Abstract
The purpose of our study was to compare the curative effect of two surgical methods for Schatzker type I to III tibia plateau fractures, arthroscopy assisted reduction percutaneous internal fixation (ARIF) and open reduction internal fixation (ORIF), with the intent of evaluating the quality of evidence to assist treatment selection. Searches of PubMed, Cochrane and China National Knowledge Infrastructure (CNKI) databases were performed to identify randomized controlled trials (RCTs) and quasi-RCTs comparing ARIF and ORIF regarding the following outcomes: functional outcomes, perioperative complications and post-traumatic osteoarthritis. Odds ratios (OR) and weighted mean differences (MDs) were pooled using either a fixed-effects model or random-effects model, depending on the heterogeneity of the trials included in the analysis. 19 RCTs and one quasi-RCT provided the data from 1272 patients. ARIF was associated with better functional outcomes, a lower risk of perioperative complications, and lower risk of post-traumatic osteoarthritis. After consideration of the quality of evidence of the included studies, the advantages provided by ARIF are not substantive over ORIF for the treatment of Schatzker type I to III tibia plateau fractures, except reducing the risk of perioperative complications.
Introduction
Tibia plateau fractures are common intra-articular injuries sustained in the lower extremities1. There are two principles in the treatment of tibia plateau fractures, one is anatomical reduction of the articular surface and reconstruction of the mechanical axis of the lower limb; the other is to reconstruct the stability of the injured knee joint2,3. According to Schatzker classification system, type I to III fractures are low energy injuries, sustained in lateral tibia plateau4–6. Traditionally, displaced tibia plateau fractures are treated with open reduction internal fixation (ORIF), even in Schatzker type I to III fractures7,8. Inevitably, infections, hematoma formation, surgical wound dehiscence and surgical wound edge necrosis are frequent complications, due to extensive soft tissue dissection during ORIF2,9–11. The anterior-lateral approach is the most widely used surgical approach when treating tibia plateau fractures surgically, especially in treating fractures located in the lateral tibia plateau12,13. The iliotibial band should be released from the Gerdy’s tubercle, and should be incised a little above the knee joint line2,11. Even more, arthrotomy of the knee joint should be performed, and the lateral meniscus should be released from the lateral tibia plateau, in order to assess fracture reduction directly2,11. The function of the knee joints may be affected by scar formation in the soft tissue aforementioned. Arthroscopy assisted reduction percutaneous internal fixation (ARIF) is emerging recently as an alternative treatment method in treating lower energy tibia plateau fractures14–18. The main advantage of this method relied on the minimally invasive nature during operation without violating the structures aforementioned14,15,17,18. There is controversy over the effectiveness of the two treatment methods, ORIF and ARIF concerning treatment of lower energy tibia plateau fractures. Accordingly, we performed this meta-analysis to compare the treatment effect of arthroscopy assisted reduction percutaneous internal fixation, in treating Schatzker type I to III tibia plateau fractures, with that of open reduction internal fixation.
Materials and Methods
Search strategy
We searched PubMed, Cochrane and China National Knowledge Infrastructure (CNKI) databases from their inception to September 2016, without search filters, using the following MeSH (Medical Subject Heading) terms and text words: tibia fractures, knee injuries, knee joint/injuries, tibial fractures, tibia plateau fractures, tibial plateau fractures, proximal tibia fractures, proximal tibial fractures, proximal metaphyseal tibia fractures, proximal metaphyseal tibial fractures, proximal epiphyseal tibia fractures, proximal epiphyseal tibial fractures, fracture fixation, fracture osteosynthesis, bone nails, bone plates, external fixation, internal fixation, plates, extramedullary fixation, osteosynthesis, intramedullary nails, external fixators, circular fixators, hybrid external fixators. (Supplemental File 1) We also searched the reference lists of the relevant studies identified to supplement our literature search.
Inclusion criteria/exclusion criteria
Only RCTs and quasi-RCTs were enrolled in our study, with non-randomized trials excluded. All the RCTs and quasi-RCTs comparing ORIF to ARIF for low energy Schatzker type I to III tibia plateau fractures were eligible, with open fractures excluded, the duration from injuries to operation should not beyond 3 weeks.
Outcomes of Interest
We included the following outcomes of interest in our analysis: the functional outcomes measured by validated scales; perioperative complications (infection, wound dehiscence, hematoma formation, surgical wound edge necrosis, nerve injuries, vascular injuries, compartment syndromes, and deep vein thrombosis); post-traumatic osteoarthritis.
Study Selection and Data Extraction
Two of our reviewers assessed the eligibility of the identified trials independently. We developed a data extraction sheet based on the Cochrane Consumers and Communication Review Group’s data extraction template19. Two reviewers collected data independently; disagreements were resolved by discussion with a senior author if necessary. We extracted the following information from the included RCTs or quasi-RCTs: research method; the inclusion and exclusion criteria of the included trials; characteristics of trial participants; fracture classification; interventions characteristics, such as the method of reduction and fixation; post-operative outcomes of interest; and risk of bias. We also attempted to contact the primary author through email to seek clarification, if information was missing.
Quality Assessment
Two review authors used the domain-based evaluation described in the Cochrane Handbook for Systematic Reviews of Interventions to evaluate the risk of bias independently20. We assessed the following five domains: random sequence generation; allocation concealment; methods of blinding, including blinding of participants, research personnel and outcome assessors; incomplete outcome data; and selective outcome reporting. Each of these criteria was assessed as ‘low risk of bias’ or ‘high risk of bias’. When there was lack of information or uncertainty over the potential for bias, then they were assessed as ‘unclear risk of bias’. The GRADE approach was used to quantify the quality of the evidence21, when disagreements between the review authors regarding the risk of bias for the identified domains appeared, they were resolved by consensus.
