Abstract
This study was performed to evaluate a healthcare strategy based on teleophthalmology for diagnosis and management of primary healthcare users. A descriptive cross-sectional study was conducted to review the medical records of patients from January 2013 to December 2014 from primary care units in the city of São Paulo. The units referred patients, who had diabetes or high blood pressure, and were users of chloroquine compounds, for a fundus examination. The images were sent to a reading center for review, diagnosis, and patient referrals. From 9173 analyzed patients, 570 (6.2%) were excluded because of poor image quality. Of the remaining patients, 4933 (57.3%) had diabetes, 7242 (84,2%) systemic hypertension, and 113 (1.3%) used chloroquine. Of these, 989 (11.5%) patients needed ophthalmologic treatment. The most frequently prescribed treatments were cataract extraction in 692 (70%) of 989 and photocoagulation in 245 (24.8%) of 989 cases. Overall, cataract extraction was indicated in 692 (8%) of 8603 cases and photocoagulation in 245 (2.8%) of 8603 cases. When only patients with diabetes were considered, the indication for photocoagulation increased to 4.5%.The results showed that non-medical professionals could produce good-quality ocular images for screening of ocular diseases in most cases; only 6.2% of ocular images did not meet quality requirements. Most patients referred for fundus examination did not need a specific treatment, indicating that this system could be an inexpensive and reliable tool for use in developing countries.
Key Words: Teleophthalmology, Primary Care, Diagnosis, Chloroquine, Diabetes, Hypertension
INTRODUCTION
With increasing life expectancies, there has been a concurrent increase in the number of chronic diseases that affect vision. In some diseases, ocular changes can help the primary healthcare team with diagnosis and management of the disease [1]. Therefore, preventative methods and timely diagnosis and treatment are required [2]. The high number of adults and elderly patients with visual problems and ocular diseases makes ophthalmology a healthcare service that is in high demand, worldwide [3]. One study found that ophthalmologic care represents 7.5% of all specialties in teaching hospitals of the Brazilian state of São Paulo [4]. In Brazil, as in many other countries, access to ophthalmologic examinations is limited, due to high demand and the dearth of ophthalmologists, requiring new technologies to be aggregated in the health system, in response to this growing demand [5]. The current study evaluated diagnostic modalities in Diabetes Mellitus (DM), systemic hypertension (HTN), and chronic use of chloroquine, through telemedicine, performed by nurse practitioners working in primary healthcare units. The study also analyzed the generated demands and its impact on the healthcare system with a multimodal approach.
MATERIALS and METHODS
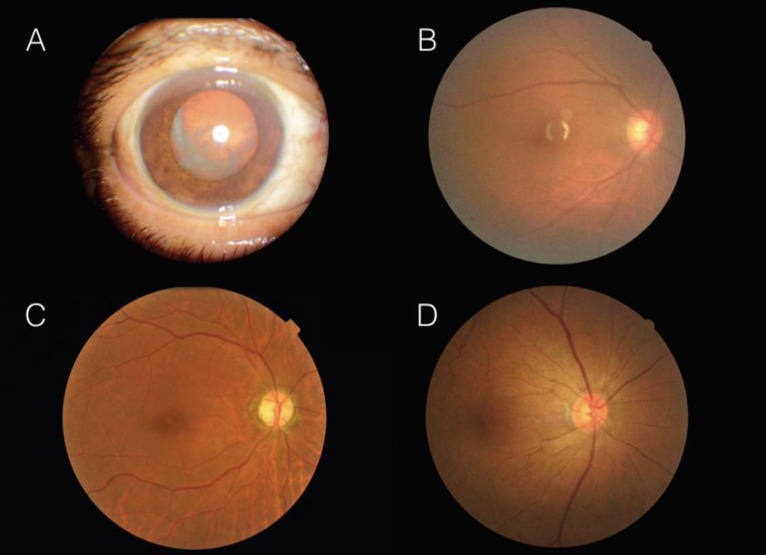
A prospective descriptive cross-sectional study was conducted and included 13 primary healthcare units of the public primary care system of the region of Vila Maria/Vila Guilherme in northern São Paulo, managed by the Paulista Association for the Development of Medicine. The Ethics Committee of the Federal University of São Paulo approved the study (110098/2015). All patients, who underwent any medical or surgical intervention, signed an informed consent. Patients with HTN or DM or those, who used chloroquine chronically, at the primary care units were referred to the study center for ocular examinations, which were conducted by non-medical health professionals, previously trained to obtain ocular images. The pupils were dilated with 1% tropicamide and images of each eye were obtained using a retina fundus camera (Canon CR2, Tokyo, Japan), according to a validated protocol that focused on the anterior segment, the macula, and the optic nerve [6]. Cataracts, classified as mild, moderate, or severe, were assessed by the ability to visualize third-, second-, and first-order retinal vessels. Patients were referred for possible cataract surgery when the lens opacification was moderate or severe (Fig 1).
