Abstract
Background:
Waiting is common in health care, delays intervention, and has negative effects on satisfaction with services.
Objectives:
To evaluate effects of a modified walk-in system, where patients were invited consecutively from the waiting list to attend the clinic on a walk-in basis, on waiting times, services, and work environment.
Study design:
Parallel-group trial.
Methods:
In all, 1286 consecutive patients in need of shoe insoles were randomized to waiting lists for modified walk-in (n = 655) or a scheduled appointment (n = 631). Seven staff members also participated.
Results:
The median indirect waiting time to first appointment was 40 days shorter for modified walk-in (135 days) than for scheduled appointment (175 days; p < 0.001); 17% of those randomized to modified walk-in did not attend the clinic compared to 6% for scheduled appointment (p < 0.001). Mean direct waiting time in the waiting room was 9.9 min longer for modified walk-in than for scheduled appointment (p < 0.001). Patients attending modified walk-in or a scheduled appointment reported similar levels of satisfaction with services. Staff reported more support from co-workers with modified walk-in than with scheduled appointment (p = 0.041).
Conclusion:
The modified walk-in can reduce indirect waiting times without any substantial worsening of direct waiting times, service quality, or work environment. Studies are needed to investigate why many patients drop out from modified walk-in.
Clinical relevance
A modified walk-in system can cut the queues and create more timely interventions by reducing indirect waiting times. This system can therefore be recommended in secondary-care prosthetic and orthotic clinics to reduce patients’ suffering from their health condition.
Keywords: Rehabilitation, lower limb orthotics, orthotics
Background
Waiting is common in health care, delays intervention, and has negative effects on patients’ satisfaction with services.1,2 It is often assumed that waiting is an inevitable consequence of demand for health-care services being higher than supply and that the solution is to add more resources.3 This has been questioned because the number of patients on a waiting list is often stable over time, indicating that supply and demand are in balance, and adding extra resources has often failed to reduce waiting times.1,3–7 Thus, waiting time is not necessarily related to lack of resources but often the problem—and the solution—is to be found in organizational structures.3,4 Studies have demonstrated that changing how patients are prioritized and scheduled are effective ways to reduce waiting times.5,6,8
Waiting time comes in two forms: indirect waiting time, which refers to the time from the patient’s request for an appointment to the actual appointment, and direct waiting time, which refers to time spent in the waiting room at the appointment.9 Indirect waiting time is a medical concern because it delays intervention, and direct waiting time is a source of patient dissatisfaction.2,10,11 In our prosthetic and orthotic (P&O) clinic, indirect waiting times have been an issue for the large group of patients in need of shoe insoles because of less severe problems; they are given lower priority in favor of patients with more severe problems. Upon referral from physicians and physiotherapists, these patients are put on a waiting list to be given a scheduled appointment (SA). At the first appointment, the certified prosthetist and orthotist (CPO) delivers a pair of prefabricated insoles or makes imprints or casts of the patient’s feet to produce custom-made insoles to be delivered at a second appointment with no waiting list. If the patient wants further adjustments after the first or second appointment or has worn out the insoles, a new appointment is scheduled, following the same queue system as the first appointment. A typical appointment lasts for 30 min. The SA system has resulted in stable workloads over the day but also long indirect waiting times. In addition, some patients cancel their appointment at short notice or do not show up, leading to loss of productivity for the CPOs.
An alternative to SA is a traditional walk-in system where patients come to the clinic at any time to wait for their turn. This virtually eliminates indirect waiting times but has been associated with long direct waiting times and stress for the staff.9,12,13 Thus, there might be a need to modify the traditional walk-in to adjust for these negative aspects and still benefit from its advantages.
Traditional walk-in systems have been used in health-care services for a long time but have not been much studied. A Cochrane review of different appointment systems’ effects on indirect waiting times found no studies on walk-in systems.14 Studies investigating other outcomes of walk-in have often used a pre-post-intervention design vulnerable to confounding by factors that change over time, such as seasonal variations in patient demand.12,14,15 Furthermore, most studies have been conducted in primary care or “walk-in clinics,” limiting the generalizability of the results. The aim of this study was to investigate the effects of a modified walk-in (MWI) system in a secondary-care P&O clinic on indirect and direct waiting times, patient satisfaction with services, and staff perceptions of the work environment.
