Abstract
Objectives
Appraising health as controllable is typically thought to be adaptive, but recent evidence suggests the paradoxical possibility that perceived control (PC) can be detrimental. We considered the premise that high PC should have a survival benefit when it is part of an adaptive mindset involving high value (importance) for health, but it might be detrimental when it is part of a mindset comprised of low health value (HV). In addition, we examined whether the survival consequences of PC and HV vary with advancing age.
Method
Interviews were conducted with a heterogeneous sample of community-dwelling adults (n = 341; 72–99 years) to assess appraisals of control and value in the domain of health. Mortality data were obtained over 12 years from a provincial health registry.
Results
Both age and HV moderated the PC effect on mortality. The predicted beneficial and detrimental PC effects emerged at younger ages: higher PC predicted longer survival times when health was highly valued but shorter survival times when health was less highly valued.
Discussion
These findings deepen the knowledge regarding the conditions under which PC is or is not adaptive, suggesting the consequences depend on age and the extent to which health is valued.
Keywords: Appraisals, Perceived control, Health value, Mortality, Survival, Motivation
Perceived control (PC) is a powerful psychological factor that has been linked to better health and longevity (e.g., Chipperfield et al., 2012; Chipperfield, Campbell, & Perry, 2004; Infurna, Gerstorf, & Zarit, 2011; Infurna & Okun, 2015). The beneficial role of PC for survival was demonstrated in an early study of older adults notable for its size (n > 4,000) and protracted 12-year follow-up period (Chipperfield, 1993). A survival benefit of PC has been replicated in epidemiological analyses of large databases in Australia, Germany, the United States, and Canada that have tracked participants for as few as several years to as long as 19 years (Andrews, Clark, & Luszcz, 2002; Fry & Debats, 2006; Infurna, Ram, & Gerstorf, 2013; Krause & Shaw, 2000; Menec, Chipperfield, & Perry, 1999).
The PC-survival relationship has been found using different well-established scales and various conceptualizations of PC (e.g., desire for control, locus of control, self-efficacy, mastery), underscoring the robustness of the linkage. Converging evidence also comes from studies examining attributions for illness, such as the belief that illness is due to an uncontrollable cause (old age). The likelihood of death was over two times greater for those who endorsed versus did not endorse the uncontrollable old age attribution, and a comparison of effect sizes suggested that believing illness was due to an uncontrollable cause (β = .24) was as important to survival as was health status (β = .21) or age (β = .25) itself (Stewart, Chipperfield, Perry, & Weiner, 2012). Additional converging evidence comes from functional magnetic resonance imaging (fMRI) studies showing that opportunities to exert control (choice) affected reward processes in the brain thought to be adaptive for survival (Leotti & Delgado, 2011).
Our study further examined the potential benefits of PC. Most past analyses of PC in the health domain have relied on a single variable (main effect) approach, although some show it is important to examine factors such as age that may moderate the PC effect (Menec & Chipperfield, 1997). Overall, however, there is a lack of consensus regarding the age-related consequences of PC. Some findings suggest that PC impacts health most for middle-aged adults (Infurna, Ram, & Gerstorf, 2013); others imply the health benefits are strongest for older adults (Infurna & Okun, 2015). Still, others show that age does not qualify the PC effect on late- life health (Infurna & Gerstorf, 2013; Infurna, Gerstorf, Ram, Schupp, & Wagner, 2011). Further complicating this issue is that the majority of studies included few old-old adults (>80 years) and the age ranges varied widely.
Thus, it is not clear if the impact of PC intensifies or subsides with age. It is plausible that the consequences of PC are compounded in late life as more and more barriers threaten the capacity to exert influence over outcomes. Alternatively, the role of psychological appraisals of control could wane in very advanced age as other factors like declining health or access to care become stronger determinants of health and survival. This underscores the need to examine a qualifying role of age on the effects of PC.
Value as a Moderator of the PC Effect
The effect of PC might also be qualified or moderated by other psychological factors. In particular, the value (importance) ascribed to an outcome could play a critical role as suggested by expectancy-value theory (EVT) that has been used to explain human motivation dating back to the 18th century (Bernoulli, 1738; Tolman, 1938). EVT argues that motivation is magnified when the expectation of obtaining an outcome is coupled with appraising the outcome as valuable. In contrast, such an expectation is thought to be irrelevant when one regards the outcome as trivial. Thus, in the absence of value, the expectation is presumably of little consequence.
A variant of EVT, control-value theory (Pekrun, 1992, 2006), is uniquely applicable to our study because it concretely defines expectancy as the anticipation of control (i.e., influence) over an outcome. The premise is that the benefits of expecting control are qualified by the extent to which one values the outcome. In other words, this theory predicts a PC × value interaction. Studies support the idea that the effects of PC depend on value in everyday life and in the social and achievement domains (e.g., Goetz, Frenzel, Stoeger, & Hall, 2010; Pekrun, Goetz, Daniels, Stupnisky, & Perry, 2010; Pekrun & Perry, 2014; Krause & Shaw, 2000).
Studies in the domain of health also support the PC × value interaction and the premise that appraising health as controllable is adaptive when one also ascribes high value (importance) to health. A mindset characterized by this combination of appraisals has been shown to predict health behaviors, including exercise, diet, smoking, and the seeking of information (Bennett, Moore, Norman, Murphy & Tudor-Smith, 1997; Norman, Bennett, Smith, & Murphy, 1998; Wallston, Maides, & Wallston, 1976). In each of these studies, PC appeared to be beneficial, but only when health was valued. This might imply that a complementary combination of high PC and high health value (HV) forms a mindset that is motivating and cultivates engagement.
A 5-year study of physician visits further suggests that a motivated mindset (high PC–high HV) fosters a strategic approach to seeking health care when it is needed (Chipperfield et al., 2016). Individuals with a motivated mindset proactively visited their physicians more frequently when they were in poor (vs good) health. However, a strategic approach was not evident if PC was high and HV was low. Individuals with this mindset failed to seek the counsel of a physician when in poor health. Such individuals also lacked fear that is presumably needed to motivate help-seeking (Mayne, 2001), and they denied risk that can undermine direct health behaviors like getting vaccinated (Brewer, Weinstein, Cuite, & Herrington 2004).
