Health. 2017;107(11):1827-1829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Castlight Health. The opioid crisis in America’s workforce. San Francisco, CA: Castlight Health Inc; 2016. http://content.castlighthealth.com/Opioid-Research-Report_LP.html. Accessed July 12, 2017.
- 19.Center for Medicaid and CHIP Services Medicaid drug programs data and resources. Baltimore, MD: Centers for Medicare and Medicaid Services (CMS); 2017. http://www.medicaid.gov/medicaid-chip-program-information/by-topics/benefits/prescription-drugs/medicaid-drug-programs-data-and-resources.html. Accessed July 12, 2017.
- 20.Han B, Compton WM, Jones CM, Cai R. Nonmedical prescription opioid use and use disorders among adults aged 18 through 64 years in the United States, 2003-2013. JAMA. 2015;314(14):1468-1478. [DOI] [PubMed] [Google Scholar]
- 21.Cicero TJ, Ellis MS. Abuse-deterrent formulations and the prescription opioid abuse epidemic in the United States: lessons learned from OxyContin. JAMA Psychiatry. 2015;72(5):424-430. [DOI] [PubMed] [Google Scholar]
- 22.Chou R, Fanciullo GJ, Fine PG, et al. ; American Pain Society-American Academy of Pain Medicine Opioids Guidelines Panel . Clinical guidelines for the use of chronic opioid therapy in chronic noncancer pain. J Pain. 2009;10(2):113-130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.US Department of Veterans Affairs VA/DoD clinical practice guidelines: management of opioid therapy (OT) for chronic pain. Washington, DC: US Department of Veterans Affairs (VA); 2010. https://www.healthquality.va.gov/guidelines/Pain/cot/. July 12, 2017.
- 24.Murthy VH. Letter From the Surgeon General. Washington, DC: Office of the Surgeon General, U.S. Department of Health and Human Services (HHS); August 25, 2016. https://turnthetiderx.org/. Accessed July 12, 2017.
- 25.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain—United States, 2016. JAMA. 2016;315(15):1624-1645. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kuehn BM; FDA committee . FDA committee: more restrictions needed on hydrocodone combination products. JAMA. 2013;309(9):862. [DOI] [PubMed] [Google Scholar]
- 27.Pacula RL, Powell D, Heaton P, Sevigny EL. Assessing the effects of medical marijuana laws on marijuana use: the devil is in the details. J Policy Anal Manage. 2015;34(1):7-31. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Wooldridge JM. Econometric Analysis of Cross Section and Panel Data. Cambridge, MA: MIT Press; 2010. [Google Scholar]
- 29.Volkow ND, McLellan AT. Opioid abuse in chronic pain—misconceptions and mitigation strategies. N Engl J Med. 2016;374(13):1253-1263. [DOI] [PubMed] [Google Scholar]
- 30.Marist College Institute for Public Opinion Yahoo News/Marist Poll Weed & the American family. Poughkeepsie, NY: Marist College Institute for Public Opinion; 2017. http://maristpoll.marist.edu/yahoo-newsmarist-poll/. Accessed February 7, 2018.
- 31.Ren Y, Whittard J, Higuera-Matas A, Morris CV, Hurd YL. Cannabidiol, a nonpsychotropic component of cannabis, inhibits cue-induced heroin seeking and normalizes discrete mesolimbic neuronal disturbances. J Neurosci. 2009;29(47):14764-14769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McCarthy J. Record-high support for legalizing marijuana use in U.S. Washington, DC: Gallup News; 2017. http://news.gallup.com/poll/221018/record-high-support-legalizing-marijuana.aspx. Accessed November 29, 2017.
- 33.Kolodny A, Courtwright DT, Hwang CS, et al. . The prescription opioid and heroin crisis: a public health approach to an epidemic of addiction. Annu Rev Public Health. 2015;36:559-574. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eTable 1. Descriptive Statistics of Study Variables Weighted by State Population
eTable 2. Effective Dates & Dispensary Status of Medical Marijuana Laws & Adult-Use Marijuana Laws between 2011 and 2016
eMethods. Variable Measurement & Model Specifications
eTable 3. Estimated Effect of Medical Marijuana Laws & Adult-Use Marijuana Laws on Medicaid-Covered Prescription Rate of & Spending on All Opioid Pain Medications
eTable 4. Estimated State-Specific Effects of Medical Marijuana Laws & Adult-Use Marijuana Laws on Medicaid-Covered Prescription Rate of & Spending on All Opioid Pain Medications
eTable 5. Estimated Effect of Medical Marijuana Laws & Adult-Use Marijuana Laws on Medicaid-Covered Prescription Rate of & Spending on Schedule II Opioid Pain Medications
eTable 6. Estimated Effect of Medical Marijuana Laws & Adult-Use Marijuana Laws on Medicaid-Covered Prescription for & Spending on Schedule III-V Opioid Pain Medications
eTable 7. Estimated Effect of Medical Marijuana Laws & Adult-Use Marijuana Laws on Medicaid-Covered Prescription Rate of & Spending on Non-Opioid Pain Medications
eTable 8. Tests for Pre-Policy Trend Differences of Medicaid-Covered Prescription for & Spending on Opioid and Non-Opioid Pain Medications between Medical Marijuana States & Comparison States, & between Adult-Use Marijuana States & Comparison States
eFigure. Trend Comparisons of Medicaid-Covered Prescription for & Spending on Opioid and Non-Opioid Pain Medications between Medical Marijuana States, Adult-Use Marijuana States & Comparison States
eTable 9. Sensitivity Analyses of Effects of Medical Marijuana Laws & Adult-Use Marijuana Laws on Medicaid-Covered Opioid Pain Medication Prescribing Rate
eTable 10. Falsification Analyses of Effects of Medical Marijuana Laws & Adult-Use Marijuana Laws on Medicaid-Covered Prescribing Rates of Blood Thinning Agents, Influenza Antiviral Drugs, and Antibiotics