Key Points
Question
Can a gracilis muscle flap be designed as a compound flap with multiple paddles for multivector reanimation after facial paralysis, and what effect does this design have on the smile display zone?
Findings
In this prospective cohort study of 12 patients who underwent facial reanimation for complete paralysis, the gracilis flap was reliably designed and transplanted as a functional double paddle muscle flap for a multivector facial reanimation. The multivector design resulted in statistically significant improvement in the dental display, smile width, and correction of paralytic labial drape.
Meaning
Designing the gracilis flap as a multivector gracilis flap with 2 or more paddles is an effective way of improving all components of the smile display zone and has the potential for restoring a Duchene-type smile in patients with facial paralysis.
This cohort study analyzes use of a double-paddle multivector gracilis flap for treatment of patients with complete facial paralysis.
Abstract
Importance
A multivector functional muscle flap that closely simulates the biomechanical effects of facial muscle groups is essential for complete smile restoration after facial paralysis.
Objective
To determine the feasibility of a multivector gracilis muscle flap design for reanimation after facial paralysis and to analyze the effect on the smile display zone.
Design, Setting, and Participants
Prospective analysis of patients who underwent a double paddle multivector gracilis flap for complete facial paralysis between June 2015 and December 2016 was carried out in a tertiary hospital.
Interventions
The gracilis muscle was harvested as a double paddle flap and inserted along 2 vectors for facial reanimation.
Main Outcomes and Measures
The primary outcome measures were: (1) dental display (the number of maxillary teeth displayed on paralyzed vs normal sides), (2) exposed maxillary gingival scaffold width, (3) interlabial gap at midline and canine, (4) facial asymmetry index (FAI), and (5) dynamic periorbital wrinkling.
Results
There were 10 women and 2 men between ages 20 and 64 years (mean [SD], 46 [15] years). Five flaps were reinnervated with facial and masseteric nerves, 5 with masseteric nerve only, and 2 with crossfacial nerve only. There was functional muscle recovery in all cases. On average there was additional 3.1 maxillary teeth exposed posttreatment when smiling (5.5 vs 8.6; CI, 7.9 to 16.6; P < .001). The mean exposed maxillary gingival scaffold width improved from 31.5 mm to 43.7 mm (95% CI, 1.9 to 4.3; P < .001). There was no significant difference in interlabial exposure at midline (7.1 mm vs 7.7 mm; CI, −1.5 to 2.7; P = .56) but a 56.4% improvement at the level of the canines (3.9 vs 6.1; CI, 0.1 to 4.3; P = .04). The mean FAI when smiling was reduced from 9.1 mm to 4.5 mm (CI, −8.0 to −1.2; P = .01). Dynamic wrinkling of the periorbital area with smiling was noted in 4 patients.
Conclusions and Relevance
The gracilis flap can be reliably designed as a functional double paddle muscle flap for a multivector facial reanimation. The multivector gracilis flap design is effective in improving all components of the smile display zone and has the potential for producing periorbital-wrinkling characteristic of a Duchenne smile.
Level of Evidence
4.
Introduction
The power of a smile is in its ability to engender feelings of happiness and positivity. The smile has been rated as the facial expression with the highest positive emotional substance and has been shown to reduce stress.1 However, not all smiles are equal in their emotional content and social impression. A genuine enjoyment smile (Duchenne smile), is a positive display of facial emotion characterized by upper lip and oral commissure elevation in tandem with periocular wrinkling.2 Electroencephalographic data has shown that Duchenne smiles increase activity in the left anterior temporal brain; an area connected with positivity.3 Duchenne smiles result from strong action of the upper lip elevators that maximally expose the dental display zone (Figure 1A). In contrast, a social smile is a posed, strained, or fake smile elicited mainly from the corners of the mouth with suppressed dental display. Social smiles result mostly from outward contraction of the zygomaticus major muscle with limited effect of other upper lip elevators. Social smiles have little emotional output.2 The illusionary contracted oral commissure in Leonardo da Vinci’s Mona Lisa painting is an example of a social smile. The Mona Lisa smile portrays symmetric lateral commissure contraction with little or no dental display.