The findings in this study (Chipperfield et al., 2016) highlight the potentially maladaptive role of a mindset that is characterized by high PC and low HV. Such a mindset is epitomized by the fearless teenager who exaggerates personal control and ignores (devalues) health and safety, or the reckless alcoholic who believes he has the will power to simply stop drinking (high PC) and lacks a concern for health (low HV). This mindset could foster a mistaken sense of invincibility and a feeling of being impervious to harm. Such an invincible mindset could fuel procrastination and exacerbate self-neglect, mitigating against the receipt of timely diagnoses and treatments. If the invincible mindset that is characterized by strong perceptions of control becomes more entrenched and increasingly dysfunctional over time, the dire consequences in adulthood would exceed those found for the fearless teenager.
Although a detrimental role of PC is seemingly paradoxical, it is compatible with the harmful consequences that arise from related constructs like unrealistic optimism (Klein et al., 2010) or from unrealistic overestimates of future life satisfaction (Lang, Weiss, Gerstorf, & Wagner, 2013). High levels of PC also appeared detrimental for well-being in an empirical study that showed subjective well-being suffered when high PC did not match the expectation of positive outcomes (Lang & Heckhausen, 2001). Together, this provides a basis for further consideration of whether there are conditions under which PC becomes detrimental.
The Present Research: PC as a Predictor of Survival
The main objective of our study was to assess the relationship between PC and survival while considering the moderating role of HV and advancing age. Our analysis goes beyond existing studies that have examined behavioral outcomes in convenience samples of young adults (Bennett et al., 1997; Norman et al., 1998). We assessed appraisals during in-home interviews with older adults and acquired objective mortality data from a provincial database. Access to a sufficiently large number of decedents over a long follow-up period (12 years) allowed for a systematic analysis of the link between PC and survival.
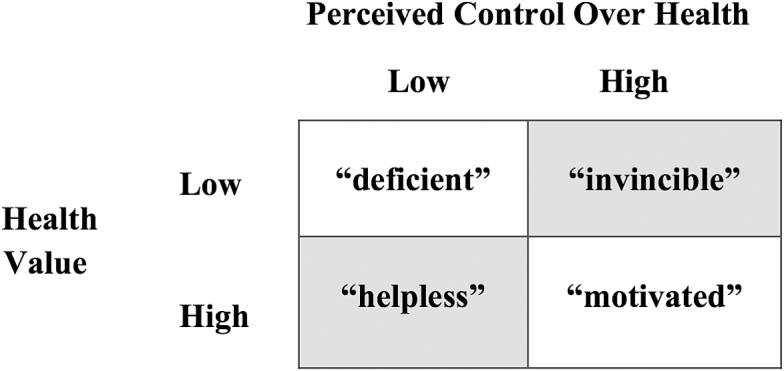
For our study, we adopted provisional labels as represented in the cells of a 2 × 2 mindset matrix (Figure 1). These labels are simply conceptual heuristics and are not intended to portray unchangeable personality types. The motivated label that identifies the most adaptive mindset involves a belief that health can be controlled when health is highly valued (high PC–high HV); the invincible label represents a mindset consisting of a belief that health can be controlled when health is also devalued (high PC–low HV); the deficient mindset refers to one consisting of a belief that health is uncontrollable and also that health is devalued (low PC–low HV); and the helpless mindset includes a belief that health is uncontrollable and also highly valued (low PC–high HV). In contrast to the adaptive role of a motivated mindset, the helpless mindset would typically be regarded as most maladaptive because hopelessness and despair likely follow from believing a highly valued outcome (e.g., health) is also uncontrollable. It is less clear what should follow from a deficient mindset since appraising health as uncontrollable while regarding it as unimportant would neither foster motivation nor hopelessness.
Figure 1.
2 × 2 appraisal group matrix distinguishing individuals varying on perceived control and health value. Adapted from “The Paradoxical Role of Perceived Control in Late Life Health Behavior,” by J. Chipperfield et al., 2016, PLoS ONE, 11, p. 4. Copyright 2016 by the authors. Adapted with permission.
The main PC × HV interaction hypothesis was that the PC effect on survival would depend on the level of HV. We hypothesized a beneficial PC effect when health was highly valued; this would be manifested by a lower risk of death for the motivated mindset (motivated < helpless). We also hypothesized a detrimental PC effect when health was not highly valued; this would be manifested by a higher risk of death for the invincible mindset (invincible > deficient). In addition, a 3-way interaction was assessed to consider whether the predicted effects would be stronger or weaker at more advanced ages. No hypothesis was stated because it is not clear whether these psychological appraisals would become stronger or weaker determinants of survival with advancing age.
Method
Database
The present analyses were conducted using the Aging in Manitoba (AIM) longitudinal database that consists of responses obtained from study participants during in-home interviews. Using a stratified random sampling procedure, the original participants were drawn from the Manitoba Health Registry that provided a comprehensive sampling frame including almost all residents of the province. The representativeness of the AIM has been supported by comparisons of the AIM sample to the overall provincial population (Chipperfield, Havens, & Doig, 1997).
In 1996, a subset of participants who had been interviewed in the AIM study (n = 1868) also completed interviews for a satellite study referred to as the Successful Aging Study (SAS). The SAS study (n = 353) that included approximately 20% of the overall 1996 AIM participants was limited to community-dwelling adults who resided in the three major cities. Also excluded from the SAS were those who were unable to be contacted or had barriers due to health (illness), cognition (comprehension), or language (inability to understand and/or speak English). Despite these exclusion criteria, the SAS sample was identical to the larger AIM sample on major demographics (e.g., gender, marital status). SAS participants, however, were significantly younger (Ms = 80 vs 82) and had higher SES (Ms = 16,057.00 vs 10,211.00), as would be expected by the exclusion of rural participants who had some barriers.