Figure 1.
Images of predefined Fields of Examinations (A, C, B) and Degrees of Cataractous Opacification (A, B)
A, An anterior Segment Image with a Cataract; B, The Fundus of a Patient with a Mild Cataract with limited Observation of the Third-Order Vessels; C, A Normal Fundus with the Macula at the Center; D, An Image of the Fundus with the Optic Nerve to the Center.
Diabetic Retinopathy (DR) was categorized using the Scottish Diabetic Retinopathy screening program and adapted to the Brazilian system by Malerbi et al., where non-proliferative retinopathy is categorized as mild, moderate, or severe non-proliferative, based on the number of red dots, i.e., microaneurysms and intra-retinal hemorrhages [6, 7]. Mild DR was defined as the presence of up to three red dots on one image, moderate as four or more hemorrhages in one hemi-field, and severe as four or more red spots in both hemi-fields or intraretinal microvascular abnormalities in one quadrant and no signs of proliferation. Proliferative DR (PDR) was defined by the presence of retinal neovascularization or a vitreous or pre-retinal hemorrhage. Patients with severe Non-Proliferative or Proliferative Retinopathy (NPDR/PDR) were referred for laser photocoagulation. Retinopathy resulting from chloroquine use was evaluated according to the American Academy of Ophthalmology protocol, published by Marmor et al., which describes the presence of macular pigmentary molting with focal hypopigmentation [8]. The images were sent through a Picture Archiving and Communication System (MediViewWeb, Rio de Janeiro, Brazil), by a Digital Imaging and Communications in Medicine protocol via the Internet, to a reading center at the Vision Institute for evaluation, by an expert ophthalmologist. The results and therapeutic guidance were sent to the basic health unit of the patient via the Web. This research studied patients from January 2013 to December 2014. Underlying systemic disease, gender, age, ophthalmologic diagnosis, and the suggested approach were registered and analyzed statistically.
RESULTS
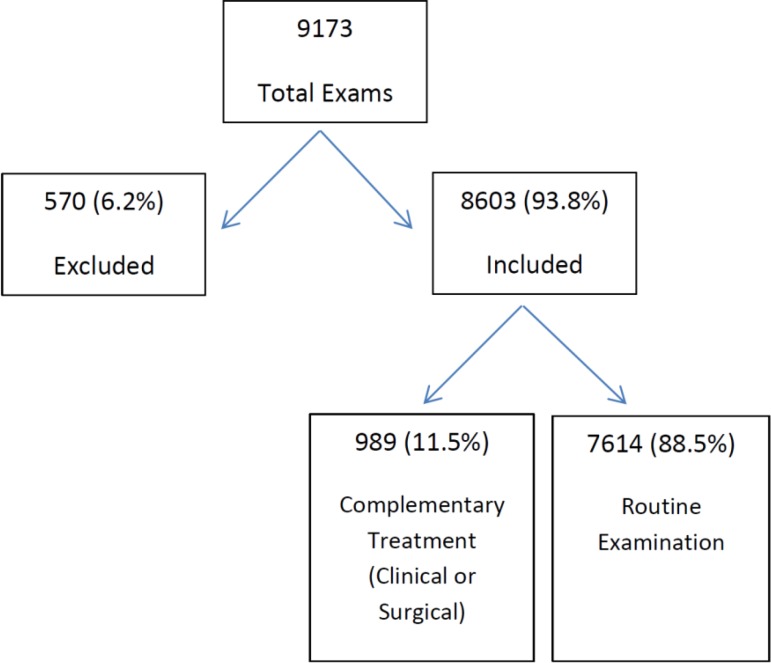
A total of 9173 patients underwent an ophthalmologic examination, of whom 570 (6.2%) were excluded because of poor image quality or the absence of the diseases under study, leaving 8603 patients (mean age, 60.2 years ± 10 years) in this study (Fig 2).
