Structured Abstract
Objective
To evaluate the effect of Medicare Shared Savings Program ACOs on hospital readmission after common surgical procedures.
Summary Background Data
Hospital readmissions following surgery lead to worse patient outcomes and wasteful spending. Accountable care organizations (ACOs), and their associated hospitals, have strong incentives to reduce readmissions from two distinct Centers for Medicare and Medicaid Services (CMS) policies.
Methods
We performed a retrospective cohort study using a 20% national Medicare sample to identify beneficiaries undergoing one of seven common surgical procedures—abdominal aortic aneurysm repair, colectomy, cystectomy, prostatectomy, lung resection, total knee arthroplasty, and total hip arthroplasty—between 2010 and 2014. The primary outcome was 30-day risk-adjusted readmission rate. We performed difference-indifferences analyses using multilevel logistic regression models to quantify the effect of hospital ACO affiliation on readmissions following these procedures.
Results
Patients underwent a procedure at one of 2,974 hospitals, of which 389 were ACO affiliated. The 30-day risk-adjusted readmission rate decreased from 8.4% (95% CI, 8.1%–8.7%) to 7.0% (95% CI, 6.7%–7.3%) for ACO affiliated hospitals (p<0.001) and from 7.9% (95% CI, 7.8%–8.0%) to 7.1% (95% CI, 6.9%–7.2%) for non-ACO hospitals (p<0.001). The difference-in-differences of the two trends demonstrated an additional 0.52% (95% CI, 0.97%–0.078%) absolute reduction in readmissions at ACO hospitals (p=0.021), which would translate to 4,410 hospitalizations avoided.
Conclusion
Readmissions following common procedures decreased significantly from 2010 to 2014. Hospital affiliation with Shared Savings ACOs was associated with significant additional reductions in readmissions. This emphasis on readmission reduction is one mechanism through which ACOs improve value in a surgical population.
Introduction
Reducing hospital readmissions is a priority for payers, policymakers and clinical leaders. Though some may be necessary, avoidable readmissions are emblematic of poor quality, leading to worse patient outcomes and wasteful spending.1–6 It is estimated that readmissions cost the Centers of Medicare and Medicaid Services (CMS) up to $17 billion annually.5 To address this issue, CMS has implemented two policies that leverage readmission rates as a measure of hospital quality: the Hospital Wide Readmission Measure and the Hospital Readmission Reduction Program.7,8 The Hospital Wide Readmission Measure was developed in 2012 and began reporting outcomes publically in 2013.7,9 This measure has also been incorporated as a care coordination performance metric for Shared Savings Program Accountable Care Organizations (ACOs).10 ACOs meeting readmission thresholds for this measure receive points towards the shared savings reward. Concurrently, CMS began penalizing all hospitals with readmission rates greater than the national average following discharges for acute myocardial infraction, pneumonia and congestive heart failure though the Hospital Readmissions Reduction Program.8 This policy expanded in 2014 to include chronic obstructive pulmonary disease and elective total knee and hip arthroplasty. Under this policy, penalties as high as 3% of total Medicare payments have been levied against three-quarters of hospitals in 2016, totaling over $420 million.11,12
Taken together, these policies provide strong financial incentives for ACOs to reduce readmissions. Since Medicare Shared Savings Program ACOs receive bonus payments for achieving quality and spending benchmarks, focusing on readmission reduction addresses both of these targets. Lower overall readmission rates increase the likelihood of receiving shared savings rewards by contributing to the ACO quality measure benchmarks and by decreasing per beneficiary spending. Furthermore, by reducing readmissions for conditions targeted by the Hospital Readmissions Reduction Program, ACO with affiliated hospitals avoid readmission penalties. Prior analyses have shown that hospitals participating in ACOs reduce readmissions from both skilled nursing facilities13 and after discharges for medical conditions targeted by the Hospital Readmission Reduction Program.14 Whether or not similar reductions can be accomplished after major surgery is unclear. In contrast to readmissions following medical discharges, which often result from exacerbation of chronic conditions or failure of care coordination, those after surgery are frequently a consequence of procedure-related complications.15–18 Consequently, the reasons for readmission differ from medical conditions, as does the degree to which they are preventable.19,20 Thus, interventions targeting improvements in care coordination— discharge navigators, care transition programs and medication reconciliation21–23—may be less effective in patients recovering from surgery.
We evaluated the effect of hospital participation in a Shared Savings ACO on 30-day readmission rates following major surgery. Since spending related to surgical care totals $500 billion annually,24 even minor improvements have the potential to lead to substantial savings.
