Abstract
Background:
The knee dislocation–3 (KD3) injury pattern is the most common form of multiligamentous injury. Medial KD3 (KD3-M) and lateral KD3 (KD3-L) are 2 anatomically different varieties of this injury.
Purpose:
To compare the surgical outcomes of KD3-M and KD3-L multiligamentous knee injury patterns and to determine the factors that could influence the outcomes after single-stage reconstruction.
Study Design:
Cohort study; Level of evidence, 3.
Methods:
A cohort of 45 patients with multiligamentous knee injuries (31 KD3-M, 14 KD3-L) who were operated on between 2011 and 2015 were compared. The cruciate ligaments were reconstructed, and the collateral ligaments were managed either conservatively or surgically depending on intraoperative laxity, tissue condition, injury site, and chronicity. The mean follow-up was 36 months (range, 24-72 months). The International Knee Documentation Committee (IKDC) score, Lysholm score, knee flexion range of motion (ROM), and laxity on stress radiographs were compared. Various factors likely to influence the outcomes were also analyzed.
Results:
The mean IKDC score, Lysholm score, and knee flexion ROM for the 45 patients were 74.74, 87.66, and 126.78°, respectively. There was no significant difference between the KD3-M and KD3-L groups in terms of the postoperative IKDC score (P = .768), Lysholm score (P = .689), knee flexion ROM (P = .798), and laxity on stress radiographs (P = .011). Patients with a transient dislocation had better outcomes (76.51, 89.41, and 128.61°, respectively) than those with a frank dislocation (67.62, 80.66, and 119.44°) (P = .037, .007, and .043). The acute group had better outcomes (77.00, 89.51, and 127.86°) when compared with the subacute (66.26, 86.00, and 121.00°) and chronic groups (67.40, 76.40, and 125.00°) (P = .045, .006, and .486). Regression analysis showed the influence of these factors on outcomes. The presence or absence of dislocations, time frame in which surgery was performed, and follow-up duration were found to influence the outcome. All other factors had no bearing on outcomes. Two patients had knee stiffness and underwent arthrolysis.
Conclusion:
Despite anatomic and biomechanical differences between KD3-M and KD3-L injuries, single-stage management did not produce any significant difference in results. The presence of a frank dislocation, delay in surgery, and duration of follow-up were found to influence outcomes.
Keywords: knee dislocation, multiligamentous knee injuries, knee dislocation–3, KD3, single-stage reconstruction
A knee dislocation is the most common cause of multiligamentous knee injuries (MLKIs), and its incidence is less than 0.02% of all orthopaedic injuries.16,17,19,36 It is a serious condition, with the potential to cause devastating complications such as popliteal artery injury,12,16,32,40 common peroneal nerve injury,2,5,34 compartment syndrome,4,15,41 and deep vein thrombosis.7,9,33 In addition to the management of acute injuries, restoring the stability and pain-free motion of the knee is also a major challenge. Restoring the function of the knee, being a major weightbearing joint, is of utmost importance. The conventional classification system of Kennedy,20 based on the position of the tibia in relation to the femur, categorizes knee dislocations into anterior, posterior, medial, lateral, and rotatory. However, most of the dislocations resolve spontaneously, and this classification system offers little applicability. The anatomic classification system developed by Schenck37 and modified by Wascher44 is more practical and defines the severity of injury; the higher the knee dislocation grade, the greater the severity and poorer the prognosis. It is based on the number of ligaments injured during a dislocation. Of the classifications, knee dislocation–3 (KD3) injuries, which involve both cruciate ligaments with one of the collateral ligaments, either medial (KD3-M) or lateral (KD3-L), are the most common pattern of knee dislocations.13,29,46,47 The timing of surgery, staging of surgery, and repair versus reconstruction of the collateral ligaments are some of the challenges faced by surgeons. While there is a concept of staging the procedure, the recent literature has supported single-stage management.11,21,31
The purpose of this study was to compare KD3-M and KD3-L injuries and to evaluate the predictive factors that influence the outcomes of single-stage reconstruction of KD3-type MLKIs. Our hypothesis was that KD3-M and KD3-L injuries would have significantly different outcomes when managed in a single stage because of their anatomic and biomechanical differences.
Methods
This was a prospective study conducted from February 2011 to August 2015 at our institute. After obtaining approval from our institutional review board, we enrolled all patients with KD3-type MLKIs and excluded those with KD1, KD2, KD4, and KD5 injuries; previous knee surgery; deformities; arthritis; open injuries; vascular injuries; and fractures around the knee. In total, 56 patients were operated on for an MLKI after a knee dislocation during this period, of which 45 patients with a KD3 injury satisfied our selection criteria. There were 39 male and 6 female patients, with a mean age of 39 years (range, 17-74 years). Thirty-six patients sustained high-energy trauma such as a road traffic accident (n = 33) and high-impact collision during sports (n = 3), while 9 patients sustained low-energy trauma such as a twisting knee injury (n = 2) and fall from a staircase (n = 7). Nine patients had a frank dislocation and presented to the emergency room with a dislocated knee; 36 patients had a transient dislocation that relocated after trauma. Overall, there were 31 KD3-M– and 14 KD3-L–type MLKIs. Ten patients had a grade 2 injury to the collateral ligaments, and the remaining 35 had a grade 3 injury based on magnetic resonance imaging (MRI). All the patients in the study underwent single-stage reconstruction.
