Abstract
Background
The zoonotic disease Q fever is caused by Coxiella burnetii and usually affects high-risk human populations. We conducted a serological survey of dairy cattle farmers in Korea to determine seroreactivity and identify risk factors for C. burnetii infection.
Methods
This cross-sectional study included 1,824 of 7,219 dairy cattle farms (25.3%) in the study region. The selected dairy cattle farmers visited the nearest public health centers or branches with completed questionnaires. Serum samples from the farmers were tested using an indirect immunofluorescence assay to detect phase II C. burnetii immunoglobulin (Ig) G or M antibodies.
Results
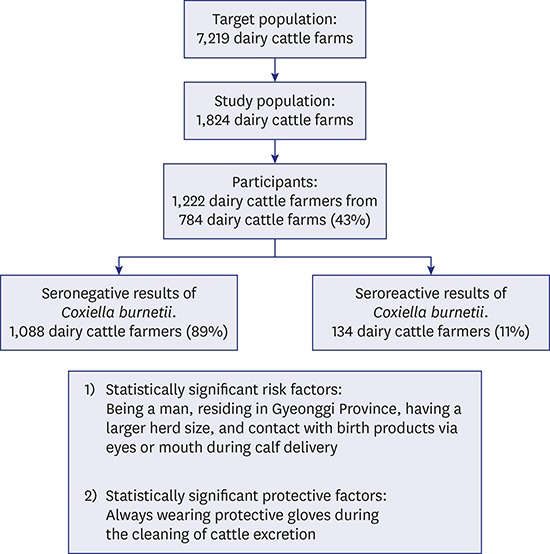
A total of 1,222 dairy cattle farmers from 784 dairy cattle farms (43.0%) participated in this study, and 11.0% (134/1,222) exhibited seroreactivity, defined as a phase II antigen IgG or IgM titer ≥ 1:16. In the multivariate analysis, male sex, residence in Gyeonggi Province, a larger herd size, and ocular/oral contact with birth products during calf delivery were significantly associated with a higher risk of C. burnetii infection. Furthermore, the risk was significantly lower among farmers who always wore protective gloves while cleaning cattle excretion, compared to those who sometimes or rarely wore protective gloves.
Conclusion
Dairy cattle farmers should exercise caution by avoiding ocular/oral contact with birth products during calf delivery and by using protective equipment (including gloves).
Keywords: Coxiella burnetii, Dairy Cattle, Farmers, Risk Factors, Serologic Tests, Korea
Graphical Abstract
INTRODUCTION
Q fever is a widespread zoonotic disease caused by Coxiella burnetii, a bacterial pathogen that frequently infects both domestic (primarily cattle, sheep, and goats) and wild ruminants.1 In animals, Q fever is usually asymptomatic or leads to reproductive disorders (e.g., abortion and stillbirth).2 In humans, acute Q fever is similarly asymptomatic in most cases, or may involve non-specific, mild influenza-like symptoms. However, a small minority of patients may develop chronic Q fever infection.3
C. burnetii is transmitted to humans mainly via the inhalation of contaminated aerosols from infected animals that have shed C. burnetii in birth products, milk, and feces,4 although the pathogen may also be transmitted via other routes, such as direct contact with contaminated materials and ingestion of unpasteurized milk.5 C. burnetii infections mostly occur among high-risk populations that have contact with animals, such as livestock farmers, slaughterhouse workers, and veterinarians.6 However, a large Q fever outbreak (> 4,000 cases) was reported in the Netherlands during 2007–2010.7
In Korea, Q fever was designated as a National Notifiable Infectious Disease in 2006, and approximately 10 cases of sporadic Q fever have been reported annually during 2006–2011.8 C. burnetii infection involves two antigenic states, phases I and II. The levels of anti-phase II antibodies are high in acute disease, whereas elevated anti-phase I antibody levels are observed in chronic disease.6 A serologic study of slaughterhouse workers in Korea identified reactive phase II antibodies among 10.2% of participants.9 However, information regarding the serologic results and risk factors of C. burnetii infection in other high-risk groups, such as dairy farmers and veterinarians, remains limited.
In the current study, dairy cattle farmers, the largest group of dairy farmers in Korea, were asked to participate in a serologic survey to evaluate the seroreactivity to C. burnetii and risk factors for infection.