Participants
For our purposes, we examined AIM respondents who also participated in the SAS satellite study and who, for the first time in 1996, provided psychological appraisals of both PC and HV. To be retained for analyses, participants must have provided complete interview data (1996) for all relevant variables described below (demographics, physical health). This resulted in the exclusion of only 12 participants. When comparing the full SAS sample (n = 353) to the analysis sample that excluded these 12 individuals (n = 341), no differences emerged on age, gender, or SES. Thus, results based on our analysis sample should generalize to urban, community-living older adults who are free of major barriers to health, comprehension, and communication.
Demographic variables
Demographic measures included: age (M = 79.88, SD = 5.63), gender (1 = female, n = 213; 2 = male, n = 128), and SES, which combined information on education (number of completed years in school, M = 10.71, SD = 2.83) and income (Canadian dollars acquired from all sources including wages, pensions/allowances, dividend interest, etc., M = 1492.79, SD = 1088.49).
Physical Health
A physical health status index captured the severity of participants’ chronic conditions, going beyond a simple self-reported count of chronic conditions that is often used. The index was created by combining both subjective and objective information in a 3-step procedure. First, participants reported whether they had experienced 22 chronic health conditions (e.g., arthritis, cancer, diabetes, stroke- and heart-related problems) within the previous year (yes, no). Second, an objective estimate of severity was assigned to each reported condition by borrowing scores from the revised seriousness of illness rating (SIRS-R) scale (Rosenberg, Hayes, & Peterson, 1987; Wyler, Masuda, & Holmes, 1970) or by obtaining medical residents’ ratings of condition seriousness. Third, a mean severity score for each participant was obtained by calculating the average of the seriousness scores of each reported chronic health condition. Higher scores corresponded to more severe conditions, that is, poorer health status (M = 296.70, SD = 196.29).
Appraisals: PC and HV
A domain-specific approach was used to measure explicit appraisals of control and value. PC over health was assessed using participants’ appraisals of the extent to which they could personally influence their health (1 = almost no influence, 10 = total influence; M = 7.52, SD = 1.97). This single quantifiable estimate of influence over health offers a domain-specific measure that has high face validity and is comparable to past single-item approaches that assess PC in specific domains (e.g., Lachman & Weaver, 1998).
HV was assessed using an adapted scale (Lau, Hartman, & Ware, 1986), as described elsewhere (Chipperfield et al., 2016). Participants’ agreement with six statements was assessed (1 = strongly disagree, 7 = strongly agree): “There is nothing more important than good health;” “There are many things I care about more than my health;” “Good health is of only minor importance in a happy life;” “If you don’t have your health you don’t have anything;” “It is important to do things that will reduce the likelihood of bad health;” “It is important to do things that will increase the chances of good health.” Reverse coding was applied so that higher scores corresponded to greater HV.
The distributions for the HV items showed interindividual variability. For example, some participants (~30%) reported agreement that “There are many things I care about more than my health.” This counters an assumption that health is universally highly valued. Instead, this conforms to anecdotal accounts of individuals who value health less than other pursuits, such as the workaholic who undergoes chronic stress in order to gain money, success, and prestige, or the student who sacrifices sleep and nutrition in the search for knowledge or good grades.
A continuous HV index was created after transforming (square root transformation) the six items that had skewed distributions. This involved calculating a mean over the six items so that high scores reflected high HV (M = 1.72, SD = .50). Psychometric analyses supported scale reliability (alpha = .72). A principal component factor analysis revealed a single factor (eigen value = 2.53, explained variance = 42.1%; item factor loadings range = .61 to .69).
Mortality
Mortality data were obtained from searches of publicly accessible online databases and administrative health records from Manitoba Health’s provincial registry that contained population-based data of the highest quality. The survivor-to-decedent ratio over the right-censored 12-year follow-up period was 149:192 (56% deceased). The mortality data were merged with the interview data, allowing for an assessment of the role of psychological appraisals on mortality.
Results
A Cox proportional hazard regression analysis (Cox, 1972; Muthén & Muthén, 1998–2015) was conducted to examine the effects of PC on mortality (days from interview) and whether they were conditional on HV and age. The model included centered continuous predictors (PC, HV, age), interaction terms, and baseline covariates (gender, SES, and health) to control for potential confounding factors. The predictors and covariates were z standardized; thus, hazard ratios (HRs) represent effect sizes in standard deviation units.
Support was found for the hypothesized PC × HV interaction (Table 1). A significant HR (0.84) showed the effect of PC on risk of death depended on HV. However, this 2-way interaction was further qualified by a significant 3-way PC × HV × age interaction (HR = 1.18). Thus, both age and HV moderated the PC effect on mortality.
Table 1.
Hazard Ratios for Predictors of 12-Year Mortality
| Predictor variables | Hazard ratio | 95% CI |
|---|---|---|
| Age | 1.61** | 1.405, 1.856 |
| Female | 0.60** | 0.441, 0.819 |
| SES | 0.94 | 0.809, 1.094 |
| Poor physical health status | 1.26** | 1.098, 1.445 |
| Perceived control (PC) | 0.93 | 0.815, 1.068 |
| Health value (HV) | 0.96 | 0.827, 1.123 |
| PC × HV | 0.84** | 0.748, 0.954 |
| PC × Age | 0.91 | 0.812, 1.012 |
| HV × Age | 1.00 | 0.873, 1.144 |
| PC × HV × Age | 1.18** | 1.044, 1.327 |
| Log likelihood | −1,720 | |
| Akaike information criterion | 3,461 | |
| n (n event) | 341 (192) | |
Note: All predictors are z standardized with the exception of gender, which has been left in its original metric to facilitate interpretation (1 = male, 2 = female). CI = confidence interval; SES = socioeconomic status.