Statistical analysis
We used the Review Manager software (RevMan Version 5.3; The Nordic Cochrane Center, Denmark) to conduct the meta-analyses. Additionally, we used the Stata software (StataSE 12.0; StataCorp LP, USA) to perform the tests for funnel plot asymmetry. Dichotomous outcomes were calculated using Odds Ratios (ORs), together with 95% confidence intervals (CIs). Mean differences (MDs), with corresponding 95% CIs, were used to express continuous outcomes. When the same outcome was measured using different scales, or the same outcome was calculated with either dichotomous and continuous data, the standardized mean difference (SMD) was calculated. We used chi-squared analysis to test the heterogeneity across the included trials, and we used the I2 statistic to assess the impact of identified heterogeneity on the analysis. If the I2 was greater than 50%, heterogeneity was defined as substantial. Estimates of the pooled data were evaluated using a random-effect model, when the substantial heterogeneity between trials included in an analysis was identified; otherwise, a fixed-effect model was chosen. Both the Begg and Egger tests were used to assess the funnel plot asymmetry.
Results
Search Results
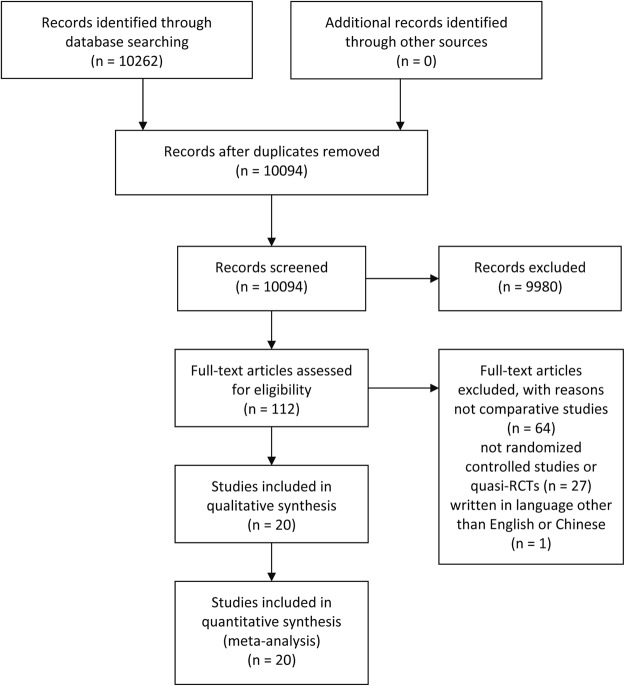
Figure 1 presents the details of the literature search strategy and exclusion criteria in the flow diagram. We identified and screened a total of 10261 titles and abstracts, eventually 20 trials satisfied our eligibility criteria22–41. 19 of the included trials were RCTs23–41, with one quasi-RCT22, comparing ORIF and ARIF in the treatment of closed Schatzker type I to III tibia plateau fractures in adults.
Figure 1.
Flow Diagram of Search.
Quality Assessment
All the included studies had serious methodological flaws that put them at either unclear or high risk of bias for at least three domains (see Figs 2 and 3). Adequate randomization method was described in 9 RCTs23,25–27,29,33,35,36,40, table of random number was used to generate random sequence. The other 10 RCTs did not describe the method of generation of randomization sequence24,28,30–32,34,37–39,41. The one quasi-RCT stated that the random sequence was based on admission number22. None of the included trials described the method of allocation concealment. Only one included trial confirmed the blinding of outcome assessors32, while the other trials did not inform status of blinding.
Figure 2.
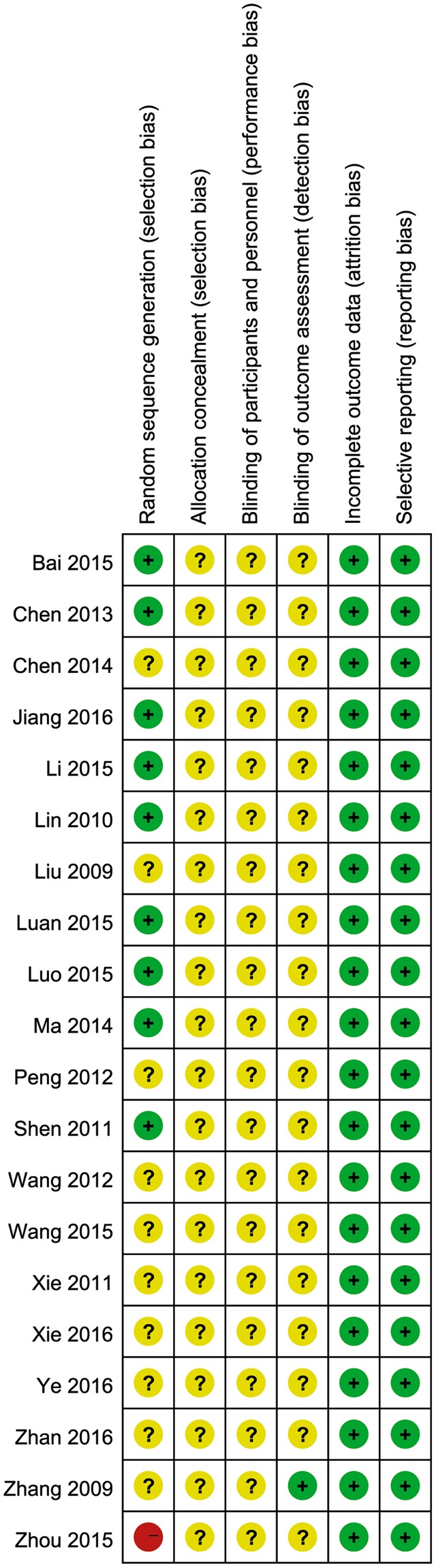
Summary of Risk Bias Assessment. Note: Reviewers’ assessment of each risk of bias item; “+”, low risk of bias; “?”, unclear risk of bias; and “−”, high risk of bias.