Methods
Study design and randomization
The study was a parallel-group trial in which each patient was randomized to one of two parallel groups: MWI or SA waiting list. One of the authors (G.J.) generated a list of random numbers on www.randomizer.org (allocation ratio 1:1) and consecutively allocated patients to the waiting lists. The study was conducted according to the Declaration of Helsinki and approved by regional ethics committee review board in Uppsala, Sweden (manuscript number 2014/342).
Participants and setting
The study was conducted over 8 months (October 2014 to May 2015) at the publicly funded P&O secondary-care clinic in Örebro, Sweden. The participating patients were individuals in need of shoe insoles because of less severe problems, typically activity-related pain in the lower extremities. The exclusion criterion was if a SA was required, for example, for a language interpretation. Those who were excluded were given a SA. The participating staff members were administrators at the patient reception and the CPOs prescribing the insoles.
Intervention: MWI
The inflow of patients to the walk-in clinic was modified as follows: each week a specific number of patients were invited by mail to the MWI any Thursday of their choice during a pre-specified 5-week period. If the patients preferred a SA, they could reschedule to a SA by contacting the clinic reception. Those who were randomized to SA were given a SA by mail 4 weeks in advance.
The first 4 months can be characterized as an initiation phase when the MWI comprised 1 day per week (two CPOs serving all patients) and the SA system comprised 2 days per week (one CPO with 11 appointment slots per day). During this first 4-month period, more new patients were invited to SA than MWI as second appointments (deliveries of custom-made insoles) were scheduled outside the SA while the MWI comprised both first and second appointments. During the last 4 months, the SA slots were used for both first and second appointments to make the circumstances similar to MWI. During this period, two CPOs were available in the morning but only one in the afternoon, as most patients arrived before lunchtime (Table 1).
Table 1.
Overview of appointment systems used in the study.
| MWI | SA | |
|---|---|---|
| First 4 months | ||
| Kinds of appointments | First and second | First |
| New patients invited/week (n) | 12 | 22 |
| CPOs/week (n)a | 2 | 2 |
| Last 4 months | ||
| Kinds of appointments | First and second | First and second |
| New patients invited/week (n) | 15 | 16b |
| CPOs/week (n)a | 1.5 | 2 |
CPOs: certified prosthetist and orthotists; SA: scheduled appointment; MWI: modified walk-in.
Full-day equivalent.
In all, 22 appointment slots minus approximately 6 needed for second appointments.
Outcomes
Primary outcome was indirect waiting time, defined as the number of days the patient spent on the waiting list. The indirect waiting time started on the date the patient was registered in the local administration system after a referral (new patients) or made a phone call to the clinic (patients who had previously attended the clinic) and ended on the date the patient attended the clinic (for the first visit) or dropped out. Patients were considered to have dropped out if they stated that they were not interested in coming or did not attend the clinic within 5 weeks (MWI group) or repeatedly canceled or failed to show up (SA group).
Secondary outcomes were as follows: (1) direct waiting time, that is, the time the patient spent in the waiting room, (2) patients’ satisfaction with services, and (3) CPOs’ and administrators’ perceptions of the work environment.
Questionnaires
At the appointment, the patients (13 years and older) received study information from the clinical administrator and were invited to participate. Each participant filled in two questionnaires. We measured patient satisfaction with the Client Satisfaction with Services (CSS) module from the Swedish version of Orthotics and Prosthetics Users’ Survey (OPUS).16–19 A study-specific questionnaire was also used, asking patients (1) the time they spent in the waiting room and (2) what kind of appointment they would prefer, by choosing between (i) a SA with 3–4 months’ indirect waiting time and no direct waiting time and (ii) a MWI with 1–2 months’ indirect waiting time and up to 1 h direct waiting time. A “no preference” option was also available.
