Zaire ebolavirus (EBOV) is the causative agent of the highly lethal Ebola virus disease and poses a significant threat to the global health community. Approved antivirals against EBOV are lacking; however, promising therapies targeting the EBOV glycoprotein are being developed. Efficacy testing of these candidate therapeutics relies on EBOV laboratory stocks, which when grown in tissue culture may acquire mutations in the glycoprotein. These mutations can produce inaccurate results in therapeutic testing. Until recently, distinguishing between tissue culture mutations and naturally occurring polymorphisms in EBOV GP was difficult in the absence of consensus clinical GP sequences. Here, we utilize recombinant VSV (rVSV) pseudotyped with the consensus clinical EBOV Makona GP to identify several mutations that have emerged or have potential to emerge in EBOV GP during tissue culture passage. Identifying these mutations informs the EBOV research community as to which mutations may arise during preparation of laboratory virus stocks.
KEYWORDS: Ebola virus, glycoprotein mutation, tissue culture adaptation, virus entry, cathepsin B, fusion loop mutations, heptad repeat mutations
ABSTRACT
The Zaire ebolavirus (EBOV) glycoprotein (GP) is cleaved into two subunits (GP1 and GP2) that are both required for virus attachment and entry into cells. Sequence changes in the GP have been proposed to increase pathogenesis and to alter virus growth properties. Mutations in GP acquired during EBOV tissue culture passage have also been reported to change virus growth properties. Here, we report the isolation of six amino acid mutations in EBOV GP that spontaneously appeared during recovery and passage of an EBOV-Makona GP-pseudotyped vesicular stomatitis virus (VSV), two of which also occur during passage of EBOV clinical isolates in tissue culture. Each of the six mutations resulted in increased virus growth in monkey and human cell lines. All mutations are located in the GP2 fusion subunit and increase entry kinetics of EBOV virus-like particles (VLPs). The gain-of-entry function mapped to two mechanistic phenotypes. Mutations in heptad repeat 1 (HR1) decreased the requirement for cathepsin B activity for viral infection. Mutations directly within the fusion loop increased entry kinetics without altering the cathepsin B dependence. Several mutations in the fusion loop were substitutions of residues present in other ebolavirus glycoproteins, illustrating the evolutionary paths for maintaining an optimally functioning fusion loop under selection pressure.
IMPORTANCE Zaire ebolavirus (EBOV) is the causative agent of the highly lethal Ebola virus disease and poses a significant threat to the global health community. Approved antivirals against EBOV are lacking; however, promising therapies targeting the EBOV glycoprotein are being developed. Efficacy testing of these candidate therapeutics relies on EBOV laboratory stocks, which when grown in tissue culture may acquire mutations in the glycoprotein. These mutations can produce inaccurate results in therapeutic testing. Until recently, distinguishing between tissue culture mutations and naturally occurring polymorphisms in EBOV GP was difficult in the absence of consensus clinical GP sequences. Here, we utilize recombinant VSV (rVSV) pseudotyped with the consensus clinical EBOV Makona GP to identify several mutations that have emerged or have potential to emerge in EBOV GP during tissue culture passage. Identifying these mutations informs the EBOV research community as to which mutations may arise during preparation of laboratory virus stocks.
INTRODUCTION
Ebolaviruses (family Filoviridae) cause a severe and deadly disease often associated with hemorrhagic fever. The species Zaire ebolavirus (EBOV) is responsible for several outbreaks on the African continent, with mortality rates that have reached 90% (1). To date, vaccines and therapeutics against EBOV are still in the development and testing stage. Many of the therapeutics under development target the virally encoded glycoprotein (GP) (2, 3, 4).
GP primarily functions to mediate virus entry into the cell. It is a 67-kDa multidomain protein comprised of two subunits (GP1 and GP2) linked by a disulfide bond (5, 6). The large subunit, GP1, contains the receptor binding region, and the smaller subunit, GP2, anchors the protein into the viral membrane and induces fusion between the viral and cellular membranes (7).
Virus entry into the cell begins with GP-mediated attachment to a cell surface receptor on the plasma membrane. The virus is then internalized by macropinocytosis (8, 9) and trafficked to the acidified late endosomes (LE) where host cysteine proteases cleave GP1, removing two glycosylated domains and exposing a region that binds to the EBOV entry receptor Neimann-Pick C1 (NPC1) (7, 10, 11, 12). Cleavage also primes GP for fusion by removal of a GP1 fragment that is believed to restrict the movement of the GP2 fusion loop (FL) and first heptad repeat (HR1) in their prefusion conformation (13, 14). Cleavage of GP during entry is proposed to occur through the concerted action of cysteine proteases (15). The dominant model suggests that cathepsins L and B (Cat-L and Cat-B) are involved in EBOV GP cleavage (14). While Cat-L and Cat-B activities are important for EBOV entry in isolated cell lines, there is likely some redundancy in the protease cleavage in vivo as mice deficient in Cat-L or Cat-B are susceptible to infection with mouse-adapted EBOV (16).
Studies in vitro report that EBOV GP entry can become independent of Cat-B activity through several specific mutations (14). These mutations have been mapped to GP1 and GP2 (GP1,2) and are positioned along the interface of the two subunits. These mutations are proposed to destabilize the prefusion conformation, making GP1,2 more prone to proteolysis by other host proteases and lowering the threshold for triggering fusion.
