Abstract
Introduction:
Hip fractures are common in elderly patients. However, this population frequently presents with significant medical comorbidities requiring extensive medical optimization.
Methods:
This study sought to elucidate optimal time to surgery and evaluate its effect on postoperative morbidity, mortality, and length of stay (LOS). We performed a retrospective analysis of data collected from 2008 to 2010 on 841 patients who underwent hip fracture surgery. Patients were classified based on time to surgery and were also classified and analyzed according to the American Society of Anesthesiologists (ASA) physical classification system.
Results:
Patients with a delay of greater than 48 hours had a significant increase in overall LOS, postoperative days, and overall postoperative complications. Patients classified as ASA 4 had an odds ratio for postoperative morbidity of 3.32 compared to the ASA 1 and 2 group (P = .0002) and 2.26 compared to the ASA 3 group (P = .0005). Delaying surgery >48 hours was also associated with increased in-hospital mortality compared to 24 to 48 hours (P = .0197). Increasing ASA classification was also associated with significantly increased mortality. Patients classified as ASA 4 had 5.52 times the odds of ASA 1 and 2 (P = .0281) of in-hospital mortality. Those classified ASA 4 had 2.97 times the odds of ASA 3 (P = .0198) of an in-house mortality. Anesthetic technique (spinal vs general) and age were not confounding variables with respect to mortality or morbidity.
Discussion:
Surgical timing and ASA classification were evaluated with regard to LOS, number postoperative days, morbidity, and mortality.
Conclusions:
Delaying surgery >48 hours, especially in those with increased ASA classification, is associated with an increase in overall LOS, postoperative days, morbidity, and mortality. However, rushing patients to surgery may not be beneficial and 24 to 48 hours of preoperative optimization may be advantageous.
Keywords: geriatric medicine, length of stay, morbidity, mortality, ASA
Introduction
Hip fractures are a common injury with an annual incidence of about 1.3 million worldwide.1 Due to significant preexisting comorbidities and subsequent difficulty in achieving favorable outcomes, hip fractures represent a major public health concern in the elderly population. Hip fractures can be devastating in terms of functional and economic loss, quality of life, and mortality with an in-hospital mortality rate up to 10%2 and 1-year mortality of 27.3%.3
Ideal time to surgery for fracture stabilization is widely debated. Current clinical guidelines recommend surgical intervention within 48 hours when medically optimized.4-7 In September 2014, the American Academy of Orthopedic Surgeons released a recommendation, backed by moderate evidence, advising hip fracture surgery be performed within 48 hours of admission.8 However, competition for operating room availability and extensive medical optimization or risk stratification often results in a delay to surgery.
Current literature provides moderate evidence of association between surgical delay and postoperative complications. Small sample-sized and low-powered studies have shown that increasing time to surgery increases length of stay (LOS).9,10 Increases in preoperative time were due to numerous factors including electrolyte imbalances, anticoagulation, and significant comorbidities affecting functional status.4,10 These studies indicate that a delay can result in significant increases in postoperative morbidity and mortality.5,6,9-11 Conversely, some literature suggests negative effects with early surgery.12,13
Our study sought to evaluate the following hypotheses:
Excessive delays to surgery will increase mortality, morbidity, and LOS in geriatric patients.
An increase in preoperative time is correlated with age and American Society of Anesthesiologist (ASA) physical classification system status.
Increases in LOS are due to type of anesthetic, ASA status, age, and sex.
Methods
This study was an institutional review board–approved retrospective analysis of data collected from 2008 to 2010 including 841 patients at a single urban institution who underwent surgical repair for hip fractures. Descriptive statistics were generated for any continuous variables, including the mean and standard deviation. Data transformations were performed to evaluate specific categories. Patients were divided into 3 groups based on time to surgery: <24 hours, 24 to 28 hours, or >48 hours. Patients were also analyzed according to the ASA. Patients were categorized into 3 groups: ASA 1 and 2, ASA 3, or ASA 4.