In April 2015, the staff answered eight items from the Swedish version of General Nordic Questionnaire for Psychological and Social Factors at Work (QPS Nordic).20 We added a study-specific question: “In general, what is your stress level when working with MWI or SA?” answered on a five-point rating scale (very low, low, neither high nor low, high, very high) and also asked what kind of appointment system they thought should be used for this patient group in the future (MWI, SA, both MWI and SA, other). The patients and staff members received written information about the study and provided written informed consent before answering the questionnaires. The administrators were asked to record the number of telephone calls related to MWI and SA during 7 weeks in March and April 2015.
Statistical analysis
Demographic characteristics were compared using a two-sided t-test for age and a chi-square test for sex. When comparing patients who attended the clinic, dropped out, and remained on the waiting list at the study end, a one-way analysis of variance (ANOVA; with Tukey’s honest significant difference (HSD) as a post hoc test) was used for age and a chi-square test for sex. A Mann–Whitney U test was used to compare indirect waiting times. The number of patients on waiting lists and indirect waiting times for patients still on the waiting lists were recorded on the first day of each month and visualized in diagrams. Direct waiting times were compared using a two-sided t-test. The CSS was analyzed item by item because its unidimensionality has been questioned,18,21 using a two-sided Mann–Whitney U test. The QPS was analyzed using a two-sided Wilcoxon signed-rank test. Patient preferences and telephone data were analyzed using a chi-square test. To reveal the impact of the type of appointment on satisfaction and direct waiting times, we analyzed CSS and direct waiting times per protocol, that is, according to the type of appointment the patients actually attended. The analyses of indirect waiting times and patient preferences were according to the intention-to-treat approach, that is, participants were analyzed according to the groups that they had been randomized to. We used IBM SPSS version 22 for statistical analyses.
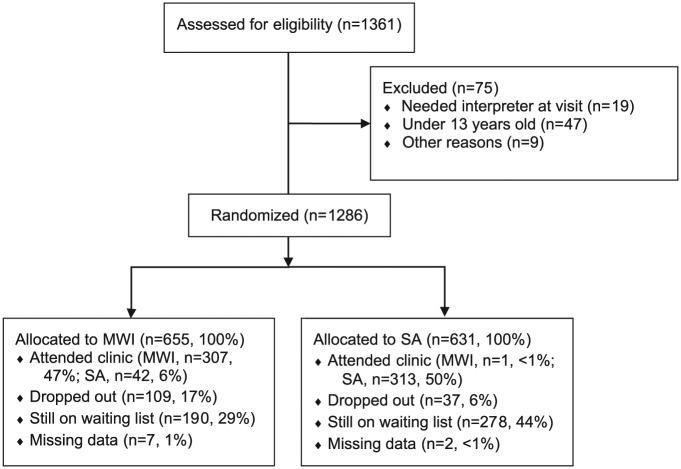
Results
Patients on the waiting list at baseline (n = 367) or who entered the study during the study period (n = 919) were randomized to the MWI and SA waiting lists (Figure 1). On average, 118.0 new patients were registered each month (standard deviation (SD): 18.1). The age and sex distributions were similar in the MWI and SA groups (Table 2). The sample consisted of 1260 unique patients and 26 patients who contacted the clinic a second time during the study period and thus were randomized a second time. Nine patients were lost after randomization without any recorded data. No patient answered the questionnaires twice; 43 patients changed groups; that is, they were randomized to MWI but had a SA or vice versa. There was no significant difference in mean age (p = 0.877) or sex distribution (p = 0.860) between patients who had an appointment of the same type as they had been randomized to and patients who changed groups.
Figure 1.
Flow diagram for participating patients.
MWI: modified walk-in; SA: scheduled appointment.
Table 2.