Following protease cleavage and NPC1 binding, GP must undergo major structural changes to induce viral and host membrane fusion. These changes include the two heptad repeat regions (HR1 and HR2) extending the FL outward from the viral membrane to penetrate the host membrane (7). Host membrane penetration is facilitated by conformational changes within the FL that are induced by acidic pH and stabilized by three residues (17, 18).
A consistent theme that has emerged from the study of EBOV GP is its sequence plasticity. This includes the observation that the EBOV GP gene often acquires an additional uracil nucleotide in a stretch of 7 U nucleotides when the virus is passaged in tissue culture (TC) (19). The conversion of 7-U nucleotide stretch to an 8-U stretch in the GP gene results in a frameshift that eliminates expression of EBOV soluble GP (sGP) (19), a truncated GP excreted by infected cells. sGP is thought to act as a decoy that interferes with host immunosurveillance against the virion-associated GP1,2 (20, 21, 22). Expression of sGP also serves to limit the expression of GP1,2, which is cytopathic when expressed at high levels (23). While sGP likely contributes to viral fitness in vivo, the loss of sGP in vitro is a selection advantage.
Other tissue culture mutations in EBOV GP1,2 that alter key aspects of GP function have been identified. These include mutation within the FL of EBOV GP that changes a threonine at 544 to an isoleucine (24, 25). The T544I mutation occurs at a critical residue in the FL (18) and suggests that the amino acids present in the FL of clinical isolates of EBOV GP do not provide optimal entry into Vero cells.
We hypothesized that the clinical Makona GP (MAK-GP) would mutate in multiple ways to adapt to replication in Vero cells. Accordingly, we searched for spontaneous growth-adaptive mutations in GP using a replicating pseudotyped virus containing the GP. Here, we report six mutations identified through plaque isolate sequencing of early passages of vesicular stomatitis virus (VSV) VSV-MAK-GP. All mutations localized to the GP2 subunit and enhanced virus growth properties on monkey and human cell lines. We hypothesize that these mutations alter two different stages of entry: (i) cleavage by Cat-B and (ii) membrane fusion. These mutations provide new insight into the adaptive profile of clinical EBOV GP when grown on certain cell lines and highlight which residues are under selection pressure in vitro and in vivo.
RESULTS
Emergence of VSV-MAK-GP clones containing single amino acid substitutions in the Makona glycoprotein during virus recovery.
Analysis of recombinant VSVs (rVSVs) expressing EBOV glycoproteins has shown that growth in cell culture can lead to the selection of growth-adaptive GP mutations (19, 25). Following recovery of a recombinant VSV encoding the glycoprotein (GP) from a clinically isolated Ebola Makona virus (VSV-MAK-GP), we assessed the extent of mutational pressure on the glycoprotein during early recovery and passage of the virus. Here, we sequenced 19 plaque isolates from the passage 1 (P1) stock of the recovered VSV-MAK-GP virus in search of amino acid substitutions in GP.
Our sequencing revealed a significant amount of GP sequence plasticity. Of the 19 individual isolates, 5 retained the wild-type (WT) GP sequence. Fourteen isolates contained a single amino acid change in GP. A total of six different amino acid substitutions in GP were found among the 14 isolates (Table 1). These included the previously reported T544I mutation (two isolates), seven independent isolates of an H549R mutation, and two isolates of a D552N mutation. Three additional mutations, D522E, R574H, and I584L, were found, each in a single isolate. None of the clones contained two or more amino acid changes in GP.
TABLE 1.
Sequencing of 19 plaque-isolated clones of VSV-MAK-GP identifies mutations in GPa
| GP type in plaque clonea | No. of plaques containing GP typeb |
|---|---|
| WT | 5 |
| H549R | 7 |
| T544I | 2 |
| D552N | 2 |
| D522E | 1 |
| R574H | 1 |
| I584L | 1 |
Fourteen of the 19 isolates contained a single amino acid change in GP. In the WT, no nucleic acid substitutions were detected by Sanger sequencing.
From first passaged stock in VeroE6 cells.
To determine if these and/or other mutations in GP could be detected in the starting P1, we sequenced the supernatant from which the mutants were isolated. Each mutation was present in the P1 pool at a percentage that correlated with its frequency in the isolated plaque clones (Table 2, P1 sequences). The H549R mutation was present at the highest percentage, with 43% of P1 sequences encoding this mutation, while the T544I and D552N mutations appeared in 8% and 9% of sequences, respectively. Mutated nucleotide peaks representing the D522E, R574H, and I584L mutations were not detectable in sequence traces. There was no indication of any other nucleotide mutation in the P1 sequences.
TABLE 2.
Mutant pool composition in VSV-MAK-GP virus recovery in stocks from P1 and P3a
| Mutation | % of sequence with the mutationb |
|
|---|---|---|
| P1 | P3 | |
| D522E | ND | ND |
| T544I | 7.7 | 10.3 |
| H549R | 42.7 | 64.2 |
| D552N | 8.9 | 7.6 |
| R574H | ND | ND |
| I584L | ND | ND |
Stocks were serially passaged in VeroE6 cells (MOI of 0.001).
As determined by Sanger sequencing. ND, the nucleotide peak representing this mutation was not detected in the trace file.