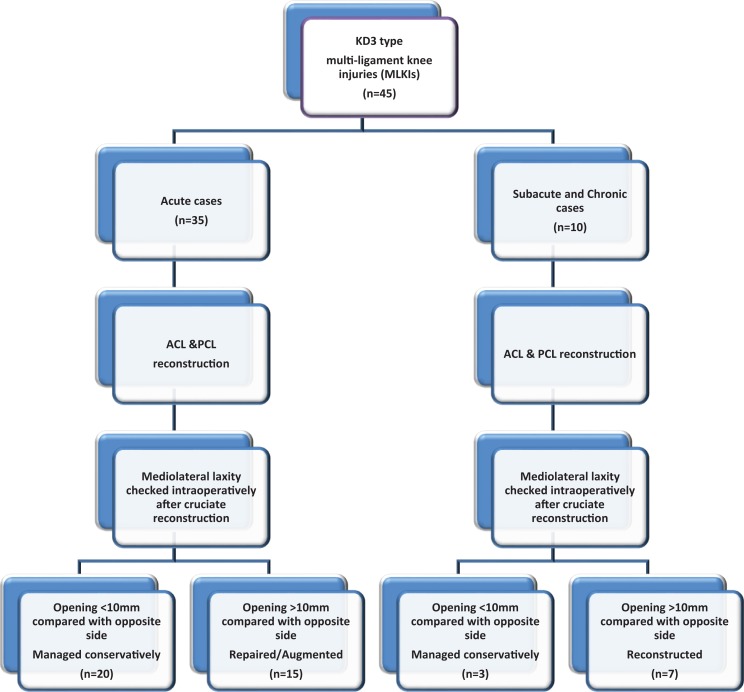
Philosophy of Management
All 45 patients were operated on by a single senior surgeon (S.R.S.), who has 13 years of experience in knee ligament reconstruction. Thirty-five patients underwent surgery in the first 6 weeks after trauma (acute: group 1), 5 patients underwent surgery between 6 and 12 weeks (subacute: group 2), and 5 patients underwent surgery after 12 weeks and within 6 months of initial trauma (delayed presentation cases; chronic: group 3) (Figure 1). All patients who presented to the emergency room were assessed as per the Advanced Trauma Life Support (ATLS) protocol. Once the general condition was found satisfactory, the knee was assessed clinically for laxity, swelling, and neurovascular status. Patients who had a frank dislocation underwent closed reduction in the emergency room. Once the neurovascular status was satisfactory, the limb was splinted, then a radiological evaluation was performed. In 1 patient, the knee was very unstable after reduction. Thus, it was stabilized in an external fixator, and ligament reconstruction was performed after 8 weeks. All the other patients who had a stable knee after reduction were immobilized for 48 hours and observed for signs of vascular compromise and compartment syndrome. After 48 hours, active range of movement and continuous passive movement were started with a hinged knee brace.
Figure 1.
Flowchart showing the management of knee dislocation–3 (KD3) injuries. ACL, anterior cruciate ligament; PCL, posterior cruciate ligament.
Most of the patients who presented acutely (n = 35) underwent surgery after 10 to 14 days. The decision regarding the time of surgery was made based on swelling, soft tissue status, range of motion (ROM), intactness of the capsule (on MRI), neurovascular status, and other comorbid illness. Once the swelling subsided and the knee gained more than 90° of preoperative flexion, patients then underwent ligament reconstruction. Written informed consent was obtained, and preoperative planning was performed. All patients underwent surgery under combined spinal and epidural anesthesia, and in all the patients, we used autologous tendon grafts (hamstring/patellar/quadriceps tendon) from both legs.
Initially, an examination of the knee was conducted under anesthesia, which was then arthroscopically evaluated for cruciate, meniscal, and cartilage injuries. The cruciate ligaments were reconstructed first using autologous tendon grafts (Table 1). Then, mediolateral laxity was assessed intraoperatively at 0° and 30° of flexion. The grade of laxity was determined intraoperatively by the senior surgeon in all the patients and was determined by a comparison with the uninjured contralateral knee. When laxity was >10 mm with a soft endpoint, it was considered grade 3; when it was 5 to 10 mm, it was considered grade 2; and when it was <5 mm with a firm endpoint, it was considered grade 1. A collateral ligament injury with grade 1 and grade 2 laxity (10 patients) was managed conservatively.
TABLE 1.
Management of Cruciate and Collateral Ligament Injuries
| No. of Cruciate Ligament Injuries |
Anterior Cruciate Ligament | Posterior Cruciate Ligament | ||||
|---|---|---|---|---|---|---|
| 26 | Reconstruction with hamstring tendon graft | Reconstruction with hamstring tendon graft | ||||
| 13 | Reconstruction with patellar tendon graft | Reconstruction with hamstring tendon graft | ||||
| 4 | Reconstruction with hamstring tendon graft | Reconstruction with quadriceps tendon graft | ||||
| 1 | Reconstruction with hamstring tendon graft | Avulsion was fixed | ||||
| 1 | Reconstruction with hamstring tendon graft | Conservative management | ||||
| No. of Collateral Ligament Injuries | Location of Injury, n | Modality of Treatment, n | ||||
| Proximal Attachment | Midsubstance | Distal Attachment | Repair | Reconstruction/Augmentation | Conservative | |
| 31 (medial) | 15 | 13 | 3 | 7 | 2 reconstruction | 22 |
| 14 (lateral) | 4 | 3 | 7 | 4 | 9 (3 augmentation and 6 reconstruction) | 1 |
All patients with grade 3 mediolateral laxity after anterior cruciate ligament (ACL) and posterior cruciate ligament (PCL) reconstruction (35 patients) underwent surgical repair/augmentation depending on the site of injury and time of presentation. Collateral avulsions from the proximal or distal attachment site were repaired (11 patients: 7 KD3-M, 4 KD3-L), while midsubstance tears were augmented with an autologous hamstring tendon graft (3 patients: KD3-L) (Table 1). In the subacute (5 patients) and chronic groups (5 patients) in the patients with grade 3 mediolateral laxity after cruciate ligament reconstruction, the collateral ligament was reconstructed (8 patients: 2 KD3-M, 6 KD3-L) (Table 1). When laxity was grade ≤2 (2 patients), injuries were managed conservatively. Two patients (subacute group, KD3-M type) needed medial collateral ligament (MCL) reconstruction, which was performed using a hamstring tendon graft using the technique described by Borden et al.3 Three patients (chronic group, KD3-L type) who had posterolateral rotatory instability (grade 3 lateral opening and >10° of external rotation asymmetry on the dial test) underwent anatomic reconstruction of the posterolateral corner (PLC) as recommended by LaPrade et al,23 whereas 3 patients (2 subacute and 1 chronic group, KD3-L type) had only lateral instability and underwent lateral collateral ligament (LCL) reconstruction as per the modified Larson26 technique.
Fifteen patients had a meniscal tear (3 medial and 12 lateral menisci), for which partial meniscectomy and debridement were performed. Six patients had an associated medial patellofemoral ligament (MPFL) injury, of which 2 had a dislocation of the patella at the time of injury. Three of the 6 MPFL injuries were treated conservatively, and 2 were repaired when the medial side was surgically exposed to repair the MCL. One patella that was unstable needed MPFL reconstruction with a gracilis tendon graft. Seven patients had grade 1 or 2 cartilage injuries, and all were managed conservatively. Two had a common peroneal nerve injury in the KD3-L group, and both of them had only partial recovery. The mean duration from injury to surgery was 39 days, with a range of 5 to 180 days.
