Abstract
Patients with high hyperopia are generally confined to either spectacle wear or contact lenses as a primary means of refractive correction. For this patient population, the surgical corrective methods, such as hyperopic laser assisted in-situ keratomileusis (LASIK) and photorefractive keratectomy (PRK) are imperfect options due to induction of higher-order aberrations, optical regression, and loss of best corrected distance visual acuity. Recently, there has been growing interest in lenticule implantation underneath a flap via lenticule intrastromal keratoplasty (LIKE) for high hyperopia correction (+3 diopters to +10 diopters). We instead propose a modified surgical technique (small-incision lenticule intrastromal keratoplasty, sLIKE), in which the lenticule is implanted inside an intrastromal pocket thereby causing less injury to the subbasal nerve plexus injury, less postoperative dry eye symptoms, less reduction in biomechanical strength, and lower chances for epithelial ingrowth. We provide an overview of these novel surgical techniques to treat high hyperopia, and compare the associated advantages and disadvantages. In addition, we will discuss the enhancement options and methods of optimization for both surgical techniques.
Key Words: Small-Incision Lenticule Intrastromal Keratoplasty (sLIKE), Hyperopia, Lenticule Intrastromal Keratoplasty (LIKE), Small-Incision Lenticule Extraction (SMILE), Hyperopia treatment, lenticule implantation
INTRODUCTION
In the United States, approximately 4% of the population, or around 14 million individuals, have hyperopia [1]. The condition can often be treated using eyeglasses or contact lenses, or by a surgical approach. For instance, the use of hyperopic LASIK when preoperative sphere is less than +5 diopters (D) has shown to be an effective and safe procedure with minimal loss of best corrected visual acuity [2-4]. However, LASIK is an imperfect option in those with higher degrees of hyperopia, such as those with great than +5.0 D. The major impediments include induction of higher-order aberrations (HOAs), [5, 6] loss of best corrected visual acuity [3], and epithelial hyperplasia leading to optical regression [7]. Even with the newest-generation excimer laser with improved software and tracking capabilities, there can be significant loss of best corrected distance visual acuity [8].
The implantation of corneal lenticules, which initially originated from extracted small incision lenticule extraction (SMILE) procedures, have shown promising results in animal studies and human case reports [9, 10], as possibly a more effective modality than LASIK to treat high hyperopia. There are two possible surgical alternatives to the lenticule implantation procedure. One is termed Lenticule Intrastromal Keratoplasty (LIKE™), coined by Theo Seiler, in which a flap is created to visualize the stromal bed and a lenticule is centrally positioned on the optical axis [11]. The second is a slight modification of this method, which we term small-incision lenticular intrastromal keratoplasty (sLIKE). In this method, the lenticule is inserted into a stromal pocket via small-incisions without the creation of a flap. We briefly discuss the technique of LIKE and compare that with sLIKE. Our aim is to provide an overview of these novel surgical techniques to treat high hyperopia, and particularly discuss why we believe sLIKE may have slight theoretical advantages over LIKE in reducing certain inevitable complications. We will also discuss re-treatment strategies for residual refractive error and methods of optimization for both techniques.
SURGICAL TECHNIQUE
Lenticule Harvesting Options
A lenticule used for hyperopia correction can be harvested by three methods. Once the tissue is serologically cleared, it can be used for re-implantation into a recipient’s cornea. First, a lenticule can be obtained from a previous myopic (-3D to -10D) SMILE donor [12]. Second, a lenticule of the same power range can also be obtained from a human cadaver eye by using an artificial anterior chamber maintainer. Notably, these lenticules are usually between 6 millimeters (mm) and 6.5 mm in diameter. Lastly, the lenticule can be derived from the FDA approved Gebauer SLc Expert Medizintechnik GmbH device (75252 Neuhausen, Germany) [11]. A lenticule from Gebauer can be ordered directly online through the company website and sent through the Georgia Eye Bank (Georgia Eye Bank Inc., Georgia, Atlanta 30342). Upon ordering, the lenticule will be sent in a preserved environment with the correct pre-marked orientation. A hyperopic lenticule comes in either a 7 mm or 8 mm diameter with Dioptric (D) power ranging from +1.0 to +12.0, although different sizes can be requested.
Lenticule Implantation Procedures
Lenticule Intrastromal Keratoplasty (LIKE)
A flap with a diameter of at least 10.0 mm and a thickness of approximately 110 µm is created with oblique side cuts at 45° using a femtosecond laser. The pre-cut donor lenticule, from any one of the aforementioned harvesting options with +3 to +10 D of power and a diameter of 7 mm, is rinsed in balanced salt solution. Subsequently, the lenticule is positioned under the flap and centered on the optical axis. The lenticule is spread until flat. The flap is then aligned carefully ensuring that the lenticule does not shift during the flap repositioning [11].