Methods
Study Population
We performed a retrospective cohort study using a 20% national Medicare sample of fee-for-service beneficiaries undergoing one of seven major surgical procedures between January 1, 2010 and November 30, 2014: abdominal aortic aneurysm (AAA) repair, colectomy, cystectomy, prostatectomy, lung resection, total knee arthroplasty and total hip arthroplasty (Supplemental Digital Content Table 1). We selected these procedures as they are common and frequently used in evaluating policy effects,20,25,26 span the spectrum of readmission rates (4.4% following total knee arthroplasty27 to 25% following cystectomy28), severity (90-day mortality rates ranging from 1.9 to 6.92,20,28,29 and reflect multiple surgical disciplines (vascular, urology, colorectal, thoracic, and orthopedic). The inclusion of knee and hip arthroplasty, two procedures targeted by the Hospital Readmission Reduction Program,8 also allows us to investigate the influence of this policy on our overall results. We restricted our cohort to patients age 66 years or older to facilitate risk adjustment. We included patients with continuous enrollment in both Medicare Part A and B one year prior to the procedure through 30 days after discharge. We excluded patients in Medicare Advantage plans due to the absence of complete claims and because they are ineligible to be assigned to ACOs.30 We further limited our sample to patients treated in acute care or critical access hospitals. Hospital participation in Medicare Shared Savings Program ACOs was determined using the 2014 Provider-level Research Identifiable File provided by the CMS. This was performed by using the last four digits of the Medicare provider number. This number is available in both Medicare data as well as the ACO provider file. If the last four digits were less than 1000 (acute care) or 1300–1399 (critical access) then the provider was included as a hospital.31 Hospital characteristics were obtained from the 2014 CMS Provider of Service file and the American Hospital Association Annual Survey.
Outcomes
Our outcome was the risk-adjusted readmission rate within 30 days of discharge following one of the index procedures. Only the first readmission was included in the analysis. Patients dying during the hospital stay for the index procedure were censored from readmission calculations. To further investigate how each procedure contributed to the overall outcome, we also estimated procedure-specific readmission rates.
Analysis
We assessed differences in patient and hospital characteristics among beneficiaries treated at ACO and non-ACO affiliated hospitals before and after implementation using chi-squared tests. We measured level of comorbidity using the Hierarchical Condition Category risk score32 and socioeconomic class was determined at the ZIP code level using established methods.33
Next, we implemented our difference-in-differences analysis.34 This approach allows us to estimate changes in readmissions among ACO hospitals from the pre- to the post-ACO implementation period, and quantify the difference between these hospitals and those not affiliated with an ACO. Further, this method allows us to account for other contemporaneous efforts to reduce readmissions,8,9,35 which would be reflected in the trends seen among non-ACO hospitals. In this context, we first defined whether a hospital was affiliated or non-affiliated with an ACO. We then specified a time variable indicating whether a hospital discharge occurred before or after implementation of Shared Savings ACOs. Since ACO enrollment occurred at multiple time points during our study period (April 1, 2012, July 1, 2012, and January 1, 2013, January 1, 2014), we defined two periods (pre-implementation and post-implementation) to reflect all time before or after the start of the ACO contract. ACO affiliated hospitals were included in the post-implementation time period based on the specific ACO’s date of enrollment. Non-ACO affiliated hospitals were included in the post-implementation time period on January 1, 2013 since this was the median date of ACO enrollment in our sample. We then used a multilevel logistic regression model to calculate the rate of readmission for ACO and non-ACO affiliated hospitals in the pre- and post-implementation periods. The model was adjusted for age, sex, race, Hierarchical Condition Category risk score, socioeconomic class, index surgery type and hospital characteristics including size, teaching status, urban or rural location, for profit status and procedure volume. Robust standard errors were used to account for clustering within hospitals. The model also included an interaction term between hospital ACO participation and time period, which allowed us to estimate how adjusted readmission rates varied between ACO and non-ACO aligned hospitals in both the pre- and post-implementation periods. The difference-in-differences of the adjusted readmission rates is the effect of ACO alignment, controlling for secular trends.36–38 We then calculated the procedure specific readmission rates using similar adjusted logistic regression models. We confirmed that trends in readmissions were parallel for ACO and non-ACO affiliated hospitals prior to ACO implementation (Supplemental Digital Content Figure 1).
Sensitivity Analyses
We performed several sensitivity analyses to test the robustness of our findings. First, in our primary analysis, we excluded patients who died during the initial hospitalization as these patients cannot be readmitted. Since it is possible that hospitals may have lower readmission rates if they have high mortality rates, we performed our analysis without excluding these patients. Second, since interventions aimed at reducing readmissions may take some time to operationalize, we performed a sensitivity analysis allowing for a three month “transition period” from the ACO implementation date and calculated differences in readmission rates for procedures occurring outside this period. Third, given the potential for differences between markets adopting early ACO contract and those that did not, we included a fixed effect for Hospital Referral Regions (HRR). Lastly, we included a fixed effect for calendar year to account for the variable length of the ACO exposure among ACO hospitals that arises from the differences in contract start dates.
All analyses were carried out in SAS 9.4 (Cary, NC) and Stata 14 (College Station, TX). All tests were two-tailed and the probability of Type 1 error was set at 0.05. The study protocol was judged to be exempt by the institutional review board of the University of Michigan.
Results
We identified 429,275 patients undergoing one of our index procedures (Table 1). A total of 2,974 hospitals were included, of which 389 were affiliated with an ACO. Compared to non-ACO hospitals, patients treated at ACO affiliated hospitals were similar in age but differed in sex, race/ethnicity, and comorbidity; however, these differences were small and unlikely to be of clinical significance. More patients treated at ACO hospitals had high socioeconomic class (38% vs. 31%, p <0.001) and resided in large metropolitan counties (51% vs. 42%, p<0.001). ACO affiliated hospitals were larger (38% vs. 25% with >500 beds, p<0.001), more likely to be teaching (25% vs. 17%, p<0.001), located in urban areas (94% vs. 88%, p<0.001) and less likely to have for-profit status (5% vs. 17%, p<0.001). Mortality rates at ACO and non-ACO affiliated hospitals did not differ significantly (2.6 vs. 2.7, p=0.12).