*p ≤ .05
**p ≤ .01.
Simple–simple slope analyses were conducted to probe the 3-way interaction, as recommended by Cohen, Cohen, West, and Aiken (2003). Specifically, the conditional effects of PC on mortality were tested at low (−1 SD) and high (+1 SD) HV and at younger (−1 SD) and older (+1 SD) ages. This permitted a test of the hypothesized beneficial and detrimental PC effects that are represented in Table 2.
Table 2.
Predictors of Mortality for Young-Old and Old-Old Adults: Conditional Effects of Perceived Control and Health Value
| Effects of predictor variables | Hazard ratio | 95% CI |
|---|---|---|
| Young-old adults | ||
| PC effect | ||
| Low HV (invincible vs deficient) | 1.43* | 1.028, 2.002 |
| High HV (motivated vs helpless) | 0.74** | 0.600, 0.909 |
| HV effect | ||
| Low PC (helpless vs deficient) | 1.34* | 1.022, 1.769 |
| High PC (motivated vs invincible) | 0.69** | 0.517, 0.927 |
| Old-old adults | ||
| PC effect | ||
| Low HV (invincible vs deficient) | 0.85 | 0.685, 1.058 |
| High HV (motivated vs helpless) | 0.84 | 0.696, 1.017 |
| HV effect | ||
| Low PC (helpless vs deficient) | 0.97 | 0.749, 1.252 |
| High PC (motivated vs invincible) | 0.96 | 0.759, 1.210 |
Note: All predictors are z standardized. Conditional effects of PC (and HV) tested with simple–simple slopes are presented at low (−1 SD) and high (+1 SD) levels of HV (and PC) and age (young-old = −1 SD; old-old = +1 SD).
*p ≤ .05
**p ≤ .01.
The HRs were significant for the young-old but not the old-old adults (see Table 2). Specifically, a beneficial effect of PC at high HV (motivated vs helpless mindset) was supported by a HR of 0.74 that indicated each standard deviation increase in PC corresponded to a 26% reduction in risk of death. A detrimental effect of PC at low HV (invincible vs deficient mindset) was also supported by a HR of 1.43 that indicated each standard deviation increase in PC corresponded to a 43% increase in risk of death.
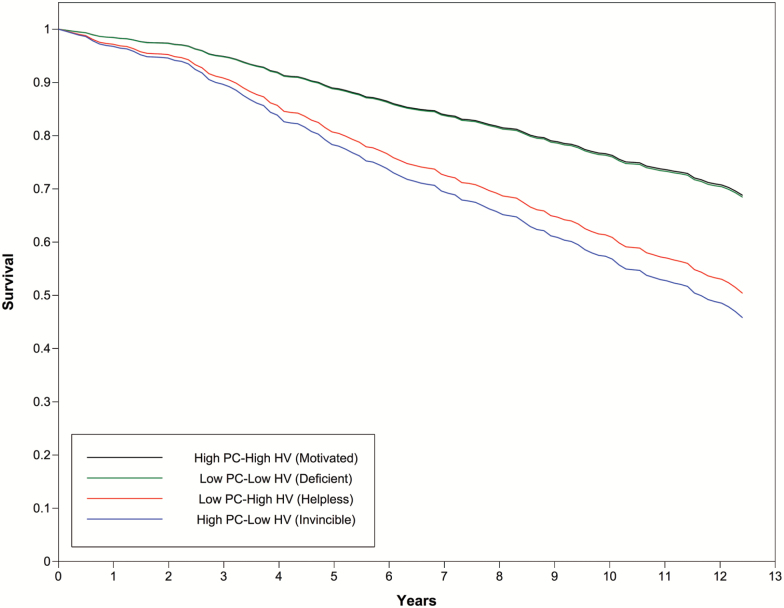
Figure 2 displays these beneficial and detrimental effects of PC for the young old by presenting four survival curves for the motivated (high PC–high HV), invincible (high PC–low HV), deficient (low PC–low HV), and helpless (low PC–high HV) mindsets. The curves reflect the simple–simple slopes associated with the conditional effect tests of (continuous) PC on mortality.
Figure 2.
Survival curves for young old adults who varied in perceived control (PC; low, high) and health value (HV; low, high). The Cox regression model controlled for age, gender, SES, and physical health status.
The beneficial effect of PC at high HV is depicted in Figure 2 by a comparison of the motivated (high PC) to the helpless (low PC) mindsets (Figure 2). A benefit of PC is implied by the significantly longer survival time for the motivated mindset. The detrimental effect of PC at low HV is implied by the significantly shorter survival time for the invincible (high PC) compared to the deficient (low PC) mindset. The striking increase in the divergence of the invincible mindset survival curve in relation to all other survival curves underscores the escalating risk of death for those with an invincible mindset.
Finally, Table 2 summarizes the HV effects. By probing the interaction at low levels of PC (−1 SD), the two low PC mindsets that varied in HV were contrasted. The significant conditional effect (HR =1.34) suggests the helpless (high HV) is more maladaptive than the deficient (low HV) mindset, conforming to our logic that the helpless mindset would be most detrimental. By probing the interaction at high levels of PC (+1 SD), the two high PC mindsets that varied in HV were contrasted. The significant conditional effect (HR = 0.69) shows the risk of death was lower for the motivated (high HV) versus the invincible (low HV) mindset. Thus, despite the invincible mindset being comprised of high PC, it was associated with a 31% increased risk of death over the motivated mindset.
Supplemental Analyses
Notably, the beneficial and detrimental effects of PC (shown in Figure 2) also emerged in a supplemental analysis that used a more traditional subgroups approach to contrast participants characterized by low (below median) or high (above median) PC and HV and younger (below median) and older (above median) ages. [This supplemental Cox regression analysis which probed the PC x HV x age interaction by categorizing participants into subgroups is not recommended because it reduces power, attenuates relationships, and can produce spurious effects (see Cohen et al., 2003; Hayes, 2013; Maxwell & Delaney, 1993; MacCallum, Zhang, Preacher, & Rucker, 2002). Nonetheless, the findings to emerge using this more traditional approach were consistent with those that emerged in the continuous simple–simple effect Cox regressions. Significant HRs were observed only for the young-old adults, and support was again found for the beneficial and detrimental effects of PC on mortality among the young-old. A HR of 0.48 (p = .029) showed that those with a motivated mindset (high PC–high HV, n = 60) had a 52% lower risk of death than their peers with a helpless mindset (low PC–high HV, n = 30). A HR of 2.22 (p = .023) indicated that risk of death for those with an invincible mindset (low PC–high HV, n = 53) was more than twice that observed for the deficient mindset (low PC–low HV, n = 39).]
