Abstract
Background
Acne scarring is a common disfiguring sequela of acne vulgaris which can lead to serious psychosocial problems and have a negative effect on patients’ quality of life. Although a variety of approaches can be used to treat atrophic acne scars, disadvantages such as long-healing time, dyspigmentation, infections, and prolonged erythema make these treatments unsatisfactory especially for Asians. Fractional micro-plasma radio-frequency is a novel technology that produces minor ablation to the epidermis to promote rapid re-epithelialization, while the radio-frequency evoked thermal effect can stimulate regeneration and remodeling of dermal fibroblasts.
Objective
To evaluate the clinical effectiveness and safety of micro-plasma radio-frequency for the treatment of facial acne scars in Chinese patients.
Materials and Methods
A total of 95 patients with facial atrophic acne scars were treated by micro-plasma radio-frequency using three sessions at 2-month intervals. Patients were seen 1 week after each treatment and 1, 3, 6 months after the final treatment. Improvement was assessed by three independent dermatologists who compared photographs taken before the first treatment and 6 months after the last treatment. Adverse effects were evaluated by a dermatologist who did not participated in the study. Patients also provided self-evaluation of satisfaction levels at the last follow-up visit.
Results
A total of 86 patients with atrophic acne scars completed the entire study. There was a significant improvement in acne scars after three treatments. The mean score of ECCA grading scale (Echelle d’Evaluation Clinique des Cicatrices d’Acné) was reduced from 107.21 to 42.27 (P <0.05). A total of 15 of 86 patients showed more than 75% improvement, 57 patients showed 50–75% improvement, and 14 patients showed 25–50%. After three treatments, all subjects showed improvements in spots, large pores, texture, UV damage, red areas, and porphyrin fluorescence. Pain, erythema, edema, effusion, and scab formation were observed in all patients. The average pain score on a visual analog scale was 6.14 ± 1.12 and all patients tolerated the treatments. The average duration of erythema was 6.26 ± 0.92 days. Hyperpigmentation, hypopigmentation, infections, and worsening of scarring were not seen. All patients were either “very satisfied” or “satisfied” with the treatment outcomes.
Conclusions
Fractional micro-plasma radio-frequency is an effective and safe treatment for acne scars, and might be a good choice for patients with darker skin. Lasers Surg. Med.
Keywords: micro-plasma, radio-frequency, acne scar
INTRODUCTION
Acne vulgaris is a very common chronic inflammatory disease of the pilosebaceous units which usually starts in adolescence and usually affects the face, back, chest, and shoulders where sebaceous glands are abundant. Moderate to severe acne often leads to serious complications, and acne scarring is one of the most common. A study reported scars were evident to some degree in 95% of acne sufferers [1]. Acne scarring can be categorized into three different types depending on whether there is a loss or damage of collagen and other tissue (atrophic scars) or a gain of collagen fibers formation (hypertrophic scars and keloids) [2]. Atrophic acne scars are the most common among the three types on the face, while hypertrophic scars and keloids are more frequently on the back and chest [1]. Atrophic acne scarring on the face is often an unfortunate and permanent disfiguring sequela, and can have a serious negative effect on psychological well-being and patients’ quality of life [2–4]. There are a number of conventional approaches for the treatment of atrophic acne scarring, including surgical techniques (punch excisions, punch grafts and subcision), dermabrasion, chemical peels, ablative laser treatment, non-ablative laser treatment, injection of dermal fillers, and autologous fat transfer [5]. Although improvements in atrophic acne scars can be achieved with these techniques, they carry different risks of adverse side effects. Ablative lasers such as the carbon dioxide laser and erbium YAG laser have been advocated to treat atrophic scars, but the procedures are associated with delayed erythema, persistent hyper-pigmentation, prolonged healing times, infections, and even worsening of scarring, limiting the application of these lasers in Asians [6]. Non-ablative lasers have been shown to be safer and to have fewer side effects, but more treatments are frequently needed to achieve the same results when compared to ablative lasers. The clinical efficacy of non-ablative lasers was not superior to ablative lasers [2,7]. Ablative fractional lasers such as the CO2 laser has been shown to have beneficial effects on atrophic acne scars with fewer side effects, shorter healing times, short downtime, and duration of erythema [8], but for Asians with Fitzpatrick skin type III or IV the possibility of hyperpigmentation cannot be ignored [9–12].