We next determined whether the pool of mutations present at P1 would remain constant through multiple passages or whether passage would lead to consolidation to a single mutant. The P1 stock was serially passaged twice (P2 and P3) in Vero E6 cells at a low multiplicity of infection ([MOI] 0.001). The same three mutations detected in P1 (T544I, H549R, and D552N) were detected again in P3 (Table 2, P3 sequences). H549R continued to be the most prevalent mutation as the percentage of sequences encoding this mutation increased from 43% in P1 to 64% in P3 while mutations of T544I and D552N showed minor changes from P1 to P3. These results suggest that multiple virus mutants can stably coexist upon passaging in Vero E6 cells.
We next asked if any of the point mutations that appeared in our pseudotyped virus were present in GP genes harbored by EBOV. We analyzed over 1,500 EBOV sequences deposited in the NCBI database, including EBOV genomic sequences from clinical samples and more than a dozen sequences from laboratory-grown stocks. We have previously noted that the T544I mutation often arises in laboratory-passaged virus (25). Our analysis showed that, in addition to this mutation, the D552N mutation that spontaneously arose in our pseudotype was also found in five laboratory-passaged EBOV sequences (Table 3). Two of these sequences (GenBank accession numbers KP096421.1 and KT013257.3) are laboratory-passaged stocks of the Makona C07 clinical isolate (26). The original nonpassaged Makona C07 clinical isolate was reported to encode D552 (27). A different EBOV variant, the 1976 Zaire Eckron strain (NCBI accession number P87671.1), was also found to encode asparagine at position 552. We also analyzed sequence data from serial passaging experiments of clinical EBOV Makona isolates carried out at the U.S. Army Medical Research Institute of Infectious Diseases (USAMRIID). This analysis showed the appearance of the D522E mutation in one isolate passaged in Vero E6 cells (Table 3).
TABLE 3.
Occurrence of GP mutations in EBOV
| Mutation | Present in EBOV | EBOV source(s)a |
|---|---|---|
| D522E | Yes | SL-3817 (USAMRIID) |
| T544I | Yes | Multiple sequences in NCBI |
| H549R | No | NA |
| D552N | Yes | GenBank accession numbers KP096421.1, P87671.1, KY425648, KY425633, KT013257.3 |
| R574Hb | No | NA |
| I584L | No | NA |
These sources were passaged in VeroE6 cells. NA, not available.
Requires two nucleotide changes in EBOV but one nucleotide change in VSV-MAK-GP due to a different codon usage.
Evidence for constant mutation pressure on EBOV GP in cell culture lines.
The spontaneous appearance of GP mutations in both pseudotyped and authentic EBOV following passage in culture suggested that the WT EBOV GP is under constant pressure to evolve. To test this hypothesis, we passaged a plaque-purified wild-type stock of VSV-MAK-GP once on Vero E6 cells in five replicate wells. Each of the five replicate passages showed an amino acid change in GP (Fig. 1, top). Four replicates had a T544I mutation, and one replicate encoded a G524R mutation. A second passage of these replicates on Vero E6 cells showed that the mutant viruses accounted for >99% of sequences in their respective replicates. G524R was not among the plaque clone mutants discussed above, making this a seventh mutation identified in VSV-MAK-GP. Of note, this new mutation was not found in the EBOV sequences we analyzed above although two clinical isolate sequences (GenBank accession numbers KP759612 and KP759759) encode G524D mutations (28). These data support the hypothesis that upon growth in Vero E6 cells, viruses containing a wild-type EBOV GP are under significant selection pressure to gain growth-adaptive mutations.
FIG 1.
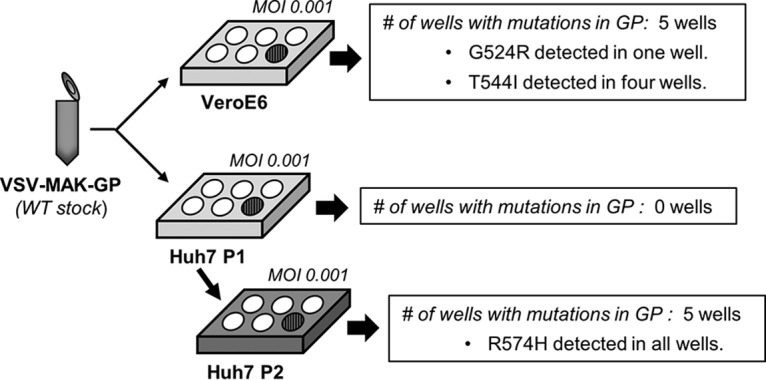
Passage of VSV-MAK-GP leads to emergence of glycoprotein mutations in HuH7 and Vero cells. The illustration shows the experimental approach for passage of WT VSV-MAK-GP on Vero E6 and HuH7 cells. Five replicates were analyzed for Vero cells at passage 1 (sequencing results are summarized in the boxes on the right). Five replicates were analyzed for HuH7 cells at passage 1 (plate P1) and at passage 2 (plate P2).