Log transformations were used to evaluate certain outcomes, such as development of postoperative complications and LOS. In-house mortality and complications were evaluated with regard to time to surgery and ASA classification. Postoperative complications evaluated included myocardial infarction (MI), cerebral vascular events (CVAs), acute kidney injury (AKI), pulmonary embolism (PE), pneumonia (PNA), and postoperative cognitive dysfunction (POCD). AKI was defined as an increase in serum creatinine (SCr) by ≥0.3 mg/dL within 48 hours or increase in SCr to ≥1.5 times baseline occurring within 7 days. Underlying chronic kidney disease was adjusted for using the Modification of Diet in Renal Disease formula (estimated glomerular filtration rate = 186 × SCr − 1.154 × age − 0.203 × [1.210 if black] × [0.742 if female]).14
Statistical analysis was performed using the Kruskal-Wallis test (or 1-way analysis of variance on ranks). Post hoc analysis involved the Bonferroni-adjusted significance tests for pairwise comparisons. Odds ratios for risk factors such as age group (<70, 70-79, and ≥80), sex, and type of anesthesia (general vs spinal/neuraxial) were obtained using logistic regression models with independent variables (ASA and preoperative days) and log postoperative days as the dependent variable. Statistical analysis was generated using SAS version 9.4 and SPSS version 23. Bonferroni correction: P value = .0167 was considered significant for all group comparisons in Table 1.
Table 1.
Effect of Time to Surgery and ASA Status on the Postoperative Length of Stay.a
| Effects on Log Postoperative | P Value |
|---|---|
| Kruskal-Wallis test: dependent variable log postoperative Days | |
| Preop: <24 hours vs >48 hours | .011 |
| Preop: 24 to 48 hours vs >48 hours | .009 |
| Preop: <24 hours vs 24-48 hours | NS |
| ASA: 1 and 2 vs 4 | <.0001 |
| ASA: 1 and 2 vs 3 | .001 |
| ASA: 3 vs 4 | <.0001 |
Abbreviations: ASA, American Society of Anesthesiologists; NS, not statistically significant; Preop, preoperative.
aBonferroni correction: P value = .0167 for 3 comparisons was considered statistically significant.
Results
Our analysis included data from 841 surgical patients. Mean patient age was 83, approximately 74% were female, 48% received spinal anesthesia, while 52% underwent general anesthesia. Descriptive statistics and frequencies are found in Table 2.
Table 2.
Descriptive Statistics.
| Descriptive Statistics and Frequencies | ||||
|---|---|---|---|---|
| Sample size (N) | 841 | |||
| Age mean (Std) | 83 (10) | |||
| Age group <70 (%) | 11% | |||
| Age group 70-79 (%) | 18% | |||
| Age group ≥80 (%) | 71% | |||
| ASA Group | <24 Hours Preop # of Patients | 24-48 Hours Preop # of Patients | >48 Hours Preop # of Patients | |
| ASA 1 or 2 | 25% | 91 | 70 | 48 |
| ASA 3 | 51% | 147 | 163 | 123 |
| ASA 4 | 24% | 49 | 55 | 95 |
| Gender | # ASA 1 and 2 | # ASA 3 | # ASA 4 | |
| Male | 26% | 39 | 101 | 77 |
| Female | 74% | 170 | 332 | 122 |
| Spinal | 48% | |||
| General | 52% | |||
| Preoperative Time to Surgery | ||||
| <24 hours (%) | 34% | |||
| 24 to 48 hours (%) | 34% | |||
| >48 hours (%) | 32% | |||
Abbreviations: ASA, American Society of Anesthesiologists; Std, standard deviation.