Methods
Study population
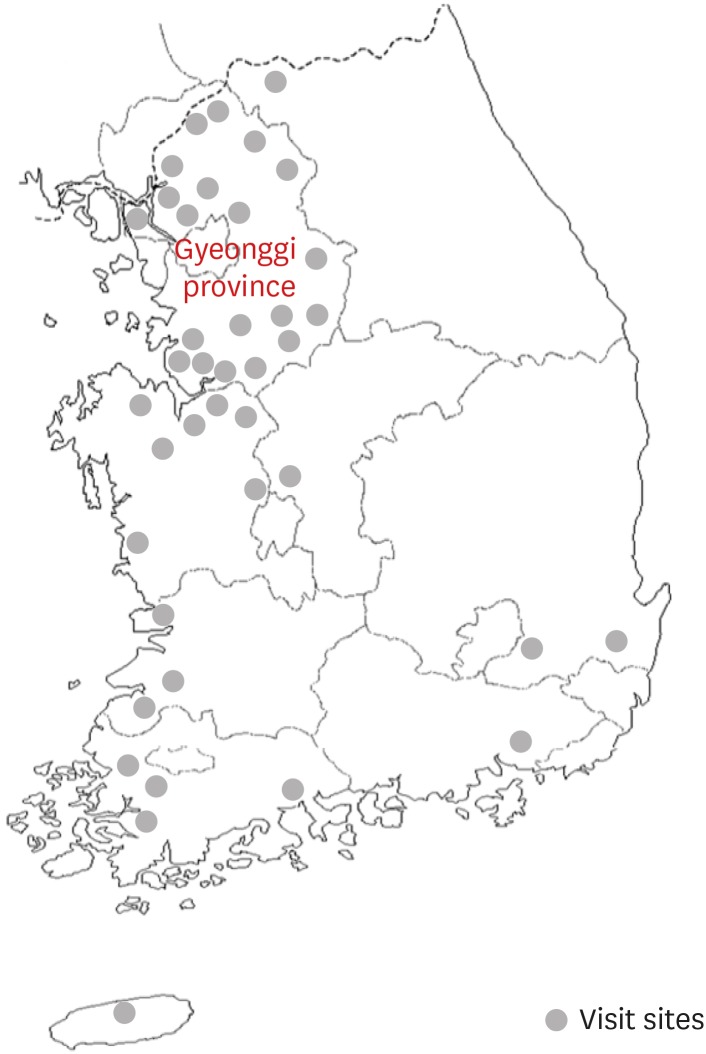
According to the Korean Statistical Information Service,10 2,889 (40.0%) and 4,330 (60.0%) dairy cattle farms were located in Gyeonggi Province and other Korean provinces, respectively, during the second quarter of 2008. In Gyeonggi Province, we selected densely populated areas with ≥ 50 dairy cattle farms per city/county/district or town/township (15 and 5 sites, respectively). In other Korean provinces, densely populated areas with ≥ 20 dairy cattle farms per town/township were selected (20 sites, Fig. 1). Of the 7,219 available dairy cattle farms, 1,824 (25.3%) were included in the study (912 farms in Gyeonggi Province and 912 farms in other Korean provinces). We requested the participation of up to 2 dairy cattle farmers per farm.
Fig. 1. Sites of serologic survey visits to evaluate the prevalence of Coxiella burnetii infection among dairy cattle farmers in Korea.
Data collection
The selected dairy cattle farms were informed about the study and received questionnaires (developed in-house) by registered mail. The questionnaires comprised inquiries about the demographic characteristics, farm-related factors, and work hygiene-related factors, with the intent to collect information about potential risk factors. The dairy cattle farmers were then requested to visit the nearest of 15 public health centers or 25 public health center branches, where researchers identified or administered the participants' questionnaires by interview during their appointments. Blood samples were also obtained from the participants for C. burnetii antibody testing. This survey was conducted during November–December 2008 in Gyeonggi Province and during June–July 2010 in other Korean provinces.
Serologic analysis
Serum samples obtained by centrifuging the collected blood were sent in a sealed icebox to the Korea Centers for Disease Control and Prevention (KCDC). An indirect immunofluorescence assay (IFA), the reference method of serologic diagnosis for Q fever,6 was used to detect phase II C. burnetii antibody immunoglobulin G (IgG) and immunoglobulin M (IgM) (Focus Diagnostics, Cyprus, CA, USA) according to the manufacturer's instruction. A positive phase II IgG or IgM antibody reaction at a dilution of ≥ 1:16 was considered seroreactive.