Recently, fractional micro-plasma radio-frequency has been introduced as a dual function modality in dermatology. It can produce a micro-ablative effect promoting rapid skin re-epithelialization, along with a thermal effect stimulating regeneration and remodeling of dermal fibroblasts. It seems to be more suitable for Asians with darker skin types [13]. Micro-plasma radio-frequency has been used for the treatment of acne scars [13,14], facial post-burn hyperpigmentation [15], skin graft contraction [16], wrinkles [13], among other disorders, and the advantages of this modality include temporary erythema, shorter healing times, and minimal downtime [14]. However, the sample sizes of these studies were relatively small, and more studies are required to show that fractional micro-plasma radio-frequency is safe and effective for atrophic acne scars. Therefore, we conducted a prospective clinical trial of 95 Chinese patients with acne scarring treated by micro-plasma radio-frequency, to determine effectiveness, safety, and adverse effects.
MATERIALS AND METHODS
Patients
This clinical study was performed at the Laser Research Unit, Department of Dermatology, Southwest Hospital, Chongqing, China. The protocol was approved by the local Institutional Review Board, and conducted in compliance with good clinical practice, and adhered to the Helsinki guidelines. A total of 95 Chinese patients with moderate to severe degree of atrophic facial acne scarring, with Fitzpa-trick skin types III or IV were enrolled in the study. All patients provided informed written consent before treatment. Exclusion criteria included pregnancy and breastfeeding, a history of keloid formation, collagen vascular disease, or a history of mental illness, dermal fillers, active dermatitis, or bacterial infection, impaired immune function, malignancy, or dermabrasion or laser treatments received in the preceding 6 months, photosensitivity or current use of photosensitive medication, oral isotretinoin use within the last 6 months. Every patient consented to provide photographs.
Treatment Protocols
After cleaning the face with a mild cleanser, the area to be treated was covered with a topical eutectic mixture of 2.5% lidocaine hydrochloric acid and 2.5% prilocaine (Beijing Ziguang Medication Manufacture Corporation Ltd, Beijing, China) and the entire face was covered by a plastic wrap to 1–1.5 hour. The face was sterilized with 70% alcohol prior to treatment. All patients received three treatment sessions at 2-month intervals using the micro-plasma radiofrequency device (Pixel RF, Accent XL; Alma Lasers, Caesarea, Israel) and were seen 6 months after the last treatment. Each session the lesions were treated with three to four passes in different directions of the roller tip at a power of 45–60 W. Patients were asked to evaluate their pain level on a point scale from 0 to 10 (0 = no pain and 10 = extremely painful) based on visual analogue scales (VAS) after each treatment. All patients were instructed to avoid contact with water and refrain from scratching for 3 to 5 days after each treatment. Patients also were encouraged to use SPF 50 sunscreen with a sun protection after epithelialization had taken place. Recombinant human basic fibroblast growth factor (rh-bFGF, State Food and Drug Administration of China approval number S20020025, Beijing Shuanglu Pharmaceutical Co., Ltd.) was applied to the treated area once a day for 1 week. Patients were asked about any discomfort after each treatment and at subsequent each follow-up visit.
Clinical Evaluations
Photographs of each patient were taken prior to every treatment and follow-up visit using the same VISIA Complexion Analysis System (Canfield Scientific, Parsippany, NJ) and digital camera, respectively. Three unbiased dermatologists who were not involved in the treatment, evaluated the improvement of facial atrophic acne scars based on photographs taken before the first treatment and 6 months after the last treatment and they did not know if the photos represented pre or post treatment. Acne scar improvement was quantified according to Echelle d’Evaluation Clinique des Cicatrices d’Acné (ECCA) scores [17]. In this system ECCA grading scales are based on semi-quantitative, weighted assessments of three types of acne scars: V-shaped atrophic scars, M-shaped atrophic scars, and U-shaped atrophic scars. Clinical response was graded using the following scale: none (no improvement, 0), mild (<25% improvement, 1), moderate (25–50% improvement, 2), good (51–75% improvement, 3), and excellent (>75% improvement, 4). The dermatologist who participated in this study recorded the side effects of each treatment by observing the treated area. The possible side effects included pain, erythema, edema, effusion, scaling, infection, scar formation, and dyschromia were recorded. Pain was assessed using visual analog scales (VAS, 0–10). Patients were asked to assess their satisfaction using a grading scale (0 = dissatisfied, 1 = somewhat satisfied, 2 = satisfied, 3 = very satisfied).
Statistical Analysis
Statistical analyses were performed using SPSS software (version 19.0, SPSS, Inc, Chicago, IL). Wilcoxon signed rank tests were used to compare parameters before and after laser treatments. Data were expressed as means plus or minus standard errors, and P <0.05 was considered statistically significant.
RESULTS
Among the 95 subjects, all patients completed the entire treatment course, 86 patients finished the follow-up visits, while the other nine patients did not. Among 86 patients, there were 53 males and 33 females with ages ranging between 18 and 29 years and with an average age of 23.2 ± 3.6 years (Table 1). The history of atrophic acne scarring ranged from 1 to 9 years (mean 4.9 ± 2.3 years).