Table 1.
Patient and hospital characteristics.
| Characteristic | ACO Hospitals (N = 389) |
Non-ACO Hospitals (N = 2,585) |
p-value |
|---|---|---|---|
| Patients, N | 80,501 | 348,774 | |
| Index procedures, N | |||
| Abdominal Aortic Aneurysm Repair | 4,267 | 16,795 | |
| Colectomy | 12,670 | 57,173 | |
| Cystectomy | 789 | 2,735 | |
| Prostatectomy | 2,383 | 9,820 | |
| Lung resection | 4,827 | 18,746 | |
| Total knee arthroplasty | 36,988 | 165,770 | |
| Total hip arthroplasty | 18,577 | 77,735 | |
| Age, mean (SD) | 75 (6.4) | 75 (6.3) | 0.78 |
| Male sex, N (%) | 33,241 (41) | 145,949 (42) | 0.004 |
| Race/Ethnicity, N (%) | |||
| White | 73,847 (92) | 318,360 (91) | <0.001 |
| Black | 4,415 (6) | 18,764 (5) | |
| Hispanic | 469 (1) | 3,393 (1) | |
| Asian | 608 (1) | 2,832 (1) | |
| Other | 1,162 (1) | 5,425 (2) | |
| HCC score, Mean (SD) | 1.44 (1.6) | 1.42 (1.6) | 0.001 |
| Socioeconomic class, N (%) | |||
| Low | 22,131 (28) | 117,200 (34) | <0.001 |
| Medium | 25,802 (32) | 113,933 (33) | |
| High | 30,492 (38) | 108,878 (31) | |
| Residential area, N (%) | |||
| ≥1 million metropolitan county | 40,960 (51) | 145,536 (42) | <0.001 |
| <1 million metropolitan county | 25,819 (32) | 124,151 (35) | |
| >2,500 urban population | 11,952 (15) | 69,124 (20) | |
| Rural or <2,500 urban population | 1,715 (2) | 9,669 (3) | |
| Hospital Size - N (%) | |||
| ≤250 beds | 18,482 (23) | 138,939 (40) | <0.001 |
| 251–500 beds | 31,721 (39) | 121,081 (35) | |
| >500 beds | 30,298 (38) | 88,738 (25) | |
| Hospital type - N (%) | |||
| Teaching | 20,009 (25) | 59,395 (17) | <0.001 |
| Urban | 75,577 (94) | 305,332 (88) | <0.001 |
| For-profit | 3,723 (5) | 58,478 (17) | <0.001 |
HCC-Hierarchical Condition Category
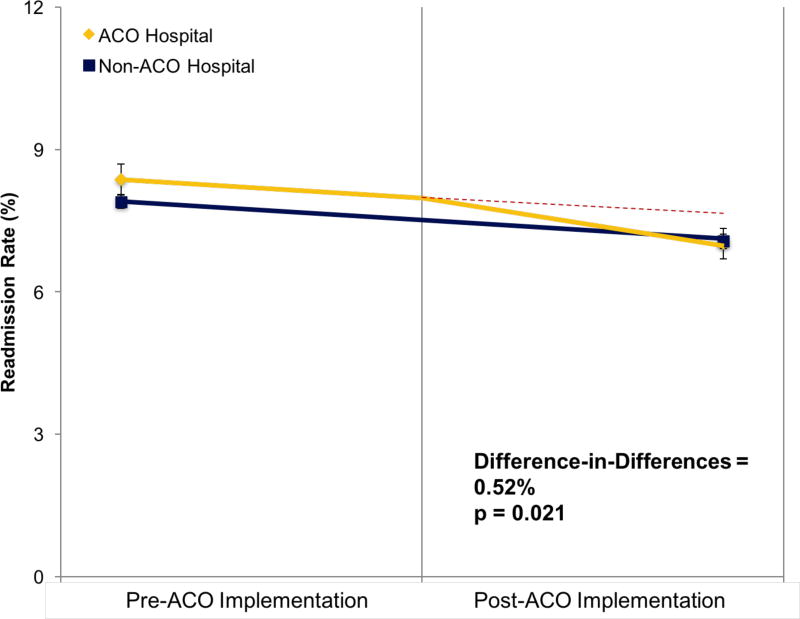
Figure 1 shows the changes in the readmission rate for ACO and non-ACO affiliated hospitals. Prior to ACO implementation, the rate of readmission for hospitals that eventually became ACO affiliated was 8.4% (95% CI, 8.1%–8.7%) compared to 7.9% (95% CI, 7.8%–8.0%) for non-affiliated hospitals. This difference of 0.48 percentage points was statistically significant (p=0.008). Post-ACO implementation, readmission rates decreased in both groups. For ACO hospitals, the rate decreased to 7.0% (95% CI, 6.7%–7.3%), a significant absolute change of 1.4 percentage points and relative change of 17% (p<0.001). For non-ACO hospitals, the rate decreased to 7.1% (95% CI, 6.9%–7.2%), which also represented a significant decrease of 0.83 percentage points (p<0.001). This 11% relative decrease compared to the pre-implementation period among non-ACO hospitals is representative of the ACO independent trends in readmissions. We found a significant effect for ACO affiliation (i.e., the difference in the readmission rate changes between our two cohorts) of −0.52 percentage points (p=0.021). This difference translates to 882 fewer readmissions in the 20% Medicare sample or 4,410 fewer readmission among all Medicare beneficiaries during the post-ACO implementation period.