Statistical analysis
A univariate logistic regression was used to calculate the odds ratios (ORs) with 95% confidence intervals (95% CIs). Subsequently, variables identified as significant (P < 0.05) in the univariate analysis were included in a multivariate logistic regression. A backward stepwise logistic regression was applied, and all variables that met the 10.0% significance level in the likelihood ratio test were maintained in the final model. The indicator of statistical significance was set at < 0.05. SPSS version 17.0 (SPSS Inc., Chicago, IL, USA) was used for all analyses.
Ethics statement
This study was reviewed and approved by the Institutional Review Board of Dongguk University Gyeongju Hospital (No. 2008-08-15 and 2010-10-11). Informed consent was obtained from all participants.
Results
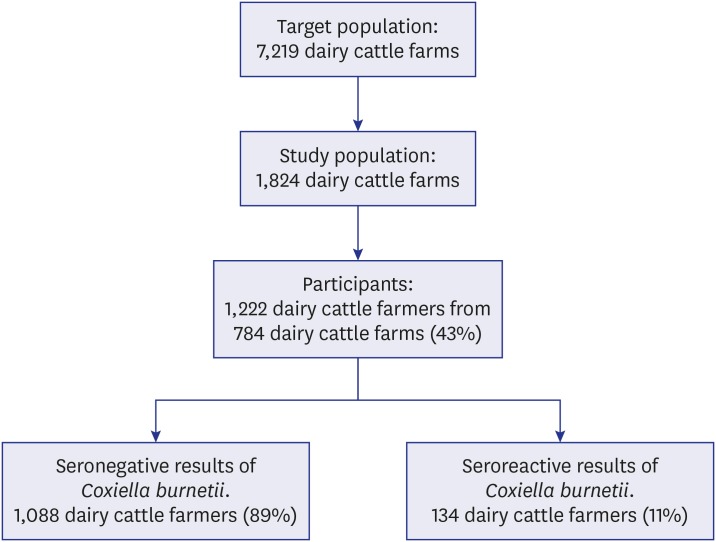
A total of 1,222 dairy cattle farmers from 784 dairy cattle farms (43.0%) participated in this study (Fig. 2), including 704 (57.6%) farmers in Gyeonggi Province and 518 (42.4%) in other provinces. The participants comprised 773 (63.3%) men and 449 (36.7%) women, with a mean age of 51.4 ± 8.9 years. The average duration of work was 20.6 ± 8.6 years, and the average herd size was 81.6 ± 69.6 dairy cattle.
Fig. 2. Flowchart of serologic study participation.
Seroreactivity of C. burnetii and serologic profiles
Overall, 134 of 1,222 participants (11.0%) exhibited seroreactivity for C. burnetii. The phase II IgG antibody titer cutoffs ranged from < 1:16 to 1:1,024, and 133 participants (10.9%) had IgG titers of ≥ 1:16. The phase II IgM antibody titer cutoffs ranged from < 1:16 to 1:16; however, only 1 participant (0.1%) had an IgM titer of ≥ 1:16 (Table 1).
Table 1. Distribution of titers against Coxiella burnetii phase II antigen among dairy cattle farmers in Korea.
| Titer | IgG | IgM |
|---|---|---|
| No. (%) | No. (%) | |
| < 1:16 | 1,089 (89.1) | 1,221 (99.9) |
| 1:16 | 31 (2.5) | 1 (0.1) |
| 1:32 | 43 (3.5) | 0 (0.0) |
| 1:64 | 30 (2.5) | 0 (0.0) |
| 1:128 | 21 (1.7) | 0 (0.0) |
| ≥ 1:256 | 8 (0.7) | 0 (0.0) |
| Total | 1,222 (100.0) | 1,222 (100.0) |
IgG = immunoglobulin G, IgM = immunoglobulin M.
Univariate analysis of C. burnetii seroreactivity and associated risk factors
Generally, sex, region, and herd size were associated with a higher risk of C. burnetii infection. Men were significantly more frequently seroreactive than women (P = 0.034), and the Gyeonggi Province region had a significantly higher prevalence of seroreactive dairy cattle farmers (P = 0.001), compared to the other provinces. A large herd size (≥ 100 dairy cattle) was significantly more likely to associate with C. burnetii seroreactivity, compared to a small herd size (< 50 dairy cattle) (OR, 1.99; 95% CI, 1.20–3.32) (Table 2). Additionally, the farming of beef or Korean native cattle was significantly associated with a lower C. burnetii infection (P = 0.002). However, the status as a farm owner or family member (P = 0.191), work type (e.g., feeding, milking, cleaning cattle excretion, compost production, calf delivery, and artificial insemination), and the consumption of raw milk were not significantly associated with C. burnetii infection (P = 0.562) (Table 3), although the latter factor was rare (4.3% of participants).