Demographic characteristics of participating patients.
| Patients randomized (n = 1286) | Randomized to MWI (n = 655)a | Randomized to SA (n = 631)b | p value | |
|---|---|---|---|---|
| Women, n (%) | 437 (67.4) | 439 (69.8) | 0.365 | |
| Mean age, years (SD) | 49.0 (21.0) | 48.4 (20.7) | 0.595 | |
| Attended the clinic (n = 663) | (n = 349) | (n = 314) | 0.207 | |
| Women, n (%) | 228 (65.3) | 211 (67.2) | 0.612 | |
| Mean age, years (SD) | 50.8 (20.8) | 49.4 (20.1) | 0.375 | |
| Dropped out (n = 146) | (n = 109) | (n = 37) | <0.001 | |
| Women, n (%) | 79 (72.5) | 29 (78.4) | 0.480 | |
| Mean age, years (SD) | 48.2 (17.7) | 51.0 (18.6) | 0.422 | |
| Still on waiting list (n = 468) | (n = 190) | (n = 278) | <0.001 | |
| Women, n (%) | 130 (68.4) | 199 (71.6) | 0.462 | |
| Mean age, years (SD) | 46.3 (22.7) | 47.0 (21.7) | 0.732 | |
| Patients answering questionnaires (n = 293) | Attended MWI (n = 168)c | Attended SA (n = 125)d | ||
| Women, n (%) | 112 (66.7) | 81 (64.8) | 0.739 | |
| Mean age, years (SD) | 54.3 (16.7) | 52.6 (15.6) | 0.392 |
MWI: modified walk-in; SA: scheduled appointment.
The p values <0.05 are written in boldface.
Data missing for seven patients.
Data missing for two patients.
Of whom one had been randomized to SA.
Of whom 11 had been randomized to MWI. Statistical comparisons used a two-sided t-test for age and a chi-square test for sex and number of patients.
The number of patients who attended the clinic did not differ significantly between the MWI and SA groups, but more patients in the MWI group dropped out and more patients in the SA group remained on the waiting list at the study end (Table 2). We compared the numbers of appointments (first and second appointments) during the last 4 months of the study; on average, 9.7 (SD 1.2) patients were seen per full-day CPO with SA and 10.2 (SD 2.3) with MWI (p = 0.467, two-sided t-test). Patients who attended the clinic were older (mean age = 50.1 years) than patients who remained on the waiting list (46.7 years, p = 0.019) but neither group differed from patients who dropped out (48.9 years; p = 0.812 and 0.494). There was no difference between the sex distributions in the three groups (p = 0.114). Median indirect waiting time was 135 days for MWI and 175 days for SA (p < 0.001). The number of patients on waiting lists developed more positively for MWI than for SA (Figure 2).
Figure 2.
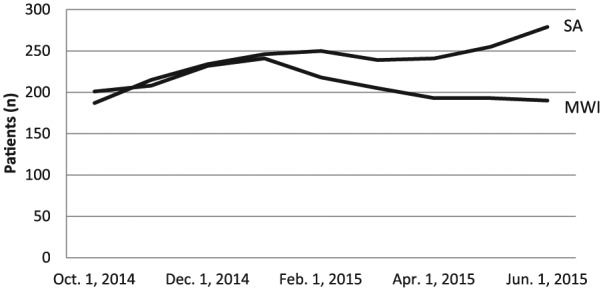
Number of patients on waiting lists.
MWI: modified walk-in; SA: scheduled appointment.
The questionnaires were answered by 316 patients. In all, 12 questionnaires were excluded from the analyses because the patient had not signed the consent to participate and another 11 were excluded because the respondent could not be identified with a patient in the randomization list. Thus, questionnaires from 293 patients were included in the analyses out of 663 patients who attended the clinic, corresponding to a response rate of 44.2%. The sex distribution was similar among respondents and non-respondents (p = 0.868) but respondents were older (mean age = 53.6 years) than non-respondents (47.3 years, p < 0.001). On average, patients attending MWI had 9.9 min longer direct waiting time (p < 0.001, 95% confidence interval (CI): 7.5, 12.3) than patients attending a SA (mean: 15.6 and 5.7 min). There was no statistically significant difference in satisfaction with services (p = 0.057–0.685) between patients attending MWI or SA; on all CSS items, the median answer was either 2 = agree or 3 = strongly agree.