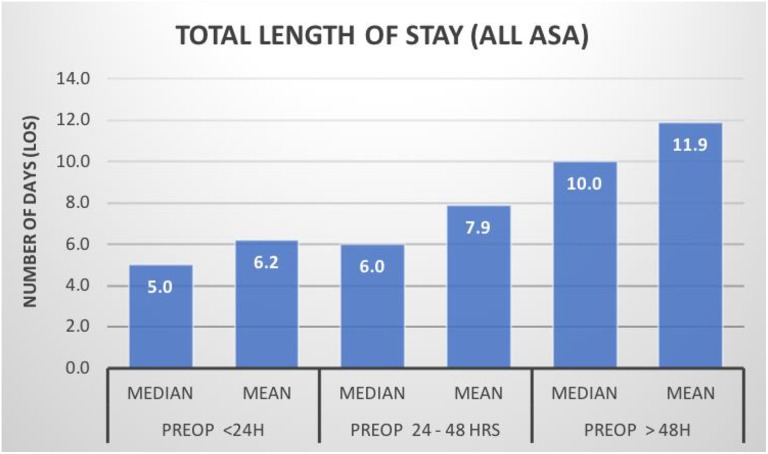
Time to Surgery
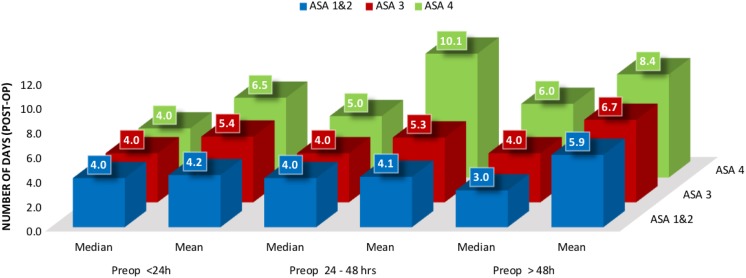
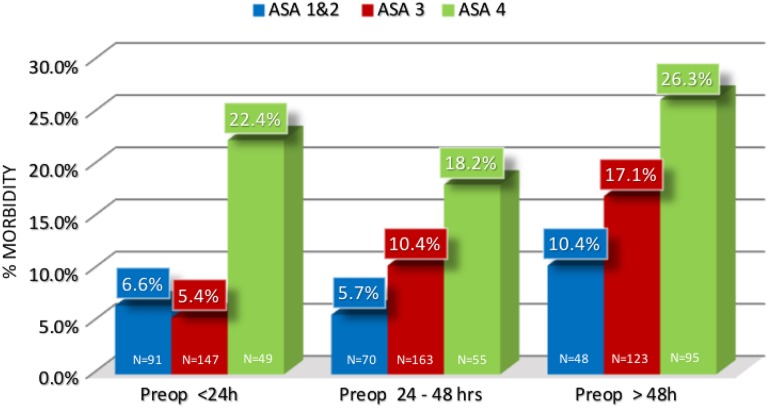
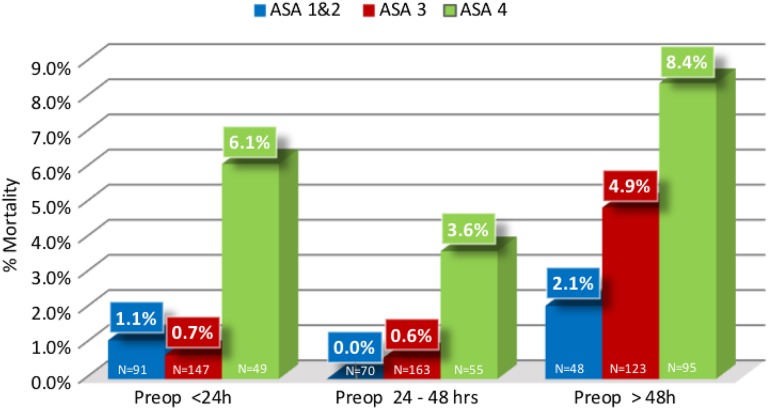
An increase in time to surgery was associated with overall increased LOS (P < .0001; Figure 1). Since an increase in preoperative time contributes to overall LOS, postoperative LOS was specifically evaluated and we found delay of >48 hours to surgery was also associated with a significant increase in postoperative days (Figure 2). In addition, patients with >48 hours to surgery had significantly increased incidence of all postoperative complication (MI, CVA, PE, PNA, AKI, POCD; Figure 3 and Table 3). Delaying surgery >48 hours correlated with an increased in-hospital mortality with 2.3% versus 1% versus 5.7% for <24 hours, 24 to 48 hours, or >48 hours, respectively (Figure 4 and Table 4). The data indicate that in-hospital mortality was significantly higher for patients with >48 hours to surgery compared to patients who had surgery between 24 and 48 hours (P = .0197; Table 4). The raw data indicate mortality for patients undergoing surgery within 24 to 48 hours was lower compared to those who had surgery in <24 hours. However, the difference was not statistically significant.