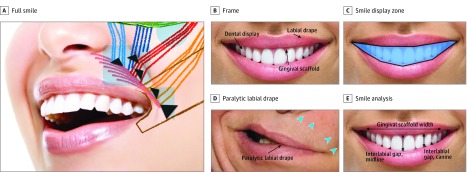
Figure 1. The Anatomy of a Smile .
A, A full smile is the result of a multivector (black arrowheads) and multizonal action (blue triangle, square, and circle zones) of the smile muscles. Upper lip and commissure elevation results from muscle action within the square and triangular zones respectively, and periorbital wrinkling in the circular zone. B, The upper and lower lip frames the smile display zone. In this framework are the components of a smile including the gingival scaffold and displayed teeth. C, The smile display zone. D, The paralyzed upper lip drapes over the smile display zone obscuring the gingival scaffold and limiting dental display. Correction of the paralytic labial drape requires a multivector muscle action (blue arrowheads). E, The horizontal and vertical components of the smile display zone can be analyzed by measuring the maximal gingival scaffold width and interlabial gap at the midline and between the canines.
The neuromuscular circuit and processes that produce a smile are complex and include orders of motor neurons interacting with other neurons inputting emotional signals. The end organs in this complex pathway are the facial muscles. In longstanding facial paralysis, irreversible degeneration of the facial muscles occur and the ability for normal facial expression is impaired. Paralysis of the zygomaticus major muscle results in the drooping of the oral commissure. Paralysis of the levator labii muscles result in draping of the upper lip over the maxillary dentition obscuring the smile display zone. The lack of wrinkling around the paralyzed eyelid takes the sparkle out of a smile. The inability to smile and the associated facial distortion that occurs in facial paralysis exacts significant social penalties that can lead to depression.4 These social and emotional penalties can be reversed with facial reanimation surgery.4,5
When facial muscles are irreversibly injured, smile restoration requires the transfer of new functional muscle units that mimic the function of the paralyzed facial muscles. Functional muscles may be transferred as pedicled regional muscle tendon unit (MTU) flaps (eg, temporalis tendon transfer) or as free functional muscle flaps (FFMF) (eg, gracilis flap). Compared with pedicled MTU flaps, FFMFs are more versatile. The gracilis flap is a common FFMF used in contemporary facial reanimation surgery for smile restoration. As a substitute donor muscle, the gracilis muscle has parallel muscle fiber pennation similar to facial muscles and adequate force generation and excursion for smile restoration. However, the gracilis muscle is a bulky muscle with a comparatively larger physiologic cross-sectional area (PCSA) than the smile muscles, and thus requires secondary modifications during flap harvest and insertion. The gracilis flap is commonly designed as a single paddle with univector excursion often mimicking the outward contraction of the zygomaticus major muscle. The smile from of a single vector contraction is more likely to consistently produce a Mona Lisa smile limited in the degree of lip elevation and dental display and lacking in any periorbital animation. To restore a Duchenne type smile for patients with facial paralysis, it is necessary to refine the current design and application of the gracilis flap for facial reanimation. In this study, we present our experience with a double paddle multivector gracilis flap design and insertion for smile restoration after facial paralysis.
The Smile Display Zone
A smile is a dynamic process that displays teeth and gingiva as a result of lip movement. These displayed components comprise the smile display zone. The upper and lower lips frame the smile display zone within which rests the teeth and gingival scaffold. (Figure 1B and C) The different types of smile (cuspid, social, Mona Lisa), a reflection of the extent to which the smile display zone is exposed, depend on the vector and degree of lip excursion (Figure 1). In facial paralysis, the paralyzed lip drapes and obscures the teeth and gingival scaffold in the smile display zone (Figure 1D). The effectiveness of a reanimation procedure may be analyzed by determining the recovery of maxillary anterior teeth display, lip drape, and gingival scaffold display (Figure 1E).