Discussion
Survival of the species is predicated on cause–effect associations; an animal will survive only if it imposes an influence over its environment that enables it to catch its prey. Our findings suggest that, in humans, survival could go beyond whether one can objectively control (influence) an outcome. Survival might hinge upon one’s subjective appraisal of control. In our study, even after statistically accounting for other well-established predictors of mortality (e.g., gender, SES, health status), a survival effect of PC emerged, although it was qualified by age and by the value (importance) ascribed to health.
The Beneficial Versus Detrimental Role of PC for the Young Old
The hypothesized beneficial survival effect of PC was confirmed, although only for the young old who highly valued their health. Control beliefs not only seem to enable such people to flourish, cultivating a healthy mind and body (Chipperfield, Hamm, Perry, & Ruthig, forthcoming), they appear to increase the chances of a long life. This extends the conclusion that people with a strong sense of personal control benefit by being “happy, healthy, wealthy, and wise” (Lachman, 2006). They also stay alive longer.
The beneficial effect of PC (lower mortality) when HV was high is in stark contrast to the detrimental effect of PC (higher mortality) that emerged when HV was low. These results extend past findings that showed control appraisals had no benefits when health was devalued (Bennett et al., 1997; Norman et al., 1998; Wallston et al., 1976). They also extend the premise in control-value theory that PC is inconsequential when an outcome is viewed as trivial (Pekrun, 1992, 2006). Instead, our findings suggest that PC becomes toxic when paired with a devaluing of health. Overall, this invincible mindset was associated with the shortest survival time (Figure 2). Whereas the probability of survival at the end of the 12-year follow-up was only 47% for the invincibles, it was 70% for the motivated mindset. A paradoxical and detrimental role of this invincible mindset is also consistent with findings that emerged in our prior study showing that the invincibles were fearless, they denied risks, and they failed to be strategic in seeking care (Chipperfield et al., 2016).
Future Directions for Research
Future research is needed to replicate the beneficial and detrimental PC effects and to understand why such effects may not extend into very advanced age. The absence of a correlation between age and either appraisal of PC and HV in our study implies these appraisals remain just as strong in very late life. However, a longitudinal design and a larger age range are required to adequately document age-related changes in appraisals and in their consequences. A systematic analysis of the age trajectories would help to determine whether an invincible mindset becomes more dysfunctional as it is repeatedly endorsed over adulthood or whether it loses its detrimental effect in very late life, which would underscore the possibility of a curvilinear relationship.
Regardless of whether appraisals change with age, it is also plausible that their function differs earlier and later in life. At younger ages, low HV could reflect a demotivation and disinterest in health, whereas, in later life it might reflect a self-protective process. That is, minimizing the importance of health (low HV) might soften the blow of a downward spiral of health.
If the low HV that characterizes the invincible mindset reflected a self-protective reaction to being in poor health, this would be relevant to the interpretation of the invincibles’ elevated risk of death. It would suggest that their higher risk of death was not due to their invincible mindset, but rather to their poor health. However, our inclusion of a statistical control for health helped to rule out health as an alternative interpretation. Nonetheless, this does not negate the possibility that low HV reflects a self-protective mechanism, showing the need for further study of what it means to devalue health.
Also unresolved is the possibility that health mediates the linkage between mindsets and mortality, which suggests that health should be scrutinized as a mediator to explain why mindsets predict death. The possibility that the invincible mindset fosters poor health would be consistent with the findings from our earlier study that showed this mindset was associated with emotions (lack of fear) and cognitions (denial of risk) that could suppress actions to seek treatment (Chipperfield et al., 2016). An absence of fear and a denial of future risks could foster procrastination and self-neglect, undermining help seeking, and ultimately leading to compromised health. This underscores the complexity of an intricate chain of cognitive, emotional, and behavioral mediators that could undermine physical health, which in turn might explain the higher risk of death for individuals with an invincible mindset.
To the extent that such maladaptive mindsets can be identified, future research should seek remedial methods to counter them. Formal interventions could be designed to simultaneously promote control-enhancing messages, as done by prior researchers (Langer & Rodin, 1976; Perry, Stupnisky, Hall, Chipperfield, & Weiner, 2010), and to encourage an appreciation of good health. Encouraging people to appreciate good health could go beyond a focus on its intrinsic value. The extrinsic value of retaining good health could also be emphasized by underscoring its role in fostering independence and quality of life and in protecting from devastating repercussions of declining health that can include financial and personal stress and becoming a burden for loved ones or for the formal systems of care.
If remedial treatments are found to be successful, this would underscore the need for education and training of clinicians and geriatricians to promote awareness regarding the importance of psychological appraisals of health. Simple tools could also be designed for caregivers, nurse practitioners, and physicians to help encourage their clients and patients to appraise heath in adaptive ways. Creative approaches would be needed for the implementation and application of such tools and intervention programs.
Strengths and Limitations
The many strengths of our study include access to the AIM database that was developed using rigorous sampling procedures and intensive tracking strategies. This resulted in outstanding retention, high response rates, and representative samples of very old adults who were tracked over a lengthy follow-up period to obtain objective and reliable mortality data. These design and measurement features allowed us to avoid interpretation problems that plague studies based on select (or convenience) samples, short follow-ups, and insufficient numbers of decedents.