Figure 3.
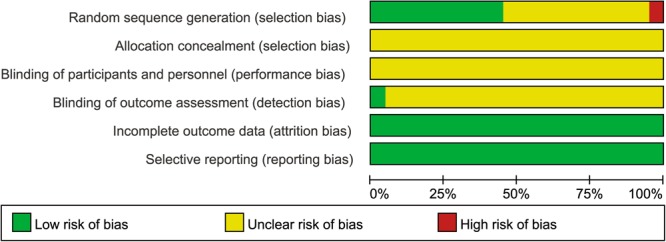
Risk of Bias Graph. Note: Reviewers’ assessment of each risk bias item, presented as a percentage across all included RCTs.
Descriptive Characteristics
All the included studies were single-center trials conducted in China, and all were reported in Chinese. There were only two intervention groups in the all included trials. Open tibia plateau fractures were not included in all 20 trials. Together, the included trials enrolled a total of 1272 patients, providing 1272 fractures, in our analysis. All of the included trials enrolled low energy lateral tibia plateau fractures, with one trial only including Schatzker type III fractures36, one trial including Schatzker type I and II fractures39, 9 trials including Schatzker type II and III fractures22,25,26,28,29,31–34, 9 including Schatzker type I to III fractures23,24,27,30,35,37,38,40,41. All the included trials stated that ORIF was performed through an anterior-lateral surgical approach, arthrotomy was performed from lateral knee compartments, with lateral meniscus being elevated, split fractures of the lateral tibia plateau were reduced by reduction clamp, depressed fractures were reduced by impacting the subchondral bone through the fracture gap or the created bony window, fixation were achieved with plates or screws; ARIF were performed through standard arthroscopic portals, reduction of the split fractures were achieved by reduction clamps, depressed fractures were elevated through the cortical window or the fracture gap using impactors under control of arthroscopy, fixation are achieved with plates or screws. The descriptive characteristics of the included studies are listed in Table 1.
Table 1.
Descriptive Characteristics of Included Trials.
| Study | Year | Sample Size (ARIF) | Sample Size (ORIF) | Gender (M/F) (ARIF) | Gender (M/F) (ORIF) | Age (ARIF) | Age (ORIF) | Follow-up Duration (Mo) (ARIF) | Follow-up Duration (Mo) (ORIF) | Schatzker classification | Functional Scale |
|---|---|---|---|---|---|---|---|---|---|---|---|
| Zhou | 2015 | 32 | 32 | 19/13 | 20/12 | 45.3 ± 6.5 | 42.5 ± 7.2 | 13.50 ± 1.07 | 13.80 ± 1.14 | II, III | HSS |
| Bai | 2015 | 64 | 64 | N/A | N/A | N/A | N/A | 12 | 12 | I, II, III | Rasmussen |
| Chen | 2014 | 36 | 21 | N/A | N/A | N/A | N/A | 14 | 14 | I, II, III | HSS |
| Li | 2015 | 34 | 33 | 20/14 | 18/15 | 47.3 ± 14.9 | 45.9 ± 15.2 | 15.8 ± 3.7 | 15.8 ± 3.7 | II, III | Rasmussen |
| Lin | 2010 | 20 | 30 | 15/5 | 21/9 | 44.7 ± 1.31 | 45.1 ± 13.5 | 10.60 ± 3.44 | 10.80 ± 3.09 | II, III | HSS |
| Luan | 2015 | 23 | 22 | 16/7 | 14/8 | 47.4 ± 12.7 | 48.5 ± 11.8 | 9.30 ± 1.5 | 9.50 ± 1.60 | I, II, III | Lysholm |
| Peng | 2012 | 34 | 34 | * | * | * | * | 13 | 13 | II, III | HSS |
| Shen | 2011 | 38 | 20 | 26/12 | 14/6 | 36.1 | 36.8 | 13.1 | 13.4 | II, III | HSS |
| Wang | 2012 | 19 | 19 | 12.7 | 13.6 | 49 | 51 | 6–16 | 6–16 | I, II, III | Lysholm |
| Xie | 2010 | 5 | 5 | ** | ** | ** | ** | 25 | 25 | II, III | Lysholm |
| Zhang | 2009 | 20 | 20 | 12.8 | 11.9 | 42.5 | 43.5 | 12 | 12 | II, III | Lysholm |
| Luo | 2015 | 54 | 54 | 29/25 | 28/26 | 34.3 ± 0.32 | 36.5 ± 0.42 | N/A | N/A | II, III | Rasmussen |
| Zhan | 2016 | 34 | 34 | 19/15 | 20/14 | 39.4 ± 3.8 | 40.3 ± 4.2 | N/A | N/A | II, III | Lysholm |
| Ma | 2014 | 48 | 48 | 27/21 | 26/22 | 34.2 ± 8.5 | 33.8 ± 7.3 | 12 | 12 | I, II, III | HSS |
| Jiang | 2016 | 40 | 40 | 28/12 | 29/11 | 58.6 ± 7.1 | 58.1 ± 7.3 | N/A | N/A | III | Rasmussen |
| Wang | 2015 | 20 | 20 | 13/7 | 12/8 | 34.8 ± 5.1 | 35.3 ± 4.6 | N/A | N/A | I, II, III | HSS |
| Xie | 2016 | 33 | 33 | 17/16 | 18/15 | 40.2 ± 2.2 | 41.5 ± 2.2 | N/A | N/A | I, II, III | Rasmussen |
| Ye | 2016 | 36 | 36 | *** | *** | *** | *** | N/A | N/A | I, II | Rasmussen |
| Chen | 2013 | 44 | 44 | 22/22 | 23/21 | 45.1 ± 12.8 | 45.9 ± 12.7 | N/A | N/A | I, II, III | Rasmussen |
| Liu | 2009 | 15 | 14 | 9/6 | 8/6 | 34.2 ± 6.0 | 35.4 ± 3.6 | N/A | N/A | I, II, III | Rasmussen |
Note: ARIF, arthroscopy assisted reduction percutaneous internal fixation; ORIF, open reduction internal fixation; M/F, male/female; Mo, month; HSS, Hospital for Special Surgery knee-rating score; Rasmussen, Rasmussen clinical assessment score; Lysholm, Lysholm score; N/A, Not Available; *a general M/F ratio of 50/18, a mean age was 36.4 ± 9.0 years; **a general M/F ratio of 5/5, a mean age was 39.5 years; ***a general M/F ratio of 39/33, a mean age was 42.4 ± 17.5 years.