Postoperative Rehabilitation
Our institutional protocol for all the patients with MLKIs was nonweightbearing mobilization with a walking frame for 6 weeks. A static knee immobilizer with posterior support was used for 6 weeks, after which a hinged knee brace was used for up to 12 weeks. At the third postoperative week, passive prone knee mobilization exercises were started. After 6 weeks, active assisted knee mobilization was started, and patients were allowed to walk with partial weightbearing, progressing to full weightbearing by the 10th week. After 3 months, weight-resistance exercises were started, and by 6 months, patients were encouraged to squat and sit cross-legged. Running and jogging were allowed only after 8 months. Patients were subsequently evaluated every 6 months. The mean follow-up period for the 45 study patients was 36 months, ranging from 24 to 72 months.
Statistical Analysis
Functional outcomes were assessed using the Lysholm score,30 International Knee Documentation Committee (IKDC) score,14 knee joint ROM, and amount of laxity on stress radiographs. A standard t test was used to compare the outcomes of the KD3-M and KD3-L groups (Table 2). Other factors that could affect outcomes were documented and analyzed statistically (Table 3). These were age, time since injury, energy of trauma (high or low), frank dislocation at the time of injury, collateral ligament injury grade and location (femoral, tibial, or midsubstance), modality of treatment for the collateral ligament injury, presence of associated injuries, type of graft, and follow-up period. All statistical analyses were conducted using SPSS version 20 software (IBM). A standard t test was used to analyze factors with 2 categories, analysis of variance was used for factors with ≥3 categories, and a scatter plot and Pearson correlation were used for continuous variables. Multiple linear regression was carried out for the variables that were found to have an association with outcomes.
TABLE 2.
Comparison of Outcomes Between KD3-M and KD3-L Groupsa
| No. of Patients | IKDC Score | Lysholm Score | Knee Flexion ROM, deg | |
|---|---|---|---|---|
| KD3-M | 31 | 75.08 | 88.03 | 127.10 |
| KD3-L | 14 | 73.97 | 86.85 | 126.07 |
| P value | .768 | .689 | .798 |
aOutcomes are presented as means. IKDC, International Knee Documentation Committee; KD3-L, lateral knee dislocation–3; KD3-M, medial knee dislocation–3; ROM, range of motion.
TABLE 3.
Analysis of Outcomes After Grouping by Variablesa
| No. of Patients | IKDC Score | Lysholm Score | Knee Flexion ROM, deg | |
|---|---|---|---|---|
| Time to surgery | ||||
| Acute (<6 wk) | 35 | 77.00 | 89.51 | 127.86 |
| Subacute (6-12 wk) | 5 | 66.26 | 86.00 | 121.00 |
| Chronic (>12 wk) | 5 | 67.40 | 76.40 | 125.00 |
| P value (ANOVA) | .045 | .006 | .486 | |
| Type of dislocation | ||||
| Frank | 9 | 67.62 | 80.66 | 119.44 |
| Transient | 36 | 76.51 | 89.41 | 128.61 |
| P value (standard t test) | .037 | .007 | .043 | |
| Type of graft | ||||
| All tendon grafts | 28 | 75.76 | 88.32 | 129.11 |
| Graft with at least 1 bone plug | 17 | 73.04 | 86.58 | 122.94 |
| P value (standard t test) | .451 | .535 | .102 | |
| Energy of trauma | ||||
| Low | 9 | 73.31 | 88.77 | 127.22 |
| High | 36 | 75.09 | 87.38 | 126.67 |
| P value (ANOVA) | .855 | .774 | .661 | |
| Treatment of collateral ligament | ||||
| Conservative | 23 | 74.36 | 87.78 | 128.70 |
| Repair | 11 | 76.10 | 88.72 | 127.27 |
| Reconstruction/augmentation | 11 | 74.16 | 86.36 | 122.27 |
| P value (ANOVA) | .906 | .829 | .364 | |
| Grade of collateral ligament injury | ||||
| Grade 2 | 10 | 70.64 | 84.40 | 125.50 |
| Grade 3 | 35 | 75.91 | 88.60 | 127.14 |
| P value (standard t test) | .207 | .194 | .713 | |
| Meniscus | ||||
| Injured | 15 | 73.73 | 86.20 | 126.33 |
| Not injured | 30 | 76.76 | 90.60 | 127.67 |
| P value (standard t test) | .414 | .122 | .735 | |
| Associated injuries in knee | 22 | 74.00 | 88.00 | 125.00 |
| P value (standard t test) | .678 | .647 | .361 |
aOutcomes are presented as means. ANOVA, analysis of variance; IKDC, International Knee Documentation Committee; ROM, range of motion.
Results
The mean IKDC and Lysholm scores for the 45 patients were 74.74 and 87.66, respectively. The mean knee flexion ROM was 126.78°. There was no statistically significant difference in outcomes between the KD3-M and KD3-L groups (Table 2). When the patients were grouped by time to surgery (acute, <6 weeks; subacute, 6-12 weeks; and chronic >12 weeks), the outcomes of the subacute and chronic groups were significantly worse than those of the acute group (Table 3). The mean IKDC score, Lysholm score, and knee flexion ROM for the 3 groups were as follows, respectively: in the acute group (35 patients), 77.00, 89.51, and 127.86°; in the subacute group (5 patients), 66.26, 86.00, and 121.00°; and in the chronic group (5 patients), 67.40, 76.40, and 125.00°. The P values of the 3 outcome variables were .045, .006, and .486, respectively.
When the influence of dislocation at the time of injury was analyzed, the mean IKDC score, Lysholm score, and knee flexion ROM of the 9 patients who had a frank dislocation were 67.62, 80.66, and 119.44°, respectively; in the 36 patients without a frank dislocation, the values were 76.51, 89.41, and 128.61°. The P values were .037, .007, and .043, respectively. Patients who had a dislocation had significantly worse outcomes in comparison with the ones who had no dislocation (Table 3).