Small-Incision Lenticule Intrastromal Keratoplasty (sLIKE)
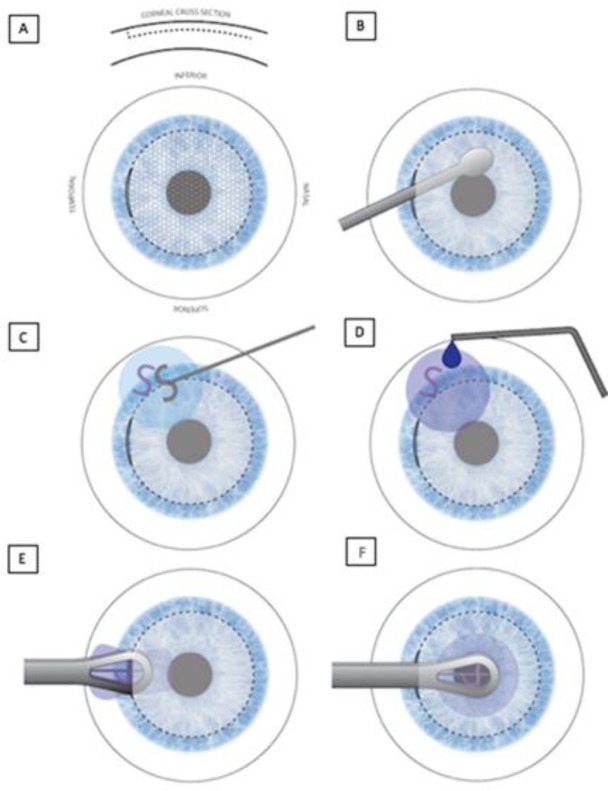
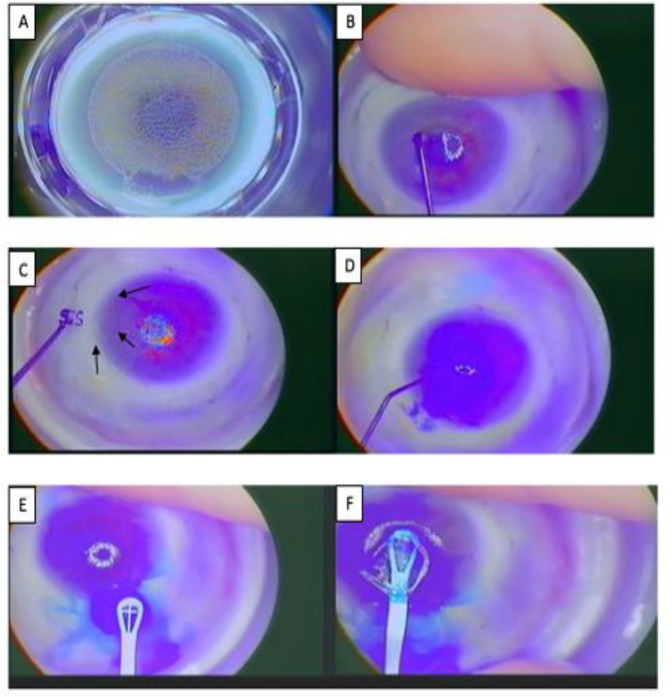
Using a femtosecond laser, a 8 mm to 9 mm diameter pocket is created at the depth of 120 µm with 5mm incision at 0º Meridian (Fig 1a). The incision is opened with a spatula and the plane of the pocket is dissected (Fig 1b). A dried lenticule is then placed on the corneal surface and marked with an “S” to indicate anterior orientation (Fig 1c). The lenticule is then soaked in 0.06% Trypan Blue Ophthalmic solution (VisionBlue® 3214 VN Zuidland, The Netherlands; Fig 1d) for 45 seconds, and subsequently, irrigated with saline to rid any excess staining. The staining will help facilitate easier centration of the lenticule. The lenticule is then inserted into the pocket using a special forceps delivery (Fig 1e & 1f; similar to KAMRA corneal inlay insertion forceps) while maintaining correct orientation via the “S” mark. The lenticule is then aligned with respect to the visual axis and pupillary center and spread out inside the stromal pocket. The actual photographic snapshots of this surgery on a cadaver eye are shown in Fig 2A-2F. Although the risk of stromal rejection is low and not as severe as endothelial rejection, we still recommend a short postoperative course of topical corticosteroids to reduce the risk of stromal rejection [13]. This will also help reduce any potential toxicity from lenticule staining.
Figure 1.
In this schematic of small-incision lenticule intrastromal keratoplasty (sLIKE), a femtosecond laser was used to create a 9 millimeter diameter pocket with depth of 120 micrometer and 5 millimeter wide incisions at 0º Meridien (A). A spatula was used to dissect the plane of the pocket (B). The lenticule was then placed on the surface of the cornea and marked with an “S” to indicate anterior orientation (C). Subsequently, the lenticule was soaked in 0.06% Trypan blue solution for approximately 45 seconds (D). Using special forceps delivery, the lenticule was placed inside the previously dissected intrastromal pocket in the correct orientation (E & F).
Figure 2.
In this cadaver eye model, the same steps outlined in Figure 1 are shown here
Management of Residual Refractive Error after LIKE & sLIKE
From prior studies, it is very likely that lenticule implantation from both techniques will likely result in a residual refractive error that will need re-treatment [9, 12, 14]. We believe that once refractive stability has been obtained by two consecutive refractions over the course of three months, surgical enhancement of any residual error can be performed after either LIKE or sLIKE.