TABLE 1.
Demographic Baseline of Patients
| Characteristic | Value |
|---|---|
| Age (years), mean ± SD | 23.2 ± 3.6 |
| Gender | |
| Male | 53 |
| Female | 33 |
| Duration of scar (years), mean ± SD | 4.9 ± 2.3 |
| Fitzpatrick skin type | |
| Type III | 36 |
| Type IV | 50 |
| Previous treatment | |
| None | 27 |
| Ablative laser | 32 |
| Non-ablative laser | 21 |
| Dermabrasion | 6 |
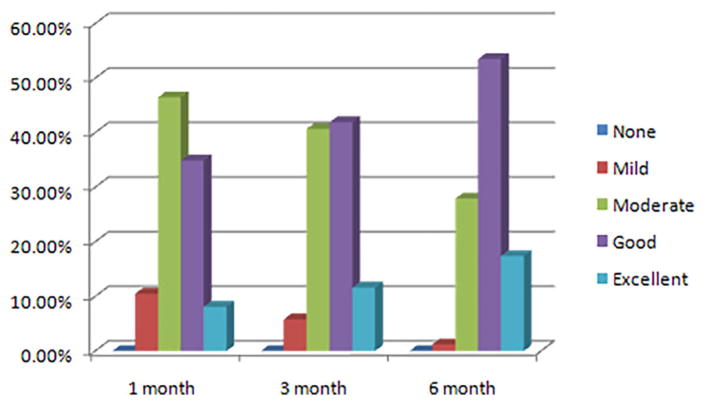
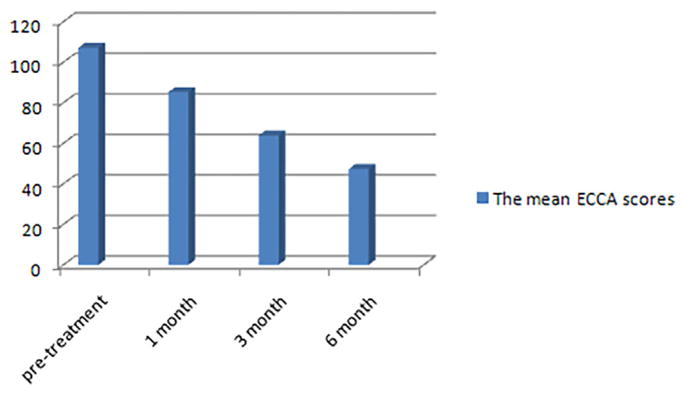
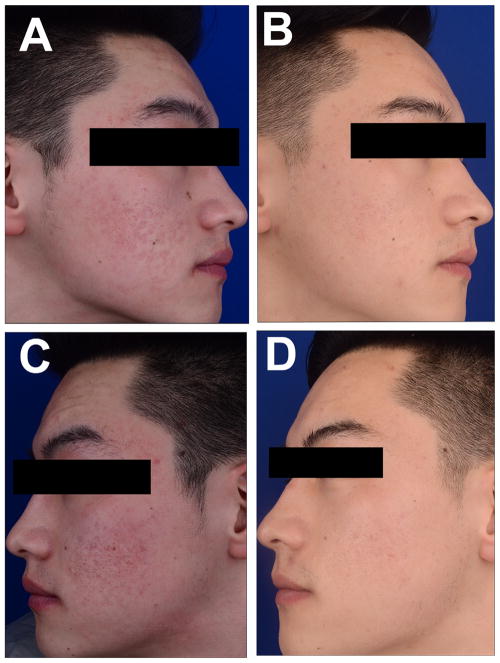
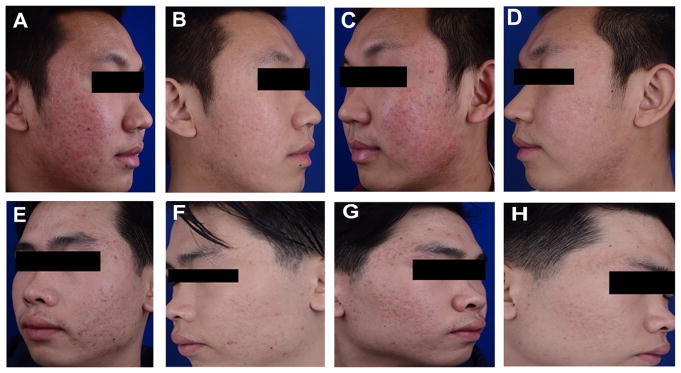
Clinical improvement in facial acne scars was evaluated by three independent blinded dermatologists at 1, 3, 6-month after the last treatment using the five-point scale described above. The acne scars of all patients showed objective improvements at the last follow-up (100% response rate), the improvement in the lesion was graded as excellent in 17.44% (15/86), good in 53.49% (46/86), moderate in 27.90% (24/86), and mild in 1.16% (1/86) (Fig. 1). The mean ECCA score reduced to 47.27 from 107.21 (P <0.05) (Fig. 2). Representative clinical photographs from three patients are presented in Figure 3 and Figure 4. In addition, 6 months after the last treatment all patients showed improvement in spots, large pores, texture, UV spots, red areas, porphyrin fluorescence (P <0.05) compared with baseline (Table 2).