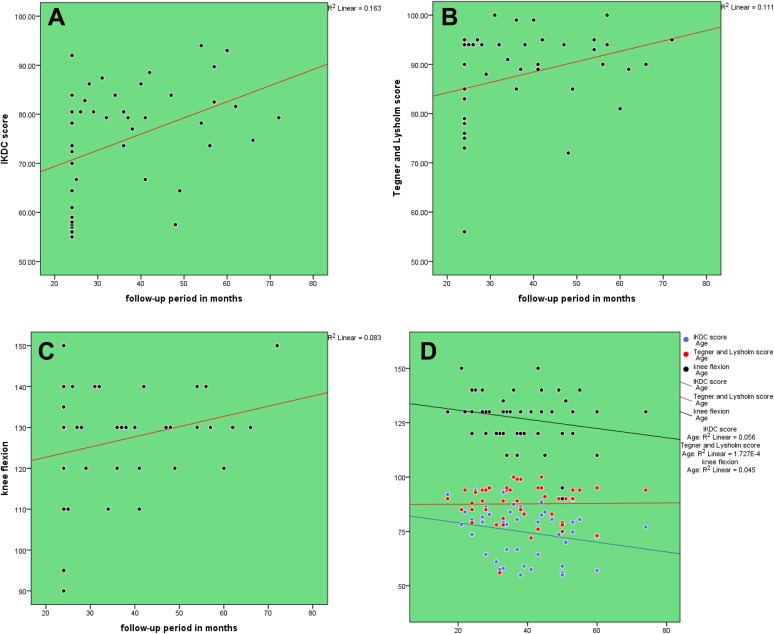
The relation between period of follow-up and IKDC score, Lysholm score, and knee flexion ROM demonstrated Pearson correlation coefficients (r) of 0.403 (P = .006), 0.333 (P = .025), and 0.391 (P = .008), respectively. A scatter plot showing these relationships is shown in Figure 2A to 2C. None of the other factors—age, type of graft, energy of trauma, collateral ligament that was injured, location and grade of injury, or meniscal injuries—had any bearing on the outcomes (Figure 2D and Table 3).
Figure 2.
(A) Scatter plot showing the relation between period of follow-up in months and International Knee Documentation Committee (IKDC) score. (B) Scatter plot showing the relation between period of follow-up in months and Lysholm score. (C) Scatter plot showing the relation between period of follow-up and postoperative knee flexion range of motion. (D) Scatter plot showing the relation between age and outcome measures: IKDC score, Lysholm score, and knee flexion range of motion.
Multiple linear regression analysis for the IKDC score showed an R 2 value of 0.321, which indicates that 32.1% of the variability in the IKDC scores can be explained by the presence or absence of dislocations, the time to surgery, and follow-up duration. Also, these factors significantly predicted the IKDC score (F(3,41) = 6.454, P = .001). The unstandardized coefficients for these 3 factors were 6.284, –4.826, and 0.319, respectively, implying the amount of variability that each of these factors produced in the IKDC score when all the other factors were held constant. Regression analysis for the Lysholm score showed an R 2 value of 0.392 (F(3,41) = 8.800, P < .01). The unstandardized coefficients for dislocation status, time to surgery, and follow-up duration were 6.247, −5.100, and 0.200, respectively. Regression analysis for knee flexion ROM showed an R 2 value of 0.169 (F(3,41) = 2.781, P = .053). The unstandardized coefficients for these 3 factors were 8.271, –1.077, and 0.237, respectively.
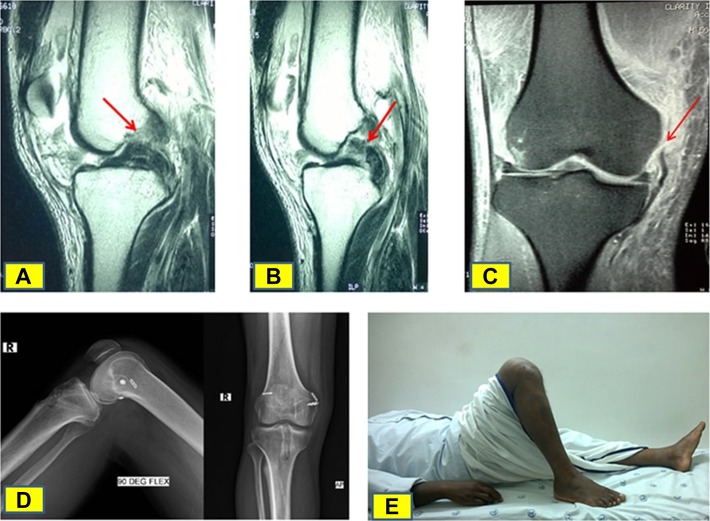
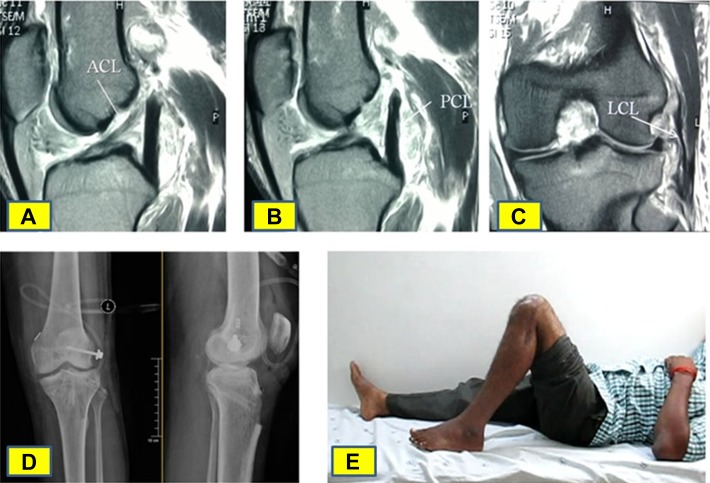
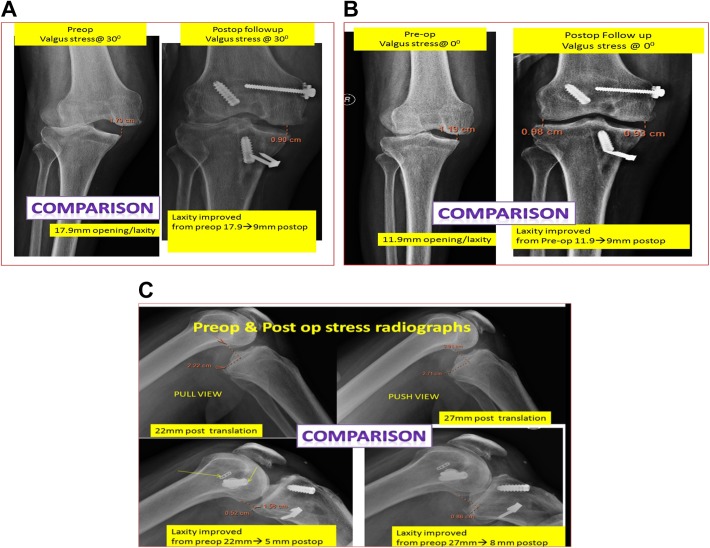
Regarding laxity on stress radiographs, the differences that were statistically significant are shown in Table 4. The differences were hardly greater than 1 or 1.5 mm. Also, there was no correlation between functional outcomes and the amount of laxity measured in stress views. Thus, the clinical significance of the difference in laxity is doubtful. Two of the 45 patients had postoperative stiffness, for which arthroscopic arthrolysis was performed. One of these patients had knee flexion ROM of 20° to 90° and improved to 0° to 120°. The other patient had only 0° to 60° of movement and improved to 0° to 130°. One patient developed an infection at the graft donor site, which needed debridement; the infection was resolved with antibiotics and wound care. A representative case sample for KD3-M and KD3-L injuries is shown in Figures 3 and 4. An example of stress radiographs is shown in Figure 5.