Figure 1.
Rate of 30-day readmission pre- and post-implementation of Medicare Shared Savings Program Accountable Care Organizations (ACO) stratified by hospital ACO affiliation. The red dashed line represents the theoretical trend in the absence of an ACO effect. ACO hospitals differed in pre-implementation readmission rates (8.4% vs. 7.9%, p=0.008). Readmissions decreased significantly in both ACO (7.0%, p<0.001) and non-ACO (7.1%, p<0.001) affiliated hospitals post-implementation. The difference in these changes results in an additional 0.52% (p=0.021) absolute reduction in readmissions, which is the effect associated with hospital ACO affiliation.
There were significant temporal changes in the procedure-specific rates of readmission (Table 2). We noted decreases in readmissions from the pre- to post-ACO implementation period for both ACO and non-ACO hospitals following AAA repair (3.2%, p=0.001; 2.4%, p<0.001), colectomy (2.1%, p=0.004; 0.9%, p-0.004), and total knee arthroplasty (1.5%, p<0.001; 0.6% p<0.001), respectively. Readmissions following total hip arthroplasty decreased significantly for non-ACO hospitals only (0.9%, p<0.001). There were no significant changes in readmission following cystectomy, prostatectomy or lung resection.
Table 2.
Overall and procedure-specific risk-adjusted rates of readmission stratified by hospital ACO status and time period. The difference-in-differences represents the added effect of hospital ACO affiliation.
| ACO Hospitals | Non-ACO Hospitals | Difference-in- Differences % (95% CI) |
|||||
|---|---|---|---|---|---|---|---|
| Pre % (95% CI) |
Post % (95% CI) |
p- value |
Pre % (95% CI) |
Post % (95% CI) |
p- value |
||
| Overall Cohort | 8.4 (8.1–8.7) | 7.0 (6.7–7.3) | <0.001 | 7.9 (7.8–8.0) | 7.1 (6.9–7.2) | <0.001 | −0.52 (−0.97 to −0.08) |
| Abdominal Aortic Aneurysm Repair | 13.5 (12.0–14.9) | 10.3 (8.7–11.8) | 0.001 | 12.7 (12.0–13.4) | 10.3 (9.5–11.1) | <0.001 | −0.84 (−3.1 to 1.4) |
| Colectomy | 15.9 (15.0–16.8) | 13.8 (12.6–15.0) | 0.004 | 15.2 (14.8–15.6) | 14.3 (13.8–14.8) | 0.004 | −1.1 (−2.6 to 0.04) |
| Cystectomy | 27.5 (22.4–32.6) | 27.6 (22.0–33.3) | 0.98 | 26.2 (23.7–28.7) | 26.4 (23.3–29.5) | 0.92 | −0.12 (−7.6 to 7.4) |
| Prostatectomy | 4.5 (3.6–5.5) | 5.2 (3.4–7.0) | 0.54 | 5.5 (4.9–6.1) | 5.1 (4.3–5.9) | 0.42 | 1.1 (−1.2 to 3.3) |
| Lung Resection | 12.5 (11.3–13.8) | 11.1 (9.7–12.6) | 0.17 | 11.7 (11.0–12.3) | 11.0 (10.3–11.7) | 0.17 | −0.75 (−2.3 to 1.4) |
| Total knee arthroplasty | 5.9 (5.5–6.3) | 4.4 (4.0–4.7) | <0.001 | 5.2 (5.0–5.3) | 4.6 (4.4–4.7) | <0.001 | −0.91 (−1.4 to −0.35) |
| Total hip arthroplasty | 6.3 (5.8–6.8) | 5.7 (5.1–6.3) | 0.12 | 6.3 (6.1–6.6) | 5.4 (5.2–5.7) | <0.001 | 0.33 (−0.47 to 1.1) |
In the procedure specific analyses, ACO affiliation significantly reduced readmissions, relative to nonaffiliated hospitals, only following total knee arthroplasty. For this procedure, hospital ACO affiliation was associated with an absolute decrease in the readmission rate of 0.91% (p<0.001) which translates to 736 fewer readmissions during the post-ACO implementation period in the 20% sample, or 3,683 Medicare beneficiaries overall. ACO affiliation was associated with non-significant differential decreases in readmissions following abdominal aortic aneurysm repair (0.84%, p=0.46), colectomy (0.94%, p=0.23), cystectomy (0.12%, p=0.98) and lung resection (0.75%, p=0.90). Readmissions increased at ACO hospitals following prostatectomy (1.1%, p=0.34) and total hip arthroplasty (0.33%, p=0.42), however neither of these changes were statistically significant.
The results of all sensitivity analysis confirmed the primary finding. By including patients that died during the initial hospitalization, ACO affiliated hospitals were associated with a 0.51 percentage point reduction in 30- day readmissions (p=0.24). Exclusion of procedures performed during the three month “transition period” following the ACO implementation date resulted in an additional 0.56 percentage point reduction in 30-day readmission rates (p=0.023) for ACO affiliated hospitals. Adjusting for regional differences (i.e. HRR) and calendar year resulted in a 0.46 percentage point (p=0.036) and 0.60 percentage point (p=0.013) for ACO affiliated hospitals, respectively.