This pressure was also observed when the pseudotyped virus was passaged in human liver cells. HuH7 cells have been suggested to be a cell line where EBOV shows increased genomic stability, particularly at the level of GP mutation (29). HuH7 cells were infected with the same VSV-MAK-GP wild-type stock used for Vero E6 cells. Sequencing of virus progeny from this first passage (HuH7 P1) showed that none of the replicates had acquired detectable mutations in GP (Fig. 1, middle) but that by passage 2, five of five separate replicates showed populations with the R574H mutation (Fig. 1, bottom). The R574 mutation accounted for >50% of the virus population in four of the replicates by passage 4. These data also support the hypothesis that the clinical Makona GP peptide sequence is under significant selection pressure to gain growth-adaptive mutations in tissue culture.
Glycoprotein mutations in VSV-MAK-GP increase virus growth kinetics.
Based on the appearance and increase of mutations in EBOV GP upon laboratory passage, we anticipated that these novel GP mutations identified above would promote replication fitness. Multicycle growth studies (MOI of 0.01) of each mutant virus done in parallel with the wild-type stock are shown in Fig. 2. Each virus that contained a point mutation displayed more rapid growth kinetics than the wild-type virus on Vero E6 (Fig. 2A). Mutant virus titers were 10- to 45-fold higher than the titer of the wild type at 16 to 28 h postinfection (hpi). All mutants had similar growth kinetics, with titers that were within 3-fold of each other. These increased growth kinetics did not appear to be cell type specific. Multicycle growth curves (MOI of 0.01) performed on HuH7 cells indicated that each mutant virus exhibited more rapid titer accumulation than the wild type by at least 10-fold at 16 hpi (Fig. 2B). These growth data show that the point mutations acquired during passage increase virus growth kinetics.
FIG 2.
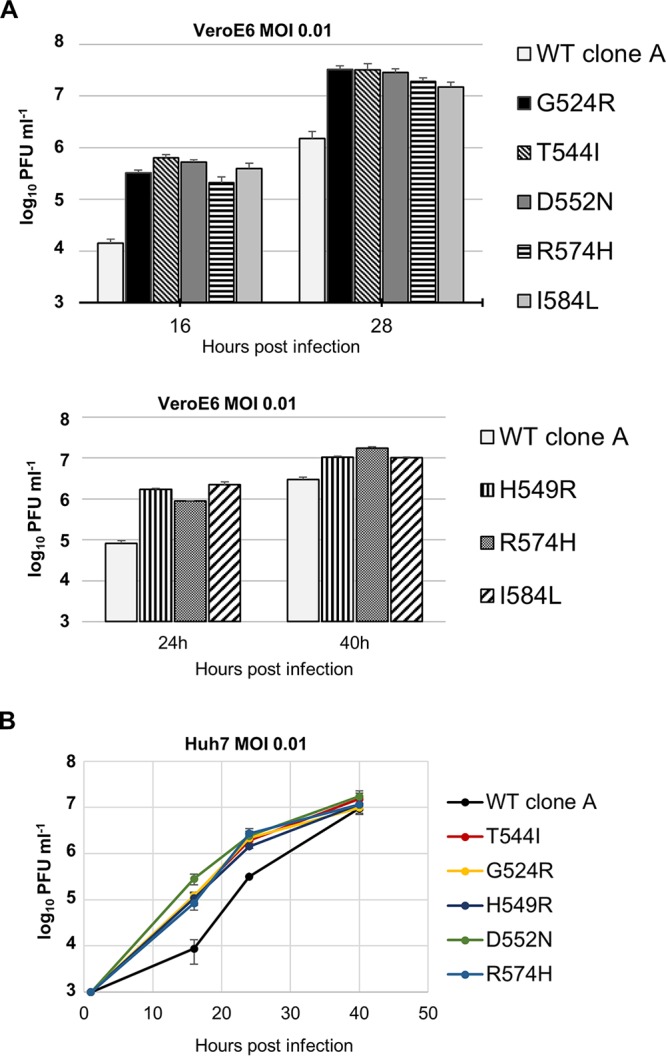
Mutations in EBOV GP increase growth kinetics of VSV-MAK-GP. Representative experiments were performed comparing growth of wild-type and mutant viruses. (A) Growth of WT and mutant viruses in Vero E6 cells at 16 and 28 hpi (MOI of 0.01). (B) Growth of WT and mutant viruses in HuH7 cells at 24 and 40 hpi (MOI of 0.01). Each graph presents data from a single experiment, representative of two replicates per virus. Error bars depict the range of the two replicates in each experiment.
Growth-adaptive mutations in VSV-MAK-GP are clustered in specific regions of the GP2 subunit.