Anatomic Basis for 2-Paddle Multivector Gracilis Flap Design
The gracilis muscle is a type II muscle based on the schema of Mathes and Nahai.6 The dominant arterial supply originates from the profunda femoris vessels and passes between the adductor longus and adductor brevis before entering the muscle hilum 8 to 10 cm from its ischiopubic attachment. Venous drainage is through paired venae commitantes. The dominant pedicle divides on entering the gracilis muscle, passing proximally and distally, parallel to the longitudinal muscle fibers.7 The motor nerve arises from the obturator nerve and enters the muscle in association with the dominant vascular pedicle. In the muscle, the nerve splits and runs longitudinally in 2 or 3 major branches parallel to the arterial branches and muscle fibers. The parallel muscle fiber architecture and the longitudinal neurovascular arrangement render the gracilis muscle suitable for functional segmental harvest and transfer.
Methods
Design, Settings, Participants
Twelve consecutive patients who underwent a double paddle multivector gracilis flap for complete facial paralysis between June 2015 and December 2016 were analyzed for this study. Patients who underwent a similar procedure for partial paralysis were excluded. The Johns Hopkins institutional review board approved this study and written informed consent was obtained. Participants were not compensated.
Smile Analysis
The dynamic smile display zone before and after the multivector gracilis flap were compared. The preoperative and post-operative smile display zones were captured using standardized digital videographic measurements adapted from the orthodontic literature8 (Figure 1A-E). Primary measures included: (1) dental display (the number of maxillary teeth displayed on both sides of midline recorded as a ratio of the number of teeth on the paralyzed side [x] to the number of teeth on the nonparalyzed side [y]), (2) width of visible maxillary gingival scaffold, (3) interlabial gap measured as the distance between the upper and lower lip margins at midline and canine, (4) and Facial Asymmetry Index (FAI). The FAI during smile, a measure of the symmetry of the oral commissure, was determined using measurement of standardized points between the affected and nonaffects sides as previously described.9 The distance between the medial canthus to the ipsilateral oral commissure was measured on the paralyzed and nonparalyzed sides. The difference was recorded as the FAI. An FAI of 1 mm depicts a difference of 1 mm between the oral commissure positions. Videographic analysis and measurements were performed using the Canfield Mirror imaging software (version 7.4, Canfield scientific). The measurements were calibrated to millimeters using the standardized corneal white-to-white diameter as a reference for all measurements. The presence or absence of dynamic lateral periorbital wrinkling when smiling was recorded.
Patient Preparation and Surgical Planning
The pattern of the patient’s smile is marked to show the vector of upward upper lip elevation and oral commissure contraction. By manually elevating the paralyzed upper lip, we determine and mark the ideal insertion sites and vector of pull necessary to achieve equal dental show. A video of the patient’s smile is captured and played in the operating room for reference throughout the case. Measurements taken from the normal side help determine and outline the desired length and vector of the muscle segments (Figure 2). The procedure is performed without any paralytic agents.
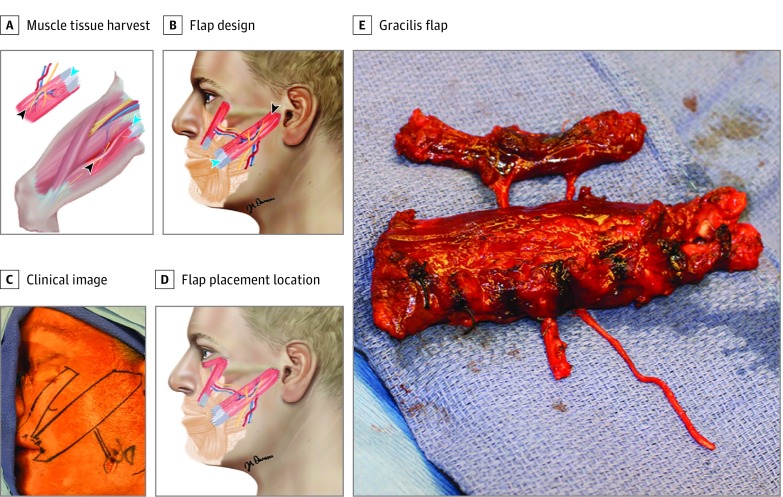
Figure 2. Design and Insertion of the Multivector Gracilis Flap .