TABLE 4.
Statistically Significant Differences in Mean Laxity on Stress Radiographsa
| Mediolateral Laxity in Extension, mm | Mediolateral Laxity in 30° of Flexion, mm | Anterior Translation, mm | Posterior Translation, mm | |||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Grade 2 Collateral Injury | Grade 3 Collateral Injury | With Dislocation | Without Dislocation | All Tendon Grafts | Graft With a Bone Plug | KD3-M | KD3-L | Acute | Subacute | Chronic |
| 2.23 | 2.97 | 4.74 | 5.06 | 5.69 | 3.86 | 4.30 | 3.29 | 2.78 | 3.21 | 5.68 |
| P = .031 | P = .032 | P = .007 | P = .011 | P = .03 | ||||||
aKD3-L, lateral knee dislocation--3; KD3-M, medial knee dislocation–3.
Figure 3.
(A) Magnetic resonance imaging (MRI) showing a torn anterior cruciate ligament (red arrow). (B) MRI showing a torn posterior cruciate ligament (red arrow). (C) MRI showing a medial collateral ligament tear at the femoral attachment (red arrow). (D) Postoperative radiograph of the knee in lateral and anteroposterior views. (E) Clinical photograph of the patient’s knee at final follow-up showing the amount of knee flexion.
Figure 4.
(A) Magnetic resonance imaging (MRI) showing a torn anterior cruciate ligament (ACL) (white arrow). (B) MRI showing a torn posterior cruciate ligament (PCL) (white arrow). (C) MRI showing a lateral collateral ligament (LCL) tear at the fibular attachment (white arrow). (D) Postoperative radiograph of the knee in anteroposterior and lateral views. (E) Clinical photograph of the patient’s knee at final follow-up showing the amount of knee flexion.
Figure 5.
(A) Comparison of preoperative and postoperative valgus stress views at 30° of flexion. (B) Comparison of preoperative and postoperative valgus stress views at 0° of flexion. (C) Comparison of preoperative and postoperative pull and push views.
Discussion
A knee dislocation with MLKI is a complex orthopaedic condition. Of all the patterns described by Schenck,37 a KD3 injury is the most common type.13,29,46,47 KD3 injuries are further divided into KD3-M and KD3-L depending on whether the MCL or LCL is injured. There is debate regarding the management of KD3 injuries, such as conservative versus operative for collateral ligaments, single-stage versus staged procedure, early versus late, and repair versus reconstruction of collateral ligaments. Historically, the management of MLKIs started with conservative treatment and progressed on to early surgical repair. Because the results of early repair of the ligaments were encouraging and were better when compared with conservative management, there was a paradigm shift toward reconstructing the injured ligaments for better restoration of knee function. In the meta-analyses performed by Dedmond and Almekinders6 and Peskun and Whelan,35 the surgical treatment for multiligamentous injuries showed better results in terms of functional outcomes and return to activity. However, these studies have not compared KD3-M and KD3-L injuries and have not looked into the influence of predictive factors and outcomes of these injuries.
There are 2 methods of staging the procedure for reconstruction in MLKIs. The first method is to repair the collateral ligament in the first stage and reconstruct the cruciate ligaments in the second stage. The second method is to reconstruct the PCL in the first stage, while the ACL and collateral ligaments are reconstructed at a later date if needed. Bin and Nam1 published their experience of the 2-staged management of MLKIs. The reason behind their approach was to decrease the operative time and the chances of arthrofibrosis. Yet, the major disadvantage is a longer recovery period; the time between the 2 surgical stages was 3 to 6 months. In young patients who are in a productive working phase of life, a long recovery and rehabilitation would lead to significant financial loss of work hours. Single-stage surgery for KD3 injuries reduces the time, cost, and morbidities associated with 2 surgical procedures. Contrary to the popular apprehension of developing arthrofibrosis with a single-stage approach, in our study, there were only 2 of 45 patients who needed arthroscopic arthrolysis, and the final outcomes of these 2 patients were satisfactory. Thus, once local and systemic conditions become optimal, single-stage reconstruction of KD3 injuries can be performed to obtain optimum results. Khakha et al21 showed good functional outcomes with a single-stage approach. In their series, 36 patients with KD3/KD4 injuries underwent surgery in a single stage, with a mean time to surgery of 12 days (range, 1-21 days). The median Lysholm score was 80. However, unlike our study, there was no separate analysis comparing subacute and chronic cases.