Discussion
We found that one in ten fewer patients are readmitted after major surgery in the post-ACO implementation period compared to the pre-ACO implementation period. Over the first three years of the Medicare Shared Savings Program, ACO affiliation was associated with an additional 0.52 absolute percentage point reduction in readmissions, translating into 4,400 fewer readmissions among Medicare beneficiaries undergoing these procedures. This added impact of ACO affiliation was a result, in large part, of reductions in readmission following total knee arthroplasty.
Our results suggest that readmission reduction is one mechanism through which ACOs improve quality and decrease spending in surgical patients. This finding is not surprising given the strong financial incentives to reduce readmissions both through the Shared Savings and Hospital Readmission Reduction Programs. Additionally, this focus on readmissions is substantiated by evidence that hospitals affiliated with ACOs are more likely to use multiple quality improvement tools to identify and track readmissions compared with those not participating in the Shared Savings Program.39 Though our analysis is the first to demonstrate an effect of ACO affiliation on readmission in surgical populations, our results align with prior work demonstrating that Pioneer or Shared Savings ACOs hospitals were associated with larger decreases in all-cause readmissions from skilled nursing facilities among Medicare beneficiaries.13 Our findings do, however, contrast early reports which found no difference in all-cause 30 day readmissions among all beneficiaries aligned with Pioneer40 or Shared Savings41 ACOs. Potential reasons for these differences include conflation of both medical and surgical discharges or a limited exposure time in those studies. Indeed, evaluation of the first four years of ACO participation demonstrated additional reductions in readmission of 0.6–0.9% following discharges for pneumonia, congestive heart failure and acute myocardial infarction at ACO affiliated.14
An alternative explanation may be that our findings highlight a selection bias regarding which hospitals became ACOs. Prior to ACO implementation, hospitals destined to become ACO affiliated had higher rates of readmission compared to non-ACO hospitals. In the post-ACO implementation period, both groups reduced readmission to similar levels. Participation in the Shared Savings Program is voluntary and the majority of ACOs participate in a one-sided risk model (i.e., no risk of financial penalties).42 Thus, hospitals with higher readmission rates may have preferentially chosen to become ACOs given the higher likelihood of meeting the spending and quality benchmarks, which are based on prior performance. This explanation is less likely. Readmission rates make up only a small fraction of the quality and spending metrics used to determine receipt of shared savings bonuses. Additionally, ACO and non-ACO affiliated hospitals had similar decreases in readmission rates for our surgical procedures during the pre-implementation period, meaning that both groups were working towards reducing readmissions. Our results are supported by similar analyses of medical readmission where, prior to the start of the Shared Savings ACO program, all hospitals had similar readmission rates for acute myocardial infarction, congestive heart failure and pneumonia.43 Nonetheless, ACO affiliation resulted in larger decreases in readmission rates for these conditions.14 This finding, in combination with the similar pre-implementation trends and strong financial incentives, make it more likely that ACOs are actively targeting readmissions as an avenue to improve value for surgical populations.
Our findings of an overall reduction in readmissions is strongly driven by changes in knee arthroplasty, a condition targeted by the Hospital Readmission Reduction Program. Larger reductions in readmissions for medical conditions targeted by this policy (acute myocardial infarction, congestive heart failure and pneumonia) were reported in multiple studies,44,45 and ACOs were shown to have a differential effect beyond the policy on these readmissions.14 This observation indicates a complementary interaction between the Shared Savings ACO and Hospital Readmissions Reduction Program policies and are aligned with Medicare’s multipronged approach to readmission reduction. In contrast, we did not see a differential effect for ACOs following hip arthroplasty, which is also targeted by the policy. Efforts to reduce readmissions after knee arthroplasty could be expected to also affect hip arthroplasty. However, differences in the reasons for readmission between these procedures may be one explanation for this. Surgical site infections and wound complications are the primary reason for readmission following knee arthroplasty while joint problems (i.e., dislocations, prosthetic misalignment, periprosthetic fractures, etc.) are the primary reason following hip arthroplasty.15,46,47 Quality improvement efforts at the hospital level are much more likely to affect wound complications as compared to joint complications that are intrinsic to the surgery itself. Though this is one potential explanation, this difference highlights the heterogeneity in readmissions among surgical patients, which may account for why broad, systems level interventions have such varied effects on procedure-specific readmission rates.
Our findings should be considered in the context of several limitations. First, hospitals in our sample varied in the duration of their exposure to the ACO program, with some having over two years while other have less than one. However, if longer participation in the ACO program is necessary to improve outcomes, inclusion of ACOs in their first year of existence would bias our findings towards the null. Thus, given the significant positive finding, the magnitude of the ACO effect may, in fact, be larger than observed. Second, there is heterogeneity with regards to ACO alignment in the patient populations treated at ACO hospitals. That is, beneficiaries are assigned to ACOs based on whether they receive the plurality of primary care from a physician that has opted into an ACO. This means that all hospitals treat both ACO and non-ACO aligned beneficiaries. However, this is not likely to lead to variation in how hospitals prevent readmissions. Since beneficiaries are assigned to most Shared Savings ACOs retrospectively, hospitals and surgeons are unaware of a patient’s ACO status and are unlikely to implement different interventions at the patient level. Alternatively, it is possible that ACO beneficiaries leveraging the ACO-level infrastructure through their primary care provider could have a decreased readmission risk due to improved care coordination and meaningful use of post-acute care services independent of hospital services. Given that some ACO beneficiaries are being treated at non-ACO hospitals, our estimates of the ACO effect are likely to be conservative. Lastly, effective readmission reduction interventions may take some time to operationalize. Thus, readmission trends in the time shortly after implementation may not reflect the ACO effect, potentially dampening the effect size. Though we found this to be true in our sensitivity analysis allowing for a three month “transition period” post-ACO implementation, the difference in the readmission reduction was small (0.04 percentage points).