Table 2. Associations of general characteristics with Coxiella burnetii seroreactivity among dairy cattle farmers in Korea.
| Variables | Total | Seroreactivity, No. (%) | OR (95% CI) | P valuea | |
|---|---|---|---|---|---|
| Sex | |||||
| Male | 773 | 96 (12.4) | 1.53 (1.03–2.28) | 0.034 | |
| Female | 449 | 38 (8.5) | Reference | ||
| Age, yr | |||||
| < 45 | 219 | 23 (10.5) | Reference | ||
| 45–59 | 797 | 84 (10.5) | 1.00 (0.62–1.63) | 0.987 | |
| ≥ 60 | 206 | 27 (13.1) | 1.29 (0.71–2.32) | 0.406 | |
| Duration of work, yr | |||||
| < 15 | 282 | 29 (10.3) | Reference | ||
| 15–29 | 740 | 84 (11.4) | 1.12 (0.71–1.75) | 0.627 | |
| ≥ 30 | 169 | 20 (11.8) | 1.17 (0.64–2.14) | 0.609 | |
| Region | |||||
| Gyeonggi Province | 704 | 96 (13.6) | 1.99 (1.34–2.96) | 0.001 | |
| Others | 518 | 38 (7.3) | Reference | ||
| Herd size (dairy cattle) | |||||
| < 50 | 387 | 33 (8.5) | Reference | ||
| 50–99 | 610 | 67 (11.0) | 1.32 (0.85–2.05) | 0.209 | |
| ≥ 100 | 217 | 34 (15.7) | 1.99 (1.20–3.32) | 0.008 | |
| Education | |||||
| Middle school or less | 655 | 70 (10.7) | 0.94 (0.65–1.34) | 0.721 | |
| High school or more | 565 | 64 (11.3) | Reference | ||
Table 3. Associations of farm-related factors with Coxiella burnetii seroreactivity among dairy cattle farmers in Korea.
| Variables | Total | Seroreactivity, No. (%) | OR (95% CI) | P valuea | |
|---|---|---|---|---|---|
| Farm owners or their families | |||||
| Yes | 1,180 | 128 (10.8) | 0.55 (0.22–1.35) | 0.191 | |
| No | 33 | 6 (18.2) | Reference | ||
| Separation between stalls and milking parlors | |||||
| Yes | 1,037 | 118 (11.4) | Reference | ||
| No | 158 | 16 (10.1) | 0.88 (0.51–1.52) | 0.642 | |
| Purchase of dairy cattle (within 1 year) | |||||
| Yes | 232 | 24 (10.3) | 0.90 (0.57–1.44) | 0.672 | |
| No | 963 | 109 (11.3) | Reference | ||
| Farm beef or Korean native cattle | |||||
| Yes | 471 | 35 (7.4) | 0.52 (0.35–0.78) | 0.002 | |
| No | 744 | 99 (13.3) | Reference | ||
| Farm dogs | |||||
| Yes | 574 | 70 (12.2) | 1.25 (0.87–1.79) | 0.220 | |
| No | 641 | 64 (10.0) | Reference | ||
| Consumption of raw milk | |||||
| Yes | 52 | 7 (13.5) | 1.27 (0.56–2.88) | 0.562 | |
| No | 1,167 | 127 (10.9) | Reference | ||
| Feeding | |||||
| Yes | 1,053 | 114 (10.8) | 0.94 (0.56–1.57) | 0.812 | |
| No | 166 | 19 (11.4) | Reference | ||
| Milking | |||||
| Yes | 1,090 | 119 (10.9) | 0.94 (0.53–1.66) | 0.831 | |
| No | 130 | 15 (11.5) | Reference | ||
| Cleaning cattle excretion | |||||
| Yes | 1,022 | 107 (10.5) | 0.74 (0.47–1.16) | 0.193 | |
| No | 198 | 27 (13.6) | Reference | ||
| Compost production | |||||
| Yes | 796 | 90 (11.3) | 1.13 (0.77–1.65) | 0.543 | |
| No | 423 | 43 (10.2) | Reference | ||
| Calf delivery | |||||
| Yes | 1,054 | 114 (10.8) | 0.89 (0.53–1.47) | 0.637 | |
| No | 166 | 20 (12.0) | Reference | ||
| Artificial insemination | |||||
| Yes | 338 | 38 (11.2) | 1.04 (0.70–1.54) | 0.858 | |
| No | 882 | 96 (10.9) | Reference | ||
The questionnaire also solicited information about the use of personal protective equipment (e.g., glasses, masks, gloves, aprons, and boots) during work (e.g., milking, cleaning cattle excretion, artificial insemination, and calf delivery); ocular or oral contact with milk, feces, and birth products during work; and the habit of showering after work. In the univariate analysis, the ORs of C. burnetii infection were significantly lower among those who always wore protective gloves during milking (0.57; 95% CI, 0.39–0.84) and when cleaning cattle excretion (0.62; 95% CI, 0.40–0.96), compared to those who sometimes or rarely wore protective gloves. Additionally, ocular or oral contact with birth products during calf delivery had a significantly higher OR (1.50; 95% CI, 1.00–2.24), compared to no such contact with these products (Table 4). All results from the univariate analysis of the association of C. burnetii seroreactivity and work hygiene-related factors are available in the supplemental materials (Supplementary Tables 1, 2, 3, 4).