Figure 2.
Flowchart of the Studied Population
In this group, 4933 (57.3%) patients had DM, 7242 (84.2%) had HTN, and 113 (1.3%) used chloroquine. Overall, 1248 (14.5%) patients only had DM, 3685 (42.8%) had both DM and HTN, and 3557 (41.3%) only had HTN (Table 1).
Table 1.
Patient Characteristics
| Number | % | |
|---|---|---|
| Diabetes | 1,248 | 14.5 |
| Diabetes/systemic hypertension | 3,685 | 42.8 |
| Systemic hypertension | 3,557 | 41.3 |
| Use of chloroquine | 113 | 1.3 |
| Total | 8603 | 100 |
After analyzing the fundus images, 989 (11.5%) patients (mean age of 70.3 ± 11.1 years) were referred for ophthalmologic consultation; of these, 692 (8%) patients were referred for cataract surgery, 245 (2.8%) for retinal photocoagulation, 25 (0.3%) for vitrectomy, and 27 (0.3%) for other treatments (Table 2).
Table 2.
Specific Procedures following ophthalmologic consultation
| Total patients, Number (%) | Total referred, Number (%) | |
|---|---|---|
| None | 7,614 (88.5) | - (-) |
| Cataract surgery | 692 (8.0) | 692 (70.0) |
| Photocoagulation | 245 (2.8) | 245 (24.8) |
| Vitrectomy | 25 (0.3) | 25 (2.5) |
| Others | 27 (0.3) | 27 (2.7) |
| Total | 8,603 (100) | 989 (100) |
Of the 113 (1.3%) patients taking chloroquine, four (3.5%) had macular lesions associated with chloroquine toxicity. Of the 245 patients referred for photocoagulation, 220 (89.8%) patients had diabetes, of whom 1.4% had diabetic maculopathy, 24.1% PDR, and 74.5% maculopathy and PDR (Table 3).
Table 3.
Diabetic Patients indicated for Laser Photocoagulation
| Retinopathy type | Number (%) |
|---|---|
| Only diabetic retinopathy | 53 (24.1) |
| Diabetic maculopathy | 3 (1.4) |
| Diabetic retinopathy and diabetic maculopathy | 164 (74.5) |
| Total | 220 (100) |
Considering only the patients with DM (4933), 220 (4.5%) needed photocoagulation for treatment of the retinopathy.
DISCUSSION
This study found that more than half (62%) of the patients, who needed treatment were females, which was similar to other prevalence studies from São Paulo [9]. The results showed a reliable correlation in asynchronous telemedicine methods with the gold standard for many eye diseases [10]. Pereira et al. reported that during their career, 86% of the interviewees needed ophthalmologic care, and about two million (19%) of these individuals could not receive care [3]. Telemedicine can help minimize the great unmet demand in patient care that requires ophthalmologic evaluation for chronic conditions, especially when the distance to an ophthalmologist can be a significant obstacle to satisfactory diagnosis and treatment [11]. In the current study, 88.5% of patients required only ophthalmologic diagnostic support and none needed specific eye care, indicating that the waiting list for ophthalmologic appointments can be shortened. Similar data were found by de Mul et al., who showed in their study that only 11% of patients were contacted for consultation with an ophthalmologist [12]. In total, 6.2% of patients were excluded from the study, mainly because of poor image quality. In the study performed by Gonzalez et al., the losses were 13% and in the study of Pareja-Rios et al., initially, losses were 15%, decreasing to 7% at the end of the study, which can be explained by the increase in experience for performing the examination [13, 14]. Hypertensive retinopathy can remain asymptomatic for years, before presenting a more intense vascular event [15]. Complications are related to vascular injury, and in the retina, in vivo changes can be observed without invasive testing [16]. The prevalence of DM continues to grow globally, and DR is the leading cause of legal blindness in industrialized countries amongst patients between the age of 20 and 74 years old [17]. Studies conducted in São Paulo have shown that the retinal manifestations were the major causes of blindness in adults, and DR was the most frequent cause of blindness among patients referred to tertiary level care [18, 19]. Furthermore, DR is the most common complication of DM and has an established relationship with cardiovascular risk factors, such as HTN and renal failure [20]. Delayed access to diagnosis worsens ocular health, resulting in greater level of blindness and higher treatment costs. Diabetic Retinopathy is a progressive disease, in which the best results are obtained with early treatment [21].