LIKE Enhancement
In the case the patient needs enhancement of a prior LIKE procedure, this can be accomplished by re-lifting the flap and performing topography-guided or conventional ablation to correct for any residual myopia, hyperopia, and/or astigmatism. While re-lifting the flap, it is important to exercise caution and avoid inadvertent lifting of the lenticule. Following re-treatment, the flap is repositioned in the normal routine manner [11, 15].
sLIKE Enhancement
The cap used in the primary procedure can be converted into a femtosecond LASIK flap using any of the femtosecond platforms at a later postoperative period (e.g., 3 months). There are two methods of carrying this out: the side cut only [16, 17] (Fig 3) or the CIRCLE method [16, 18] (Fig 4). The type of enhancement option can be dictated by the platform that was initially chosen for primary treatment. For example, if a surgeon used IntraLase Femtosecond Advanced (iFS) or Wavelight FS200 Femtosecond Laser (FS200) for the initial sLIKE procedure, we recommend using the side cut only technique since these platforms do not support CIRCLE software.
Figure 3.
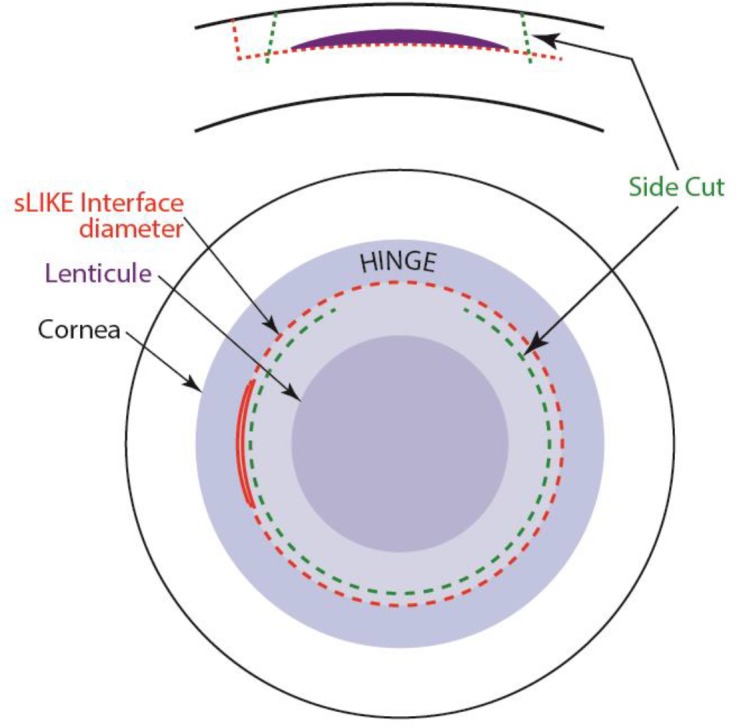
A schematic corresponding the cross-sectional view of side cut only to the surgeon’s view. The side cut will be inside the original small-incision lenticule extraction (SMILE) incision in side cut only. The cut will be inside the clearance zone but outside the optical zone
Figure 4.
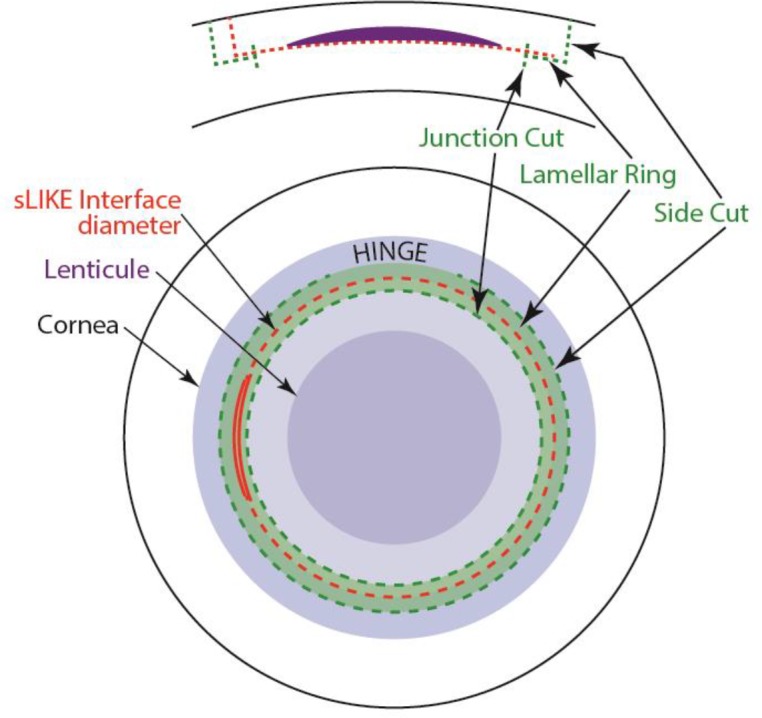
A schematic corresponding the cross-sectional view of CIRCLE to the surgeon’s view. The side will be outside the original small-incision lenticule extraction (SMILE) incision in CIRCLE. This option will create a lamellar ring adjacent to the cap to meet the side cut in the clearance zone with the help of a junction cut. The ring pattern created by the femtosecond laser cuts is demonstrated
In contrast, if a surgeon used VisuMax femtosecond laser (VisuMax) for the initial sLIKE procedure, we recommend using CIRCLE software for enhancement since this is ideal for smaller pockets and flaps.