Figure 1.
Effect of time to surgery on length of stay—an increase in time to surgery was associated with overall increased length of stay.
Figure 2.
Effect of time to surgery on number of inpatient days postoperatively—a patient who had >48 hours to surgery was associated with a significant increase in the number of postoperative days (P < .05). As American Society of Anesthesiologists status increased, the length of postoperative days also significantly increases (P ≤ .001).
Figure 3.
Effect of number of preoperative time in hours on morbidity. Postoperative complications evaluated included myocardial infarction (MI), cerebral vascular events (CVAs), acute kidney injury (AKI), pulmonary embolism (PE), pneumonia (PNA), and postoperative cognitive dysfunction (POCD). N = Number of patients in each group.
Table 3.
Effect of Preoperative Time and ASA Status on Morbidity.
| Logistic Regression: Dependent Variable (Morbidity) | ||
|---|---|---|
| Effect on Morbidity | Odds Ratio | P Value |
| Preop: <24 hours vs >48 hours | 2.04 (1.20-3.44) | .0079 |
| Preop: 24-48 hours vs >48 hours | 1.68 (1.02-2.75) | .0405 |
| Preop: <24 hours vs 24-48 hours | NS | NS |
| ASA: 1 and 2 vs 4 | 3.32 (1.77-6.25) | .0002 |
| ASA: 3 vs 4 | 2.26 (1.43-3.58) | .0005 |
Abbreviations: NS, not statistically significant; Preop, preoperative.
a P value <.05 was statistically significant.
Figure 4.
Effect of preoperative time in hours on mortality. N = Number of patients in each group.
Table 4.
The Effect of Time to Surgery and ASA Status on Mortality.a
| Logistic Regression: Dependent Variable (In-House Deaths) | ||
|---|---|---|
| Effect on Mortality | Odds Ratio (95% CI) | P Value |
| Preop: <24 hours vs >48 hours | NS | NS |
| Preop: 24-48 hours vs >48 hours | 4.50 (1.27-15.9) | .0197 |
| Preop: <24 hours vs 24-48 hours | NS | NS |
| ASA: 1 and 2 vs 4 | 5.52 (1.20-25.6) | .0281 |
| ASA: 3 vs 4 | 2.96 (1.19-7.41) | .0198 |
Abbreviations: ASA, American Society of Anesthesiologists; CI, confidence interval; NS, not statically significant; Preop, preoperative.
a P value <.05 was statistically significant.
Stratifying time to surgery by ASA status shows that ASA 1 and 2 patients had a shorter time to surgery than ASA 3 and ASA 4 patients (Table 2). Chi-square analysis of ASA status versus time to surgery showed that the 2 groups were statistically different (P < .0001). Approximately 43% (91/209) of ASA 1 and 2 patients had surgery in less than 24 hours, and only around 23% (48/209) waited more than 48 hours. In contrast, only approximately 34% (14//433) of ASA patients had surgery within 24 hours and 28% (123/433) waited more than 48 hours. ASA 4 patients experienced even grater disparity compared to the ASA 1&2 groups with only about 25% (49/199) going to surgery within 24 hours and almost 50% waited more than 48 hours (95/199; Table 2).
American Society of Anesthesiologist Status
Length of postoperative days also significantly increases as ASA status increases (Figure 2 and Table 2). Patients classified as ASA 4 had an odds ratio of 3.32 when compared to the ASA 1 and 2 group (P = .0002) of any postoperative morbidity and an odds ratio of 2.26 compared to ASA 3 (P = .0005; Figure 3 and Table 3). Increasing ASA classification was associated with a significant increase in mortality. Odds ratio for in-hospital mortality is 5.52 (1.20-25.6) for ASA 4 compared to ASA 1 and 2 (P = .0281) and 2.97 (1.19-7.41) when compared to ASA 3 (P = .0198; Table 4).