Effects of Interventions
Functional Outcome
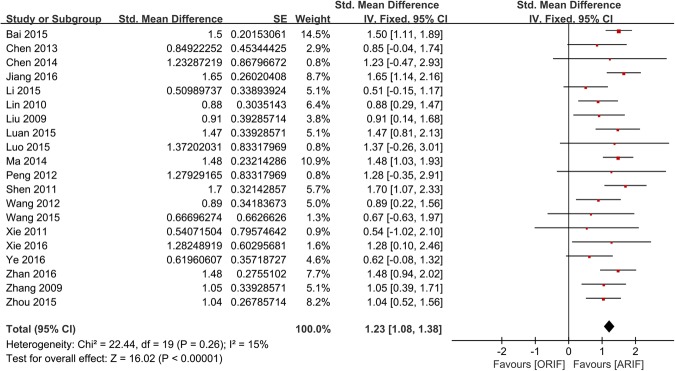
3 different validated scales were used across the included trials to measure the patients’ functional scores: 7 trials used the Hospital for Special Surgery knee-rating score (HSS);22,24,26,28,29,35,37 5 trials the Lysholm score27,30–32,34; 8 the Rasmussen clinical assessment score23,25,33,36,38–41. Pooled data, shown in Fig. 4, indicated statistically significant better post-operative functional outcomes for patients treated with ARIF, compared to ORIF (SMD = 1.23, 95% CI, 1.08–1.38; p < 0.00001).
Figure 4.
Forest Plot of SMDs and Associated 95% Confidence Intervals for Functional Outcomes.
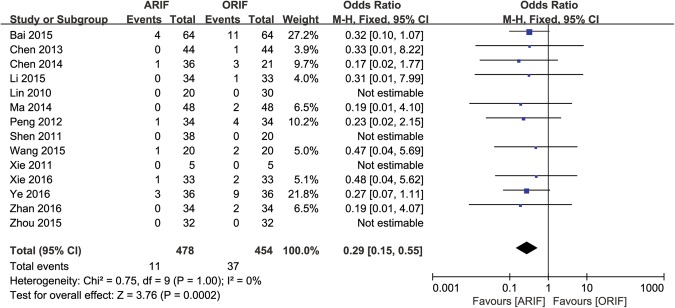
Perioperative Complications
Although perioperative complications were reported in 14 trials22–26,28,29,31,34,35,37–40, there were 4 trials that reported no perioperative complications in either ARIF and ORIF group, which could not be estimated with Odds Ratio, so we included the other 10 trails in the analysis, with a calculated OR of 0.29 (95% CI, 0.15–0.55; p = 0.0002; Fig. 5). The perioperative complications in ORIF group included 22 infections, 4 surgical wound dehiscence, 4 surgical wound necrosis, 4 deep vein thrombosis, and 2 compartment syndromes. The perioperative complication in ARIF group included 7 infections, one wound dehiscence, one wound necrosis, and three deep vein thrombosis. The authors didn’t describe the severity, treatment and prognosis of these perioperative complications.
Figure 5.
Forest Plot of OR, and Associated Confidence Intervals, for perioperative complications.
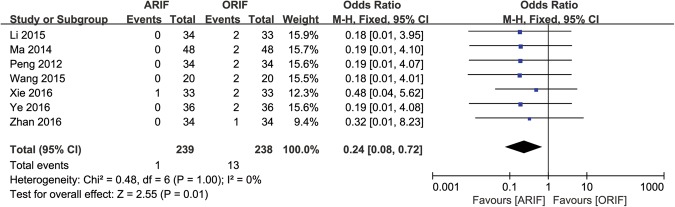
Post-traumatic Osteoarthritis
7 trials reported the outcome of post-traumatic osteoarthritis25,28,34,35,37–39, with a calculated OR of 0.24 (95% CI, 0.08–0.72; p = 0.01; Fig. 6).
Figure 6.
Forest Plot of OR, and Associated Confidence Intervals, for post-traumatic osteoarthritis.
Publication Bias
We conducted the assessments of publication bias for the factors of the functional outcomes, perioperative complications, and post-traumatic osteoarthritis. Both Egger’s test and Begg’s test did not identify any potential publication bias in the functional outcomes (Egger’s test, P = 0.104; Begg’s test, p = 0.229), and perioperative complications (Egger’s test, p = 0.662; Begg’s test, p = 0.721). Potential publication bias was identified in post-traumatic osteoarthritis in Egger’s test (p = 0.032), but not in Begg’s test (p = 0.133). The funnel plots of these three outcomes of interest are illustrated in Figs 7–9.