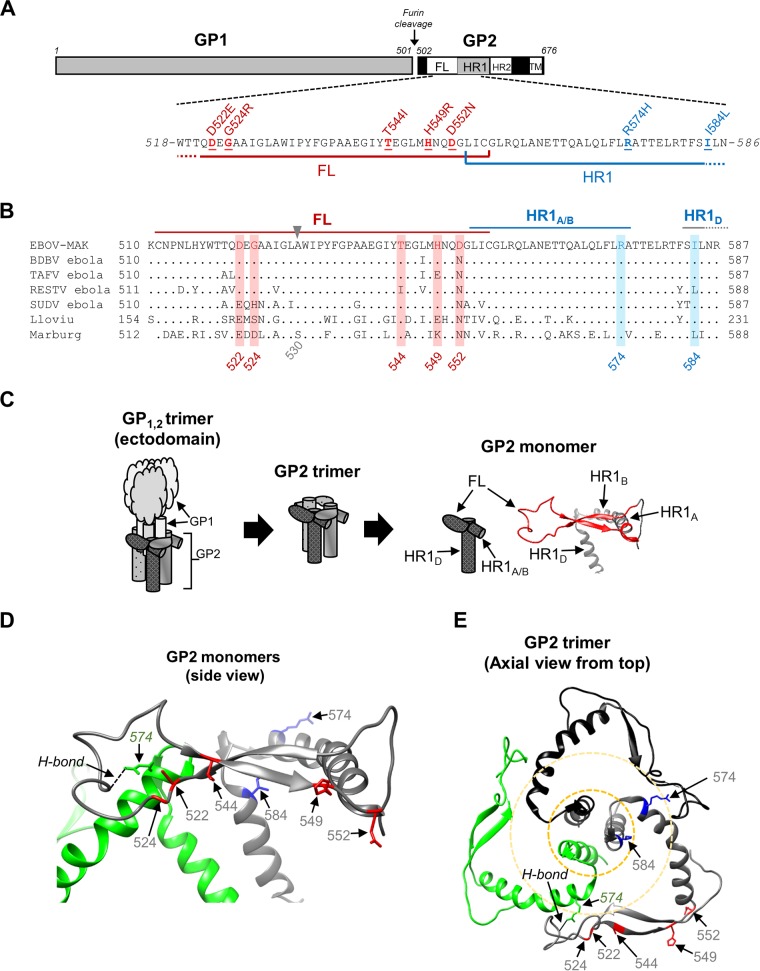
To gain insight into the positioning of the growth-adaptive mutations, we mapped each mutation on the primary and tertiary structures of EBOV GP1,2. The seven mutations we identified are situated within 62 amino acids of one another in the GP2 primary sequence (Fig. 3A). Five mutations (D522E, G524R, T544I, H549R, and D552N) are located within the fusion loop (FL), which is defined as residues 511 to 556 (7). Two mutations (R574H and I584L) are positioned just downstream of the FL in the first heptad repeat region (HR1). An alignment of these regions in filovirus GP shows that variability occurs at most of these mutation positions except at residue R574, which is fully conserved across the filoviruses (Fig. 3B).
FIG 3.
Mutations identified in VSV-MAK-GP are positioned in the fusion loop (FL) and heptad repeat 1 (HR1) of the GP2 subunit. (A) Linear depiction of GP1 and GP2 subunits showing mutation positions in the GP2 primary sequence. Mutations in the FL (red bar) are highlighted in red; mutations in HR1 (blue bar) are highlighted in blue. (B) Sequence alignment of filovirus fusion loops and HR1 regions. Representative FL and HR1 sequences for Ebola-MAK, Sudan (SUDV), Tai Forest (TAFV), Reston (RESTV), and Bundibugyo (BDBV) ebolavirus species as well as for Marburg and Lloviu sequences are shown. FL and HR1 amino acids are indicated by the red and blue lines above the sequences, respectively. Mutation positions are noted by the amino acid number and the red or blue shading for the FL and HR1 mutations, respectively; Lloviu numbers refer to GP2 residues only. (C) Cartoon illustrating the placement and structure of a GP2 monomer within the GP1,2 trimer structure. A molecular structure of the FL (in red) and HR1 subregions is shown on the far right. (D) Side view of two adjacent GP2 monomers showing the FL and HR1 regions (shaded gray) and the HR1 region (green). Amino acid positions where mutations were identified in VSV-MAK-GP are shown; numbers are colored according to the monomer on which they lie. Wild-type residues on the gray monomer are shown as red and blue sticks for FL and HR1 positions, respectively. Monomers are joined by a predicted intermolecular hydrogen bond (dashed line) between A530 (gray FL) and R574 (green HR1). (E) Axial view of the GP2 trimer showing mutation positions relative to the protein outer surface and inner stalk. Mutation positions are shown on the gray monomer as described in panel D. Dashed circles delineate regions that are increasingly buried within the trimer structure. Molecular structures in panels C to E are derived from Protein Data Bank structure 3CSY (13) and portrayed as ribbons generated with the UCSF Chimera package (39).
A cartoon offering a simplified breakdown of the mutations in the GP1,2 trimer structure is shown in Fig. 3C. In this simplified view of the ectodomain, the three GP1 subunits are bundled together in the inner region of the complex. The GP1 bundle is encircled by the three outer GP2 subunits that anchor the full ectodomain into the viral membrane via their transmembrane domains (Fig. 3C, left). Looking only at the GP2 subunit FL and HR1 regions, the three subunits appear to interact (Fig. 3C, middle and right). At the outer region of the GP2 bundle, the FL domain of one monomer extends to interact with HR1 subregions A and B (HR1A and HR1B) of the neighboring monomer (Fig. 3C, middle and right in diagram). The GP2 monomers may also interact hydrophobically at the interior of the GP2 bundle by way of the helical subregion D of HR1 (HR1D). An axial view of the GP2 trimer molecular structure shown in Fig. 3E gives a more detailed view of the monomer interactions occurring at the outer and inner regions of the GP2 bundle.
