Highlights
-
•
The authors present a rare case of multiple giant eccrine spiradenomas of the head and neck.
-
•
A young girl presented with multiple swellings over the head and neck.
-
•
The patient had a psychological trauma with a negative impact on her social life.
-
•
There is need to establish a surgical protocol for the treatment of adnexal tumors.
-
•
Our integrated surgical approach showed excellent aesthetic and functional results.
Abstract
Introduction
The authors present a “four-step” integrated surgical protocol to treat a rare case of multiple giant eccrine spiradenoma (ES) of the head and neck in a young patient.
Presentation of case
An 18-year-old female patient presented with multiple swellings in the head and neck regions. The patient had a severe psychological trauma with a negative impact on her social life. Physical examination revealed multiple papulo-nodular swellings measuring between 5 cm × 8 cm and up to 10 cm × 20 cm in size with cerebriform aspect and soft consistency. Major lesions were located in the scalp, frontal area, neck, occipitotemporal, and retroauricular regions. Tissue biopsy found a benign composite adnexal neoplasm consisted in ES, trichoepithelioma, and cylindroma, a typical feature of Brooke-Spiegler Syndrome. A staged excision was planned, and available reconstructive options were considered. Scalp reconstruction included tissue expansions, advancement flaps, skin grafts, and dermal regeneration template (Integra®). All treatments were successful, and no recurrence was observed. The patient returned to a normal social life, and a radical excision with satisfying aesthetic results was achieved.
Discussion
Although adnexal tumors are benign in most of the cases, these lesions are prone to arise in the craniofacial region, thereby causing aesthetic discomfort associated with pain, hemorrhage, and infection to the patient every day. Furthermore, there is a potential risk of malignant transformation. These concerns demonstrate the need to establish a surgical protocol for the treatment of adnexal tumors.
Conclusions
Our integrated surgical approach showed excellent aesthetic and functional results with benefits to the patient’s life and complete oncological excision.
1. Introduction
Eccrine spiradenoma (ES) is a rare benign adnexal neoplasm first described by Kersting and Helwig [1] in 1956. It has been historically described as a tumor with eccrine differentiation, although it is currently considered as an apocrine process [2,3].
The majority of ES presentations are solitary. ES mostly occurs in patients aged between 15 and 35 years, with nearly equal incidence in both males and females.
The presence of concomitant cylindroma, trichoepithelioma, and spiradenoma should promptly suspect a diagnosis of Brooke–Spiegler Syndrome (BSS) [2,4]. BSS is a rare autosomal dominant disorder characterized by a predisposition for the development of multiple adnexal neoplasms. Although the exact etiology is unknown, mutations or loss of heterozygosity in the cylindromatosis (CYLD) gene (16q12-q1) are identified in the majority of the cases [5,6].
Malignant ES, or spiradenocarcinoma, is exceedingly rare but quite aggressive. It generally arises from long-standing benign ES [4,7,8]. Dabska et al. [9] first described spiradenocarcinoma in 1972 and only ∼150 cases of malignant transformation are reported in the literature [10].
ES usually appears as a small, painful, grey-to-pink nodule on the upper half of the body. Multiple ES is an extremely rare presentation comprising less than 2% of all cases and appears to be predominant among women.
The designation “giant eccrine spiradenoma” was first introduced by Lauret et al. [11] in 1977. Later, the name “giant vascular eccrine spiradenoma” (GVES) was introduced in 1986 by Cotton et al. [12] to describe those rare cases of giant ES clinically distinguished by a large size (>2 cm) and histopathologically by a marked vascularity [13,14].
Histological findings of ES may present as tumors arranged in sheets, cords, or islands. Tumor cells are strongly basophilic. Sometimes, lymphocyte infiltration and abundant telangiectasia are detected in the tumor area. Both ES and dermal cylindroma are adnexal tumors. They are closely related and share many morphological features. Occasionally, the histological results demonstrate hybrid tumors with spiradenomatous and cylindromatous components within the same biopsy [4,10].