Our analysis of mortality data permitted an extension of past studies that focused on appraisals of control and value as predictors of behavioral outcomes such as information seeking or physician visits (e.g., Chipperfield et al., 2016; Wallston et al., 1976). We extended those findings by showing that these appraisals also predict whether one lives or dies. Notably, our approach to examining these appraisals addressed a general criticism of past researchers who have underestimated, overlooked, and forgotten to explicitly test the very interaction implied by EVT (Nagengast et al., 2011). In contrast to past analyses of PC and value that have not directly tested the interaction (Krause & Shaw, 2000), more definitive conclusions can be drawn from analyses such as ours that explicitly examine a PC × HV interaction.
Despite the strengths of our study, there are possible limitations. First, our analysis could have failed to include potentially important covariates such as subjective well-being that overlap with appraisals of PC or HV. However, the 3-way interaction that emerged in our survival analysis remained significant in supplemental analyses that included covariates for loneliness (p = .008), life satisfaction (p = .007), and perceived stress (p = .013). This helps to rule out the alternative explanation that the beneficial effect of PC was due to higher subjective well-being that accompanied high PC.
Second, our PC measure could be challenged with regard to the questionable validity of single-item measures. However, this criticism is disputed by compelling evidence from prior research showing that a simple appraisal of health was an even more powerful predictor of mortality than an objective health measure (Mossey & Shapiro, 1982). Nonetheless, to provide assurance that our PC measure produced a reliable effect, we conducted a supplemental Cox regression analysis that replaced the single-item PC measure with a composite measure of PC that was based on three domains (health, pain, fitness). The PC × HV × age interaction (HR = 1.14, p = .024) was replicated, providing further confidence in the reliability of our effect.
Conclusions and Implications
Our findings suggest that PC has consequences for survival, at least up until very late in life. The survival benefit that emerged when individuals valued their health is consistent with past scientific studies (e.g., Chipperfield, 1993; Infurna, Gerstorf, & Zarit, 2011; Infurna & Okun, 2015). Paradoxically, however, when health was devalued, PC was associated with a higher risk of death, suggesting it is maladaptive to simultaneously hold this seemingly dissonant set of appraisals.
Our findings underscore the need for a greater emphasis on the study of complex mindsets comprised of multiple appraisals instead of viewing PC as a single entity. By examining simultaneous appraisals of PC and HV, both adaptive (e.g., motivated) and maladaptive (e.g., invincible) mindsets can be identified and their consequences can be better understood. Just as we suggest it is detrimental to hold a dissonant set of beliefs (high PC and low HV), it might be damaging to endorse a conflicting combination of strategies. Our examination of control strategies from the perspective of the motivational theory of life-span development (Heckhausen, Wrosch, & Schulz, 2010) identified a potentially harmful conflicted engagement mindset that included high levels of strategies that promote psychological commitment to a goal (selective secondary control) and low levels of proactive goal striving (selective primary control) strategies (Hamm, Chipperfield, Perry, Heckhausen, & Mackenzie, 2014). This conflicted engagement predicted poorer cardiorespiratory health as assessed by lower blood oxygen saturation, highlighting the knowledge that can be gained by studying the consequences of complex mindsets.
In conclusion, our findings deepen the knowledge regarding the conditions under which PC is or is not adaptive. The survival benefit of PC that emerged in our study should not be overshadowed by the paradoxical finding that suggests PC is maladaptive when health is devalued. Rather, our message is that it is equally important to cultivate a motivated mindset and to discourage an invincible mindset. Discouraging this mindset could have broad implications if a mistaken invincibility fosters self-neglect and disengagement that compromise health and independence and erode physical and functional well-being. Moreover, if an invincible mindset exacerbates the needs for informal and formal care systems, the implications would go beyond the individual to the societal level. Thus, undoing this maladaptive mindset has the potential to not only enhance quality and quantity of life for individuals but to benefit society by easing caregiver burden and offsetting costs and mounting pressures facing the health care system.
Funding
This work was supported by a Canadian Institutes of Health Research (MOP-130382; to J. G. C., R. P. P., R. P.), a Konrad Adenauer Award from the Royal Society of Canada and the Alexander von Humboldt Foundation (to R. P. P.); a Research Chair grant from the University of Munich (Grant VII.1-H172.10) and a John G. Diefenbaker Award from the Canadian Council of Arts and the Alexander von Humboldt Foundation (to R. P.); and a Social Sciences and Humanities Research Council of Canada Post-Doctoral Fellowship (to J. M. H.).
Acknowledgments
We would like to thank Loring Chuchmach for assistance with data analyses and Dr. Depeng Jiang (Director of the Biostatistical Consulting Unit in Community Health Sciences, University of Manitoba) for his statistical advice. We would like to acknowledge our appreciation for access to the Aging in Manitoba Database that was established by the late Dr. Betty Havens and for access to the provincial health registry (Manitoba Health) through the Manitoba Centre for Health Policy for access to data from. The results and conclusions presented in this manuscript are those of the authors. No official endorsement by Manitoba Health is intended or should be inferred.