Figure 8.
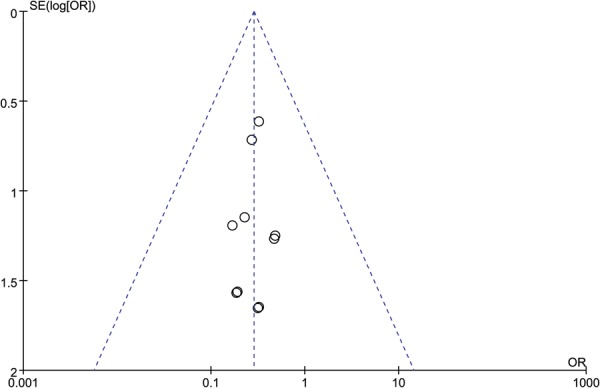
Funnel Plot of OR and Associated Confidence Intervals, for perioperative complications.
Figure 7.
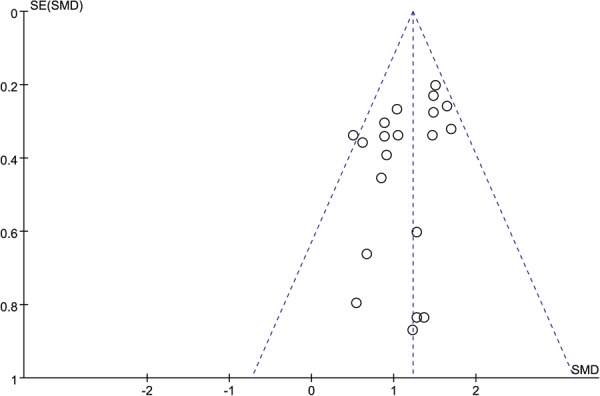
Funnel Plot of SMD and SE, for functional outcomes.
Figure 9.
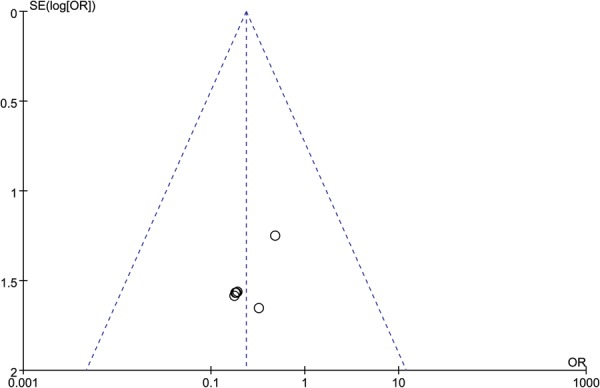
Funnel Plot of OR and Associated Confidence Intervals, for post-traumatic osteoarthritis.
Discussion
Tibia plateau fractures are frequent injuries sustained in the lower extremities1. The anterior-lateral surgical approach is often used to reduce and internally fixate tibia plateau fractures, especially in lateral tibia plateau injuries12,13. Traditionally, the purpose of arthrotomy of the lateral knee joint compartment and elevation of meniscus from tibia plateau in Schatzker I to III fractures is to assess the effect of fractures reduction directly, decompression of the articulate surface is completed from the fracture gap or bony window in metaphyseal area42–44. With the development of arthroscopic technique, the reduction assessment could be achieved without arthrotomy, the fracture fixation could be completed in minimally invasive fashion45–47. In recent years, there’s trend to treat low energy tibia plateau fractures using ARIF technique in China, but there are no clear guidelines as to the superiority between ARIF and ORIF in the treatment of Schaztker I to III fractures. The purpose of our meta-analysis is to critically compare the functional outcomes and complications, between ARIF and ORIF in treating low energy tibia plateau fractures.
Our meta-analysis indicates that the difference in functional outcomes is statistically significant between the two groups: ARIF is superior than ORIF. All the function scales used in the included trials are validated in the literature48–50. We deduce that the integrity of the lateral knee capsule and the avoidance of meniscus detachment preserve the maximum function of the affected knees. In accordance with other minimally invasive procedures in treating fractures other than tibia plateau fractures, risk of perioperative complications in ARIF group is statistically significantly lower than ORIF group in our meta-analysis9,51. Surgical site infections are the most common perioperative complications. We thought the there would be a difference between the aggressive nature of ORIF and the minimally invasive nature of ARIF. Although our included trials didn’t describe the management and prognoses of these complications, we suppose the decrease of perioperative complications could at least shorten the length of hospital stay, reduce the patient’s suffering and the practitioners’ workload. The post-traumatic osteoarthritis of the knee joints is a severe complication in the long term; it is complex and challenging to manage52,53. Our meta-analysis indicated that there is a statistically significant lower risk of post-traumatic osteoarthritis in ARIF group. Although there were 7 trials that reported the outcome of post-traumatic osteoarthritis, only 2 trials reported the follow-up duration, none of the follow-up duration exceeded 24 months postoperatively, whilst none of the other 5 trials stated the length of the follow-up period. None of the included trials described the diagnostic criteria of post-traumatic osteoarthritis.
None of the included studies gave information about allocation concealment, and almost none of the included trials described the method of blinding of participants, practitioners and outcome assessment. Because of the surgical intervention nature of our included trials, we suppose it is hard to execute allocation concealment and blinding. Also taking into account the fact that only 9 of the included trials reported methods of random sequence generation, we conclude that the quality of the data for the functional outcomes to be low. Bearing in mind the aforementioned reasons, but due to the large effect, we deduced the quality of the data for the outcome of perioperative complications to be moderate. Due to the limited information of diagnostic criteria and follow-up duration, combined with the potential for publication bias, we reasoned the quality of the data for incidences of post traumatic osteoarthritis to be very low.