Once the flap is created using either technique, the flap edge will be lifted using a Sinskey hook under a surgical microscope similar to a standard LASIK procedure. The flap will be retracted fully to the hinge using a blunt spatula with caution to avoid inadvertent lifting of the lenticule as aforementioned. The appropriate excimer laser treatment will be applied to correct any refractive residual error in the form of residual hyperopia, myopia, and/or astigmatism. The following two paragraphs will describe the detail parameters for each enhancement technique post-sLIKE.
Side Cut Only Method (iFS or FS200; Fig 3 )
Using the side cut only method, a side cut is created to meet the cap cut within the clearance zone but outside the optical zone. A 9 mm cap size is used with a standard 7 mm lenticule. However, a smaller lenticule diameter or one as large as 8 mm can be used in this technique. With a 7 mm lenticule, this set up results in a 1.0 mm-wide clearance zone on each side. The femtosecond laser settings will include 8.0 mm flap diameter, perpendicular side cut depth of 140 µm (in order ensure we are beyond the original 120 µm pocket depth), and a side cut angle between 75° to 90° to prevent any chance the side cut interferes with the optical zone (Table 1; Fig 3). The flap with a hinge of 5.0 mm width is made at 90° away from the original pocket incision of sLIKE.
Table 1.
The enhancement parameters post small incision lenticule intrastromal keratoplasty (sLIKE)
| Method | Cap Diameter | Flap diameter | Lenticule diameter | Side Cut Depth | Side Cut Angle | Hinge Position | Junction Diameter | Junction Upper Depth | Junction Lower Depth |
|---|---|---|---|---|---|---|---|---|---|
| Side Cut Only | 9.0 mm | 8.0 mm | 7 mm or less* | 140 µm | 75-90º | Superior | NA | NA | NA |
| CIRCLE | 7.5 mm | 7.9 mm | 6.5 mm or less | 120 µm | 90º | Superior | 6.9 mm | 100 µm | 140 µm |
As large as 8mm may be used depending on surgeon preference.
CIRCLE Method (VisuMax; Fig 4 )
The CIRCLE option allows the creation of three fundamental components: lamellar ring, side cut with hinge, and a junction cut. This option will create a lamellar ring adjacent to the cap to meet the side cut in the clearance zone with the help of a junction cut. The femtosecond laser parameters can be adjusted to produce these three basic components. The cap size will be 7.5 mm with a lenticule diameter of 6.5 mm or less. This set up results in a 0.5 mm-wide clearance zone on each side. The VisuMax laser settings will include 7.9 mm lamellar diameter with junction diameter of 6.9 mm, side cut depth of 120 µm, and side cut angle at 90 degrees (Table 1; Fig 4). The flap with a hinge of 5.0 mm width is made 90° away from the initial sLIKE incision. A 40 µm vertical junction will extend both anteriorly and posteriorly from the lamellar ring. The junctional upper depth and junctional lower depth are 100 µm and 140 µm, respectively.
DISCUSSION
The extraction of a whole lenticule from a myopic SMILE or using the Gebauer SLc Expert to harvest new lenticules opens up the possibility of re-implanting these lenticules to correct severe hyperopia. This may be a better alternative to hyperopic LASIK since the shape of the cornea is more natural following tissue addition rather than tissue substraction [19]. The idea of lenticule implantation was first described by Ignacio Barrquer in 1980 in which a disc of corneal tissue with the correct refractive power can be inserted into an instrastromal pocket [20]. In 2013, Pradhan et al [12] described the first case of an allogenic -10.50 D lenticule implanted into an aphakic patient with +11.25 D and reduced the SE to +6.00 D of hyperopia using a small incision. Furthermore, Ganesh et al [19] demonstrated the implantation of cryopreserved lenticules in eight hyperopic eyes via a small incision.
Recently, Theo Seiler popularized the technique of LIKE, in which a thick lenticule is deposited under a flap. We present a modification of this technique, termed sLIKE. In the method described, we chose to deposit the thick lenticule inside a minimally invasive pocket incision instead of underneath a flap. Similar to SMILE, the creation of a pocket via small-incisions peripherally avoids invasive damage to the anterior surface of the cornea. Theoretically, this would result in less injury to the subbasal nerve plexus [21], less flap-related complications (see below), less reduction in biomechanical strength [22, 23], and less dry eye symptoms (Table 2). For example, Denoyer et al [24] showed not only that corneal nerve density is higher but also that patients required less tear substitutes for dry eye symptoms when the procedure involved using a small-incision was created versus making a flap.
Table 2.
Comparing the advantages and disadvantages of LIKE versus sLIKE for high hyperopia treatment
| Advantages | Disadvantages | |
|---|---|---|
| LIKE | Surgical approach similar to LASIK Easier centration Simple and straightforward enhancement (flap re-lift), if needed Preliminary evidence shows efficacy and safety |
Increased risk for epithelial ingrowth Higher risk for dry eyes Significant weakening of corneal biomechanics Higher risk for DLK Other flap-related complications Flap size of at least 10 mm is difficult to create on most FS platforms |
| sLIKE | Less weakening of corneal biomechanics Less dry eye symptoms Less risk for epithelial ingrowth Less risk for DLK No flap |
More surgically challenging More difficult centration Use of dye Converting cap-to-flap for enhancement purposes can be more challenging |
sLIKE: Small-Incision Lenticule Intrastromal Keratoplasty; LIKE: Lenticule Intrastromal Keratoplasty; LASIK: Laser Assisted in-situ Leratomileusis; DLK: Diffuse Lamellar Keratitis; FS: femtosecond.