A, A right-sided gracilis flap designed for a left-sided paralysis. The tendinous segment (blue arrowheads) was inserted into the orbicular oris and the distal end (black arrowheads) fixated to the periosteum of the malar bone and zygoma. The primary (larger) muscle paddle was harvested from the anterior aspect of the gracilis muscle and the secondary (smaller) paddle from the posterior aspect. Image copyright www.dnaillustrations.com. B, Two divergent muscle vectors simulating the function of the zygomaticus and levator labii muscles. C, Outline of planned muscle insertion. D, Design of 3-paddle multivector gracilis flap. E, The gracilis flap is harvested as a free functional composite flap with 2 isolated muscle paddles connected by a common-source neurovascular pedicle.
Muscle Harvest
We typically harvest a right-sided gracilis flap for a paralyzed left face and vice versa (Figure 2A and B). This naturally aligns the graciis pedicle with the facial artery and vein and the tendinous portion of the muscle with the lip. Harvesting the gracilis flap from the ipsilateral side is also feasible. The gracilis muscle belly and neurovascular pedicle is exposed and dissected in a typical fashion. To determine and guide the optimal length- tension relationship, marking sutures are placed on the gracilis surface at measured intervals prior to dividing the muscle. This is a rough guide to reestablishing the ideal sarcomere length for optimal force generation. The primary muscle belly (approximately 2.5 to 3 cm wide) is harvested from the anterior third of the muscle and the secondary belly (approximately 1 to 1.5 cm wide) from the posterior third. The central intervening muscle segment is carefully resected around a bridging neurovascular pedicle. A small cuff of muscle may be preserved around the bridging pedicle. The 2 muscle bellies are dissected and separated in situ with the aid of a Doppler and nerve stimulator. The muscle is reduced in thickness as needed. We are careful to maintain a layer of myomysium and gliding fascia around the harvested muscle. At the end of the dissection the 2 muscle bellies can be independently oriented (Figure 2E). Doppler signals to each segment and independent muscle contraction are verified (Video).
Video. Double Paddle Multivector Gracilis Flap for Facial Reanimation.
Preparation of the Recipient Bed
The incision to expose and prepare the recipient bed is typically a modified facelift incision. A relaxing temporal hair tuft incision facilitates exposure of the subzygomatic triangle for mobilization of the masseteric nerve, exposure of the malar eminence, zygomatic arch and temporalis fascia for flap fixation.10 The surgical bed is infiltrated with 1:100 000 epinephrine solution. A skin flap is elevated in a subcutaneous musculoaponeurotic system (subSMAS) plane extending beyond the melolabial fold to expose the orbicularis oris muscle. When a crossfacial nerve has been previously placed, it is identified and preserved during flap elevation. When a masseteric nerve innervation is planned, the nerve is identified and mobilized in the subzygomatic triangle and tagged with a vessel loop. To accommodate the added bulk from the gracilis muscle, we created a trough by removing a section of the buccal fat and masseter muscle. The source vessels for revascularizing the gracilis flap, commonly the facial artery and vein, are isolated and prepped. Anchoring sutures were placed around the lip at the desired insertion sites. The sutures were placed close to the free lip margin capturing the orbicularis oris muscle or its fibrous replacement, to maximize the translated effect of muscle contraction on the smile display zone. Separate anchor sutures were placed for the 2 muscle paddles. We usually used 2.0 PDS sutures but alternative sutures may be used.
Flap Insertion, Revascularization, and Nerve Coaptation
For stable flap insertion, we created a pseudotendon with running vicryl sutures when the tendinous portion of the harvested flap was inadequate to hold sutures. Under direct visualization, the anchoring sutures were sequentially secured to the muscle tendon or psuedotendon. The secondary paddle was secured to the periosteum over the lateral aspect of the malar bone at the level of the lower eyelid. The tension on the muscle was set close to its passive length. The tension was adjusted to account for secondary slippage at the suture sites. The muscle flap was revascularized using the recipient source vessels. In cases of dual innervation, the masseteric nerve was coapted end-to-end to the obturator nerve and the crossfacial nerve was connected to the obturator nerve in a geometric end-to-side manner through a small neurotomy closer to the hilum of the muscle. The nerve coaptation was performed with 10-0 nylon sutures, reinforced with fibrin glue, and covered with a collagen matrix or entubulated in a vein graft. The primary muscle paddle was then secured at the desired tension to the periosteum of the zygomatic arch and deep temporal fascia. The SMAS flap was suspended as in a facelift to support the muscle flap from bulging or drooping. The skin incision was then closed over a drain.