Another set of analyses was performed. We carried out linear regression modeling on preoperative LOS and ASA classification versus complications (that included mortality as a complication). When performed, only ASA classification was significant (P < .0001). However, we found the most significant group with respect to complications was the preoperative LOS >48 hours. Therefore, we reanalyzed the linear regression with the preoperative LOS with only 2 groups: we combined the <24 hours and 24 to 48 cohorts and the second group was >48 hours. This regression of preoperative LOS and ASA versus complication was significant for both LOS and ASA versus complication (P < .019 and P < .0001, respectively). These results indicate the possibility that >48 hours delay to surgery and high ASA classification is associated with worse outcomes.
Gender, Age, and Choice of Anesthetic
Female gender is associated with a lower mortality. Males had 2.85 times the mortality rate compared to females (P < .0001). Stratifying gender by ASA status shows that approximately 27% (170/624) of females were ASA 1 and 2, while over 50% (332/624) were ASA 3 and less than 20% (122/624) were ASA 4. In comparison, less than 20% (39/217) of males were ASA 1 and 2, approximately 46% (101/217) were ASA 3, and only about 35% (77/217) were ASA 4. Chi-square analysis showed that the 2 groups were statistically different (Table 1, P < .0001). Logistic regression analysis showed that male gender and ASA classification were independently and significantly associated with having complications (P < .0001, and P < .0001, respectively). Additionally, logistic regression analysis showed that male gender and ASA classification were both associated with increased 30-day mortality (P < .004 and P < .03, respectively). However, only ASA classification was associated with increased 60-day mortality (P <. 005). Our study did not find anesthetic technique (spinal vs general) or age-group (<70, 70-80, >80) to be variables that affected morbidity or mortality.
Discussion
Over 300 000 hip fractures occur every year in the United States and over 1.3 million worldwide mostly involving the elderly population age 65 and older.3,15 As the geriatric population grows, hip fracture incidence is expected to rise. These injuries are significant life-changing events with mortality rates estimated at close to 30% even in patients who undergo surgery.3,16,17 Morbidity and mortality from hip fractures result in significant economic burdens on families and the health-care system. In an effort to improve outcomes, quality of care, and reduce costs, research has focused on evaluating potentially adjustable variables such as type of anesthesia, fracture stabilization technique, pharmacological prophylaxis, and time to surgery.8
Many studies have shown that fracture stabilization surgery within 48 hours improves outcomes or decreased LOS. A Canadian prospective study of 3007 patients by Bohm et al6 used 48 hours as a benchmark. The study concluded a reduction in time to surgery decreased LOS and reduced adjusted in-hospital mortality and 1-year mortality. Uzoigwe et al18 performed a similar study involving 2056 patients stratified by time to surgery within 12, 24, and after 36 hours and found that mortality increased after 36 hours and decreased with time to surgery within 12 to 24 hours. A meta-analysis performed by Simunovic et al19 reported a significant decrease in mortality when patients had surgery within 24 to 72 hours. Moja et al20 performed a review analysis of 35 published studies (between 1948 and 2011) including 191 873 patients and found lower all-cause mortality rates in patients who had surgery 24 to 48 hours after admission. Siegmeth et al21 performed a prospective study of 3628 patients over a 15-year period, which excluded patients who had a delay for medical reasons, and found that patients who had surgery within 48 hours of admission shortened their mean LOS from 32.5 to 21.6 days.
These studies present data substantiating our findings: Surgery within 48 hours is associated with lower mortality rates and decreased LOS. Our study also suggested a decrease in postoperative morbidity and mortality if surgery is performed specifically between 24 and 48 hours. Patients who underwent surgery prior to 24 hours had an increase in mortality and overall LOS. However, this was not statistically significant. Our analysis went further and also investigated preoperative functional status effect on outcomes and found that patients with poorer overall health, as indicated by higher ASA scores, had increased delays to surgery and increased mortality rates.
We were concerned that our findings of increased mortality and LOS in the <24-hour cohort was skewed by the ASA 4 group. However, a close examination of our data shows that far more ASA 4 patients had delayed time to surgery and less than 25% had surgery within 24 hours. ASA 4 patients are actually overrepresented in the >48 hours to surgery group at around 48%, which may partially account for their increased rate of poor outcomes (Table 2).