Although the optimal depth of implantation is quite debatable, we chose to make the intrastromal pocket more shallow (120 µm) than deep. It has been demonstrated that if a lenticule is implanted more shallow in the corneal stroma (i.e., 110 µm depth vs. 160 µm depth), a greater percentage of the intended correction is achieved due to greater anterior stromal steepening and less posterior stromal flattening [9]. However, other studies have demonstrated that increasing the depth of implantation induces less inflammatory changes [25], less reduction in relative tensile strength [26, 27], and possibly less visual symptoms. We hypothesize that the shallower the implantation, the greater the likelihood of achieving emmetropia or the greater risk of overcorrecting rather than undercorrecting due to more significant anterior stromal steepening. We opined that erring on the side of overcorrection is the more judicious decision since correction of myopic astigmatism is more efficacious than correction in the form of a hyperopic astigmatism. Moreover, in order to prevent instances of undercorrection, we recommend using a lenticule with a slightly higher plus power than one would normally use based on the patients’ cycloplegic refraction to achieve emmetropia.
Based on the available evidence, we feel comfortable proposing two methods of enhancement for post-sLIKE eyes. One is the CIRCLE option that can be used in those who have a VisuMax platform. In SMILE re-treatment, this method has been shown to be safe and effective [18, 28]. Importantly, there is substantial evidence to support the observations that the flap is easily lifted and the flap-bed surface is smooth and undisrupted [17, 18, 28]. This method can be adopted quickly by surgeons familiar with SMILE and the CIRCLE enhancement software. Additionally, the smaller pocket size in the CIRCLE option may allow for better centration. However, VisuMax is unable to create flap diameters as large as the other two femtosecond lasers. The resulting reduced treatment area may make it a less ideal approach for residual hyperopic enhancement. With this method, it’s important to ensure the patient will be overcorrected rather than undercorrected. This may include reducing the cap depth to 110 µm. For surgeons without the VisuMax platform, a side cut only method can be used via iFS or FS200. Using these femtosecond lasers, a much larger pocket and flap size can be generated. Thus, this enhancement option is more effective for hyperopia treatment (undercorrected patients) since it has the capability to ablate more peripheral tissue. However, this may make centration more difficult. A comprehensive list of advantages and disadvantages of both recommended enhancement techniques is provided in Table 3. We do not feel comfortable recommending a thin-flap LASIK given the elevated risk for bubble gas breakthrough or buttonhole that could result in an irregular astigmatism that may not be amenable to treatment. If the cap depth is increased, this option may be another safe alternative. Surface ablation is also another alternative, however due to the accompanying pain, postoperative haze, and slower visual recovery, this may not be an attractive option for patients.
Table 3.
Comparing the advantages and disadvantages of the two recommended enhancement options after small-incision lenticule intrastromal keratoplasty (sLIKE).
| Advantages | Disadvantages | |
|---|---|---|
| CIRCLE | Can be adopted quickly by surgeons who routinely perform SMILE Flap easily lifted and flap-bed surface is smooth and undisrupted Biomechanically more friendly because flaps are smaller Has shown to be effective and safe in SMILE enhancement |
CIRCLE software only available on VisuMax platform |
| Side Cut Only | Side cut software is available on all existing femtosecond platforms (iFS, FS200, and VisuMax) Flap easily lifted and flap-bed surface is smooth and undisrupted |
Biomechanically less friendly because flaps are larger |
SMILE: Small-Incision Lenticule Extraction; iFS: IntraLase Femtosecond; FS200: Femtosecond 200
The creation of a flap in LIKE poses various challenges that may not be present when using sLIKE. For instance, having the flap overlay a thick lenticule in LIKE may increase the chance for poor adhesion and dislocation of the flap edge. This would likely cause a large gutter between the edge of the flap and attachment point on the stroma. We know from past studies that poor adhesion and dislocation of the flap edge is recognized as a significant risk factor for post-LASIK epithelial ingrowth [29]. Literature has also associated hyperopic LASIK as a significant risk factor in epithelial ingrowth due to the ablation-induced conformational change closer to the flap edge (i.e., the mid-periphery of the cornea) [30]. Given that a hyper-oblate lenticule used to correct hyperopia would also cause a similar mid-periphery conformation change, we can extrapolate that a similar risk factor would exist in LIKE. Furthermore in LIKE, the flap is re-lifted after 1 to 3 months once stability in refraction has been achieved to enhance the refraction over the lenticule via an excimer laser. Literature has shown that the risk of epithelial ingrowth is about 1% to 3% post-LASIK. However, the risk significantly increased by up to 10-20% when the same flap is re-lifted for enhancement [31]. The additive nature of all these risk factors may increase the likelihood of epithelial ingrowth towards the visual axis leading to significant visual disturbances, irregular astigmatism, and possibly flap necrosis [32, 33]. In contrast, sLIKE uses a small incision for lenticule implantation and minimizes re-lifting of the same flap for enhancement. Consequently, this may decrease the overall likelihood for epithelial ingrowth.