Statistical Analysis
Statistical analysis for the impact of the multivector gracilis flap on the smile display zone was performed using the paired t test with Bonferroni adjusted α levels. An outcome measure was considered statistically significant for adjusted P < .01. Statistical analysis was performed using Microsoft Excel (version 2013, Microsoft).
Results
There were 10 women and 2 men between ages 20 and 64 years. Five flaps were reinnervated with combined facial and masseteric neural input, 5 with masseteric neural input only, and 2 crossfacial innervation (Table 1). In all cases there was clinical evidence of recovered gracilis function by 4 months and improvement in all measures of the smile display zone. The mean FAI when smiling was reduced from 9.1 mm to 4.5 mm (P = .01) (Table 2). On average, there was exposure of 3.1 additional maxillary teeth when smiling after the multivector gracilis flap. The horizontal exposure of the gingival scaffold posttreatment improved from a mean of 31.5 mm to 43.7 mm (P < .001). There was no significant difference in the average interlabial exposure at midline (7.1 mm vs 7.7 mm, P = .06) but a 56.4% improvement at the level of the canine (3.9 mm vs 6.1 mm, P = .04). Animated wrinkling of the periorbital area when smiling was noted in 4 patients. A sample smile outcome is shown in Figure 3.
Table 1. Effect of the Multivector Gracilis Flap on the Smile Display Zone.
| Patient Age, y/Sex | Type of Innervation | Facial Asymmetry Index, mm | Maxillary Dental Display (x/y)a | Maximum Gingival Scaffold Width, mm | Interlabial Distance at Midline, mm | Interlabial Distance at Canine, mm |
|---|---|---|---|---|---|---|
| 23/M | Single stage xVII + V | 8.4 | 1/5 | 34.4 | 10.3 | 6.8 |
| 4.9 | 3/5 | 39.9 | 7.4 | 5.8 | ||
| 53/F | V | 5.1 | 0/3 | 34.4 | 5.3 | 0.0 |
| 5.7 | 4/5 | 44.3 | 6.1 | 4.2 | ||
| 22/F | Single stage VII+ V | 11.7 | 1/4 | 33.4 | 5.1 | 2.2 |
| 2.1 | 4/4 | 47.7 | 8.9 | 6.3 | ||
| 43/F | 2 Stages xVII + V | 10.5 | 1/5 | 31.6 | 4.0 | 2.8 |
| 0.7 | 4/4 | 50.7 | 6.4 | 4.4 | ||
| 54/F | 2 Stages xVII + V | 2.8 | 1/5 | 40.7 | 9.5 | 3.8 |
| 9.4 | 4/4 | 46.4 | 8.4 | 6.9 | ||
| 54/F | V | 17.6 | 1/5 | 31.1 | 12.1 | 9.1 |
| 9.3 | 4/4 | 47.2 | 12.3 | 12.0 | ||
| 59/F | V | 5.8 | 0/5 | 25.5 | 4.8 | 3.1 |
| 2.2 | 5/5 | 41.6 | 4.6 | 4.2 | ||
| 52/F | 2 Stages xVII | 14.1 | 1/5 | 21.1 | 5.4 | 1.7 |
| 8.5 | 5/5 | 42.3 | 6.2 | 6.2 | ||
| 56/F | V | 13.3 | 2/5 | 31.6 | 4.5 | 2.1 |
| 0.5 | 5/6 | 43.4 | 9.9 | 7.3 | ||
| 64/F | VII + V | 2.8 | 3/5 | 38.2 | 9.8 | 7.2 |
| 2.9 | 5/6 | 43.8 | 8.6 | 6.4 | ||
| 49/M | V | 6.5 | 0/4 | 21.0 | 8.8 | 6.2 |
| 3.4 | 2/4 | 37.3 | 5.6 | 4.3 | ||
| 20/F | 2 Stages xVII | 11.0 | 1/4 | 34.7 | 5.5 | 1.4 |
| 4.2 | 3/4 | 39.7 | 8.1 | 4.7 |
(x/y) Dental display on paralyzed side / dental display on normal side. Data recorded as preoperative in upper row, postoperative in lower row.