Fig. 1.
Improvement in acne scars in 86 patients after three treatments. Evaluations were conducted using photographs taken before and 1, 3, and 6 months after the last treatment by three independent blinded dermatologists, using a five-point improvement scale.
Fig. 2.
Mean ECCA scores at pre-treatment, and 1, 3, and 6 months after the last treatment.
Fig. 3.
Representative photographs of one patient who received three sessions of micro-plasma radio-frequency (roller tip, 50 W, three passes). (A and C) Pre-treatment. (B and D) Post treatment at 6-month follow-up. An obvious improvement can be observed.
Fig. 4.
Representative photographs of another two patients showing before and after treatments. A–D shows one case with pre- (A and C) and post treatment (B and D) at 6-month follow-up. (E, F) Shows another case with pre- (E and G) and post treatment (F and H) at 6-month follow-up.
TABLE 2.
Comparison of VISIA Values Between Baseline and After 6 Months of Last Treatment
| Items | Baseline | After 6 months of last treatment | P |
|---|---|---|---|
| Spots | 3.40 ± 0.92 | 2.48 ± 0.53 | <0.05 |
| Wrinkles | 5.69 ± 3.57 | 6.92 ± 8.83 | n.s. |
| Texture | 6.19 ± 2.51 | 4.41 ± 2.25 | <0.05 |
| Pores | 3.05 ± 1.06 | 2.29 ± 1.19 | <0.05 |
| UV spots | 5.80 ± 2.25 | 4.85 ± 1.98 | <0.05 |
| Brown spots | 0.90 ± 0.56 | 0.72 ± 0.57 | n.s. |
| Red areas | 2.63 ± 0.66 | 2.22 ± 0.69 | <0.05 |
| Porphyrins | 1.53 ± 0.99 | 0.83 ± 0.59 | <0.05 |
6-month follow-up. An obvious improvement was observed.
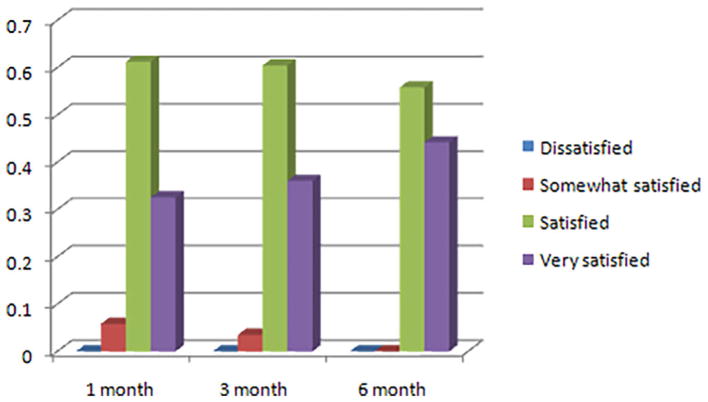
After three treatments and three follow-up visits, the levels of patient satisfaction revealed that 38 (44.19%) patients were “very satisfied” and 48 (55.81%) patients were satisfied at the third follow-up. No patients were dissatisfied at the clinical response of the treatment for atrophic acne scars (Fig. 5). The average score for satisfaction for improvement of acne scars was 2.44 at last follow-up.
Fig. 5.
Satisfaction levels of 86 patients for the improvement of the acne scars reported at 1, 3, and 6 months after the last treatment.
Adverse Effects
There were no serious adverse effects during the treatment and follow-up visits. The main side effects were pain, edema, erythema, scaling, and effusion (Micro-plasma radio frequency results in mild epidermal ablation and perforate effusion.). Although all patients could tolerate the micro-plasma radio-frequency treatments, most of them complained about the pain after each treatment. The pain scores ranged between 4 and 8 on the visual analog scale and the mean pain scores was 6.14 ± 1.12. The number of hours the pain lasted ranged from 2 to 9 hours and the average duration was 4.96 ± 1.39 hours. The duration of post-therapy erythema ranged from 4 to 8 days and the average duration was 6.26 ± 0.92 days. The mean duration of post-therapy scaling and edema was 5.40 ± 0.92 days (range 4–7 days), 1.76 ± 0.59 days (range 1–3 days), respectively. A slight effusion was seen in all patients after each treatment and the average duration was 4.61 ± 1.15 hours. Two patients experienced acne eruption in the treated area at 1 week post-procedure, but this condition subsided without any treatment. Infections, hyperpigmentation, hypopigmentation, worsening of scarring were not observed during the treatments and follow-up visits (Table 3).