However, other studies have been performed showing lower correlation with early time to surgery and improved mortality. Khan et al22 reviewed 52 studies including 291 143 patients and concluded that surgery performed within 48 hours of admission was unlikely harmful but effects on reduced mortality were unproven.22 Vidan et al23 found that increases in mortality in those with delays to surgery, could be explained by the underlying medical reasons for surgical delay. A prospective analysis of 2660 patients performed by Moran et al24 found that surgery performed within 4 days of admission had no effect on mortality, but surgical delays of greater than 4 days did result in significant increases in 90-day and 1-year mortality even in patients without comorbidities; however, patients with significant comorbidities and delayed surgery had 2.5 times the risk of death within 30 days compared to patients without significant comorbidities. While there are many studies analyzing patient databases evaluating time to surgery and effect on outcomes, there exists a paucity of randomized controlled trials providing more definitive support that hip fracture surgery should be performed within 48 hours.
Choice of anesthetic technique, namely, neuraxial versus general anesthesia, was not found to affect postoperative LOS. Yet, despite minimal evidence,25,26 practice guidelines have called for broader use of neuraxial or regional anesthesia.27 Moreover, most studies actually supporting regional anesthesia over general anesthesia are retrospective or observational in nature. Proponents of neuraxial anesthesia have argued that it decreases pain scores, blood loss, intraoperative hemodynamic lability, and incidence of deep vein thromboses (DVTs). Guay et al28 performed a meta-analysis of research examining neuraxial versus general anesthesia for hip fracture surgery and included 31 studies in the Cochrane database totaling 3231 participants. No difference in neuraxial versus general anesthesia was found in regard to length of surgery, LOS, 1 month mortality, and morbidity (with the exception of risk of DVT).25,28 Another study by Neuman et al26 concluded that among adults in acute care hospitals in New York State undergoing hip repair, use of regional anesthesia when compared to general anesthesia was not associated with a decrease in 30-day mortality. A 0.6-day shorter LOS was the only benefit associated with neuraxial anesthesia. However, an observational cohort study of 10 868 patients by Perlas et al29 found a strong association between spinal anesthesia and lower 30-day mortality and shorter hospital LOS.
Our study examined the impact of delay to surgery on development of several major complications including MI, CVA, PE, PNA, ARF, and POCD. However, we did not look at development of pressure ulcers, wound complications, and total rehabilitation time as potential significant problems associated with delay to surgery. A study by Grimes et al30 found delaying surgery for more than 96 hours significantly increased the incidence of pressure sores or ulcers. Our study also did not scrutinize specific causes of delay to surgery. Anecdotally, delays in surgery often involve patients who present to the hospital with complex medical problems requiring extensive workup and optimization prior to surgery including serial lab draws for cardiac markers of ischemia and advanced imaging such as cardiac catheterizations, carotid duplex scans, and echocardiograms. When patients present on weekends and limited resources are available to aid in their optimization, delays may be prolonged. A recent study by Adair et al31 regarding use of preoperative echocardiograms in hip fracture patients highlights the topic of preoperative optimization as a particularly important area of focus to improve time to surgery and outcomes. In their retrospective analysis of 100 patients, it was concluded that transthoracic echocardiograms could have been avoided in 34% of patients if accepted clinical practice guidelines recommended by the American College of Cardiology/American Heart Association had been employed, thereby reducing unnecessary resource utilization without adversely affecting patient outcomes.31
There are a few weaknesses in our study. First, it is a single-center study. Furthermore, the study is retrospective and can only find relationships and cannot address causality. Additionally, the data were collected from 2008 to 2010. Future research elucidating causes for delays to surgery may help mitigate surgical postponement and improve outcomes.
Conclusion
Our data show delaying surgery for more than 2 days was associated with an increase in overall LOS, postoperative days, morbidity, and mortality. This was correlated with an increase in ASA classification. Although patients with increased comorbidities might require increased preoperative time for surgical optimization, delaying surgery may contribute to increased morbidity and mortality. The data also suggest that rushing patients to surgery may not be beneficial and 2 days of preoperative optimization may be advantageous since mortality for 2 preoperative days was lower compared to 1 preoperative day. However, the difference was not statistically significant. Our results also indicate the possibility that >48 hours delay to surgery and high ASA classification are associated with worse outcomes when analyzed via linear regression.