Table 2. Statistical Analysis of the Effect of the Mutivector Gracilis Flap on the Smile Display Zone.
| Variable | Pretreatment, Mean | Posttreatment, Mean | Standard Error (95% CI) | T Statistic | P Value |
|---|---|---|---|---|---|
| FAI, mm | 9.1 | 4.5 | 1.6 (−8.0 to −1.2) | −2.8 | .01 |
| Gingival scaffold width, mm | 31.5 | 43.7 | 0.6 (1.9 to 4.3) | 5.2 | <.001 |
| Interlabial distance at midline, mm | 7.1 | 7.7 | 1.0 (−1.5 to 2.7) | 0.6 | .56 |
| Interlabial distance at canine, mm | 3.9 | 6.1 | 1.0 (0.1 to 4.3) | 2.1 | .04 |
| Dental display, no. | 5.5 | 8.6 | 2.1 (7.9 to 16.6) | 5.8 | <.001 |
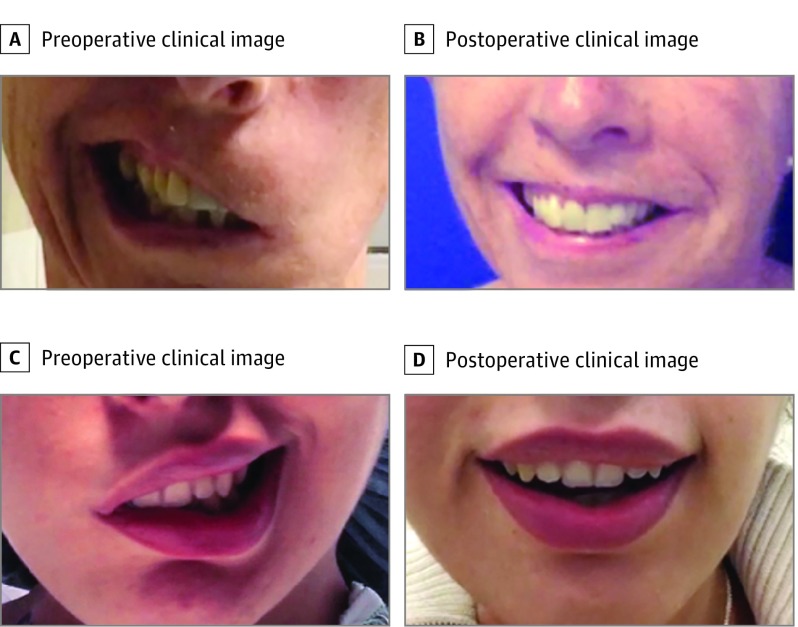
Figure 3. Sample Smile Outcome Following Multivector Double Paddle Gracilis Flap in 2 Patients With Complete Facial Paralysis .
Discussion
We have shown that the gracilis muscle can be reliably transferred as a multivector flap for smile restoration. Analysis of the multivector gracilis flap showed improved exposure of the smile display zone and oral commissure symmetry when smiling. The composite effective of the multivector design was improved lip excursion in the vertical and horizontal dimensions closely matching the nonparalyzed side. The secondary muscle paddle inserted close to the lateral orbital region introduced a desirable periorbital wrinkling typical of a Duchenne smile.