Table 4. Associations of significant (P < 0.05) work hygiene-related factors with Coxiella burnetii seroreactivity among dairy cattle farmers in Korea.
| Variables | Total | Seroreactivity, No. (%) | OR (95% CI) | P valuea | ||
|---|---|---|---|---|---|---|
| During milking | ||||||
| Wearing protective gloves | ||||||
| Always | 684 | 60 (8.8) | 0.57 (0.39–0.84) | 0.004 | ||
| Sometimes or rarely | 403 | 58 (14.4) | Reference | |||
| No milking | 130 | 15 (11.5) | 0.78 (0.42–1.42) | 0.412 | ||
| While cleaning cattle excretion | ||||||
| Wearing protective gloves | ||||||
| Always | 794 | 75 (9.4) | 0.62 (0.40–0.96) | 0.032 | ||
| Sometimes or rarely | 221 | 32 (14.5) | Reference | |||
| No cleaning | 198 | 27 (13.6) | 0.93 (0.54–1.62) | 0.804 | ||
| During calf delivery | ||||||
| Contact with birth products via eyes or mouth | ||||||
| Yes | 331 | 45 (13.6) | 1.50 (1.00–2.24) | 0.048 | ||
| No | 716 | 68 (9.5) | Reference | |||
| No calf delivery | 166 | 20 (12.0) | 1.31 (0.77–2.22) | 0.324 | ||
Multivariate analysis between C. burnetii seroreactivity and risk factors
The following factors identified as significant (P < 0.05) in the univariate analysis were included in the multivariate model: sex, region, herd size, farm beef or Korean native cattle, wearing protective gloves during milking and while cleaning cattle excretion, and ocular/oral contact with birth products during calf delivery. After a backward stepwise regression, six variables remained in the model. Of these variables, male sex (OR, 1.79; 95% CI, 1.14–2.82), residence in Gyeonggi Province (OR, 2.10; 95% CI, 1.30–3.40), a large herd size (≥ 100 dairy cattle; OR, 2.02; 95% CI, 1.18–3.45), and ocular/oral contact with birth products during calf delivery (OR, 1.54; 95% CI, 1.02–2.33) were significantly associated with a higher risk of C. burnetii infection. Furthermore, the risk of infection was significantly lower among farmers who always wore protective gloves while cleaning cattle excretion (OR, 0.63; 95% CI, 0.39–0.99), compared to those who sometimes or rarely wore protective gloves (Table 5).
Table 5. Multivariate logistic regression analysis of variables associated with Coxiella burnetii seroreactivity among dairy cattle farmers in Korea.
| Variables | OR (95% CI) | P value | |
|---|---|---|---|
| Sex | |||
| Male | 1.79 (1.14–2.82) | 0.012 | |
| Female | Reference | ||
| Region | |||
| Gyeonggi Province | 1.88 (1.24–2.86) | 0.003 | |
| Others | Reference | ||
| Herd size (dairy cattle) | |||
| < 50 | Reference | ||
| 50–99 | 1.31 (0.83–2.06) | 0.249 | |
| ≥ 100 | 2.02 (1.18–3.45) | 0.010 | |
| Farm beef or Korean native cattle | |||
| Yes | 0.66 (0.43–1.01) | 0.054 | |
| No | Reference | ||
| Wearing protective gloves during cleaning cattle excretion | |||
| Always | 0.63 (0.39–0.99) | 0.046 | |
| Sometimes or rarely | Reference | ||
| No cleaning | 1.13 (0.59–2.14) | 0.715 | |
| Contact with birth products via eyes or mouth during calf delivery | |||
| Yes | 1.54 (1.02–2.33) | 0.040 | |
| No | Reference | ||
| No calf delivery | 1.56 (0.85–2.88) | 0.154 | |
OR = odds ratio, CI = confidence interval.