For patients randomized to MWI (n = 178), significantly more patients preferred MWI than SA (p < 0.001, 67.4% preferred MWI, 8.4% preferred SA, 10.7% no preference, and 13.5% missing data). For patients randomized to SA (n = 115), there was no significant difference between the number who preferred MWI or SA (p = 0.811, 29.6% preferred MWI, 31.3% preferred SA, 28.7% no preference, and 10.4% missing data).
Both of the administrators (two women) and six out of seven CPOs (three women and three men) answered the questionnaire. They reported similar experiences when working with MWI and SA but a higher level of support and help from co-workers with MWI (Table 3). On the stress question, the median was 4 (= high) for MWI and 3.5 (3 = neither high nor low) for SA (p = 0.334). Two staff members preferred MWI for patients in need of shoe insoles, one preferred SA, and five preferred that we should use both MWI and SA. A total of 82 incoming and outgoing telephone calls were recorded during the 7 weeks. More outgoing telephone calls were related to SA (n = 22) than to MWI (n = 0; p < 0.001). There was no significant difference between the number of incoming telephone calls related to MWI (n = 26) and SA (n = 34, p = 0.302).
Table 3.
Staff members’ views of their work environment based on type of appointment system, median values (first and third quartiles).
| Item (QPS Nordic domain, item number) | MWI | SA | p valuea |
|---|---|---|---|
| Is your workload irregular so that the work piles up? (JD, 12) | 3 (3, 4) | 3.5 (2, 4) | 0.679 |
| Is it necessary to work at a rapid pace? (JD, 14) | 3 (3, 4) | 3.5 (3, 4) | 0.783 |
| Do you have too much to do? (JD, 15) | 3 (2.25, 4) | 3 (3, 3.75) | 0.854 |
| Do you know exactly what is expected of you at work? (RE, 40) | 5 (5, 5) | 5 (4.25, 5) | 0.317 |
| Are you content with the quality of the work you do? (MW, 66) | 4 (3.25, 4) | 4 (4, 4) | 0.157 |
| Are you content with the amount of work that you get done? (MW, 67) | 4 (3.25, 4) | 4 (3.25, 4) | 0.564 |
| If needed, can you get support and help with your work from your co-workers? (SI, 72) | 4 (4, 5) | 3.5 (1.25, 4) | 0.041 |
| If needed, can you get support and help with your work from your immediate superior? (SI, 73) | 3.5 (2.25, 4) | 3.5 (2, 4) | 0.317 |
QPS Nordic: General Nordic Questionnaire for Psychological and Social Factors at Work; MWI: modified walk-in; SA: scheduled appointment; JD: job demands; RE: role expectations; MW: mastery of work; SI: social interactions.
Rating scale: 1 = very seldom or never, 2 = rather seldom, 3 = sometimes, 4 = rather often, and 5 = very often or always.
The p values <0.05 are written in boldface.
Two-sided Wilcoxon signed-rank test.
Discussion
This is the first study evaluating a MWI system, and the results suggest that MWI can reduce indirect waiting times without any substantial negative effects on direct waiting times, service quality, or work environment.
It could be argued that MWI reduces indirect waiting times because there are no late cancellations of appointments or no shows. However, our results seem to be explained mainly by other factors. Staff sick leave made rescheduling of SA patients necessary on several occasions, as demonstrated in our telephone data, while it was not possible for the clinic to cancel a MWI: other CPOs had to replace the CPO on sick leave. In addition, a larger proportion of patients dropped out from MWI than from SA. The majority of these patients gave no explicit reason for dropping out, and the sex and age distribution among dropouts was similar to that of patients who attended. Importantly, direct waiting times were acceptable for both SA and MWI, indicating that MWI overcomes one of the drawbacks with the traditional walk-in system.12
The preference question was posed to elicit patients’ trade-off between indirect and direct waiting times, and the preferences differed substantially. Patients who had been randomized to MWI strongly favored MWI, whereas patients randomized to SA varied in their preferences. Perhaps patients not only took the hypothetical alternatives into account but also actual experience. Few patients changed the type of appointment from what they had been randomized to, and according to the CSS results, experiences of the appointment were mostly positive. This is in line with a study in which patients’ relative preferences for two kinds of appointment systems changed after changing systems at the clinic.12 The MWI group was more positive about MWI than the SA group was about SA, as the latter expressed no clear preference about type of appointment. This result seems to favor MWI.