Our meta-analysis searched multiple data bases, using numerous MeSH terms and text words, without search filters. The search strategy and research protocol strictly adhered to the PRISMA statement for reporting systematic reviews and meta-analysis54. (Supplemental File 2) The detailed procedure in the two interventions, namely ARIF and ORIF, are highly coincident in the included trials. Still, there are several limitations in our meta-analysis. First, all the included trials were conducted in China, and all were written in Chinese. Second, all the included trials were small, single center studies. Third, although we only included Schaztker I to III fractures, the concomitant injuries such as meniscus injuries, collateral ligaments injuries, and cruciate ligaments injuries were different between the included studies. Fourth, because of language barriers, we excluded studies written in languages other than English and Chinese. We acknowledge that failure to include studies in other languages will result in missing data. Fifth, treating tibial plateau fractures through ARIF is much more technically demanding than ORIF, there will be a long learning curve confronted by the treating surgeons, the treating surgeons’ experience should be heterogeneous in the included studies. But the focus of our study is Schaztker I to III tibia plateau fractures, which are low energy injuries and easy to reduce and fix, the operative procedures are much more programmatic compared with high energy tibia plateau fractures.
In summary, out study is the first meta-analysis to compare functional outcomes and complications between ARIF and ORIF for the treatment of low energy tibia plateau fractures. Based on the evidence evaluated, ARIF provided no substantive advantage over ORIF in treating Schaztker I to III tibia plateau fractures, except in reducing the risk of perioperative complications. In the future, we need multicenter RCTs, with high methodological quality and long follow-up duration to inform the differences in functional outcomes and risk of post traumatic osteoarthritis between these two treatment methods.
Electronic supplementary material
Acknowledgements
We would like to thank Rasheed Aaman Robinson for English language editing. The study was supported by Wenzhou Municipal Science and Technology Bureau (CN) (Y20160389).
Author Contributions
Conceived and designed the experiments: Y.Y.W., J.P.W., J.B.W. Performed the experiments: Y.Y.W., J.P.W., Y.F.Z., L.Y., J.T. Analyzed the data: Y.Y.W., Y.F.Z., J.T., J.B.W. Contributed reagents/materials/analysis tools: L.Y., J.T. Wrote the paper: Y.Y.W., J.B.W.
Competing Interests
The authors declare no competing interests.
Footnotes
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Electronic supplementary material
Supplementary information accompanies this paper at 10.1038/s41598-018-32201-y.
References
- 1.Moore TM, Patzakis MJ, Harvey JP. Tibial plateau fractures: definition, demographics, treatment rationale, and long-term results of closed traction management or operative reduction. J Orthop Trauma. 1987;1:97–119. doi: 10.1097/00005131-198702010-00001. [DOI] [PubMed] [Google Scholar]
- 2.Papagelopoulos PJ, et al. Complications after tibia plateau fracture surgery. Injury. 2006;37:475–84. doi: 10.1016/j.injury.2005.06.035. [DOI] [PubMed] [Google Scholar]
- 3.Streubel PN, et al. Sagittal Plane Deformity in Bicondylar Tibial Plateau Fractures. J Orthop Trauma. 2011;25:560–565. doi: 10.1097/BOT.0b013e318200971d. [DOI] [PubMed] [Google Scholar]
- 4.Schatzker J, McBroom R, Bruce D. The tibial plateau fracture. The Toronto experience 1968–1975. Clin Orthop Relat Res. 1979;138:94–104. [PubMed] [Google Scholar]
- 5.Liu Y, et al. Characteristics of unilateral tibial plateau fractures among adult patients hospitalized at an orthopaedic trauma centre in China. Sci Rep. 2017;7:40647. doi: 10.1038/srep40647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Molenaars RJ, Mellema JJ, Doornberg JN, Kloen P. Tibial Plateau Fracture Characteristics: Computed Tomography Mapping of Lateral, Medial, and Bicondylar Fractures. J Bone Joint Surg Am. 2015;97:1512–20. doi: 10.2106/JBJS.N.00866. [DOI] [PubMed] [Google Scholar]
- 7.van Dreumel RL, van Wunnik BP, Janssen L, Simons PC, Janzing HM. Mid- to long-term functional outcome after open reduction and internal fixation of tibial plateau fractures. Injury. 2015;46:1608–12. doi: 10.1016/j.injury.2015.05.035. [DOI] [PubMed] [Google Scholar]
- 8.Júnior MK, et al. Tibial Plateau Fractures. Rev Bras Ortop. 2015;44:468–74. doi: 10.1590/S0102-36162009000600002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Wu J, Zhou F, Yang L, Tan J. Percutaneous Reduction and Fixation with Kirschner Wires versus Open Reduction Internal Fixation for the Management of Calcaneal Fractures: A Meta-Analysis. Sci Rep. 2016;6:30480. doi: 10.1038/srep30480. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Mahadeva D, Costa ML, Gaffey A. Open reduction and internal fixation versus hybrid fixation for bicondylar/severe tibial plateau fractures: a systematic review of the literature. Arch Orthop Trauma Surg. 2008;128:1169–75. doi: 10.1007/s00402-007-0520-7. [DOI] [PubMed] [Google Scholar]