We believe the use of collagen cross-linking may improve both of these surgical enhancements. Optical regression due to peripheral ring hyperplasia of the corneal epithelium is one of the major challenges preventing hyperopic LASIK from obtaining good visual outcomes [7]. Hence, it was proposed that lenticule re-implantation using either LIKE or sLIKE may prevent this complication since it avoids ablation of the peripheral cornea. A recent study by Williams et al [10] demonstrated the first comprehensive evaluation comparing all modalities for hyperopia in non-human primates. Surprisingly, their findings illustrated that lenticular implantation had a greater likelihood of optical regression than either LASIK or SMILE when correcting for lower hyperopia (+2.0 D) than higher hyperopia (+4.0 D). Additionally, lenticule implantation is associated with significant increases in the thickness of the central and mid-peripheral cornea. Although this tissue remodeling may help treat advanced keratoconus [9, 34], it may be a deterrent in achieving good visual outcomes from LIKE or sLIKE for hyperopia. Previous studies have shown that collagen cross-linking using riboflavin can slow epithelial hyperplasia and help ameliorate the accompanying optical regression [35]. Thus, prophylactic collagen cross-linking of the lenticule after implantation may help reduce some of the regression found in animal studies and improve visual outcomes for both LIKE and sLIKE.
CONCLUSION
Overall, although we may theorize that implanting a thick lenticule inside an intrastromal cap instead of underneath a flap provides certain advantages, both LIKE and sLIKE equip us with new refractive surgical techniques to help treat our high hyperopia patients. Early data concerning the use of allogenic corneal inlay prepared from a SMILE lenticule for presbyopia has already shown great safety and efficacy with excellent satisfaction at the 6-month postoperative follow-up [36]. Given the preliminary success with lenticule transplant in treating presbyopia, we have no doubt that both LIKE and sLIKE will emerge as frontiers in effectively treating high hyperopia patients in the future.
DISCLOSURE
Ethical issues have been completely observed by the authors. All named authors meet the International Committee of Medical Journal Editors (ICMJE) criteria for authorship for this manuscript, take responsibility for the integrity of the work as a whole, and have given final approval for the version to be published. No conflict of interest has been presented.
References
- 1.Vitale S. Prevalence of Refractive Error in the United States, 1999-2004. Archives of Ophthalmology. 2008;126:1111. doi: 10.1001/archopht.126.8.1111. doi: 10.1001/archopht.126.8.1111. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Suarez E, Torres F, Duplessie M. LASIK for correction of hyperopia and hyperopia with astigmatism. Int Ophthalmol Clin. 1996;36:65–72. doi: 10.1097/00004397-199603640-00010. pmid: 9072516. [DOI] [PubMed] [Google Scholar]
- 3.Varley GA, Huang D, Rapuano CJ, Schallhorn S, Boxer Wachler BS, Sugar A, et al. LASIK for hyperopia, hyperopic astigmatism, and mixed astigmatism: a report by the American Academy of Ophthalmology. Ophthalmology. 2004;111:1604–17. doi: 10.1016/j.ophtha.2004.05.016. doi: 10.1016/j.ophtha.2004.05.016 pmid: 15288995. [DOI] [PubMed] [Google Scholar]
- 4.Ditzen K, Huschka H, Pieger S. Laser in situ keratomileusis for hyperopia. J Cataract Refract Surg. 1998;24:42–7. doi: 10.1016/s0886-3350(98)80073-4. pmid: 9494898. [DOI] [PubMed] [Google Scholar]
- 5.Llorente L, Barbero S, Merayo J, Marcos S. Total and corneal optical aberrations induced by laser in situ keratomileusis for hyperopia. J Refract Surg. 2004;20:203–16. doi: 10.3928/1081-597X-20040501-03. pmid: 15188896. [DOI] [PubMed] [Google Scholar]
- 6.Ma L, Atchison DA, Albietz JM, Lenton LM, McLennan SG. Wavefront aberrations following laser in situ keratomileusis and refractive lens exchange for hypermetropia. J Refract Surg. 2004;20:307–16. doi: 10.3928/1081-597X-20040701-02. pmid: 15307391. [DOI] [PubMed] [Google Scholar]
- 7.Moshirfar M, J DD, B DW, M SM, O CB C. Hoopes P S. Mechanisms of Optical Regression Following Corneal Laser Refractive Surgery: Epithelial and Stromal Responses. Med Hypothesis Discov Innov Ophthalmol. 2018;7:1–9. pmid: 29644238. [PMC free article] [PubMed] [Google Scholar]