In the three-dimensional crystal structure, these mutations cluster into two separate regions. One region is at the base of the FL, where the H549R and D552N mutations are positioned (Fig. 3D and E). The second region of mutations is within the FL hydrophobic tip region where the D522E, G524R, and T544I mutations are positioned near each other. Just behind these residues, in HR1, lies the R574H mutation of the adjacent monomer. The WT R574 residue forms a hydrogen bond with the carboxyl group of residue of A530 in the FL hydrophobic tip (Fig. 3D and E). The I584L mutation, although in the same general area as the R574H mutation, is separated from the other two regions of mutations and is more internally buried in the trimer complex. The locations of the mutations in key regions of the GP2 fusion machinery suggest that these mutations enhance the fusion step of entry.
To experimentally determine if entry efficiency is increased by these mutations, we measured entry of wild-type and mutant GPs using EBOV virus-like particles (VLPs) that contain an EBOV VP40 protein fused with the beta-lactamase enzyme (VP40-BlaM). VLPs containing VP40-BlaM and either wild-type or mutant GP were produced. Western blots analyzing VLP preparations indicated that the mutant GP was incorporated into VLPs at levels similar to wild-type GP. Mutant VLPs were added to cells in equivalent particle amounts as wild-type VLPs based on VP40-BlaM levels. Coumarin cephalosporin fluorescein acetoxymethyl ester (CCF2-AM), a BlaM substrate with fluorescence reporter activity, was added to cells, and BlaM-positive cells were quantified by flow-cytometry.
Repeated experiments showed that VLPs containing the FL mutations G524R, T544I, and D552N had a significant increase in entry over VLPs containing wild-type GP by a factor of 2- to 2.5-fold (Fig. 4A, left). The two other FL mutations, D522E and H549R, also yielded, on average, greater entry than the wild type but not to the same degree as the other FL mutations and with inconsistent results (Fig. 4A, right). The variability produced by these two FL mutations was observed in repeated VLP preparations. The HR1 mutations R574H and I584L also yielded a significant increase in entry over the wild-type VLPs (Fig. 4B). These data are consistent with entry being enhanced at the step of fusion and highlight that these mutations modulate GP function apart from pseudotyped VSV.
FIG 4.
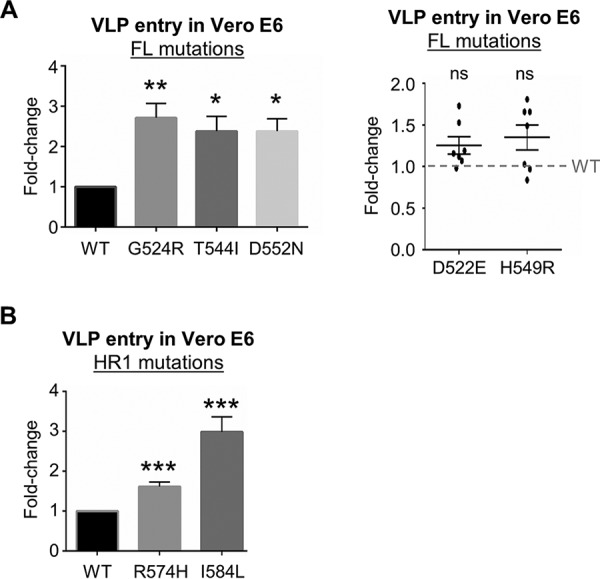
Mutations identified in VSV-MAK-GP increase entry efficiency of EBOV virus-like particles (VLPs). (A) Entry efficiencies of VLPs bearing GP proteins that contain a fusion loop mutant. The bar graph on the left shows fusion loop mutants that conferred a statistically significant increase in entry efficiency (n = 5). The scatter plot on the right shows fusion loop mutants that showed an inconsistent increase in entry that was not statistically significant (n = 7). The dashed line represents wild-type entry. (B) Entry efficiencies of VLPs bearing GP proteins that contain an HR1 mutation (n = 9). Entry efficiencies shown in panels A and B were determined as the percentage of beta-lactamase-positive cells using the CCF2-AM substrate and flow cytometry. Statistical significance for each mutant was determined by a two-tailed paired t test (*, P < 0.05; **, P < 0.01; ***, P < 0.001; ns P > 0.05).
A subset of mutations in VSV-MAK-GP alters the cathepsin B requirement for infection of Vero E6 cells.
We next investigated whether the growth-adaptive mutations changed the protease requirements of the EBOV-GP. It has been reported that mutations at amino acid 584 in HR1 of the EBOV Mayinga GP render cathepsin-B activity dispensable for Mayinga-pseudotyped VSV infection (14, 30). Thus, we were interested in determining whether the I584L mutation in the clinical Makona GP also changed the Cat-B protease requirement of EBOV GP.