TABLE 3.
Adverse Reactions after Treatment With a Micro-Plasma Radio-Frequency in Chinese Patients
| Side effects | Mean ± SD |
|---|---|
| Pain (VAS/mean ± SD) | 6.14 ± 1.12 |
| Pain (hours/mean ± SD) | 4.96 ± 1.39 |
| Erythema (days/mean ± SD) | 6.26 ± 0.92 |
| Crust (days/mean ± SD) | 5.40 ± 0.92 |
| Edema (days/mean ± SD) | 1.76 ± 0.59 |
| Effusion (hours/mean ± SD) | 4.61 ± 1.15 |
| Hyperpigmentation | None |
| Hypopigmentation | None |
| Infections | None |
| Worsening of scarring | None |
DISCUSSION
Acne scarring is one of the most common and unfortunate complications of acne vulgaris which commonly appears mostly on the face and can be associated with poor self-esteem, depression, distress, anxiety, unemployment, and even suicide [3]. Scarring results from damage to the skin and is associated with a loss or decrease in the deposition of collagen during the wound healing process after inflammatory lesions. Atrophic acne scarring can be divided into three types depending on the morphology: ice pick, boxcar, and rolling scars [4]. The degree of acne scarring has been linked to patient age and sex, site of the acne, severity and the duration of the inflammation occurring in the acne lesions, as well the lack of adequate therapy for the acne lesions [1,18]. Therefore, an early and adequate treatment regimen to reduce the inflammation of acne lesions may be advisable to prevent acne scarring [18]. Although there are a great number of options to treat atrophic acne scars, a satisfactory clinical response is challenging and there are no methods that can remove them completely. During the past decade, the role of lasers and other energy devices have steadily changed from a secondary treatment option to a primary treatment option for scar management. Current types of dermatological laser devices extend the treatment availability and provide options for most scar categories [19]. It is well known that fractional lasers (ablative or non-ablative) have been able to provide good clinical results, however side-effects are hard to avoid, such as delayed erythema, prolonged healing times, infections, and dyschromia [20–22]. The carbon dioxide laser is considered to be a gold standard for skin resurfacing, however, persistent hyperpigmentation has been reported as a side-effect, especially for darker skin types [23]. Walgrave et al. reported 32.1% incidence of post-inflammatory hyperpigmentation at the 1-month follow-up visit and 12% at the 3-month follow-up visit after fractional carbon dioxide laser treatment of acne scars [24]. With the fast development of science and technology, picosecond laser with a lens array was used for treatment acne scars, the mechanism is not clear and the main principle may be laser-induced optical breakdown in the skin [25–26].
Fractional micro-plasma radio-frequency technology is a new modality that makes use of a discharge of radio-frequency energy acting on a stream of nitrogen gas very close to the surface of the skin by spicules on the roller. A portion of the gas molecules is ionized into a high-energy state of matter called “plasma” [15,27]. As plasma is very sensitive to electromagnetic fields, the RF energy triggers micro-sparks in the plasma between the skin surface and the spicules of the handpiece. These sparks cause mild epidermal ablation and perforate the dermis superficially to form micro-channels. These micro-channels can increase penetration of the drug into the skin. Rh-bFGF can promote the wound healing and increase secretion of the collagen [28–29]. Therefore, in our study we applied rh-bFGF to the treated area to promote the lesion re-epithelialization and new collagen synthesis rapidly. What is more, many other therapeutic methods may also promote improve atrophic scars. Recently, platelet-rich plasma (PRP) is used for treatment of acne scars by combing with fractional laser and is proved to be may increase clinical efficacy [30–31]. Besides, there is also a modest associated thermal effect. The mild epidermal ablation triggers rapid re-epithelialization, along with the thermal effect which promotes extensive dermal remodeling, including new collagen synthesis and deposition [32]. The mechanism of collagen synthesis is also not very clear, it may be related to expression of fibrogenetic biomolecules [33]. The ablative effect of the fractional micro-plasma radio-frequency technology is minimal compared with the fractional carbon dioxide laser. Fractional carbon dioxide laser will result in a deep and narrow microscopic treatment zone, while fractional micro-plasma radio-frequency results in a broad and superficial microscopic treatment zone [34]. Therefore, theoretically micro-plasma is safer and should have a shorter duration of erythema, hyperpigmentation, and less downtime.