Considering the rarity of multiple giant ES in the current literature, the authors report this case to increase awareness and help establish the most appropriate approach in managing the disease in terms of physical examination, histological findings, and treatment [2].
Treatments for ES have not yet been routinely established. The gold standard is surgical excision with reported low rates of recurrence for both benign and malignant ES [2,3].
Reconstruction after removal of oncologic lesions in the head and neck regions remains a surgical challenge. The repair of skin defects poses a significant problem for many clinicians, especially when the lesions are aesthetically intolerable, painful, and increasing in size or number [15].
The purpose of this case report is to present our reconstructive protocol after the surgical resection of multiple giant adnexal tumors in a young female patient. This case highlights the need to develop and establish an integrated surgical protocol for the treatment of this kind of tumors to achieve satisfying aesthetic results and radical oncological resection. The work is compliant with the SCARE Guidelines [16].
2. Presentation of case
In March 2012, an 18-year-old female patient with multiple swellings in the head and neck regions (Fig. 1) was admitted to the Department of Plastic Surgery. History records revealed that the patient developed lesions at the age of 4 years, which then gradually progressed with increasing pain and burning sensation. She did not have other comorbidities. The patient presented with severe psychological trauma, which had a negative impact on her social life and education.
Fig. 1.
An 18-year old female patient affected with Brooke–Spiegler Syndrome. The patient presented with multiple swellings in the head and neck regions, with histological diagnosis of adnexal tumors (eccrine spiradenoma, trichoepithelioma, and cylindroma).
Local examination revealed multiple papulo-nodular swellings measuring between 5 cm × 8 cm and up to 10 cm × 20 cm in size with cerebriform aspect, soft consistency, and bleeding after minimal trauma. Lesions were tender, firm, and fixed to the skin. Major lesions were located on the scalp, frontal, neck, occipitotemporal, and retroauricular regions, with multiple smaller lesions located at the nuchal and laterocervical regions. Regional adenopathy was not present. Magnetic resonance imaging (MRI) confirmed that lesions were confined to the skin with no involvement of deeper structures.
During the same period, multiple biopsies, each measuring 1.6 cm × 0.8 cm × 2 cm, were collected. Histological analysis diagnosed benign adnexal neoplasm with ES, trichoepithelioma, and cylindroma. On the basis of the clinical findings and histopathological examination, the patient was diagnosed with BSS (Fig. 2).
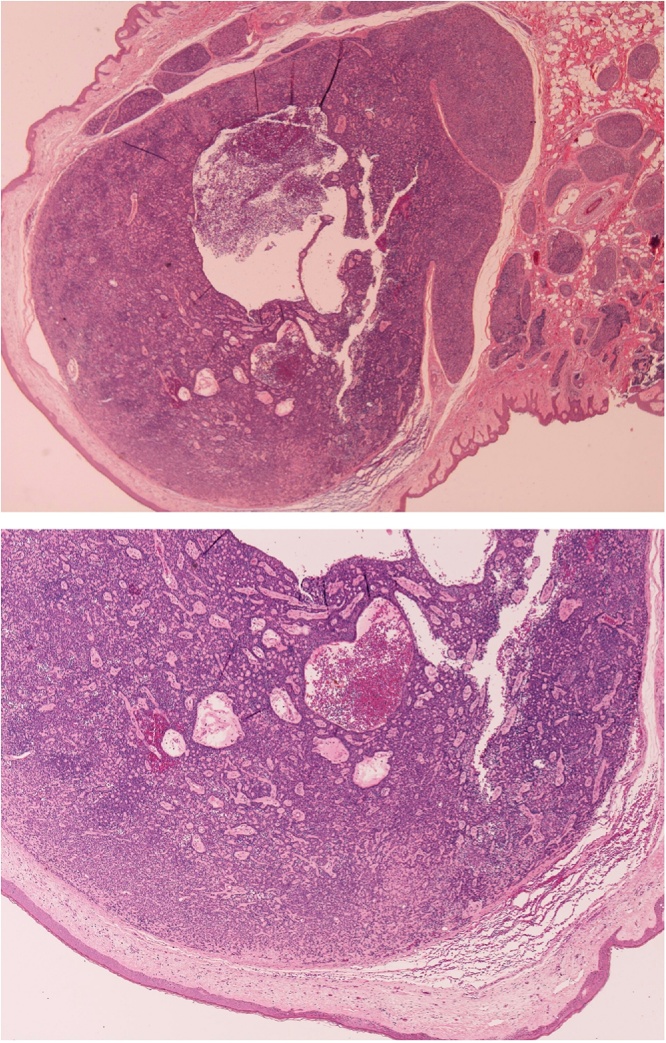
Fig. 2.