Discussion
In this study, we observed an overall seroreactivity rate of 11.0% against C. burnetii and seroprevalence rate (phase II IgG or IgM titer ≥ 1:32) of 8.3% (102/1,222). These patterns applied to dairy cattle farmers nationwide. The C. burnetii seroprevalence was considerably higher among these farmers than among non-symptomatic people who attended routine health screenings in Korea (seroprevalence rate = 1.5%).11 Another Korean study of slaughterhouse workers, a high-risk group for Q fever, reported a seroreactivity rate of 10.2%, similar to that observed among dairy cattle farmers in our study.9 However, among European studies, a higher seroprevalence was reported among dairy cattle farmers in the Netherlands, compared to their Korean counterparts,12 and a study of dairy cattle farmers in Denmark reported a seropositivity rate (defined as an IgG or IgM titer ≥ 1:256) of 3.1%; again, this exceeded our findings (0.7%; 8/1,222).13 Regarding other Asian studies, a seroprevalence of 35.6% was reported among cattle farmers and farm residents in China.14 In summary, we observed reduced seroprevalence and seroreactivity among dairy cattle farmers in Korea than among their counterparts in other countries.
In Korea, dairy cattle farms are characterized by family-based management and small-scale farming; in the former, men are more likely to participate in dairy cattle farming. The male-to-female ratio of Q fever prevalence was > 2:1 in both Australia and France, where the extensive occupational exposure of men to Q fever is assumed to influence the ratio.3 Similarly, a study of dairy cattle farmers in the Netherlands reported a higher seroprevalence among men than among women.12 We additionally observed regional differences in C. burnetii seroreactivity between Gyeonggi Province and other provinces in Korea. The overall seroprevalence among dairy cattle in Korea was 25.6%, and the highest regional rate of 59.3% was observed among dairy cattle in Gyeonggi Province,11 which corresponded with the high rate of seroreactivity among dairy cattle farmers in this province. Furthermore, a large herd size was associated with C. burnetii seroreactivity in our study, consistent with a study from the Netherlands wherein the seroprevalence of C. burnetii infection among dairy cattle farmers tended to increase with herd size.12
We further identified ocular or oral contact with birth products during calf delivery as a significant correlate of C. burnetii seroreactivity. C. burnetii are present in large populations in the birth products of infected dairy cattle; accordingly, direct contact with these products facilitates the spread of infection.15,16,17 Our analysis revealed that wearing a protective mask during calf delivery was not significantly associated with C. burnetii infection. As healthcare personnel have been recommended to use N-95 masks when performing potentially aerosol-generating procedures for patients with suspected or confirmed Q fever,18 we assume that dairy cattle farmers may be using insufficiently protective masks (e.g., cloth masks and face masks). C. burnetii is similarly present in feces, therefore dairy cattle farmers should minimize fecal exposure.4 We found that among work hygiene-related factors, the consistent use of protective gloves while cleaning cattle excretion yielded a significantly lower OR for infection, compared to the occasional or infrequent use of such gloves. Full compliance with the use of gloves during and around calving was found to protect against C. burnetii infection in a cross-sectional study of dairy cattle farmers in the Netherlands.12 In summary, gloves protect the hands from direct contact with feces and might lower the risk of fecal-oral transmission.
The consumption of raw milk has also been identified as a risk factor in the transmission of C. burnetii.19 We note that dairy cattle farmers in Korea rarely consume raw milk and although this consumption was slightly more frequent among seroreactive dairy cattle farmers, it was not significantly associated with C. burnetii infection. Our univariate analysis also revealed a significantly lower number of farm beef or Korean native cattle among seroreactive dairy cattle farmers, although this significance was not maintained in the multivariate analysis. Interestingly, a previous study of the seroprevalence of C. burnetii infection among cattle in Korea observed a lower seroprevalence among Korean native cattle (1.7%) than among dairy cattle (10.5%).20
To the best of our knowledge, this was the first nationwide cross-sectional study of C. burnetii infection among dairy farmers in Korea. However, several factors might affect C. burnetii seroreactivity. First, a disproportionately large percentage of the farmers in the study were from Gyeonggi Province. Second, this study was conducted during the winter season in Gyeonggi Province and the summer season in the other provinces. As a Danish study of dairy cattle observed higher seroprevalence rates during the summer and winter,21 we must consider the potential effects of seasonal differences on seroreactivity among dairy cattle farmers in Korea.