- 8.Alio JL, El Aswad A, Vega-Estrada A, Javaloy J. Laser in situ keratomileusis for high hyperopia (>50 diopters) using optimized aspheric profiles: efficacy and safety. J Cataract Refract Surg. 2013;39:519–27. doi: 10.1016/j.jcrs.2012.10.045. doi: 10.1016/j.jcrs.2012.10.045 pmid: 23375692. [DOI] [PubMed] [Google Scholar]
- 9.Damgaard IB, Ivarsen A, Hjortdal J. Biological Lenticule Implantation for Correction of Hyperopia: An Ex Vivo Study in Human Corneas. J Refract Surg. 2018;34:245–52. doi: 10.3928/1081597X-20180206-01. doi: 10.3928/1081597X-20180206-01 pmid: 29634839. [DOI] [PubMed] [Google Scholar]
- 10.Williams GP, Wu B, Liu YC, Teo E, Nyein CL, Peh G, et al. Hyperopic refractive correction by LASIK, SMILE or lenticule reimplantation in a non-human primate model. PLoS One. 2018;13 doi: 10.1371/journal.pone.0194209. doi: 10.1371/journal.pone.0194209 pmid: 29590157. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.The tool for additive hyperopia surgery - creating refractive lenticules for LIKE surgery. [[cited 2018 June 10]]. Available from: https://www.gebauermedical.com/refractive/
- 12.Pradhan KR, Reinstein DZ, Carp GI, Archer TJ, Gobbe M, Gurung R. Femtosecond laser-assisted keyhole endokeratophakia: correction of hyperopia by implantation of an allogeneic lenticule obtained by SMILE from a myopic donor. J Refract Surg. 2013;29:777–82. doi: 10.3928/1081597X-20131021-07. doi: 10.3928/1081597X-20131021-07 pmid: 24203809. [DOI] [PubMed] [Google Scholar]
- 13.Guilbert E, Laroche L, Borderie V. Le rejet d’allogreffe de cornée. Journal Français d'Ophtalmologie. 2011;34:331–48. doi: 10.1016/j.jfo.2011.02.001. doi: 10.1016/j.jfo.2011.02.001. [DOI] [PubMed] [Google Scholar]
- 14.Jankov M, Mrochen M, Seiler T. Laser intrastromal keratoplasty-Case report. Journal of Refractive Surgery. 2004;20:79–84. doi: 10.3928/1081-597X-20040101-14. [DOI] [PubMed] [Google Scholar]
- 15.Moshirfar M, Jehangir N, Fenzl CR, McCaughey M. LASIK Enhancement: Clinical and Surgical Management. J Refract Surg. 2017;33:116–27. doi: 10.3928/1081597X-20161202-01. doi: 10.3928/1081597X-20161202-01 pmid: 28192591. [DOI] [PubMed] [Google Scholar]
- 16.Riau AK, Liu YC, Lim CHL, Lwin NC, Teo EP, Yam GH, et al. Retreatment strategies following Small Incision Lenticule Extraction (SMILE): In vivo tissue responses. PLoS One. 2017;12:e0180941. doi: 10.1371/journal.pone.0180941. doi: 10.1371/journal.pone.0180941 pmid: 28708898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Riau AK, Ang HP, Lwin NC, Chaurasia SS, Tan DT, Mehta JS. Comparison of four different VisuMax circle patterns for flap creation after small incision lenticule extraction. J Refract Surg. 2013;29:236–44. doi: 10.3928/1081597X-20130318-02. doi: 10.3928/1081597X-20130318-02 pmid: 23557221. [DOI] [PubMed] [Google Scholar]
- 18.Siedlecki J, Luft N, Mayer WJ, Siedlecki M, Kook D, Meyer B, et al. CIRCLE Enhancement After Myopic SMILE. J Refract Surg. 2018;34:304–9. doi: 10.3928/1081597X-20180308-02. doi: 10.3928/1081597X-20180308-02 pmid: 29738585. [DOI] [PubMed] [Google Scholar]
- 19.Ganesh S, Brar S, Rao PA. Cryopreservation of extracted corneal lenticules after small incision lenticule extraction for potential use in human subjects. Cornea. 2014;33:1355–62. doi: 10.1097/ICO.0000000000000276. doi: 10.1097/ICO.0000000000000276 pmid: 25343698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Swinger CA, Barraquer JI. Keratophakia and keratomileusis--clinical results. Ophthalmology. 1981;88:709–15. doi: 10.1016/s0161-6420(81)34958-6. pmid: 7033859. [DOI] [PubMed] [Google Scholar]
- 21.Moshirfar M, McCaughey MV, Reinstein DZ, Shah R, Santiago-Caban L, Fenzl CR. Small-incision lenticule extraction. Journal of Cataract & Refractive Surgery. 2015;41:652–65. doi: 10.1016/j.jcrs.2015.02.006. [DOI] [PubMed] [Google Scholar]
- 22.Osman IM, Helaly HA, Abdalla M, Shousha MA. Corneal biomechanical changes in eyes with small incision lenticule extraction and laser assisted in situ keratomileusis. BMC Ophthalmol. 2016;16:123. doi: 10.1186/s12886-016-0304-3. doi: 10.1186/s12886-016-0304-3 pmid: 27457241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Wang D, Liu M, Chen Y, Zhang X, Xu Y, Wang J, et al. Differences in the corneal biomechanical changes after SMILE and LASIK. J Refract Surg. 2014;30:702–7. doi: 10.3928/1081597X-20140903-09. doi: 10.3928/1081597X-20140903-09 pmid: 25291754. [DOI] [PubMed] [Google Scholar]