Other noteworthy findings in our study include a decreased odds ratio for mortality associated with female gender, partially explained by increased illness severity represented by higher ASA scores associated with our male hip fracture cohort, and that choice of anesthetic technique (spinal vs general) and age were not variables that affected morbidity or mortality.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Aakash Patel, BS  http://orcid.org/0000-0002-9776-890X
http://orcid.org/0000-0002-9776-890X
Dennis E. Feierman, PhD, MD  http://orcid.org/0000-0001-5824-5404
http://orcid.org/0000-0001-5824-5404
References
- 1. Johnell O, Kanis JA. An estimate of the worldwide prevalence, mortality and disability associated with hip fracture. Osteoporos Int. 2004;15(11):897–902. [DOI] [PubMed] [Google Scholar]
- 2. Frost SA, Nguyen ND, Black DA, Eisman JA, Nguyen TV. Risk factors for in-hospital post-hip fracture mortality. Bone. 2011;49(3):553–558. [DOI] [PubMed] [Google Scholar]
- 3. Panula J, Pihlajamaki H, Mattila VM, et al. Mortality and cause of death in hip fracture patients aged 65 or older: a population-based study. BMC Musculoskelet Disord. 2011;12:105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Tran T, Delluc A, de Wit C, Petrcich W, Le Gal G, Carrier M. The impact of oral anticoagulation on time to surgery in patients hospitalized with hip fracture. Thromb Res. 2015;136(5):962–965. [DOI] [PubMed] [Google Scholar]
- 5. Simunovic N, Devereaux PJ, Bhandari M. Surgery for hip fractures: does surgical delay affect outcomes? Indian J Orthop. 2011;45(1):27–32. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Bohm E, Loucks L, Wittmeier K, Lix LM, Oppenheimer L. Reduced time to surgery improves mortality and length of stay following hip fracture: results from an intervention study in a Canadian Health Authority. Can J Surg. 2015;58(4):257–263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. American Academy of Orthopaedic Surgeons. Moderate evidence supports that hip fracture surgery within 48 hours of admission is associated with better outcomes. (n.d.). Retrieved August 13, 2018, from http://www.orthoguidelines.org/guideline-detail?id=1233.
- 8. Management Of Hip Fractures In The Elderly: evidence based clinical practice guidelines. Retrieved September 5, 2014 http://www.aaos.org/cc_files/aaosorg/research/guidelines/hipfxguideline.pdf. 2014. Accessed August 13, 2018.
- 9. Alonso-Fernandez P, Romero E, Chung M, Garcia-Salmones M, Cabezas P, Mora J. Delayed surgery in hip fracture patients. Can we afford it? Int J Health Plann Manage. 2017;32(4):653–659. [DOI] [PubMed] [Google Scholar]
- 10. Shah AA, Kumar S, Shakoor A, Haroon R, Noordin S. Do delays in surgery affect outcomes in patients with inter-trochanteric fractures? J Pak Med Assoc. 2015;65(11 suppl 3): S21–S24. [PubMed] [Google Scholar]
- 11. Nyholm AM, Gromov K, Palm H, et al. Time to surgery is associated with thirty-day and ninety-day mortality after proximal femoral fracture: a retrospective observational study on prospectively collected data from the Danish Fracture Database Collaborators. J Bone Joint Surg Am. 2015;97(16):1333–1339. [DOI] [PubMed] [Google Scholar]
- 12. Johnson-Lynn S, Ngu A, Holland J, Carluke I, Fearon P. The effect of delay to surgery on morbidity, mortality and length of stay following periprosthetic fracture around the hip. Injury. 2016;47(3):725–727. [DOI] [PubMed] [Google Scholar]
- 13. Gan L, Zhong J, Zhang R, et al. The immediate intramedullary nailing surgery increased the mitochondrial DNA release that aggravated systemic inflammatory response and lung injury induced by elderly hip fracture. Mediators Inflamm. 2015;2015:587378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Levey AS, Bosch JP, Lewis JB, Greene T, Rogers N, Roth D. A more accurate method to estimate glomerular filtration rate from serum creatinine: a new prediction equation. Modification of Diet in Renal Disease Study Group. Ann Intern Med. 1999;130(6):461–470. [DOI] [PubMed] [Google Scholar]