The technique of harvesting a double paddle gracilis flap is similar to the microvascular transfer of compound flaps. Compound flaps are subtyped as composite, conjoined, and chimeric. Composite flaps have multiple tissue components dependent on a solitary vascular source. Conjoin flaps have multiple flap territories, with some common physical continuity but each territory retains its independent vascular supply. Chimeric flaps have multiple physically independent territories, each with an independent vascular supply linked by a common source vessel.11 By this nomenclature, the double belly gracilis flap is a sophisticated chimeric flap with preserved neural input for contraction.
The segmental neurovascular pattern of the gracilis muscle allows for designing a functional flap with 2 or 3 muscle paddles.7 Each paddle can be oriented independent of the other for a multivector effect (Figure 2B and D). In a youthful smile, 75% to 100% of the maxillary central incisors should be positioned below an imaginary line drawn between the commissures (Morley ratio).12 In paralyzed faces, the upper lip drapes over the maxillary dentition masking their display when smiling. Correcting the vertical dimension of paralytic smile improves anterior dental display and upper lip drape. A 2-paddle gracilis flap oriented to more closely simulate the action of upper lip elevators has the potential of reproducing a more youthful smile. The secondary paddle is ideally oriented to more effectively elevate the medial upper lip. In addition, contraction of the secondary muscle in the periorbital region has the potential of introducing a Duchenne-type periorbital wrinkling and animation.
Multiple paddle latissimus and serratus flaps have been described for facial reanimation.12,13,14 Whitney et al13 described 100 cases using multiple slips of the seratus muscle. Allevi et al14 reported the outcome of a single case of double-bellied latissimus dorsi free flap used to restore a full dental smile. Ueda et al15 presented 2 cases of a combined latissimus and serratus flap used for upper and lower lip animation. Compared with the latissimus and serratus flaps, the gracilis is a more robust muscle with a larger PCSA. Owing to the large PCSA, excessive bulk is a common drawback of the gracilis flap. Introducing a second muscle paddle introduces more bulk. However, the independence of the 2 muscle paddles allows optimal positioning of the composite flap while minimizing bulk in the medial or lateral cheek. Dissecting out the secondary or even a third muscle paddle requires technical confidence in the neurovascular pattern of the gracilis muscle (Figure 2).
To evaluate the smile outcome of the multivector gracilis flap, we adopted measurements routinely used by orthodontists for smile analysis.8,12 In 1 study, the faces of 122 male participants were filmed during spontaneous Duchenne and posed social smiling.16 Maxillary and mandibular lip-line heights, tooth display, and smile width were measured using a digital videographic smile analysis similar to the one used in our study. Compared with spontaneous smiling, tooth display during social smiling decreased by up to 30%, along with a significant reduction of smile width. Using a similar smile analysis method, we showed that following the multivector gracilis flap, tooth display improved by 3.1 teeth (56.4%, P < .001) and gingival scaffold width by 38.7% (P < .001). There was a 54.6% improvement in the interlabial distance measured at the canines (2.2 mm, P = .04). Paralytic labial drape is typically pronounced at the mid upper lip. We inserted the secondary muscle paddle close to the mid point of the paralyzed hemi-lip where it was expected to have the most vertical effect on labial drape. The effect of the primary muscle paddle on vertical correction of labial drape at the level of the canine is likely to be minimal given its vector. The vector of the secondary muscle is divergent from that of the primary paddle and is directed toward the lateral orbital rim (Figures 2B-D).
In 4 patients there was dynamic periorbital wrinkling which was likely the effect of the secondary paddle in the periorbital region. Further technical refinement will be necessary to achieve a more consistent periorbital animation. We will report our experience with a third muscle paddle inserted for lower eyelid support in future studies (Figure 2D).
Limitations
This study does not compare outcomes between a double-paddle multivector and a single-paddle gracilis flap or other forms of FFMF. We also do not assess other dimensions of a smile such as initiation, melolabial folds, or cheeks mounds.17
Conclusions
As a biomechanical system, the multivector gracilis muscle flap design is an attempt to move from Mona Lisa and social smiles toward full enjoyable smiles that reflect positive emotion for patients undergoing facial reanimation. The multivector gracilis flap design is effective in improving all components of the smile display zone and has the potential for producing periorbital-wrinkling characteristic of a Duchenne smile.