In conclusion, we observed a C. burnetii seroreactivity rate of 11.0% among dairy cattle farmers in Korea. Our multiple logistic regression analysis led us to identify several risk factors (male sex, residence in Gyeonggi Province, larger herd size, ocular/oral contact with birth products during calf delivery) and one protective factor (wearing protective gloves while cleaning cattle excretion). To prevent C. burnetii infection, dairy cattle farmers must take precautions during calf delivery to avoid ocular or oral contact with birth products and should fully comply with the recommended use of protective equipment, including gloves.
Footnotes
Funding: This research was supported by grants (2008-S1-C-003 and 2010-E00651-00) from Korea Centers for Disease Control and Prevention.
Disclosure: The authors have no potential conflicts of interest to disclose.
Author Contributions: Conceptualization: Lim HS, Chu H. Data curation: Park JH, Yoo SJ, Chu H, Hwang KJ. Formal analysis: Park JH. Investigation: Yoo SJ, Park JH, Lim HS. Writing - original draft: Park JH.
SUPPLEMENTARY MATERIALS
Associations of work hygiene-related factors during milking with Coxiella burnetii seroreactivity among dairy cattle farmers in Korea
Associations of work hygiene-related factors while cleaning cattle excretion with Coxiella burnetii seroreactivity among dairy cattle farmers in Korea
Associations of work hygiene-related factors during artificial insemination with Coxiella burnetii seroreactivity among dairy cattle farmers in Korea
Associations of work hygiene-related factors during calf delivery with Coxiella burnetii seroreactivity among dairy cattle farmers in Korea
References
- 1.Rodolakis A. Q fever in dairy animals. Ann N Y Acad Sci. 2009;1166(1):90–93. doi: 10.1111/j.1749-6632.2009.04511.x. [DOI] [PubMed] [Google Scholar]
- 2.Guatteo R, Seegers H, Taurel AF, Joly A, Beaudeau F. Prevalence of Coxiella burnetii infection in domestic ruminants: a critical review. Vet Microbiol. 2011;149(1-2):1–16. doi: 10.1016/j.vetmic.2010.10.007. [DOI] [PubMed] [Google Scholar]
- 3.Parker NR, Barralet JH, Bell AM. Q fever. Lancet. 2006;367(9511):679–688. doi: 10.1016/S0140-6736(06)68266-4. [DOI] [PubMed] [Google Scholar]
- 4.Roest HI, Bossers A, van Zijderveld FG, Rebel JM. Clinical microbiology of Coxiella burnetii and relevant aspects for the diagnosis and control of the zoonotic disease Q fever. Vet Q. 2013;33(3):148–160. doi: 10.1080/01652176.2013.843809. [DOI] [PubMed] [Google Scholar]
- 5.Maurin M, Raoult D. Q fever. Clin Microbiol Rev. 1999;12(4):518–553. doi: 10.1128/cmr.12.4.518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Eldin C, Mélenotte C, Mediannikov O, Ghigo E, Million M, Edouard S, et al. From Q fever to Coxiella burnetii infection: a paradigm change. Clin Microbiol Rev. 2017;30(1):115–190. doi: 10.1128/CMR.00045-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Schneeberger PM, Wintenberger C, van der Hoek W, Stahl JP. Q fever in the Netherlands - 2007-2010: what we learned from the largest outbreak ever. Med Mal Infect. 2014;44(8):339–353. doi: 10.1016/j.medmal.2014.02.006. [DOI] [PubMed] [Google Scholar]
- 8.Kwak W, Chu H, Hwang S, Park JH, Hwang KJ, Gwack J, et al. Epidemiological characteristics of serologically confirmed Q fever cases in South Korea, 2006–2011. Osong Public Health Res Perspect. 2013;4(1):34–38. doi: 10.1016/j.phrp.2012.12.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Chu H, Yoo SJ, Hwang KJ, Lim HS, Lee K, Park MY. Seroreactivity to Q fever among slaughterhouse workers in South Korea. J Prev Med Public Health. 2017;50(3):195–200. doi: 10.3961/jpmph.17.017. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Korean Statistical Information Service. Number of farm and domestic animals by provinces. [Updated 2017]. [Accessed November 20, 2017]. http://kosis.kr/statHtml/statHtml.do?conn_path=K2&tblId=DT_1EO099&orgId=101#.