- 11.Phisitkul P, McKinley TO, Nepola JV, Marsh JL. Complications of locking plate fixation in complex proximal tibia injuries. J Orthop Trauma. 2007;21:83–91. doi: 10.1097/BOT.0b013e318030df96. [DOI] [PubMed] [Google Scholar]
- 12.Lowe JA, Tejwani N, Yoo BJ, Wolinsky PR. Surgical techniques for complex proximal tibial fractures. Instr Course Lect. 2012;61:39–51. [PubMed] [Google Scholar]
- 13.Lee TC, et al. Bicondylar tibial plateau fracture treated by open reduction and fixation with unilateral locked plating. J Knee Surg. 2017;30:204–211. doi: 10.1055/s-0037-1598077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dall’oca C, et al. Tibial plateau fractures: compared outcomes between ARIF and ORIF. Strateg Trauma Limb Reconstr. 2012;7:163–175. doi: 10.1007/s11751-012-0148-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang Z, Tang Z, Liu C, Liu J, Xu Y. Comparison of outcome of ARIF and ORIF in the treatment of tibial plateau fractures. Knee Surg Sports Traumatol Arthrosc. 2017;25:578–583. doi: 10.1007/s00167-016-4285-9. [DOI] [PubMed] [Google Scholar]
- 16.Kayali C, Oztürk H, Altay T, Reisoglu A, Agus H. Arthroscopically assisted percutaneous osteosynthesis of lateral tibial plateau fractures. Can J Surg. 2008;51:378–82. [PMC free article] [PubMed] [Google Scholar]
- 17.Pogliacomi F, et al. Combined arthroscopic and radioscopic management of tibial plateau fractures: report of 18 clinical cases. Acta Biomed. 2005;76:107–14. [PubMed] [Google Scholar]
- 18.Siegler J, et al. Percutaneous fixation of tibial plateau fractures under arthroscopy: a medium term perspective. Orthop Traumatol Surg Res. 2011;97:44–50. doi: 10.1016/j.otsr.2010.08.005. [DOI] [PubMed] [Google Scholar]
- 19.Higgins, J. P. T. & Deeks, J. J. Chapter 7: Selecting studies and collecting data. Available at, www.handbook.cochrane.org (Accessed: 1st October 2016) (2011).
- 20.Higgins, J. P. T., Altman, D. G., & Sterne, J. A. C. Chapter 8: Assessing risk of bias in included studies. Available at, www.handbook.cochrane.org (Accessed: 1st October 2016) (2011).
- 21.GRADE Working Group Grading quality of evidence and strength of recommendations. BMJ. 2004;328:1490–1494. doi: 10.1136/bmj.328.7454.1490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Zhou H, Qu W. Clinical study of minimally invasive treatment of home-made instruments assisted by arthroscopic for Schatzker type II, III tibial plateau fracture. China Medical Herald. 2015;12:92–96. [Google Scholar]
- 23.Bai X. Effect of arthroscopic assisted minimally invasive internal fixation on the knee function in patients with fracture of tibial plateau. Modern Instruments & Medical Treatment. 2015;21:40–42. [Google Scholar]
- 24.Chen Q, Ye Z, Xia T, Zhang Y. Comparison between arthroscopy and open reduction method in the treatment of various types of Schatzker tibial plateau fractures. Journal of Chongqing Medical University. 2014;39:223–226. [Google Scholar]
- 25.Li J, Pan L, Huang B. Arthroscopy combined with less invasive stabilization system for treatment of tibial plateau fractures accompanied with soft tissue injuries. Chinese Journal of Bone and Joint Surgery. 2015;8:120–124. [Google Scholar]
- 26.Lin, T. Clinical comparative study of tibial plateau fractures treatment with arthroscopic assisted fixation versus traditional reduction internal fixation. Available at, http://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD2011&filename=2010251164.nh&v=MjM4ODhIOURLcTVFYlBJUjhlWDFMdXhZUzdEaDFUM3FUcldNMUZyQ1VSTDJmWStSbkZ5cmhVTHpKVjEyNkhyRzk= (Accessed: 1st October 2016) (2010).
- 27.Luan Y, Zhang M. Arthroscopic percutaneous bone grafting and internal fixation for the treatment of Schatzker I–III tibial plateau fractures. J Trauma Surg. 2015;17:341–344. [Google Scholar]
- 28.Peng Z. Application of minimally invasive internal fixation in treating Schatzker type II and III tibia plateau fractures. Chinese and Foreign Medical Research. 2012;10:28–29. [Google Scholar]
- 29.Shen G, Zhou J. Comparison study on effectiveness between arthroscopy assisted percutaneous internal fixation and open reduction and internal fixation for Schatzker type II and III tibial plateau fractures. Chinese Journal of Reparative and Reconstructive Surgery. 2011;25:1201–1204. [PubMed] [Google Scholar]
- 30.Wang, S. Clinical study of arthroscopy assisted surgical treatment for tibial plateau fractures. Available at, http://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD201301&filename=1013158119.nh&v=MjY4NjFyQ1VSTDJmWStSbkZ5M2xVTDdJVkYyNkhiS zlGdEROcHBFYlBJUjhlWDFMdXhZUzdEaDFUM3FUcldNMUY= (Accessed: 1st October 2016) (2012).
- 31.Xie J, Zhang H, Yin S, Wu T, Peng Z. Arthroscopy assisted calcium orthophosphate grafting in treating tibial plateau fractures. Chinese Journal of Bone and Joint Injury. 2010;25:934–935. [Google Scholar]
- 32.Zhang, Z. The design of guided reduction and bone-grafting instrument and its application research in tibial plateau fractures. Available at, http://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD2010&filename=2009248347.nh&v=MjYxNDFyQ1VSTDJmWStSbkZ5M21VcnpCVjEyN0Y3RzhGdExJcUpFYlBJUjhlWDFMdXhZUzdEaDFUM3FUcldNMUY= (Accessed: 1st October 2016) (2009).