Of the 989 patients, who needed additional assessment, cataract was the most prevalent in 692 (70.0%) patients. Studies have shown that cataract is an important cause of blindness, and this is also true in patients with DM [22]. The surgical indication rate of the current study was 8%. Thus, the findings are higher than the 2.5% rate of cataract surgeries in the general population, reported by Carlos et al. and similar to the 7.9%, reported in the São Paulo eye study [19, 23]. Retinal photocoagulation was indicated in 245 (24.8%) patients. When only patients with DM were considered, this number increased to 4.5% of the total sample. Unlike cataract surgery, which is independent of time regarding its success, laser treatment is a preventive therapy, in which the indication depends on the disease stage and timely treatment to obtain better results [24, 25].
The current research identified four (3.5%) chloroquine users with retinal injuries resulting from drugs. This medication is widely used to treat rheumatic diseases, and this group of patients usually have no access to proper eye examinations. Tests, such as visual perimetry and optical coherence tomography can identify changes in the early stages and are more efficient, however, these exams are not widely available in the Brazilian public health system while retinography is still used as a viable alternative [8].
CONCLUSION
The current study showed that non-medical professionals can produce good-quality ocular images for screening. Most patients referred for ophthalmologic examinations for fundus examinations did not need a specific treatment, indicating that this system could be a viable tool in countries, such as Brazil, in which healthcare assistance remains a challenge because of the size of the country and the dearth of doctors in certain areas. Further investigations should be conducted to better evaluate the full cost-effectiveness of this technology.
DISCLOSURE
Ethical issues have been completely observed by the authors. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. No conflict of interest has been presented.
References
- 1.Blomdahl S, Calissendorff B, Jacobsson U. Patient-focused urban tele-ophthalmology services. J Telemed Telecare. 2002;8 Suppl 2:43–4. doi: 10.1177/1357633X020080S219. pmid: 10.1177/1357633X020080S219 pmid: 12217130. [DOI] [PubMed] [Google Scholar]
- 2.Nathan DM. Diabetes: Advances in Diagnosis and Treatment. JAMA. 2015;314(10):1052–62. doi: 10.1001/jama.2015.9536. pmid: 10.1001/jama.2015.9536 pmid: 26348754. [DOI] [PubMed] [Google Scholar]
- 3.Pereira JM, Salomao SR, Cinoto RW, Mendieta L, Sacai PY, Berezovsky A, et al. [Eye care services evaluation in a low-income urban population of Sao Paulo City--Brazil] Arq Bras Oftalmol. 2009;72(3):332–40. doi: 10.1590/s0004-27492009000300010. pmid: 19668962. [DOI] [PubMed] [Google Scholar]
- 4.Belfort R, Jr 80 years of Arquivos Brasileiros de Oftalmologia (ABO) Arq Bras Oftalmol. 2018;81(1):0. doi: 10.5935/0004-2749.20180002. pmid: 10.5935/0004-2749.20180002 pmid: 29538603. [DOI] [PubMed] [Google Scholar]