Despite these limitations, our findings have important implications. Our results validate ACOs as an effective tool to improve value in surgical patients but also highlight the heterogeneity in the effect depending on the procedure. In light of the differences in the reasons for readmission, systems-level interventions effective in reducing readmissions after medical conditions may be ineffective in driving change for surgical patients. The finding that ACO and non-ACO affiliated hospitals reached the same rate of readmission in the post-implementation period also raises the possibility of a “floor” rate in readmissions (i.e., some readmissions are unavoidable and therefore the readmission rate will never be zero). Consequently, the ability of policy to continue driving improvement in readmission rates may diminish. This is an important consideration with the shift toward alternative payment models as part of the Medicare Access and CHIP Reauthorization Act.48
Conclusions
Readmissions following common major surgeries decreased significantly from 2010 to 2014. Hospital affiliation with Shared Savings Program ACOs was associated with significant additional reductions in readmissions. The emphasis on reducing readmissions is one mechanism through which ACOs improve value in surgical populations. The ACO effect was strongly driven by changes in readmission following total knee arthroplasty, a procedure targeted by a separate readmission reduction policy. This supports the possibility that ACOs proactively responded to strong financial incentives implied by both the possibility of Shared Savings bonuses and penalties related to the Hospital Readmission Reduction Program. These findings further validate Medicare’s multipronged approach to reducing readmissions and, as a consequence, spending growth.
Supplementary Material
Supplemental Digital Content Figure 1. Rate of 30-day readmission for ACO and non-ACO affiliated hospitals prior to implementation of Medicare Shared Savings Program Accountable Care Organizations. Similar trends in quarterly readmission rates are noted for both ACO and non-ACO affiliated hospitals.
Acknowledgments
Funding/Support: This study was supported by National Institute on Aging R01 AG048071 (BKH) and R01 AG039434 (JBD), National Cancer Institute Grant R01 CA174768 (DCM), T32 CA180984 (TB), Agency for Health Care Research and Quality R01 HS024728 (JMH) and R01 HS024525 (JMH).
Role of Funder/Sponsor: Funders had no role in the design and conduct of the study, collection, management, analysis, and interpretation of the data; preparation, review, or approval of the manuscript; and decision to submit the manuscript for publication.
Footnotes
Conflicts of Interest: Dr. Dimick has a financial interest in Arbormetrix, Inc.
Disclaimer: The views expressed in this article do not reflect the views of the federal government.
References
- 1.Benbassat J, Taragin M. Hospital readmissions as a measure of quality of health care: advantages and limitations. Archives of internal medicine. 2000;160(8):1074–1081. doi: 10.1001/archinte.160.8.1074. [DOI] [PubMed] [Google Scholar]
- 2.Gonzalez AA, Abdelsattar ZM, Dimick JB, Dev S, Birkmeyer JD, Ghaferi AA. Time-to-readmission and Mortality After High-risk Surgery. Annals of surgery. 2015;262(1):53–59. doi: 10.1097/SLA.0000000000000912. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Varacallo MA, Herzog L, Toossi N, Johanson NA. Ten-Year Trends and Independent Risk Factors for Unplanned Readmission Following Elective Total Joint Arthroplasty at a Large Urban Academic Hospital. The Journal of arthroplasty. 2016 doi: 10.1016/j.arth.2016.12.035. [DOI] [PubMed] [Google Scholar]
- 4.Dharmarajan K, Hsieh AF, Lin Z, et al. Diagnoses and timing of 30-day readmissions after hospitalization for heart failure, acute myocardial infarction, or pneumonia. Jama. 2013;309(4):355–363. doi: 10.1001/jama.2012.216476. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jencks SF, Williams MV, Coleman EA. Rehospitalizations among patients in the Medicare fee-for-service program. The New England journal of medicine. 2009;360(14):1418–1428. doi: 10.1056/NEJMsa0803563. [DOI] [PubMed] [Google Scholar]
- 6.Dimick JB, Ghaferi AA. Hospital readmission as a quality measure in surgery. Jama. 2015;313(5):512–513. doi: 10.1001/jama.2014.14179. [DOI] [PubMed] [Google Scholar]
- 7.Horwitz L, Partovian C, Lin Z, et al. In: Hospital-Wide All-Cause Unplanned Readmission Measure Final Technical Report. (CMS) CfMMS, editor. 2012. [Google Scholar]
- 8.Readmission Reduction Program (HRRP) Baltimore: Centers for Medicare and Medicaid Services; 2016. [Accessed March 11, 2017]. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/AcuteInpatientPPS/Readmissions-Reduction-Program.html. [Google Scholar]
- 9.Hospital Compare downloadable database. Baltimore: Centers for Medicare & Medicaid Services; https://data.medicare.gov/data/hospital-compare. [Google Scholar]
- 10.CMS.gov. ACO #8 Risk Standardized All Condition Readmission. Baltimore: Centers for Medicare and Medicaid Services; https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Quality-Measures-Standards.html. [Google Scholar]
- 11.Rau J. Half of Nation’s Hospitals Fail Again to Escape Medicare Readmission Penalties. 2015 Aug 3; http://khn.org/news/half-of-nations-hospitals-fail-again-to-escape-medicares-readmission-penalties/