References
- 1.Kraft TL, Pressman SD. Grin and bear it: the influence of manipulated facial expression on the stress response. Psychol Sci. 2012;23(11):1372-1378. [DOI] [PubMed] [Google Scholar]
- 2.Messinger DS, Fogel A, Dickson KL. What’s in a smile? Dev Psychol. 1999;35(3):701-708. [DOI] [PubMed] [Google Scholar]
- 3.Ekman P, Davidson RJ, Friesen WV. The Duchenne smile: emotional expression and brain physiology. II. J Pers Soc Psychol. 1990;58(2):342-353. [PubMed] [Google Scholar]
- 4.Dey JK, Ishii M, Boahene KD, Byrne PJ, Ishii LE. Changing perception: facial reanimation surgery improves attractiveness and decreases negative facial perception. Laryngoscope. 2014;124(1):84-90. [DOI] [PubMed] [Google Scholar]
- 5.Lindsay RW, Bhama P, Hadlock TA. Quality-of-life improvement after free gracilis muscle transfer for smile restoration in patients with facial paralysis. JAMA Facial Plast Surg. 2014;16(6):419-424. [DOI] [PubMed] [Google Scholar]
- 6.Mathes SJ, Nahai F. Classification of the vascular anatomy of muscles: experimental and clinical correlation. Plast Reconstr Surg. 1981;67(2):177-187. [PubMed] [Google Scholar]
- 7.Morris SF, Yang D. Gracilis muscle: arterial and neural basis for subdivision. Ann Plast Surg. 1999;42(6):630-633. [DOI] [PubMed] [Google Scholar]
- 8.Krishnan V, Daniel ST, Lazar D, Asok A. Characterization of posed smile by using visual analog scale, smile arc, buccal corridor measures, and modified smile index. Am J Orthod Dentofacial Orthop. 2008;133(4):515-523. [DOI] [PubMed] [Google Scholar]
- 9.Albathi M, Oyer S, Ishii LE, Byrne P, Ishii M, Boahene KO. Early nerve grafting for facial paralysis after cerebellopontine angle tumor resection with preserved facial nerve continuity. JAMA Facial Plast Surg. 2016;18(1):54-60. [DOI] [PubMed] [Google Scholar]
- 10.Collar RM, Byrne PJ, Boahene KD. The subzygomatic triangle: rapid, minimally invasive identification of the masseteric nerve for facial reanimation. Plast Reconstr Surg. 2013;132(1):183-188. [DOI] [PubMed] [Google Scholar]
- 11.Hallock GG. Further clarification of the nomenclature for compound flaps. Plast Reconstr Surg. 2006;117(7):151e-160e. [DOI] [PubMed] [Google Scholar]
- 12.Morley J, Eubank J. Macroesthetic elements of smile design. J Am Dent Assoc. 2001;132(1):39-45. [DOI] [PubMed] [Google Scholar]
- 13.Whitney TM, Buncke HJ, Alpert BS, Buncke GM, Lineaweaver WC. The serratus anterior free-muscle flap: experience with 100 consecutive cases. Plast Reconstr Surg. 1990;86(3):481-490. [PubMed] [Google Scholar]
- 14.Allevi F, Motta G, Colombo V, Biglioli F. Double-bellied latissimus dorsi free flap to correct full dental smile palsy [published online July 20, 2015]. BMJ Case Rep. doi: 10.1136/bcr-2015-210436. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Ueda K, Harii K, Yamada A. Free vascularized double muscle transplantation for the treatment of facial paralysis. Plast Reconstr Surg. 1995;95(7):1288-1296.. [PubMed] [Google Scholar]
- 16.Van Der Geld P, Oosterveld P, Berge SJ, Kuijpers-Jagtman AM. Tooth display and lip position during spontaneous and posed smiling in adults. Acta Odontol Scand. 2008;66(4):207-213. [DOI] [PubMed] [Google Scholar]
- 17.Iacolucci CM, Banks C, Jowett N, et al. Development and validation of a spontaneous smile assay. JAMA Facial Plast Surg. 2015;17(3):191-196. [DOI] [PubMed] [Google Scholar]