- 5.Andonegui J, Serrano L, Eguzkiza A, Berastegui L, Jimenez-Lasanta L, Aliseda D, et al. Diabetic retinopathy screening using tele-ophthalmology in a primary care setting. J Telemed Telecare. 2010;16(8):429–32. doi: 10.1258/jtt.2010.091204. pmid: 10.1258/jtt.2010.091204 pmid: 20813892. [DOI] [PubMed] [Google Scholar]
- 6.Malerbi FK, Morales PH, Farah ME, Drummond KR, Mattos TC, Pinheiro AA, et al. Comparison between binocular indirect ophthalmoscopy and digital retinography for diabetic retinopathy screening: the multicenter Brazilian Type 1 Diabetes Study. Diabetol Metab Syndr. 2015;7:116. doi: 10.1186/s13098-015-0110-8. pmid: 10.1186/s13098-015-0110-8 pmid: 26697120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Philip S, Fleming AD, Goatman KA, Fonseca S, McNamee P, Scotland GS, et al. The efficacy of automated "disease/no disease" grading for diabetic retinopathy in a systematic screening programme. Br J Ophthalmol. 2007;91(11):1512–7. doi: 10.1136/bjo.2007.119453. pmid: 10.1136/bjo. 2007.119453 pmid: 17504851. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Marmor MF, Carr RE, Easterbrook M, Farjo AA, Mieler WF. American Academy of O Recommendations on screening for chloroquine and hydroxychloroquine retinopathy: a report by the American Academy of Ophthalmology. Ophthalmology. 2002;109(7):1377–82. doi: 10.1016/s0161-6420(02)01168-5. pmid: 12093666. [DOI] [PubMed] [Google Scholar]
- 9.Schmidt MI, Duncan BB, Hoffmann JF, Moura L, Malta DC, Carvalho RM. Prevalence of diabetes and hypertension based on self-reported morbidity survey, Brazil, 2006. Rev Saude Publica. 2009;43 Suppl 2:74–82. doi: 10.1590/s0034-89102009000900010. pmid: 19936501. [DOI] [PubMed] [Google Scholar]
- 10.Tan JC, Poh EW, Srinivasan S, Lim TH. A pilot trial of tele-ophthalmology for diagnosis of chronic blurred vision. J Telemed Telecare. 2013;19(2):65–9. doi: 10.1177/1357633x13476233. pmid: 10.1177/1357633X13476233 pmid: 23520212. [DOI] [PubMed] [Google Scholar]
- 11.Blomdahl S, Maren N, Lof R. Tele-ophthalmology for the treatment in primary care of disorders in the anterior part of the eye. J Telemed Telecare. 2001;7 Suppl 1:25–6. doi: 10.1177/1357633X010070S110. pmid: 10.1177/1357633X010070S110 pmid: 11576480. [DOI] [PubMed] [Google Scholar]
- 12.de Mul M, de Bont AA, Reus NJ, Lemij HG, Berg M. Improving the quality of eye care with tele-ophthalmology: shared-care glaucoma screening. J Telemed Telecare. 2004;10(6):331–6. doi: 10.1258/1357633042602107. pmid: 10.1258/1357633042602107 pmid: 15603630. [DOI] [PubMed] [Google Scholar]
- 13.Pareja-Rios A, Bonaque-Gonzalez S, Serrano-Garcia M, Cabrera-Lopez F, Abreu-Reyes P, Marrero-Saavedra MD. Tele-ophthalmology for diabetic retinopathy screening: 8 years of experience. Arch Soc Esp Oftalmol. 2017;92(2):63–70. doi: 10.1016/j.oftal.2016.08.006. pmid: 10.1016/j.oftal.2016.08.006 pmid: 27756515. [DOI] [PubMed] [Google Scholar]
- 14.Gonzalez F, Iglesias R, Suarez A, Gomez-Ulla F, Perez R. Teleophthalmology link between a primary health care centre and a reference hospital. Med Inform Internet Med. 2001;26(4):251–63. doi: 10.1080/14639230110082424. pmid: 11783710. [DOI] [PubMed] [Google Scholar]