- 15. Torio CM (AHRQ), Andrews RM (AHRQ). National Inpatient Hospital Costs: The Most Expensive Conditions by Payer, 2011. HCUP Statistical Brief #160. Agency for Healthcare Research and Quality, Rockville, MD. August 2013 http://www.hcup-us.ahrq.gov/reports/statbriefs/sb160.pdf. [PubMed]
- 16. Lee DJ, Elfar JC. Timing of hip fracture surgery in the elderly. Geriatr Orthop Surg Rehabil. 2014;5(3):138–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Goldacre MJ, Roberts SE, Yeates D. Mortality after admission to hospital with fractured neck of femur: database study. BMJ. 2002;325(7369):868–869. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Uzoigwe CE, Burnand HG, Cheesman CL, Aghedo DO, Faizi M, Middleton RG. Early and ultra-early surgery in hip fracture patients improves survival. Injury. 2013;44(6):726–729. [DOI] [PubMed] [Google Scholar]
- 19. Simunovic N, Devereaux PJ, Sprague S, et al. Effect of early surgery after hip fracture on mortality and complications: systematic review and meta-analysis. CMAJ. 2010;182(15):1609–1616. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Moja L, Piatti A, Pecoraro V, et al. Timing matters in hip fracture surgery: patients operated within 48 hours have better outcomes. A meta-analysis and meta-regression of over 190,000 patients. PLoS One. 2012;7(10):e46175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Siegmeth AW, Gurusamy K, Parker MJ. Delay to surgery prolongs hospital stay in patients with fractures of the proximal femur. J Bone Joint Surg Br. 2005;87(8):1123–1126. [DOI] [PubMed] [Google Scholar]
- 22. Khan SK, Kalra S, Khanna A, Thiruvengada MM, Parker MJ. Timing of surgery for hip fractures: a systematic review of 52 published studies involving 291,413 patients. Injury. 2009;40(7):692–697. [DOI] [PubMed] [Google Scholar]
- 23. Vidan MT, Sanchez E, Gracia Y, Maranon E, Vaquero J, Serra JA. Causes and effects of surgical delay in patients with hip fracture: a cohort study. Ann Intern Med. 2011;155(4):226–233. [DOI] [PubMed] [Google Scholar]
- 24. Moran CG, Wenn RT, Sikand M, Taylor AM. Early mortality after hip fracture: is delay before surgery important? J Bone Joint Surg Am. 2005;87(3):483–489. [DOI] [PubMed] [Google Scholar]
- 25. Parker MJ, Handoll HH, Griffiths R. Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev. 2004;(4):CD000521. [DOI] [PubMed] [Google Scholar]
- 26. Neuman MD, Rosenbaum PR, Ludwig JM, Zubizarreta JR, Silber JH. Anesthesia technique, mortality, and length of stay after hip fracture surgery. JAMA. 2014;311(24):2508–2517. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Association of Anaesthetists of Great Britain and Ireland, Griffiths R, Alper J, Beckingsale A, et al. Management of proximal femoral fractures 2011: Association of Anaesthetists of Great Britain and Ireland. Anaesthesia. 2012;67(1):85–98. [DOI] [PubMed] [Google Scholar]
- 28. Guay J, Parker MJ, Gajendragadkar PR, Kopp S. Anaesthesia for hip fracture surgery in adults. Cochrane Database Syst Rev. 2016;2:CD000521. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Perlas A, Chan VW, Beattie S. Anesthesia technique and mortality after total hip or knee arthroplasty: a retrospective, propensity score-matched cohort study. Anesthesiology. 2016;125(4):724–731. [DOI] [PubMed] [Google Scholar]
- 30. Grimes JP, Gregory PM, Noveck H, Butler MS, Carson JL. The effects of time-to-surgery on mortality and morbidity in patients following hip fracture. Am J Med. 2002;112(9):702–709. [DOI] [PubMed] [Google Scholar]
- 31. Adair C, Swart E, Seymour R, Patt J, Karunakar MA. Clinical practice guidelines decrease unnecessary echocardiograms before hip fracture surgery. J Bone Joint Surg Am. 2017;99(8):676–680. [DOI] [PubMed] [Google Scholar]