- 24.Denoyer A, Landman E, Trinh L, Faure JF, Auclin F, Baudouin C. Dry eye disease after refractive surgery: comparative outcomes of small incision lenticule extraction versus LASIK. Ophthalmology. 2015;122:669–76. doi: 10.1016/j.ophtha.2014.10.004. doi: 10.1016/j.ophtha.2014.10.004 pmid: 25458707. [DOI] [PubMed] [Google Scholar]
- 25.Moshirfar M, Walker BD, Linn SH, Birdsong OC, Hoopes PC Jr. Optimal Pocket Depth for Corneal Inlays. J Refract Surg. 2018;34:288. doi: 10.3928/1081597X-20180209-01. doi: 10.3928/1081597X-20180209-01 pmid: 29634846. [DOI] [PubMed] [Google Scholar]
- 26.Kohlhaas M, Spoerl E, Schilde T, Unger G, Wittig C, Pillunat LE. Biomechanical evidence of the distribution of cross-links in corneas treated with riboflavin and ultraviolet A light. J Cataract Refract Surg. 2006;32:279–83. doi: 10.1016/j.jcrs.2005.12.092. doi: 10.1016/j.jcrs.2005.12.092 pmid: 16565005. [DOI] [PubMed] [Google Scholar]
- 27.Scarcelli G, Pineda R, Yun SH. Brillouin optical microscopy for corneal biomechanics. Invest Ophthalmol Vis Sci. 2012;53:185–90. doi: 10.1167/iovs.11-8281. doi: 10.1167/iovs.11-8281 pmid: 22159012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Chansue E, Tanehsakdi M, Swasdibutra S, McAlinden C. Safety and efficacy of VisuMax(R) circle patterns for flap creation and enhancement following small incision lenticule extraction. Eye Vis (Lond) 2015;2:21. doi: 10.1186/s40662-015-0031-5. doi: 10.1186/s40662-015-0031-5 pmid: 26709375. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Ting DSJ, Srinivasan S, Danjoux JP. Epithelial ingrowth following laser in situ keratomileusis (LASIK): prevalence, risk factors, management and visual outcomes. BMJ Open Ophthalmol. 2018;3:e000133. doi: 10.1136/bmjophth-2017-000133. 10.1136/bmjophth-2017-000133 pmid: 29657982. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Mohamed TA, Hoffman RS, Fine IH, Packer M. Post-laser assisted in situ keratomileusis epithelial ingrowth and its relation to pretreatment refractive error. Cornea. 2011;30:550–2. doi: 10.1097/ico.0b013e3182000ac3. pmid: 21598428. [DOI] [PubMed] [Google Scholar]
- 31.Caster AI, Friess DW, Schwendeman FJ. Incidence of epithelial ingrowth in primary and retreatment laser in situ keratomileusis. J Cataract Refract Surg. 2010;36:97–101. doi: 10.1016/j.jcrs.2009.07.039. doi: 10.1016/j.jcrs.2009.07.039 pmid: 20117711. [DOI] [PubMed] [Google Scholar]
- 32.Rapuano CJ. Management of epithelial ingrowth after laser in situ keratomileusis on a tertiary care cornea service. Cornea. 2010;29:307–13. doi: 10.1097/ICO.0b013e3181b7f3c5. doi: 10.1097/ICO.0b013e3181b7f3c5 pmid: 20098302. [DOI] [PubMed] [Google Scholar]
- 33.Chen LY, Kung JS, Manche EE. Management of Complex Epithelial Ingrowth After Laser In Situ Keratomileusis Using Fibrin Tissue Glue. Eye Contact Lens. 2017 doi: 10.1097/ICL.0000000000000447. doi: 10.1097/ICL.0000000000000447 pmid: 29219897. [DOI] [PubMed] [Google Scholar]
- 34.Mastropasqua L, Nubile M, Salgari N, Mastropasqua R. Femtosecond Laser-Assisted Stromal Lenticule Addition Keratoplasty for the Treatment of Advanced Keratoconus: A Preliminary Study. J Refract Surg. 2018;34:36–44. doi: 10.3928/1081597X-20171004-04. doi: 10.3928/1081597X-20171004-04 pmid: 29315440. [DOI] [PubMed] [Google Scholar]
- 35.Kanellopoulos AJ, Asimellis G. Epithelial remodeling after femtosecond laser-assisted high myopic LASIK: comparison of stand-alone with LASIK combined with prophylactic high-fluence cross-linking. Cornea. 2014;33:463–9. doi: 10.1097/ICO.0000000000000087. doi: 10.1097/ICO.0000000000000087 pmid: 24622298. [DOI] [PubMed] [Google Scholar]
- 36.Jacob S, Kumar DA, Agarwal A, Agarwal A, Aravind R, Saijimol AI. Preliminary Evidence of Successful Near Vision Enhancement With a New Technique: PrEsbyopic Allogenic Refractive Lenticule (PEARL) Corneal Inlay Using a SMILE Lenticule. J Refract Surg. 2017;33:224–9. doi: 10.3928/1081597X-20170111-03. doi: 10.3928/1081597X-20170111-03 pmid: 28407161. [DOI] [PubMed] [Google Scholar]