References
- Andrews G. Clark M., & Luszcz M (2002). Successful aging in the Australian Longitudinal Study of Aging: Applying the MacArthur model cross-nationally. Journal of Social Issues, 58, 749–765. doi:10.1111/1540–4560.00288 [Google Scholar]
- Bennett P. Moore L. Norman P. Murphy S., & Tudor-Smith C (1997). Health locus of control and value for health in smokers and nonsmokers. Health Psychology, 16, 179–182. doi:10.1037/0278-6133.16.2.179 [DOI] [PubMed] [Google Scholar]
- Bernoulli D. (1738). Specimen theoriae novae de mensura sortis. Commentarii Academiae Scientiarium Imperialis Petropoliotanae, 5, 175–192. [Google Scholar]
- Brewer N. T. Weinstein N. D. Cuite C. L., & Herrington J. E. Jr (2004). Risk perceptions and their relation to risk behavior. Annals of Behavioral Medicine, 27, 125–130. doi:10.1207/s15324796abm2702_7 [DOI] [PubMed] [Google Scholar]
- Chipperfield J. G. (1993). Perceived barriers in coping with health problems: A twelve-year longitudinal study of survival among elderly individuals. Journal of Aging and Health, 5, 123–139. doi:10.1177/089826439300500106 [Google Scholar]
- Chipperfield J. G. Campbell D. W., & Perry R. P (2004). Stability in perceived control: implications for health among very old community-dwelling adults. Journal of Aging and Health, 16, 116–147. doi:10.1177/0898264303260447 [DOI] [PubMed] [Google Scholar]
- Chipperfield J. G. Hamm J. M. Perry R. P., & Ruthig J. C.(forthcoming). Perspectives on studying perceived control in the 21st century. In M. D., Robinson, M., Eid (Eds.), The happy mind: Cognitive contributions to well-being. New York, NY: Springer. [Google Scholar]
- Chipperfield J. G. Havens B., & Doig W. D (1997). Method and description of the aging in Manitoba project: A 20-year longitudinal study. Canadian Journal on Aging, 16, 606–625. doi:10.1017/S0714980800010990 [Google Scholar]
- Chipperfield J. G. Newall N. E. Perry R. P. Stewart T. L. Bailis D. S., & Ruthig J. C (2012). Sense of control in late life: Health and survival implications. Personality & Social Psychology Bulletin, 38, 1081–1092. doi:10.1177/0146167212444758 [DOI] [PubMed] [Google Scholar]
- Chipperfield J. G. Perry R. P. Pekrun R. H. Barchfeld P. Lang F. R., & Hamm J. M (2016). Paradoxical effects of perceived control on health behavior. PLoS ONE, 11, 1–16. doi:10.1371/journal.pone.0148921 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cohen J. Cohen P. West S. G., & Aiken L. S (2003). Applied multiple regression/correlation analysis for the behavioral sciences (3rd ed). London, UK: Lawrence Erlbaum Associates. [Google Scholar]
- Cox D. R. (1972). Regression models and life tables. Journal of the Royal Statistical Society Series B (Methodological), 34, 187–220. [Google Scholar]
- Fry P. S., Debats D. L. (2006). Sources of life strengths as predictors of late-life mortality and survivorship. International Journal of Aging and Human Development, 62, 303–334. doi:10.2190/3VAT-D77G-VCNQ-6T61 [DOI] [PubMed] [Google Scholar]
- Goetz T. Frenzel A. C. Stoeger H., & Hall N. C (2010). Antecedents of everyday positive emotion: An experience sampling analysis. Motivation and Emotion, 34, 49–62. doi:10.1007/s11031-009-9152-2 [Google Scholar]
- Hamm J. M. Chipperfield J. G. Perry R. P. Heckhausen J., & Mackenzie C. S (2014). Conflicted goal engagement: undermining physical activity and health in late life. The Journals of Gerontology. Series B, Psychological Sciences and Social Sciences, 69, 533–542. doi:10.1093/geronb/gbu048 [DOI] [PubMed] [Google Scholar]
- Hayes A. F. (2013). Introduction to mediation, moderation, and conditional process analysis: A regression-based approach. New York, NY: The Guilford Press. [Google Scholar]
- Heckhausen J. Wrosch C., & Schulz R (2010). A motivational theory of life-span development. Psychological Review, 117, 32–60. doi:10.1037/a0017668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infurna F. J., & Gerstorf D (2013). Linking perceived control, physical activity, and biological health to memory change. Psychology and Aging, 28, 1147–1163. doi:10.1037/a0033327 [DOI] [PubMed] [Google Scholar]
- Infurna F. J. Gerstorf D., & Zarit S. H (2011). Examining dynamic links between perceived control and health: Longitudinal evidence for differential effects in midlife and old age. Developmental Psychology, 47, 9–18. doi:10.1037/a0021022 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infurna F. J. Gerstorf D. Ram N. Schupp J., & Wagner G. G (2011). Long-term antecedents and outcomes of perceived control. Psychology and Aging, 26, 559–575. doi:10.1037/a0022890 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Infurna F. J., & Okun M. A (2015). Antecedents and outcomes of level and rates of change in perceived control: The moderating role of age. Developmental Psychology, 51, 1420–1437. doi:10.1037/a0039530 [DOI] [PubMed] [Google Scholar]
- Infurna F. J. Ram N., & Gerstorf D (2013). Level and change in perceived control predict 19-year mortality: Findings from the Americans’ changing lives study. Developmental Psychology, 49, 1833–1847. doi:10.1037/a0031041 [DOI] [PubMed] [Google Scholar]
- Klein W. M. Lipkus I. M. Scholl S. M. McQueen A. Cerully J. L., & Harris P. R (2010). Self-affirmation moderates effects of unrealistic optimism and pessimism on reactions to tailored risk feedback. Psychology & Health, 25, 1195–1208. doi:10.1080/08870440903261970 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Krause N., Shaw B. A. (2000). Role-specific feelings of control and mortality. Psychology and Aging, 15, 617–626. doi:10.1037/0882-7974.15.4.617 [DOI] [PubMed] [Google Scholar]
- Lachman M. E., & Weaver S. L (1998). Sociodemographic variations in the sense of control by domain: Findings from the MacArthur Studies of Midlife. Psychology and Aging, 13, 553–562. doi:10.1037/0882-7974.13.4.553 [DOI] [PubMed] [Google Scholar]