Regarding the timing of surgery, early surgery (<10 days) has many issues such as wound healing, risk of infection, arthrofibrosis, extravasation of fluid, and compartment syndrome.13,28 On the contrary, late surgery (>6 weeks) can cause scarring of the collateral ligaments, in which the chances of repair become bleak.42 Ideally, repair can be performed within 3 to 4 weeks when the tissues are amenable to repair. In our study, we repaired the collateral ligaments when intraoperative laxity was grade 3. Early surgery is particularly important when allografts are not available and all reconstruction procedures have to be performed using autografts. In a meta-analysis conducted by Levy et al,28 after evaluating the results of 5 studies10,13,29,43,45 with a total of 130 patients, the authors concluded that the early operative treatment of a multiligament-injured knee yields improved functional and clinical outcomes compared with nonoperative management or delayed surgery. Observations from our study also showed better outcomes in the acute group. Thus, we recommend early reconstruction by the second week once the swelling has subsided and 90° of knee flexion is attained, when expected capsular healing also occurs.
Apart from reconstructing the cruciate ligaments, identifying and managing collateral ligament injuries are essential. Gross mediolateral laxity will lead to failure of cruciate ligament reconstruction because of increased stress on the grafts. King et al22 compared the outcomes of surgically treated KD3-M and KD3-L injuries over a period of 20 years. They found that medial-sided repair had poorer outcomes when compared with medial-sided reconstruction, lateral-sided repair, and lateral-sided reconstruction. Unlike our study, they had no patients whose collateral ligament injury was conservatively managed, and the approach to their decision of repair/reconstruction was not explained. Further, this was a study spanning 20 years in which there can be possible changes in approach, techniques, surgical protocols, instrumentation, and implants. In our study, there was no significant difference in the functional outcomes between the KD3-M and KD3-L groups and also between the modes of treatment of the collateral ligament injury. However, of the 31 patients with an MCL injury, only 7 (22.5%) were repaired and 2 (6.5%) were reconstructed, whereas of 14 LCL/PLC injuries, 4 (28.5%) were repaired and 9 (64.3%) were reconstructed, depending on the time of presentation.
As observed in our series, compared with KD3-M injuries, KD3-L injuries needed more surgical attention, implying the greater importance and anatomic complexity of the PLC. Earlier studies have shown that the conservative treatment of PLC injuries leads to residual laxity.18 Deficiencies in the PLC put more stress on the ACL graft during varus loading and internal rotation and more stress on the PCL graft during varus stress and external rotation.24,25 Stannard et al39 compared repair and reconstruction of PLC injuries in 57 knees and found a failure rate of 37% in repaired cases and 9% in reconstructed cases. They concluded that reconstruction is a better option for PLC injuries. A similar study conducted by Levy et al27 also favored reconstruction of the LCL and PLC over repair. Stannard et al38 also compared the outcomes of posteromedial corner repair with reconstruction after a knee dislocation in 73 patients. With an average follow-up of 43 months, 5 (20%) of the 25 repairs failed, whereas only 2 (4%) of the 48 reconstructions failed. These authors concluded that reconstruction of the posteromedial corner yields better stability than repair.
The management of collateral ligaments is the crucial step in KD3 injuries because cruciate ligaments are generally reconstructed and addressing collateral ligament injuries determines the difference in final outcomes. In the literature, there is no clear-cut philosophy on conservative versus surgical treatment for collateral ligament injuries after cruciate ligament reconstruction, and the importance of an intraoperative assessment of collateral ligaments needs to be stressed for decision making. In our opinion, the management of collateral ligament injuries should be individualized depending on chronicity, soft tissue damage, reparability based on an intraoperative assessment, and site of injury on MRI. The intraoperative assessment of mediolateral laxity after reconstruction of the cruciate ligaments reduced the number of collateral ligament injuries that were treated surgically. The reason that we found no difference in outcomes between the KD3-L and KD3-M groups, and between the 3 treatment modalities, was because appropriate management was instituted on a case-by-case basis.
The site of an MCL injury determines the healing of the ligament. It is widely perceived that a tibial-side avulsion of both the superficial and deep MCL does not heal because the synovial fluid tracks down and impairs ligament bone healing.48 However, in our study, there was no such difference (see Table 3). The reason for this is also probably because of appropriate management based on the situation. Twenty-two patients had an associated injury to ≥1 structures (meniscus, cartilage, MPFL, patellar tendon) in addition to the cruciate and collateral ligaments. These structures were managed based on the severity and feasibility of repair. The presence of these injuries did not produce any significant difference in the final outcomes of these patients when compared with the other patients.
Knee function after dislocations caused by high-energy trauma is usually worse compared with low-energy trauma because of additional injuries to the soft tissue components around the knee.46 High-energy trauma is known to result in a higher incidence of vascular injuries.8 In our study, the energy of the trauma did not seem to have a significant influence on the outcomes of surgery. However, the presence of dislocations influenced the outcomes significantly. The energy of trauma that we mention in our study is basically the nature of the force that caused the accident but not the exact amount of energy absorbed by the knee. A frank dislocation at the time of injury signifies that the amount of trauma sustained by the knee at the time of injury is high, whereas a transient dislocation and relocation could mean a low-energy impact. Rather than the energy of trauma, energy absorbed by the knee (ie, presence or absence of dislocations) should be more significant, thereby influencing the outcomes.
All the grafts used in our study were tendon autografts. We used 1 or more of the 3 commonly used tendon grafts: hamstring tendon, patellar tendon, and quadriceps tendon. Because a mixture of these tendons was used in many cases, comparing the influence of these tendon grafts on outcomes will be difficult and inappropriate. Yet, we made a comparison between cases with entirely tendinous grafts (ie, all hamstring) and cases with at least 1 graft with a bony component (ie, patellar tendon or quadriceps tendon), and we found no significant difference in outcomes (see Table 3).
Multiple linear regression analysis showed that 3 factors, namely, the presence or absence of dislocations, the time to surgery, and the follow-up duration, had a significant association with outcomes. Thus, in KD3 injuries in which a standard protocol as described in our study is followed, outcomes can be predicted by these 3 factors.
Limitations
The number of patients in our study was limited. There was no case managed in 2 stages to make a comparison with single-stage management. Although all patients returned to their previous occupation level, no one became involved in any contact sports or high-level physical activity. The reason for this was because of a low-demand lifestyle and apprehension after surgery. This reduced the functional outcome scores less than expected because patients never tried to push to the maximum level. The intraoperative measurement of laxity was assessed by a clinical comparison with the contralateral uninjured limb; instead, a measurement performed using a radiological ruler under fluoroscopy would have been more appropriate. Also, the KT-1000 arthrometer was not employed to measure objective laxity.