Staff reported more support from co-workers with MWI than they did with SA. This was probably because SA sessions are considered as each CPO’s own responsibility, whereas the CPOs had been instructed to help each other out if work piled up at MWI.
Before implementing a new appointment system as a traditional walk-in or the advanced access model,6 current waiting lists must be eliminated. This may pose a barrier to implementation because clinics struggling with long waiting lists often do not have extra resources to spend on this. However, as shown in this study, a MWI system can be implemented without eliminating current waiting lists.
Study limitations
One limitation of our study was that 75 patients were not randomized but given a SA. One reason was children under 13 years old who entered the waiting list in the first 2 months were not randomized but given a SA, as we were afraid that the direct waiting time with MWI would be too long. However, this imbalance cannot fully explain the results because more staff resources were spent on SA. During the last 4 months, we tried to make the staff resources spent on MWI and SA as similar as possible, and during this period, the difference between the waiting lists accelerated (Figure 2). Still, the appointment systems were not fully comparable; 2 days each week were used for SA and 1 for MWI, possibly making patients drop out from MWI because of less flexibility in the choice of day. Other potential limitations were that the time the CPOs spent with each patient and the quality of the insoles were not documented and that self-report was used to measure direct waiting times. These aspects need to be studied in future research. Finally, the study was conducted in a single P&O clinic with a small number of staff members, thus limiting the power of the statistical comparisons and the generalizability of the results.
There is probably no such thing as a perfect appointment system, but by modifying the traditional walk-in, we could balance the positive and negative aspects of walk-in and SA. Moreover, by keeping some control over the inflow of patients, it was possible to predict and match the supply and demand for services, which is one of the main challenges in organizing health-care services. An effective system for large patient groups with minor problems, as in this study, is important to free resources for smaller patient groups with larger problems.
Conclusion
A MWI system can reduce indirect waiting times without any substantial worsening of direct waiting times, service quality, or work environment. However, many patients drop out from MWI and the reasons for this need to be investigated in future studies. In addition, studies are needed to investigate the generalizability of the results.
Acknowledgments
The results of this study have previously been presented at Diamantendagen (regional day for quality improvement), Örebro University Hospital, Örebro, Sweden, 25 November 2015.
Footnotes
Author contribution: G.J. designed the study, collected data, analyzed data, drafted the manuscript, and approved the final version. L.H. designed the study, made critical revision of the manuscript, and approved the final version.
Declaration of conflicting interests: The author(s) declared the following potential conflicts of interest with respect to the research, authorship, and/or publication of this article: G.J. is a consultant for Novo Nordisk but does not consider this to be a relevant conflict of interest. L.H. has no conflicts of interest in this study.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This study was supported by Region Örebro County, Sweden.