- Lachman M. E. (2006). Perceived control over aging-related declines: Adaptive beliefs and behaviors. Current Directions in Psychological Science, 15, 282–286. doi:10.1111/j.1467-8721.2006.00453.x [Google Scholar]
- Lang F. R., & Heckhausen J (2001). Perceived control over development and subjective well-being: Differential benefits across adulthood. Journal of Personality and Social Psychology, 81(3), 509–523. doi:10.1037/0022-3514.81.3.509 [DOI] [PubMed] [Google Scholar]
- Lang F. R. Weiss D. Gerstorf D., & Wagner G. G (2013). Forecasting life satisfaction across adulthood: Benefits of seeing a dark future?Psychology and Aging, 28(1), 249–261. doi:10.1037/a0030797 [DOI] [PubMed] [Google Scholar]
- Langer E. J., & Rodin J (1976). The effects of choice and enhanced personal responsibility for the aged: A field experiment in an institutional setting. Journal of Personality and Social Psychology, 34, 191–198. doi:10.1037/0022-3514.34.2.191 [DOI] [PubMed] [Google Scholar]
- Lau R. R. Hartman K. A., & Ware J. E (1986). Health as a value: Methodological and theoretical considerations. Health Psychology, 5, 25–43. doi:10.1037/0278-6133.5.1.25 [DOI] [PubMed] [Google Scholar]
- Leotti L. A., & Delgado M. R (2011). The inherent reward of choice. Psychological Science, 22, 1310–1318. doi:10.1177/0956797611417005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- MacCallum R. C. Zhang S. Preacher K. J., & Rucker D. D (2002). On the practice of dichotomization of quantitative variables. Psychological Methods, 7, 19–40. doi:10.1037//1082-989X.7.1.19 [DOI] [PubMed] [Google Scholar]
- Maxwell S. E., & Delaney H. D (1993). Bivariate median splits and spurious statistical significance. Psychological Bulletin, 113, 181–190. doi:10.1037/0033-2909.113.1.181 [Google Scholar]
- Mayne T. J. (2001). Emotions and health. In T. J. Mayne and G. A. Bonanno (Eds.), Emotions: Current issues and future directions (pp. 361–397). New York, NY: Guildford Press. [Google Scholar]
- Menec V. H., & Chipperfield J. G (1997). The interactive effects of perceived control and functional status on health and mortality among the young-old and the old-old. Journals of Gerontology, Series B: Psychological Sciences, 52, 118–126. doi:10.1093/geronb/52B.3.P118 [DOI] [PubMed] [Google Scholar]
- Menec V. H. Chipperfield J. G., & Perry R. P (1999). Self-perceptions of health: A prospective analysis of mortality, control, and health. Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 54, 85–93. doi:10.1093/geronb/54B.2.P85 [DOI] [PubMed] [Google Scholar]
- Mossey J. M., Shapiro E. (1982). Self-rated health: A predictor of mortality among the elderly. American Journal of Public Health, 72, 800–808. doi:10.2105/AJPH.72.8.800 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Muthén L. K., & Muthén B. O (1998–2015). Mplus user’s guide (7th ed). LA: Muthén & Muthén. [Google Scholar]
- Nagengast B. Marsh H. W. Scalas L. F. Xu M. K. Hau K. T., & Trautwein U (2011). Who took the “x” out of expectancy-value theory? A psychological mystery, a substantive-methodological synergy, and a cross-national generalization. Psychological Science, 22, 1058–1066. doi:10.1177/0956797611415540 [DOI] [PubMed] [Google Scholar]
- Norman P. Bennett P. Smith C., & Murphy S (1998). Health locus of control and health behaviour. Journal of Health Psychology, 3, 171–180. doi:10.1177/135910539800300202 [DOI] [PubMed] [Google Scholar]
- Pekrun R. (1992). Expectancy-value theory of anxiety: Overview and implications. In D.G. Forgays T. Sosnowski, & K. Wrzesniewski (Eds.), Anxiety: Recent developments in self-appraisal, psychophysiological and health research (pp. 23–41). Washington, DC: Hemisphere. [Google Scholar]
- Pekrun R. (2006). The control-value theory of achievement emotions: Assumptions, corollaries, and implications for educational research and practice. Educational Psychology Review, 18, 315–341. doi:10.1007/s10648-006-9029-9 [Google Scholar]
- Pekrun R. Goetz T. Daniels L. M. Stupnisky R. H., & Perry R. P (2010). Boredom in achievement settings: Control-value antecedents and performance outcomes of a neglected emotion. Journal of Educational Psychology, 102, 531–549. doi:10.1037/a0019243 [Google Scholar]
- Pekrun R., & Perry R. P (2014). Control-value theory of achievement emotions. In R., Pekrun, L., Linnenbrink-Garcia (Eds.), International handbook of emotions in education (pp. 120–141). New York, NY: Taylor & Francis. [Google Scholar]
- Perry R. P. Stupnisky R. H. Hall N. C. Chipperfield J. G., & Weiner B (2010). Bad starts and better finishes: Attributional retraining and initial performance in competitive achievement settings. Journal of Social and Clinical Psychology, 29, 668–700. doi:10.1521/jscp.2010.29.6.668 [Google Scholar]
- Rosenberg S. J. Hayes J. R., & Peterson R. A (1987). Revising the seriousness of illness rating scale: Modernization and re-standardization. International Journal of Psychiatry in Medicine, 17, 85–92. doi:10.2190/JWMW-8Q1U-71DJ-AN6E [DOI] [PubMed] [Google Scholar]
- Stewart T. L. Chipperfield J. G. Perry R. P., & Weiner B (2012). Attributing illness to ‘old age:’ consequences of a self-directed stereotype for health and mortality. Psychology & Health, 27, 881–897. doi:10.1080/08870446.2011.630735 [DOI] [PubMed] [Google Scholar]
- Tolman E. C. (1938). The determiners of behavior at a choice point. Psychological Review, 45, 1–35. doi:10.1037/h0062733 [Google Scholar]
- Wallston K. A. Maides S. A., & Wallston B. S (1976). Health-related information seeking as a function of health-related locus of control and health value. Journal of Research in Personality, 10, 215–222. doi:10.1016/0092-6566(76)90074-X [Google Scholar]
- Wyler A. R. Masuda M., & Holmes T. H (1970). Seriousness of illness rating scale: Reproducibility. Journal of Psychosomatic Research, 14, 59–64. doi:10.1016/0022-3999(70)90070 [DOI] [PubMed] [Google Scholar]