- 12.Christina Boccuti GC. [Accessed March 10, 2017];Aiming for Fewer Hospital U-turns: The Medicare Hospital Readmission Reduction Program. 2017 http://kff.org/medicare/issue-brief/aiming-for-fewer-hospital-u-turns-the-medicare-hospital-readmission-reduction-program/
- 13.Winblad U, Mor V, McHugh JP, Rahman M. ACO-Affiliated Hospitals Reduced Rehospitalizations From Skilled Nursing Facilities Faster Than Other Hospitals. Health affairs. 2017;36(1):67–73. doi: 10.1377/hlthaff.2016.0759. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Ryan AM, Krinsky S, Adler-Milstein J, Damberg CL, Maurer KA, Hollingsworth JM. Association Between Hospitals' Engagement in Value-Based Reforms and Readmission Reduction in the Hospital Readmission Reduction Program. JAMA internal medicine. 2017 doi: 10.1001/jamainternmed.2017.0518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Bernatz JT, Tueting JL, Anderson PA. Thirty-day readmission rates in orthopedics: a systematic review and meta-analysis. PloS one. 2015;10(4):e0123593. doi: 10.1371/journal.pone.0123593. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hicks CW, Bronsert M, Hammermeister KE, et al. Operative variables are better predictors of postdischarge infections and unplanned readmissions in vascular surgery patients than patient characteristics. Journal of vascular surgery. 2016 doi: 10.1016/j.jvs.2016.10.086. [DOI] [PubMed] [Google Scholar]
- 17.Gani F, Lucas DJ, Kim Y, Schneider EB, Pawlik TM. Understanding Variation in 30-Day Surgical Readmission in the Era of Accountable Care: Effect of the Patient, Surgeon, and Surgical Subspecialties. JAMA surgery. 2015 doi: 10.1001/jamasurg.2015.2215. [DOI] [PubMed] [Google Scholar]
- 18.Kim Y, Gani F, Lucas DJ, et al. Early versus late readmission after surgery among patients with employer-provided health insurance. Annals of surgery. 2015;262(3):502–511. doi: 10.1097/SLA.0000000000001429. discussion 509–511. [DOI] [PubMed] [Google Scholar]
- 19.Feigenbaum P, Neuwirth E, Trowbridge L, et al. Factors contributing to all-cause 30-day readmissions: a structured case series across 18 hospitals. Medical care. 2012;50(7):599–605. doi: 10.1097/MLR.0b013e318249ce72. [DOI] [PubMed] [Google Scholar]
- 20.Tsai TC, Joynt KE, Orav EJ, Gawande AA, Jha AK. Variation in Surgical-Readmission Rates and Quality of Hospital Care. New England Journal of Medicine. 2013;369(12):1134–1142. doi: 10.1056/NEJMsa1303118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Jenq GY, Doyle MM, Belton BM, Herrin J, Horwitz LI. Quasi-Experimental Evaluation of the Effectiveness of a Large-Scale Readmission Reduction Program. JAMA internal medicine. 2016;176(5):681–690. doi: 10.1001/jamainternmed.2016.0833. [DOI] [PubMed] [Google Scholar]
- 22.Jack BW, Chetty VK, Anthony D, et al. A reengineered hospital discharge program to decrease rehospitalization: a randomized trial. Annals of internal medicine. 2009;150(3):178–187. doi: 10.7326/0003-4819-150-3-200902030-00007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Hamar B, Rula EY, Wells AR, Coberley C, Pope JE, Varga D. Impact of a scalable care transitions program for readmission avoidance. The American journal of managed care. 2016;22(1):28–34. [PubMed] [Google Scholar]
- 24.Birkmeyer JD, Gust C, Baser O, Dimick JB, Sutherland JM, Skinner JS. Medicare payments for common inpatient procedures: implications for episode-based payment bundling. Health services research. 2010;45(6 Pt 1):1783–1795. doi: 10.1111/j.1475-6773.2010.01150.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ibrahim AM, Nathan H, Thumma JR, Dimick JB. Impact of the Hospital Readmission Reduction Program on Surgical Readmissions Among Medicare Beneficiaries. Annals of surgery. 2017;266(4):617–624. doi: 10.1097/SLA.0000000000002368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Mehtsun WT, Papanicolas I, Zheng J, Orav EJ, Lillemoe KD, Jha AK. National Trends in Readmission Following Inpatient Surgery in the Hospital Readmissions Reduction Program Era. Annals of surgery. 2017 doi: 10.1097/SLA.0000000000002350. [DOI] [PubMed] [Google Scholar]
- 27.Borza T, Oerline MK, Skolarus TA, et al. Association of the Hospital Readmissions Reduction Program With Surgical Readmissions. JAMA surgery. 2017 doi: 10.1001/jamasurg.2017.4585. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stimson CJ, Chang SS, Barocas DA, et al. Early and late perioperative outcomes following radical cystectomy: 90-day readmissions, morbidity and mortality in a contemporary series. The Journal of urology. 2010;184(4):1296–1300. doi: 10.1016/j.juro.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 29.Dummit LA, Kahvecioglu D, Marrufo G, et al. Association Between Hospital Participation in a Medicare Bundled Payment Initiative and Payments and Quality Outcomes for Lower Extremity Joint Replacement Episodes. Jama. 2016;316(12):1267–1278. doi: 10.1001/jama.2016.12717. [DOI] [PubMed] [Google Scholar]
- 30.Medicare.gov. Accountable Care Organizations. Baltimore: The official US government site for Medicare; https://www.medicare.gov/manage-your-health/coordinating-your-care/accountable-care-organizations.html. [Google Scholar]
- 31.Research Data Assistance Center D, MN. Provider Number. 2016 https://www.resdac.org/cms-data/variables/provider-number.