Skin biopsies stained with hematoxylin–eosin (HE) revealed benign eccrine spiradenoma associated with circumscribed epithelial neoplasm in the mid-to-deep dermis with basaloid inclusion (cylindromas) and basaloid inclusions with immature hair follicles and abundant stroma (trichoepithelioma) (HE, original magnification, x20 and x40).
A staged wide excision was planned, and reconstruction of the scalp, face, and neck defects was considered.
The patient underwent a four-step surgical protocol.
-
1
The first surgical step consisted in a partial excision of scalp lesions and contextual insertion of three 50 ml tissue expanders under the muscle layer of the frontal region and under the galea aponeurotica of the scalp. Vacuum drainages were positioned. Expanders were filled with normal saline (50 ml each one) at 1 week intervals. After 3 months, tissue expanders were removed and the lesion was partially excised at the same time. Two advancement flaps were mobilized for reconstruction.
-
2
The second surgical step was performed in May 2013, after 1 year from the first intervention, with insertion of two 100 ml rectangular tissue expanders under the scalp (Fig. 3). Fulfilled expanders were removed after 3 months, and the residual lesion was completely excised. Local flaps were used to cover the residual defect, and lifting of the right eyebrow was performed.
-
3
The third surgical procedure was performed 2 years later, in December 2015. Surgical debulking of occipitotemporal and retroauricular lesions was completed. Primary reconstruction with Integra® Dermal Regeneration Template was made. After 4 weeks, the outer silicone layer of Integra® was removed and a thin (1 mm) split-thickness skin graft from the internal thigh was used for definitive coverage.
-
4
The last step included the excision of further frontal and laterocervical lesions. Additionally, multiple tumors of the occipital region were removed.
Fig. 3.
Second surgical step. The patient was treated with two 100 ml rectangle tissue expanders on the scalp, which were completely expanded after 3 months.
All procedures were successful, and the patient underwent an uneventful course. After more than 6 years of follow-up, no recurrence was observed. The patient experienced a highly improved quality of life and reported an increase in overall self-confidence and social interaction capabilities (Fig. 4).
Fig. 4.
After 6 years of constant follow-up, the patient showed excellent aesthetic and functional results without any recurrence or complications observed.
3. Discussion
BSS is a rare autosomal dominant disease, with tumors arising from the adnexa of the skin. Although benign in most instances, the tumors are prone to arise in the craniofacial region, thereby causing to the patient a great deal of practical and aesthetic discomfort with local pain, hemorrhage, local infections, and, in some cases, even chronic anemia [17]. Furthermore, there is a potential risk of the cylindroma turning malignant and becoming cylindrocarcinoma, particularly in the case of multiple scalp cylindromas, thereby strengthening the indication for surgical treatment [10].
To date, different therapeutic approaches have been implemented. However, surgical excision remains the gold standard with the lowest rate of relapse compared to dermabrasion, electrodessication, cryotherapy, radiotherapy, argon, and CO2 lasers [18].