- 11.Kim WJ, Hahn TW, Kim DY, Lee MG, Jung KS, Ogawa M, et al. Seroprevalence of Coxiella burnetii infection in dairy cattle and non-symptomatic people for routine health screening in Korea. J Korean Med Sci. 2006;21(5):823–826. doi: 10.3346/jkms.2006.21.5.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Schimmer B, Schotten N, van Engelen E, Hautvast JL, Schneeberger PM, van Duijnhoven YT. Coxiella burnetii seroprevalence and risk for humans on dairy cattle farms, the Netherlands, 2010-2011. Emerg Infect Dis. 2014;20(3):417–425. doi: 10.3201/eid2003.131111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Bosnjak E, Hvass AM, Villumsen S, Nielsen H. Emerging evidence for Q fever in humans in Denmark: role of contact with dairy cattle. Clin Microbiol Infect. 2010;16(8):1285–1288. doi: 10.1111/j.1469-0691.2009.03062.x. [DOI] [PubMed] [Google Scholar]
- 14.Sun WW, Cong W, Li MH, Wang CF, Shan XF, Qian AD. Coxiella burnetii seroprevalence and risk factors in cattle farmers and farm residents in three Northeastern Provinces and inner mongolia autonomous region, China. BioMed Res Int. 2016;2016:7059196. doi: 10.1155/2016/7059196. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Agerholm JS. Coxiella burnetii associated reproductive disorders in domestic animals--a critical review. Acta Vet Scand. 2013;55(1):13. doi: 10.1186/1751-0147-55-13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Garcia-Ispierto I, López-Helguera I, Tutusaus J, Serrano B, Monleón E, Badiola JJ, et al. Coxiella burnetii shedding during the peripartum period and subsequent fertility in dairy cattle. Reprod Domest Anim. 2013;48(3):441–446. doi: 10.1111/rda.12095. [DOI] [PubMed] [Google Scholar]
- 17.Freick M, Enbergs H, Walraph J, Diller R, Weber J, Konrath A. Coxiella burnetii: serological reactions and bacterial shedding in primiparous dairy cows in an endemically infected herd-impact on milk yield and fertility. Reprod Domest Anim. 2017;52(1):160–169. doi: 10.1111/rda.12878. [DOI] [PubMed] [Google Scholar]
- 18.Anderson A, Bijlmer H, Fournier PE, Graves S, Hartzell J, Kersh GJ, et al. Diagnosis and management of Q fever--United States, 2013: recommendations from CDC and the Q Fever Working Group. MMWR Recomm Rep. 2013;62(RR-03):1–30. [PubMed] [Google Scholar]
- 19.Gale P, Kelly L, Mearns R, Duggan J, Snary EL. Q fever through consumption of unpasteurised milk and milk products - a risk profile and exposure assessment. J Appl Microbiol. 2015;118(5):1083–1095. doi: 10.1111/jam.12778. [DOI] [PubMed] [Google Scholar]
- 20.Lyoo KS, Kim D, Jang HG, Lee SJ, Park MY, Hahn TW. Prevalence of antibodies against Coxiella burnetii in Korean native cattle, dairy cattle, and dogs in South Korea. Vector Borne Zoonotic Dis. 2017;17(3):213–216. doi: 10.1089/vbz.2016.1977. [DOI] [PubMed] [Google Scholar]
- 21.Paul S, Agger JF, Markussen B, Christoffersen AB, Agerholm JS. Factors associated with Coxiella burnetii antibody positivity in Danish dairy cows. Prev Vet Med. 2012;107(1-2):57–64. doi: 10.1016/j.prevetmed.2012.05.015. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Associations of work hygiene-related factors during milking with Coxiella burnetii seroreactivity among dairy cattle farmers in Korea
Associations of work hygiene-related factors while cleaning cattle excretion with Coxiella burnetii seroreactivity among dairy cattle farmers in Korea
Associations of work hygiene-related factors during artificial insemination with Coxiella burnetii seroreactivity among dairy cattle farmers in Korea
Associations of work hygiene-related factors during calf delivery with Coxiella burnetii seroreactivity among dairy cattle farmers in Korea