References
- 1. Murray M, Berwick DM. Advanced access: reducing waiting and delays in primary care. JAMA 2003; 289(8): 1035–1040. [DOI] [PubMed] [Google Scholar]
- 2. Bar-dayan Y, Leiba A, Weiss Y, et al. Waiting time is a major predictor of patient satisfaction in a primary military clinic. Mil Med 2002; 167(10): 842–845. [PubMed] [Google Scholar]
- 3. Kreindler SA. Watching your wait: evidence-informed strategies for reducing health care wait times. Qual Manag Health Ca 2008; 17(2): 128–135. [DOI] [PubMed] [Google Scholar]
- 4. Walley P, Silvester K, Steyn R. Knowledge and behaviour for a sustainable improvement culture. Healthc Pap 2006; 7(1): 26–33; discussion 74–77. [DOI] [PubMed] [Google Scholar]
- 5. Murray M, Bodenheimer T, Rittenhouse D, et al. Improving timely access to primary care: case studies of the advanced access model. JAMA 2003; 289(8): 1042–1046. [DOI] [PubMed] [Google Scholar]
- 6. Murray M, Tantau C. Same-day appointments: exploding the access paradigm. Fam Pract Manag 2000; 7(8): 45–50. [PubMed] [Google Scholar]
- 7. Kenis P. Waiting lists in Dutch health care: an analysis from an organization theoretical perspective. J Health Organ Manag 2006; 20(4): 294–308. [DOI] [PubMed] [Google Scholar]
- 8. Harding KE, Leggat SG, Bowers B, et al. Reducing waiting time for community rehabilitation services: a controlled before-and-after trial. Arch Phys Med Rehabil 2013; 94(1): 23–31. [DOI] [PubMed] [Google Scholar]
- 9. Gupta D, Denton B. Appointment scheduling in health care: challenges and opportunities. IIE Trans 2008; 40(9): 800–819. [Google Scholar]
- 10. Arain M, Nicholl J, Campbell M. Patients’ experience and satisfaction with GP led walk-in centres in the UK: a cross sectional study. BMC Health Serv Res 2013; 13: 142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Van Uden CJ, Ament AJ, Hobma SO, et al. Patient satisfaction with out-of-hours primary care in the Netherlands. BMC Health Serv Res 2005; 5(1): 6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Cassell JA, Brook MG, Mercer CH, et al. Maintaining patient access to GUM clinics: is it compatible with appointments? Sex Transm Infect 2003; 79(1): 11–15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Fallon CW, Hamilton I, Bhopal JS, et al. Introduction of an appointment system in a general practice: surveys of patients and staff. Health Bull 1990; 48(5): 232–237. [PubMed] [Google Scholar]
- 14. Ballini L, Negro A, Maltoni S, et al. Interventions to reduce waiting times for elective procedures. Cochrane Database Syst Rev 2015; 2: CD005610. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Tideman RL, Pitts MK, Fairley CK. Effects of a change from an appointment service to a walk-in triage service at a sexual health centre. Int J STD AIDS 2003; 14(12): 793–795. [DOI] [PubMed] [Google Scholar]
- 16. Heinemann AW, Bode RK, O’Reilly C. Development and measurement properties of the Orthotics and Prosthetics Users’ Survey (OPUS): a comprehensive set of clinical outcome instruments. Prosthet Orthot Int 2003; 27(3): 191–206. [DOI] [PubMed] [Google Scholar]
- 17. Jarl G, Holmefur M, Norling Hermansson L. Test-retest reliability of the Swedish version of the Orthotics and Prosthetics Users’ Survey. Prosthet Orthot Int 2014; 38(1): 21–26. [DOI] [PubMed] [Google Scholar]
- 18. Jarl GM, Heinemann AW, Norling Hermansson LM. Validity evidence for a modified version of the Orthotics and Prosthetics Users’ Survey. Disabil Rehabil Assist Technol 2012; 7(6): 469–478. [DOI] [PubMed] [Google Scholar]
- 19. Jarl GM, Norling Hermansson LM. Translation and linguistic validation of the Swedish version of Orthotics and Prosthetics Users’ Survey. Prosthet Orthot Int 2009; 33(4): 329–338. [DOI] [PubMed] [Google Scholar]
- 20. Dallner M, Elo A-L, Gamberale F, et al. Validation of the General Nordic Questionnaire (QPS Nordic) for Psychological and Social Factors at Work. Copenhagen: Nordic Council of Ministers, 2000. [Google Scholar]
- 21. Jarl G, Lindner HY, Heinemann AW, et al. Cross-cultural validity and differential item functioning of the Orthotics and Prosthetics Users’ Survey with Swedish and United States users of lower-limb prosthesis. Arch Phys Med Rehabil 2015; 96: 1615–1626. [DOI] [PubMed] [Google Scholar]