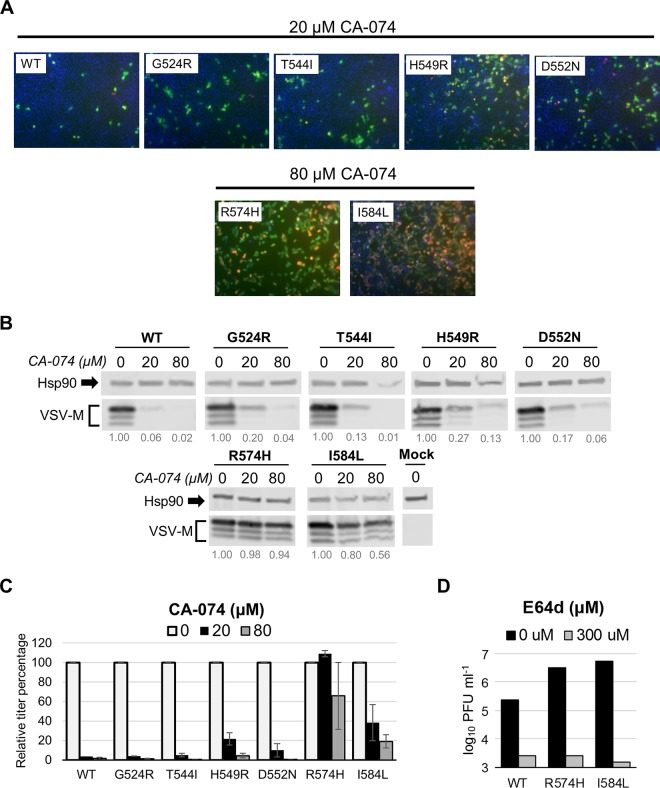
To determine if I584L and the other mutations identified in VSV-MAK-GP altered Cat-B dependence, we analyzed the effects of the Cat-B-specific inhibitor CA-074 on wild-type and mutant VSV-MAK-GP infections. Vero E6 cells were pretreated with CA-074 at 20 or 80 μM for 4 h prior to infection (MOI of 4). Infected cells were then probed for viral protein expression (VSV matrix [M] and Makona GP) by immunofluorescence at 16 hpi. Parallel control infections for wild-type and mutant viruses in the absence of the CA-074 inhibitor showed that most of the cells were positive for viral protein expression (data not shown). Treatment with 20 μM CA-074 blocked WT VSV-MAK-GP infection. Only about 1% of cells expressed viral proteins (Fig. 5A). Replication of FL mutants G524R, T544I, and D552N was also severely inhibited with 20 μM CA-074 (Fig. 5A, top row). The FL mutant H549R did show a modestly higher percentage of infected cells (∼5%) that was consistent across the monolayer. These results show that the increased viral replication and faster entry that resulted from these mutations were not due to an alteration in Cat-B sensitivity. In sharp contrast, the HR1 mutants R574H and I584L produced robust infections in the presence of 20 μM CA-074, with most cells expressing viral proteins (data not shown). The same was observed when the concentration of CA-074 was increased to 80 μM (Fig. 5A, second row).
FIG 5.
Makona GP mutations R574H and I584L reduce the dependency on cathepsin-B activity for VSV-MAK-GP infection of Vero E6 cells. (A) Immunofluorescence labeling of virally infected cells pretreated with the cathepsin-B inhibitor CA-074. The top row shows representative images of cells pretreated with 20 μM CA-074 and infected with the indicated virus. The second row shows cells pretreated with 80 μM CA-074 and infected with the indicated virus. Cells are labeled with 4′,6′-diamidino-2-phenylindole (blue) and antibodies against VSV matrix protein (green) and EBOV GP (red). Images were captured using a 10× objective. (B) Western blots measuring VSV matrix (M) protein accumulation in infected cell lysates at the indicated CA-074 concentrations. Relative levels of M protein accumulation (compared to the level with no treatment) are below each lane. Heat shock protein 90 (Hsp90) was used to normalize M protein values. (C) Reduction of virus growth titers by CA-074 inhibitor treatment. Values represent the mean and range of two independent experiments. (D) Representative experiment measuring growth titers in the absence and presence of E64D. Infection was performed at an MOI of 4, and growth was analyzed at 16 hpi.
These results were corroborated through experiments that determined viral protein accumulation. Immunoblotting showed that M protein accumulation was drastically reduced in the presence of the CA-074 inhibitor for wild-type virus (94% reduction at 20 μM) (Fig. 5B). The FL mutants also showed a drastic reduction in M protein accumulation in the presence of CA-074 (Fig. 5B, top row). Protein accumulation in the R574H infection at 80 μM CA-074 was essentially the same as that in untreated cells (Fig. 5B, bottom row). The I584L mutant, while still robust, was moderately affected by the inhibitor with protein reductions of 20% and 44% at 20 and 80 μM, respectively (Fig. 5B, bottom row).
Growth titers of the two experiments were measured by plaque assay and correlated well with the immunofluorescence and Western blot data. Reductions in titers due to CA-074 were essentially identical between the wild type and most FL mutants (95 to 97% reduction at 20 μM), with the H549R mutant showing less of a reduction in titer (79%) at the same concentration (Fig. 5C). The R574H mutant showed no decrease in titer in either experiment at 20 μM; however, the I584L mutation at the same concentration did show a moderate decrease in titer in both experiments (80% and 42% decrease), consistent with it being more sensitive to the effects of CA-074 than to those of the R574H mutant.
These data indicate that the HR1 mutations in VSV-MAK-GP reduce the dependency on Cat-B activity for productive infection but that the FL mutations do not have a major impact on Cat-B dependency. All viruses retained a requirement for cysteine protease activity as all were sensitive to the pan-cysteine protease inhibitor E64D [2S,3S-trans-(ethoxycarbonyloxirane-2-carbonyl)-l-leucine-(3-methylbutyl) amide], as shown by R574H and I584L titer reductions (Fig. 5D). Together, these studies provide evidence that there are differences between the mechanisms by which mutations in the FL and the HR1 promote virus replication. Interestingly, mutations in GP that emerge during authentic EBOV replication in tissue culture all fall into the category of mutations that increase entry without altering protease sensitivity.