Conclusion
Despite anatomic and biomechanical differences between the KD3-M and KD3-L types of MLKIs, single-stage management did not produce any significant difference in outcomes. Addressing all the 3 damaged structures in KD3 injuries at a single stage provided favorable clinical outcomes, thereby obviating the need for the traditional method of staged reconstruction. This minimized the morbidity of 2 surgical procedures and shortened the rehabilitation time. Surgical management within the first 6 weeks provided better outcomes in these complex MLKIs. Early intervention provided us with an opportunity for repairing the collateral ligaments. The presence of a frank dislocation at the time of presentation was an indicator of serious and high-energy trauma and could produce poorer outcomes. Regarding the management of collateral ligament injuries after cruciate ligament reconstruction, we recommend repair for cases in which there is grade 3 mediolateral laxity, provided the procedure is performed within 3 to 4 weeks of injury. If the injury is chronic, then reconstruction has to be performed. When laxity is grade ≤2 after cruciate ligament reconstruction, collateral ligaments can be managed conservatively.
Footnotes
The authors declare that they have no conflicts of interest in the authorship and publication of this contribution. AOSSM checks author disclosures against the Open Payments Database (OPD). AOSSM has not conducted an independent investigation on the OPD and disclaims any liability or responsibility relating thereto.
Ethical approval for this study was obtained from the institutional review board of Ganga Medical Centre and Hospitals (No. 00004503).
References
- 1. Bin SI, Nam TS. Surgical outcome of 2-stage management of multiple knee ligament injuries after knee dislocation. Arthroscopy. 2007;23(10):1066–1072. [DOI] [PubMed] [Google Scholar]
- 2. Bonnevialle P, Dubrana F, Galau B, et al. Common peroneal nerve palsy complicating knee dislocation and bicruciate ligaments tears. Orthop Traumatol Surg Res. 2010;96:64–69. [DOI] [PubMed] [Google Scholar]
- 3. Borden PS, Kantaras AT, Caborn DN. Medial collateral ligament reconstruction with allograft using a double-bundle technique. Arthroscopy. 2002;18(4):E19. [DOI] [PubMed] [Google Scholar]
- 4. Cole BJ, Harner CD. The multiple ligament injured knee. Clin Sports Med. 1999;18:241–262. [DOI] [PubMed] [Google Scholar]
- 5. Cush G, Irgit K. Drop foot after knee dislocation: evaluation and treatment. Sports Med Arthrosc. 2011;19:139–146. [DOI] [PubMed] [Google Scholar]
- 6. Dedmond BT, Almekinders LC. Operative versus nonoperative treatment of knee dislocations: a meta-analysis. Am J Knee Surg. 2001;14(1):33–38. [PubMed] [Google Scholar]
- 7. Eger M, Huler T, Hirsch M. Popliteal artery occlusion associated with dislocation of the knee joint: report of a case with successful surgical repair. Br J Surg. 1970;57:315–317. [DOI] [PubMed] [Google Scholar]
- 8. Engebretsen L, Risberg MA, Robertson B, Ludvigsen TC, Johansen S. Outcome after knee dislocations: a 2-9 years follow-up of 85 consecutive patients. Knee Surg Sports Traumatol Arthrosc. 2009;17(9):1013–1026. [DOI] [PubMed] [Google Scholar]
- 9. Fanelli GC. Treatment of combined anterior cruciate ligament-posterior cruciate ligament-lateral side injuries of the knee. Clin Sports Med. 2000;19:493–502. [DOI] [PubMed] [Google Scholar]
- 10. Fanelli GC, Giannotti BF, Edson CJ. Arthroscopically assisted combined posterior cruciate ligament/posterior lateral complex reconstruction. Arthroscopy. 1996;12:521–530. [DOI] [PubMed] [Google Scholar]
- 11. Fanelli GC, Orcutt DR, Edson CJ. The multiple-ligament injured knee: evaluation, treatment, and results. Arthroscopy. 2005;21(4):471–486. [DOI] [PubMed] [Google Scholar]
- 12. Green NE, Allen BL. Vascular injuries associated with dislocation of the knee. J Bone Joint Surg Am. 1977;59:236–239. [PubMed] [Google Scholar]
- 13. Harner CD, Waltrip RL, Bennett CH, Francis KA, Cole B, Irrgang JJ. Surgical management of knee dislocations. J Bone Joint Surg Am. 2004;86:262–273. [DOI] [PubMed] [Google Scholar]
- 14. Hefti F, Muller W, Jakob RP, Staubli HU. Evaluation of knee ligament injuries with the IKDC form. Knee Surg Sports Traumatol Arthrosc. 1993;1:226–234. [DOI] [PubMed] [Google Scholar]
- 15. Hegyes MS, Richardson MW, Miller MD. Knee dislocation: complications of nonoperative and operative management. Clin Sports Med. 2000;19:519–543. [DOI] [PubMed] [Google Scholar]
- 16. Hoover NW. Injuries of the popliteal artery associated with fractures and dislocations. Surg Clin North Am. 1961;41:1099–1112. [DOI] [PubMed] [Google Scholar]
- 17. Jones RE, Smith EC, Bone GE. Vascular and orthopedic complications of knee dislocation. Surg Gynecol Obstet. 1979;149:554–558. [PubMed] [Google Scholar]
- 18. Kannus P. Nonoperative treatment of grade II and III sprains of the lateral ligament compartment of the knee. Am J Sports Med. 1989;17:83–88. [DOI] [PubMed] [Google Scholar]
- 19. Kannus P, Järvinen M. Nonoperative treatment of acute knee ligament injuries: a review with special reference to indications and methods. Sports Med. 1990;9:244–260. [DOI] [PubMed] [Google Scholar]
- 20. Kennedy J. Complete dislocation of knee joint. J Bone Joint Surg Am. 1963;45:889–904. [PubMed] [Google Scholar]
- 21. Khakha RS, Day AC, Gibbs J, et al. Acute surgical management of traumatic knee dislocations: average follow-up of 10 years. Knee. 2016;23:267–275. [DOI] [PubMed] [Google Scholar]