- 15.Arriozola-Rodriguez KJ, Serna-Ojeda JC, Martinez-Hernandez VA, Rodriguez-Loaiza JL. Hypertensive Retinopathy as the First Manifestation of Advanced Renal Disease in a Young Patient: Report of a Case. Case Rep Ophthalmol. 2015;6(3):415–9. doi: 10.1159/000442660. pmid: 10.1159/000442660 pmid: 26955342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Grunwald JE, Alexander J, Ying GS, Maguire M, Daniel E, Whittock-Martin R, et al. Retinopathy and chronic kidney disease in the Chronic Renal Insufficiency Cohort (CRIC) study. Arch Ophthalmol. 2012;130(9):1136–44. doi: 10.1001/archophthalmol.2012.1800. pmid: 10.1001/archophthalmol. 2012.1800 pmid: 22965589. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Cheung N, Mitchell P, Wong TY. Diabetic retinopathy. Lancet. 2010;376(9735):124–36. doi: 10.1016/S0140-6736(09)62124-3. pmid: 10.1016/S01 40-6736(09)62124-3 pmid: 20580421. [DOI] [PubMed] [Google Scholar]
- 18.Araujo Filho A, Salomao SR, Berezovsky A, Cinoto RW, Morales PH, Santos FR, et al. Prevalence of visual impairment, blindness, ocular disorders and cataract surgery outcomes in low-income elderly from a metropolitan region of Sao Paulo--Brazil. Arq Bras Oftalmol. 2008;71(2):246–53. doi: 10.1590/s0004-27492008000200021. pmid: 18516427. [DOI] [PubMed] [Google Scholar]
- 19.Salomao SR, Cinoto RW, Berezovsky A, Araujo-Filho A, Mitsuhiro MR, Mendieta L, et al. Prevalence and causes of vision impairment and blindness in older adults in Brazil: the Sao Paulo Eye Study. Ophthalmic Epidemiol. 2008;15(3):167–75. doi: 10.1080/09286580701843812. pmid: 10.1080/09286 580701843812 pmid: 18569812. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Yau JW, Rogers SL, Kawasaki R, Lamoureux EL, Kowalski JW, Bek T, et al. Global prevalence and major risk factors of diabetic retinopathy. Diabetes Care. 2012;35(3):556–64. doi: 10.2337/dc11-1909. pmid: 10.2337/dc11-1909 pmid: 22301125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Mohamed Q, Gillies MC, Wong TY. Management of diabetic retinopathy: a systematic review. JAMA. 2007;298(8):902–16. doi: 10.1001/jama.298.8.902. pmid: 10.1001/jama.298.8.902 pmid: 17712074. [DOI] [PubMed] [Google Scholar]
- 22.Schellini SA, Carvalho GM, Rendeiro FS, Padovani CR, Hirai FE. Prevalence of diabetes and diabetic retinopathy in a Brazilian population. Ophthalmic Epidemiol. 2014;21(1):33–8. doi: 10.3109/09286586.2013.868004. pmid: 10.3109/092865 86.2013.868004 pmid: 24467560. [DOI] [PubMed] [Google Scholar]
- 23.Carlos GA, Schellini SA, Espindola RF, Lana FP, Rodrigues AC, Padovani CR. Cataract prevalence in Central-West region of Sao Paulo State, Brazil. Arq Bras Oftalmol. 2009;72(3):375–9. doi: 10.1590/s0004-27492009000300018. pmid: 19668970. [DOI] [PubMed] [Google Scholar]
- 24.Royle P, Mistry H, Auguste P, Shyangdan D, Freeman K, Lois N, et al. Pan-retinal photocoagulation and other forms of laser treatment and drug therapies for non-proliferative diabetic retinopathy: systematic review and economic evaluation. Health Technol Assess. 2015;19(51):v–xxviii, 1-247. doi: 10.3310/hta19510. pmid: 10.3310/hta19510 pmid: 26173799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Stitt AW, Curtis TM, Chen M, Medina RJ, McKay GJ, Jenkins A, et al. The progress in understanding and treatment of diabetic retinopathy. Prog Retin Eye Res. 2016;51:156–86. doi: 10.1016/j.preteyeres.2015.08.001. pmid: 10.1016/j.preteyeres.2015.08. 001 pmid: 26297071. [DOI] [PubMed] [Google Scholar]