- 32.Pope GC, Kautter J, Ellis RP, et al. Risk adjustment of Medicare capitation payments using the CMS-HCC model. Health care financing review. 2004;25(4):119–141. [PMC free article] [PubMed] [Google Scholar]
- 33.Jacobs BL, Zhang Y, Schroeck FR, et al. Use of advanced treatment technologies among men at low risk of dying from prostate cancer. Jama. 2013;309(24):2587–2595. doi: 10.1001/jama.2013.6882. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dimick JB, Ryan AM. Methods for evaluating changes in health care policy: the difference-in-differences approach. Jama. 2014;312(22):2401–2402. doi: 10.1001/jama.2014.16153. [DOI] [PubMed] [Google Scholar]
- 35.Lucas DJ, Haider A, Haut E, et al. Assessing readmission after general, vascular, and thoracic surgery using ACS-NSQIP. Annals of surgery. 2013;258(3):430–439. doi: 10.1097/SLA.0b013e3182a18fcc. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Karaca-Mandic P, Norton EC, Dowd B. Interaction terms in nonlinear models. Health services research. 2012;47(1 Pt 1):255–274. doi: 10.1111/j.1475-6773.2011.01314.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Herrel LA, Norton EC, Hawken SR, Ye Z, Hollenbeck BK, Miller DC. Early impact of Medicare accountable care organizations on cancer surgery outcomes. Cancer. 2016 doi: 10.1002/cncr.30111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Ai C, Norton E. Interaction Terms in Logit and Probit Models. Economics Letters. 2003;80(1):123–129. [Google Scholar]
- 39.Mora AM, Walker D. Quality Improvement Strategies in Accountable Care Organization Hospitals. Quality management in health care. 2016;25(1):8–12. doi: 10.1097/QMH.0000000000000081. [DOI] [PubMed] [Google Scholar]
- 40.Nyweide DJ, Lee W, Cuerdon TT, et al. Association of Pioneer Accountable Care Organizations vs traditional Medicare fee for service with spending, utilization, and patient experience. Jama. 2015;313(21):2152–2161. doi: 10.1001/jama.2015.4930. [DOI] [PubMed] [Google Scholar]
- 41.McWilliams JM, Hatfield LA, Chernew ME, Landon BE, Schwartz AL. Early Performance of Accountable Care Organizations in Medicare. The New England journal of medicine. 2016 doi: 10.1056/NEJMsa1600142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.CMS.gov. Fast Facts. All Medicare Shared Savings Program (Shared Savings Program) ACOs and Pioneer ACOs. Baltimore: Centers for Medicare and Medicaid Services; [Accessed March 23, 2017]. https://www.cms.gov/Medicare/Medicare-Fee-for-Service-Payment/sharedsavingsprogram/Downloads/PioneersMSSPCombinedFastFacts.pdf. [Google Scholar]
- 43.Epstein AM, Jha AK, Orav EJ, et al. Analysis of early accountable care organizations defines patient, structural, cost, and quality-of-care characteristics. Health affairs. 2014;33(1):95–102. doi: 10.1377/hlthaff.2013.1063. [DOI] [PubMed] [Google Scholar]
- 44.Zuckerman RB, Sheingold SH, Orav EJ, Ruhter J, Epstein AM. Readmissions, Observation, and the Hospital Readmissions Reduction Program. The New England journal of medicine. 2016;374(16):1543–1551. doi: 10.1056/NEJMsa1513024. [DOI] [PubMed] [Google Scholar]
- 45.Desai NR, Ross JS, Kwon JY, et al. Association Between Hospital Penalty Status Under the Hospital Readmission Reduction Program and Readmission Rates for Target and Nontarget Conditions. Jama. 2016;316(24):2647–2656. doi: 10.1001/jama.2016.18533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Siracuse BL, Chamberlain RS. A Preoperative Scale for Determining Surgical Readmission Risk After Total Hip Replacement. JAMA surgery. 2016;151(8):701–709. doi: 10.1001/jamasurg.2016.0020. [DOI] [PubMed] [Google Scholar]
- 47.Ramkumar PN, Chu CT, Harris JD, et al. Causes and Rates of Unplanned Readmissions After Elective Primary Total Joint Arthroplasty: A Systematic Review and Meta-Analysis. American journal of orthopedics (Belle Mead, NJ) 2015;44(9):397–405. [PubMed] [Google Scholar]
- 48.CMS.gov. Quality Payment Program. Baltimore: Centers for Medicare and Medicaid Services; [Accessed March 25, 2017]. https://qpp.cms.gov/ [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Digital Content Figure 1. Rate of 30-day readmission for ACO and non-ACO affiliated hospitals prior to implementation of Medicare Shared Savings Program Accountable Care Organizations. Similar trends in quarterly readmission rates are noted for both ACO and non-ACO affiliated hospitals.