- 22. King A, Krych AJ, Prince MR, Pareek A, Stuart MJ, Levy BA. Surgical outcomes of medial versus lateral multiligament-injured, dislocated knees. Arthroscopy. 2016;32(9):1814–1819. [DOI] [PubMed] [Google Scholar]
- 23. LaPrade RF, Johansen S, Wentorf FA, Engebretsen L, Esterberg JL, Tso A. An analysis of an anatomical posterolateral knee reconstruction: an in vitro biomechanical study and development of a surgical technique. Am J Sports Med. 2004;32(6):1405–1414. [DOI] [PubMed] [Google Scholar]
- 24. LaPrade RF, Muench C, Wentorf F, Lewis JL. The effect of injury to the posterolateral structures of the knee on force in a posterior cruciate ligament graft: a biomechanical study. Am J Sports Med. 2002;30:233–238. [DOI] [PubMed] [Google Scholar]
- 25. LaPrade RF, Resig S, Wentorf F, Lewis JL. The effects of grade III posterolateral knee complex injuries on anterior cruciate ligament graft force: a biomechanical analysis. Am J Sports Med. 1999;27:469–475. [DOI] [PubMed] [Google Scholar]
- 26. Larson RV. Isometry of the lateral collateral and popliteofibular ligaments and techniques for reconstruction using a free semitendinosus tendon graft. Oper Tech Sports Med. 2012;20:65–71. [Google Scholar]
- 27. Levy BA, Dajani KA, Morgan JA, Shah JP, Dahm DL, Stuart MJ. Repair versus reconstruction of the fibular collateral ligament and posterolateral corner in the multiligament-injured knee. Am J Sports Med. 2010;38:804–809. [DOI] [PubMed] [Google Scholar]
- 28. Levy BA, Dajani KA, Whelan DB, et al. Decision making in the multiligament-injured knee: an evidence-based systematic review. Arthroscopy. 2009;25(4):430–438. [DOI] [PubMed] [Google Scholar]
- 29. Liow RY, McNicholas MJ, Keating JF, Nutton RW. Ligament repair and reconstruction in traumatic dislocation of the knee. J Bone Joint Surg Br. 2003;85:845–851. [PubMed] [Google Scholar]
- 30. Lysholm J, Gillquist J. Evaluation of knee ligament surgery results with special emphasis on use of a scoring scale. Am J Sports Med. 1982;10:150–154. [DOI] [PubMed] [Google Scholar]
- 31. Mariani PP, Margheritini F, Camillieri G. One-stage arthroscopically assisted anterior and posterior cruciate ligament reconstruction. Arthroscopy. 2001;17:700–707. [DOI] [PubMed] [Google Scholar]
- 32. McDonough EB, Jr, Wojtys EM. Multiligamentous injuries of the knee and associated vascular injuries. Am J Sports Med. 2009;37:156–159. [DOI] [PubMed] [Google Scholar]
- 33. Montgomery JB, Steadman JR. Rehabilitation of the injured knee. Clin Sports Med. 1985;4:333–343. [PubMed] [Google Scholar]
- 34. Niall DM, Nutton RW, Keating JF. Palsy of the common peroneal nerve after traumatic dislocation of the knee. J Bone Joint Surg Br. 2005;87:664–667. [DOI] [PubMed] [Google Scholar]
- 35. Peskun CJ, Whelan DB. Outcomes of operative and non operative treatment of multiligament knee injuries: an evidence-based review. Sports Med Arthrosc Rev. 2011;19(2):167–173. [DOI] [PubMed] [Google Scholar]
- 36. Rihn JA, Groff YJ, Harner CD, Cha PS. The acutely dislocated knee: evaluation and management. J Am Acad Orthop Surg. 2004;12:334–346. [DOI] [PubMed] [Google Scholar]
- 37. Schenck RC. The dislocated knee. Instr Course Lect. 1994;43:127–136. [PubMed] [Google Scholar]
- 38. Stannard JP, Black BS, Azbell C, Volgas DA. Posteromedial corner injury in knee dislocations. J Knee Surg. 2012;25(5):429–434. [DOI] [PubMed] [Google Scholar]
- 39. Stannard JP, Brown SL, Farris RC, McGwin G, Jr, Volgas DA. The posterolateral corner of the knee: repair versus reconstruction. Am J Sports Med. 2005;33:881–888. [DOI] [PubMed] [Google Scholar]
- 40. Stannard JP, Sheils TM, Lopez-Ben RR, McGwin G, Jr, Robinson JR, Volgas DA. Vascular injuries in knee dislocations: the role of physical examination in determining the need for arteriography. J Bone Joint Surg Am. 2004;86:910–915. [PubMed] [Google Scholar]
- 41. Steele HL, Singh A. Vascular injury after occult knee dislocation presenting as compartment syndrome. J Emerg Med. 2012;42:271–274. [DOI] [PubMed] [Google Scholar]
- 42. Tay AK, MacDonald PB. Complications associated with treatment of multiple ligament injured (dislocated) knee. Sports Med Arthrosc. 2011;19(2):153–161. [DOI] [PubMed] [Google Scholar]
- 43. Tzurbakis M, Diamantopoulos A, Xenakis T, Georgoulis A. Surgical treatment of multiple knee ligament injuries in 44 patients: 2-8 years follow-up results. Knee Surg Sports Traumatol Arthrosc. 2006;14:739–749. [DOI] [PubMed] [Google Scholar]
- 44. Wascher DC. High-velocity knee dislocation with vascular injury: treatment principles. Clin Sports Med. 2000;19:457–477. [DOI] [PubMed] [Google Scholar]
- 45. Wascher DC, Becker JR, Dexter JG, Blevins FT. Reconstruction of the anterior and posterior cruciate ligaments after knee dislocation: results using fresh-frozen non irradiated allografts. Am J Sports Med. 1999;27:189–196. [DOI] [PubMed] [Google Scholar]
- 46. Wascher DC, Dvirnak PC, DeCoster TA. Knee dislocation: initial assessment and implications for treatment. J Orthop Trauma. 1997;11:525–529. [DOI] [PubMed] [Google Scholar]
- 47. Werier J, Keating JF, Meek RN. Complete dislocation of the knee: the long-term results of ligamentous reconstruction. Knee. 1998;5:255–260. [Google Scholar]
- 48. Wilson TC, Satterfield WH, Johnson DL. Medial collateral ligament “tibial” injuries: indications for acute repair. Orthopedics. 2004;27(4):389–393. [DOI] [PubMed] [Google Scholar]