- 33.Luo H. The efficacy of the treatment of reduction and internal fixation with bone graft assisted with knee arthroscopy for tibial plateau compression fracture. Chinese Community Doctors. 2015;31:57–58. [Google Scholar]
- 34.Zhan Z, et al. Arthroscopy assisted minimally invasive locking compression plates fixation in treating tibial plateau compression fractures. Journal of Yangtze University. 2016;13:22–23. [Google Scholar]
- 35.Ma C, Li K, Wang Z, Wei S, Tan Y. The efficacy of arthroscopy assisted minimally invasive surgical treatment for tibial plateau fractures. Guangxi Medical Journal. 2014;36(1330–1331):1341. [Google Scholar]
- 36.Jiang Q, Chen G, Chen X, Yang Z, Yang Y. Study on Percutaneous Balloon Dilatation in Treatment of Schatzkerl III Tibial Plateau Fractures Under Arthroscopy. Clinical Medicine & Engineering. 2016;23:411–412. [Google Scholar]
- 37.Wang S. To Explore the Effect on Arthroscopic Minimally Invasive Treatment of Tibial Plateau Fractures. China Continuing Medical Education. 2015;7:38–39. [Google Scholar]
- 38.Xie B. Clinical Comparison of Arthroscopic-Assisted Minimally Invasive Surgery and Traditional Surgery for the Treatment of Tibial Plateau Fracture. Clinical Medicine & Engineering. 2016;23:341–342. [Google Scholar]
- 39.Ye F, Lan S, Wu Q. Efficacy of fixation with knee arthroscopy as adjuvant therapy for lateral tibial plateau fracture. China Journal of Endoscopy. 2016;22:25–28. [Google Scholar]
- 40.Chen F, Xu H, Zhu G, Qiao T. Clinical efficacy comparison of minimally invasive surgery by mirror auxiliary and traditional operation for treatment of tibial plateau fractures. China Modern Doctor. 2013;51:154–158. [Google Scholar]
- 41.Liu Y. Clinical efficacy of arthroscopy assisted surgery combined with Chinese washing side in treating low energy tibial plateau fractures. Available at, http://kns.cnki.net/KCMS/detail/detail.aspx?dbcode=CMFD&dbname=CMFD2011&filename=2010268532.nh&v=MTc5ODBGckNVUkwyZlkrUm5GeS9rV3JyTFYxMjZIckcrRnRUUHJaRWJQSVI4ZVgxTHV4WVM3RGgxVDNxVHJXTTE= (Accessed: 1st October 2016) (2009).
- 42.Cross WW, III., Levy BA, Morgan JA, Armitage BM, Cole PA. Periarticular raft constructs and fracture stability in split-depression tibial plateau fractures. Injury. 2013;44:796–801. doi: 10.1016/j.injury.2012.12.028. [DOI] [PubMed] [Google Scholar]
- 43.Wang PC, Ren D, Zhou B. Surgical Technique of Anterolateral Approach for Tibial Plateau Fracture. Orthop Surg. 2015;7:368–70. doi: 10.1111/os.12205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Cove R, Keenan J. Tibial bone grafting for lateral tibial plateau fractures. Ann R Coll Surg Engl. 2009;91:268–9. doi: 10.1308/rcsann.2009.91.3.268b. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Benea H, Tomoaia G, Martin A, Bardas C. Arthroscopic management of proximal tibial fractures: technical note and case series presentation. Clujul Med. 2015;88:233–6. doi: 10.15386/cjmed-422. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Burdin G. Arthroscopic management of tibial plateau fractures: surgical technique. Orthop Traumatol Surg Res. 2013;99:S208–18. doi: 10.1016/j.otsr.2012.11.011. [DOI] [PubMed] [Google Scholar]
- 47.van Glabbeek F, van Riet R, Jansen N, D’Anvers J, Nuyts R. Arthroscopically assisted reduction and internal fixation of tibial plateau fractures: report of twenty cases. Acta Orthop Belg. 2002;68:258–64. [PubMed] [Google Scholar]
- 48.Rasmussen PS. Tibial condylar fractures. Impairment of knee joint stability as an indication for surgical treatment. J Bone Joint Surg Am. 1973;55:1331–50. doi: 10.2106/00004623-197355070-00001. [DOI] [PubMed] [Google Scholar]
- 49.Insall JN, Ranawat CS, Aglietti P, Shine J. A comparison of four models of total knee-replacement prostheses. J Bone Joint Surg Am. 1976;58:754–65. doi: 10.2106/00004623-197658060-00003. [DOI] [PubMed] [Google Scholar]
- 50.Briggs KK, et al. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am J Sports Med. 2009;37:890–7. doi: 10.1177/0363546508330143. [DOI] [PubMed] [Google Scholar]
- 51.Wang X, et al. A meta-analysis of plate fixation versus intramedullary nailing for humeral shaft fractures. J Orthop Sci. 2013;18:388–97. doi: 10.1007/s00776-013-0355-8. [DOI] [PubMed] [Google Scholar]
- 52.Whittaker JL, Woodhouse LJ, Nettel-Aguirre. A, Emery CA. Outcomes associated with early post-traumatic osteoarthritis and other negative health consequences 3–10 years following knee joint injury in youth sport. Osteoarthritis Cartilage. 2015;23:1122–9. doi: 10.1016/j.joca.2015.02.021. [DOI] [PubMed] [Google Scholar]
- 53.Stiebel M, Miller LE, Block JE. Post-traumatic knee osteoarthritis in the young patient: therapeutic dilemmas and emerging technologies. Open Access J Sports Med. 2014;5:73–9. doi: 10.2147/OAJSM.S61865. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Moher D, Liberati A, Tetzlaff J, Altman DG, The PRISMA Group Preferred Reporting Items for Systematic Reviews and Meta-Analyses: The PRISMA Statement. Plos Med. 2009;6:e1000097. doi: 10.1371/journal.pmed.1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.