Scalp reconstruction after tumor excision may include any of the following techniques: secondary or primary closure, advancement, rotational or transpositional flaps, tissue expansion, locoregional or free flaps, and split-thickness or full-thickness skin graft [15,19]. The choice depends on the anatomic side, patient-related factors, and experience of the operator.
Owing to the well-vascularized nature of the cylindroma tumors, there is a high risk of perioperative and postoperative bleeding. We chose a safe integrated strategy with sequential reconstructive steps considering the combination of tissue expanders, dermal regeneration template, and split-thickness skin grafts and local flaps to reduce life-threatening conditions such as excessive bleeding, prolonged operating time, infection, or skin necrosis.
Reconstruction of the cephalic extremity in this particular case represented a challenge for the plastic surgeon. However, the use of different techniques allowed a synergistic action obtaining more favorable results than using a single technique, with overall reduction in complication rate.
Our protocol presents further advantages like the ability to preserve color consistency and hair-bearing areas, improved vascularization of the local tissue due to skin expansion, and the possibility of subsequent reconstruction. Some disadvantages included frequent sessions, strict follow-up, discomfort, and temporary deformity due to the refilling of expanders. Nevertheless, the surgical strategy chosen and the excellent aesthetic outcomes achieved in the absence of complications and life-threatening conditions resulted in a general improvement of patient self-esteem and quality of life.
4. Conclusions
ES is a dermal tumor of the sweat glands and its etiology is not fully understood. ES may present de novo or congenitally with different clinical presentations [20]. A prompt diagnosis and early treatment is very important owing to the potential malignant transformation, especially in the case of multiple or symptomatic lesions. Although extremely rare, malignant ES can be lethal if undiagnosed and left untreated. Treatment for ES is not well established; however, several studies [3,18] recommend surgical excision as the best therapeutic approach with low rates of recurrence.
This complex clinical case demonstrates that our integrated approach led to excellent results, as evidenced by photographic documentation, with benefit to patient quality of life and no recurrence. The correct preoperative planning and the various reconstructive techniques allowed us to achieve an excellent result in the absence of complications.
Funding
The Article has been published with the contribution of 5×1000 IRPEF funds in favor of the University of Foggia, in the memory of Gianluca Montel.
References
- 1.Kersting D.W., Helwig E.B. Eccrine spiradenoma. AMA Arch Derm. 1956;73(3):199–227. doi: 10.1001/archderm.1956.01550030001001. [DOI] [PubMed] [Google Scholar]
- 2.Englander L., Emer J.J., McClain D., Amin B., Turner R.B. A rare case of multiple segmental eccrine spiradenomas. J. Clin. Aesthet. Dermatol. 2011;4(April (4)):38–44. [PMC free article] [PubMed] [Google Scholar]