Our results revealed the mean duration of post-therapy erythema was 6.26 ± 0.92 days, which was much shorter than the duration of erythema found with fractional CO2 laser treatment of acne scars, it was reported the prolonged erythema of 27% patients was more than 1 month and in half of the patients within 1 month [25]. The fractional micro-plasma radio-frequency device is a non-chromophore-dependent energy source so that its mechanism of action is not dependent on the skin color. The epidermal ablation is mild and the epidermal layer of the treated area is intact. What is more, we set the power of fractional micro-plasma radio-frequency range between 45 and 60 W, this is a relative moderate energy to treat acne atrophic scars and it did not cause a lot of damage to skin of the treated area. In the future, we can try to set a broader range of energy of fractional micro-plasma radio-frequency to find the more suitable energy. That may explain why no post-inflammatory hyperpigmentation was observed in this study. This is consistent with a report from Zhang et al. who compared fractional CO2 laser with fractional micro-plasma radio-frequency, and found that the former caused 12 patients to show post-inflammatory hyperpigmentation, while no hyperpigmentation was observed with the latter [14].
In this study, the significant improvement of facial atrophic acne scars was observed after a series of three sessions of treatment. With each treatment, an improved outcome was observed, although the data was only collected at 6 months after the third treatment. It has been reported that the improvement could continue for up to 6 months [30]. Therefore, there may be additional improvement if we continue to follow the patients. No severe adverse effects were seen in this study. Pain, edema, erythema, scaling, and effusion were observed in all patients, however all of them could tolerate these side-effects. The average duration of pain, edema, erythema, scaling, and effusion was relatively transitory. There were no infections, dyschromia, worsening of scarring in the study, and all patients expressed satisfaction with the results. The results revealed the fractional micro-plasma radio-frequency is an effective and safe method for the treatment of atrophic acne scars. We also noted that some active acne lesions within the treatment area in several patients underwent improvement to some extent, possibly because due to thermal effects acting on the sebaceous gland function in the dermis and lessening the secretion of sebum [13]. Photographs of each patient taken by the VISIA system demonstrated visible results in the improvement of spots, large pores, texture, UV spots, red areas, and porphyrin fluorescence (P <0.05) within the treatment area. Due to the fact that all of the patients were young people, and the follow-up time was only 6 months, no improvement was observed in any wrinkles and brown spots within the treatment area. We can extend the age range of subjects enrolled to explore the improvement in wrinkles and skin aging in a future study.
In conclusion, our results provide evidence that fractional micro-plasma radio-frequency is not only an effective and safe method for the treatment of atrophic acne scars, but also can improve active acne lesions, spots, large pores, texture, UV spots, red areas, porphyrin fluorescence, and possibly even wrinkles within the treatment area. No severe side effects were observed when used in patients with darker skin. However, most of the patients still complained of pain after the treatment, so clinical studies in the future should explore different methods of alleviating this pain by using a forced cool air chiller before treatment, or performing plasma treatment under general anesthesia. In short, fractional micro-plasma radio-frequency device is a good method to treat atrophic acne scars in Chinese patients.
Acknowledgments
Contract grant sponsor: National Natural Science Foundation of China; Contract grant number: 81571902; Contract grant sponsor: National Institute of Allergy and Infectious Diseases; Contract grant numbers: R01AI050875, R21AI121700; Contract grant sponsor: Southwest Hospital Clinical Innovation Research Foundation, Third Military Medical University; Contract grant number: SWH2014LC17.
Footnotes
Conflict of Interest Disclosures: All authors have completed and submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest and have disclosed the following: Dr. Rui Yin received research grant (No. 81571902) from National Natural Science Foundation of China and clinical research grant (SWH2014LC17) from Southwest Hospital, Third Military Medical University for this work. Michael R Hamblin was supported by US NIH grants R01AI050875 and R21AI121700 No authors hold stock, or receive royalties from any companies.