- 3.Dhua S., Sekhar D.R. A rare case of eccrine spiradenoma-treatment and management. Eur. J. Plast. Surg. 2016;39:143–146. doi: 10.1007/s00238-015-1103-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Zheng Y., Tian Q., Wang J., Dong X., Jing H., Wang X., Feng Y., Xiao S. Differential diagnosis of eccrine spiradenoma: a case report. Exp. Ther. Med. 2014;8(October (4)):1097–1101. doi: 10.3892/etm.2014.1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pinho A.C., Gouveia M.J., Gameiro A.R., Cardoso J.C., Gonçalo M.M. Brooke-spiegler syndrome – an underrecognized cause of multiple familial scalp tumors: report of a new germline mutation. J. Dermatol. Case Rep. 2015;9(September (3)):67–70. doi: 10.3315/jdcr.2015.1208. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lavorato F.G., Miller M.D., Obadia D.L., Nery N.S., Silva R.S. Syndrome in question. Brooke-spiegler syndrome. An Bras. Dermatol. 2014;89(January–February (1)):175–176. doi: 10.1590/abd1806-4841.20142194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Seyhan T., Borman H., Bal N. Malignant eccrine spiradenoma of the scalp. J. Craniofac. Surg. 2008;19(November (6)):1608–1612. doi: 10.1097/SCS.0b013e31818b4143. [DOI] [PubMed] [Google Scholar]
- 8.Ben Brahim E., Sfia M., Tangour M., Makhlouf R., Cribier B., Chatti S. Malignant eccrine spiradenoma: a new case report. J. Cutan. Pathol. 2010;37(April (4)):478–481. doi: 10.1111/j.1600-0560.2009.01320.x. [DOI] [PubMed] [Google Scholar]
- 9.Dabska M. Malignant transformation of eccrine spiradenoma. Pol. Med. J. 1972;11(2):388–396. [PubMed] [Google Scholar]
- 10.van der Horst M.P., Marusic Z., Hornick J.L., Luzar B., Brenn T. Morphologically low-grade spiradenocarcinoma: a clinicopathologic study of 19 cases with emphasis on outcome and MYB expression. Mod. Pathol. 2015;28(July (7)):944–953. doi: 10.1038/modpathol.2015.48. [DOI] [PubMed] [Google Scholar]
- 11.Lauret P., Boullie M.C., Thomine E., Stewart W.M. Giant eccrine spiradenoma. Ann. Dermatol. Venereol. 1977;104(June–July (6–7)):485–487. [PubMed] [Google Scholar]
- 12.Cotton D.W., Slater D.N., Rooney N. Giant vascular eccrine spiradenomas: a report of two cases with histology, immunohistology and electron microscopy. Histopathology. 1986;10:1093–1099. doi: 10.1111/j.1365-2559.1986.tb02546.x. [DOI] [PubMed] [Google Scholar]
- 13.Georgesen C., Magro C. Myoepithelial-rich and infiltrative giant vascular eccrine spiradenoma: a unique presentation of a rare adnexal tumor. Am. J. Dermatopathol. 2018;40(June (6)):428–432. doi: 10.1097/DAD.0000000000001007. [DOI] [PubMed] [Google Scholar]
- 14.Kim M.H., Cho E., Lee J.D., Cho S.H. Giant vascular eccrine spiradenoma. Ann. Dermatol. 2011;23(October (Suppl. 2)):S197–200. doi: 10.5021/ad.2011.23.S2.S197. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gentile P., Bottini D.J., Felici M., Garelli A., Nicoli F., Cervelli V. Loss of substance from the cranial vault: alternative technique in reconstructive surgery. J. Craniofac. Surg. 2008;19(March):558–559. doi: 10.1097/SCS.0b013e3181577b44. [DOI] [PubMed] [Google Scholar]
- 16.Agha R.A., Fowler A., Saetta A., Barai I., Rajmohan S., Orgill D.P., SCARE Group The SCARE statement: consensus-based surgical case report guidelines. Int. J. Surg. 2016;34(October):180–186. doi: 10.1016/j.ijsu.2016.08.014. [DOI] [PubMed] [Google Scholar]
- 17.Kim C., Kovich O.I., Dosik J. Brooke-Spiegler syndrome. Dermatol. Online J. 2007;13(1):10. [PubMed] [Google Scholar]
- 18.Rathi M., Awasthi S., Budania S.K., Ahmad F., Dutta S., Kumar A. Brooke-Spiegler syndrome: a rare entity. Case Rep. Pathol. 2014:231895. doi: 10.1155/2014/231895. 2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zhang Y.X., Xi W., Lazzeri D., Zhou X., Li Z., Nicoli F., Zenn M.R., Torresetti M., Grassetti L., Spinelli G. Bipaddle radial forearm flap for head and neck reconstruction. J. Craniofac. Surg. 2015;26:350–353. doi: 10.1097/SCS.0000000000001468. [DOI] [PubMed] [Google Scholar]
- 20.Englander L., Emer J.J., McClain D., Amin B., Turner R.B. A rare case of multiple segmental eccrine spiradenomas. J. Clin. Aesthet. Dermatol. 2011;4(April (4)):38–44. [PMC free article] [PubMed] [Google Scholar]