References
- 1.Layton AM, Henderson CA, Cunliffe WJ. A clinical evaluation of acne scarring and its incidence. Clin Exp Dermatol. 1994;19(4):303–308. doi: 10.1111/j.1365-2230.1994.tb01200.x. [DOI] [PubMed] [Google Scholar]
- 2.Rivera AE. Acne scarring: a review and current treatment modalities. J Am Acad Dermatol. 2008;59(4):659–676. doi: 10.1016/j.jaad.2008.05.029. [DOI] [PubMed] [Google Scholar]
- 3.Fife D. Evaluation of acne scars how to assess them and what to tell the patient. Dermatol Clin. 2016;34(2):207–213. doi: 10.1016/j.det.2015.11.009. [DOI] [PubMed] [Google Scholar]
- 4.Sánchez Viera M. Management of acnes cars: fulfilling our duty of care for patients. Br J Dermatol. 2015;172(Suppl 1):47–51. doi: 10.1111/bjd.13650. [DOI] [PubMed] [Google Scholar]
- 5.Pavlidis AI, Katsambas AD. Therapeutic approaches to reducing atrophic acne scarring. Clin Dermatol. 2017;35(2):190–194. doi: 10.1016/j.clindermatol.2016.10.013. [DOI] [PubMed] [Google Scholar]
- 6.Jordan R, Cummins C, Burls A. Laser resurfacing of the skin for the improvement of facial acne scarring: a systematic review of the vidence. Br J Dermatol. 2000;142(3):413–423. doi: 10.1046/j.1365-2133.2000.03350.x. [DOI] [PubMed] [Google Scholar]
- 7.Cohen BE, Brauer JA, Geronemus RG. Acne scarring: a review of available therapeutic lasers. Lasers in Surgery and Medicine. 2016;48(2):95–115. doi: 10.1002/lsm.22410. [DOI] [PubMed] [Google Scholar]
- 8.Hedelund L, Haak CS, Togsverd-Bo K, Bogh MK, Bjerring P, Haedersdal M. Fractional CO2 laser resurfacing for atrophic acne scars: a randomized controlled trial with blinded response evaluation. Lasers Surg Med. 2012;44(6):447–452. doi: 10.1002/lsm.22048. [DOI] [PubMed] [Google Scholar]
- 9.Ong MWS, Bashir SJ. Fractional laser resurfacing for acne scars: a review. Br J Dermatol. 2012;166(6):1160–1169. doi: 10.1111/j.1365-2133.2012.10870.x. [DOI] [PubMed] [Google Scholar]
- 10.Chan NP, Ho SG, Yeung CK, Shek SY, Chan HH. Fractional ablative carbon dioxide laser resurfacing for skin rejuvenation and acne scars in Asians. Lasers Surg Med. 2010;42(9):615–623. doi: 10.1002/lsm.20974. [DOI] [PubMed] [Google Scholar]
- 11.Kim S, Cho KH. Clinical trial of dual treatment with an ablative fractional laser and a nonablative laser for the treatment of acne scars in Asian patients. Dermatol Surg. 2009;35(7):1089–1098. doi: 10.1111/j.1524-4725.2009.01193.x. [DOI] [PubMed] [Google Scholar]
- 12.Elcin G, Yalici-Armagan B. Fractional carbon dioxide laser for the treatment of facial atrophic acne scars: prospective clinical trial with short and long-term evaluation. Lasers Med Sci. 2017;32(9):2047–2054. doi: 10.1007/s10103-017-2322-7. [DOI] [PubMed] [Google Scholar]
- 13.Zhang Z, Fei Y, Chen XD, Lu WL, Chen JN. Comparison of a fractional micro plasma radio frequency technology and carbon dioxide fractional laser for the treatment of atrophic acne scars: a randomized split-face clinical study. Dematol Surg. 2013;39(4):559–556. doi: 10.1111/dsu.12103. [DOI] [PubMed] [Google Scholar]
- 14.Halachmi S, Orenstein A, Meneghel T, Lapidoth M. A novel fractional micro-plasma radio-frequency technology for the treatment of facial scars and rhytids: a pilot study. J Cosmet Laser Ther. 2010;12(5):208–212. doi: 10.3109/14764172.2010.514921. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Wang LZ, Ding JP, Yang MY, Chen DW, Chen B. Treatment of facial post-burn hyperpigmentation using micro-plasma radiofrequency technology. Lasers Med Sci. 2015;30(1):241–245. doi: 10.1007/s10103-014-1649-6. [DOI] [PubMed] [Google Scholar]
- 16.Ding JP, Fang L, Wang LZ. The use of micro-plasma radiofrequency technology in secondary skin graft contraction: 2 case reports. J Cosmet Laser Ther. 2015;17(6):301–303. doi: 10.3109/14764172.2015.1027230. [DOI] [PubMed] [Google Scholar]
- 17.Dreno B, Khammari A, Orain N, Noray C, Mérial-Kieny C, Méry S, Nocera T. ECCA grading scale: an original validated acne scar grading scale for clinical practice in dermatology. Dermatology. 2007;214(1):46–51. doi: 10.1159/000096912. [DOI] [PubMed] [Google Scholar]
- 18.Yin R, Lin L, Xiao Y, Hao F, Hamblin MR. Combination ALA-PDT and ablative fractional Er:YAG laser(2,940nm) on the treatment of severe acne. Laser Surg Med. 2014;46(3):165–172. doi: 10.1002/lsm.22219. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Balaraman B, Geddes ER, Friedman PM. Best reconstructive techniques: improving the final scar. Dermatol Surg. 2015;41(19):265–275. doi: 10.1097/DSS.0000000000000496. [DOI] [PubMed] [Google Scholar]
- 20.Shin MK, Choi JH, Ahn SB, Lee MH. Histologic comparison of microscopic treatment zones induced by fractional lasers and radiofrequency. J Cosmet Laser Ther. 2014;16(6):317–323. doi: 10.3109/14764172.2014.957216. [DOI] [PubMed] [Google Scholar]
- 21.Wat H, Wu DC, Chan HH. Fractional resurfacing in the Asian patient: current state of the art. Lasers Surg Med. 2017;49(1):45–59. doi: 10.1002/lsm.22579. [DOI] [PubMed] [Google Scholar]
- 22.Verner I. Clinical evaluation of the efficacy and safety of fractional bipolar radiofrequency for the treatment of moderate to severe acne scars. Dermatol Ther. 2016;29(1):24–27. doi: 10.1111/dth.12275. [DOI] [PubMed] [Google Scholar]
- 23.Luping H, Huang L. A new modality for fractional CO2 laser resurfacing for acne scars in Asians. Lasers Med Sci. 2013;28(2):627–632. doi: 10.1007/s10103-012-1120-5. [DOI] [PubMed] [Google Scholar]
- 24.Walgrave SE, Ortiz AE, MacFalls HT, et al. Evaluation of a novel fractional resurfacing device for treatment of acne scarring. Lasers Surg Med. 2009;41(2):122–127. doi: 10.1002/lsm.20725. [DOI] [PubMed] [Google Scholar]
- 25.Dierickx C. Using normal and high pulse coverage with picosecond laser treatment of wrinkles and acne scarring: long term clinical observations. Lasers Surg Med. 2018;50(1):51–55. doi: 10.1002/lsm.22763. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bernstein EF, Schomacker KT, Basilavecchio LD, Plugis JM, Bhawalkar JD. Treatment of acne scarring with a novel fractionated, dual-wavelength, picosecond-domain laser incorporating a novel holographic beam-splitter. Lasers Surg Med. 2017;49(9):796–802. doi: 10.1002/lsm.22734. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Wang S, Mi J, Li Q, Jin R, Dong J. Fractional microplasma radiofrequency technology for non-hypertrophic post-burn scars in Asians: a prospective study of 95 patients. Lasers Surg Med. 2017;49(6):563–569. doi: 10.1002/lsm.22640. [DOI] [PubMed] [Google Scholar]
- 28.Fayazzadeh E, Ahmadi SH, Rabbani S, Boroumand MA, Salavati A, Anvari MS. A comparative study of recombinant human basic fibroblast growth factor (bFGF) and erythropoietin (EPO) in prevention of skin flap ischemic necrosis in rats. Arch Iran Med. 2012;15(9):553–556. [PubMed] [Google Scholar]
- 29.Xing B, Wu F, Li T, Qi S, Xie J, Ye Z. Experimental study of comparing rhEGF with rhβFGF on improving the quality of wound healing. Int J Clin Exp Med. 2013;6(8):655–661. [PMC free article] [PubMed] [Google Scholar]
- 30.Min S, Yoon JY, Park SY, Moon J, Kwon HH, Suh DH. Combination of platelet rich plasma in fractional carbon dioxide laser treatment increased clinical efficacy of for acne scar by enhancement of collagen production and modulation of laser-induced inflammation. Lasers Surg Med. 2017:1–9. doi: 10.1002/lsm.22776. [DOI] [PubMed] [Google Scholar]
- 31.Zhu JT, Xuan M, Zhang YN, et al. The effcacy of autologous platelet-rich plasma combined with erbium fractional laser therapy for facial acne scars or acne. Mol Med Rep. 2013;8(1):233–237. doi: 10.3892/mmr.2013.1455. [DOI] [PubMed] [Google Scholar]
- 32.Li X, Fang L, Huang L. In vivo histological evaluation of fractional ablative microplasma radio frequency technology using a rollertip: an animal study. Lasers Med Sci. 2015;30(9):2287–2294. doi: 10.1007/s10103-015-1810-x. [DOI] [PubMed] [Google Scholar]
- 33.Min S, Park SY, Moon J, Kwon HH, Yoon JY, Suh DH. Comparison between Er:YAG laser and bipolar radiofrequency combined with infrared diode laser for the treatment of acne scars: differential expression of fibrogenetic biomolecules may be associated with differences in efficacy between ablative and non-ablative laser treatment. Lasers Surg Med. 2017;49(4):341–347. doi: 10.1002/lsm.22607. [DOI] [PubMed] [Google Scholar]
- 34.Shin MK, Choi JH, Ahn SB, Lee MH. Histologic comparison of microscopic treatment zones induced by fractional lasers and radiofrequency. J Cosmet Laser Ther. 2014;16(6):317–323. doi: 10.3109/14764172.2014.957216. [DOI] [PubMed] [Google Scholar]