DISCUSSION
We have observed the appearance of seven mutations in the EBOV Makona GP following its inclusion in a replicating rVSV backbone and passage in different cell types. These mutations are growth adaptive for the pseudotyped virus and break down into two groups determined by their positions in GP2 and their mechanisms of action. In the first group are five mutations in FL (D522E, G524R, T544I, H549R, and D552N). These mutations increase infectivity but do not alter Cat-B dependence. Three of these five mutations also appear in tissue culture-passaged EBOV. The second functional group of mutations includes two mutations within HR1, R574H and I584L. These mutations also confer increases in pseudotyped-virus infectivity and, in contrast to the FL mutations, decrease the dependence of the EBOV GP on Cat-B activity during the entry process.
Mutations in the fusion loop.
A striking aspect of our findings was the isolation of five different mutations that are within the fusion loop region of GP2, each providing a growth advantage. Of these five, the T544I mutation has been extensively discussed elsewhere (25). Two of the remaining four mutations in FL (D522E and D552N) occur spontaneously in TC-adapted EBOV. Interestingly, both of these mutations are representative of change from the consensus EBOV residue to the consensus Sudan ebolavirus (SUDV) residue (compare sequences shown in Fig. 3B). A third mutation in FL, G524R, represents a mutation that is chemically similar to the consensus residue in SUDV GP (H524). These SUDV residues do not change in sequences derived from SUDV clinical isolates (31) and sequences derived from tissue-cultured SUDV. All three of these mutations showed increased entry kinetics using EBOV VLPs. Assuming that these mutations also confer increased entry in vivo, the functional gain seen through these mutations raises an interesting evolutionary question between EBOV and SUDV. Why do clinical SUDV viruses encode the entry-optimal residues but clinical EBOV viruses encode the entry-suboptimal residues?
Two other FL mutations we identified, D522E and H549R, displayed greater entry efficiency than wild-type GP, but this increase was inconsistent. The variability exhibited by these mutants occurred in repeated VLP preparations. The advantage provided by these two mutations may require a condition or factor that varies during propagation in Vero E6 cells, resulting in variable effects on entry. Even so, D522E emerged under positive selection in at least one EBOV stock grown in Vero E6 cells (Table 3). These findings demonstrate that the FL mutations identified here increase entry efficiency, consistent with an enhancement of the fusion mechanism.
How do these mutations potentiate entry? Based on their clustered location in the FL, we propose that these mutations are modulating the fusion step of entry. We previously utilized nuclear magnetic resonance (NMR) structures of FL reported by other investigators to propose that the mutated I544 residue produced a more stable membrane-penetrating “fist” structure at pH 5.5 (17, 18, 25). Mapping the new GP mutations on the NMR structure shows that D522E and G524R are positioned just behind the penetrating hydrophobic surface area, or at the knuckles in the fist analogy. H549R and D552N are at the opposite end of the FL structure near the base of the wrist. The effects these mutations might have on the low-pH structure of FL are not apparent. We speculate that D522E and G524R might increase the surface charge of the FL to further compact the hydrophobic residues together and that H549R and D552N act like a wrist to modulate the angle of the fist for optimal penetration into the membrane.
Alternatively, some mutations may alter the FL prefusion structure. In the various prefusion crystal structures of EBOV GP, D522 and G524 lie in a short stretch of residues (∼521 to 525) that do not align when the FLs from these structures are superimposed, while the rest of the FL structures align well. It is possible that D522E and G524R function to better stabilize the FL prefusion conformation under TC conditions.
Heptad repeat region mutants.
The I584L mutation in VSV-MAK-GP appearing as a Cat-B-independent mutation of EBOV GP is evocative of earlier work that identified I584F and I584L as mutations that conferred Cat-B independence in a pseudotyped VSV bearing the EBOV Mayinga GP that lacked a mucin-like domain (14, 30). These reports did not note that mutations at position 584 provided increased growth kinetics; this may reflect that the GP sequence used contained a T544I mutation, which provides a growth advantage of its own. It is possible that the I584F/I584L mutations do not confer a growth advantage in addition to that provided by the T544I mutation.
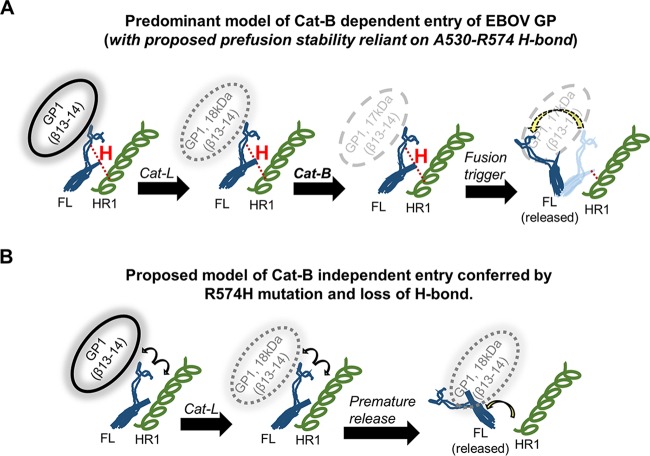
Our studies identify R574 as a new position within GP2 where mutation confers Cat-B independent entry. I584 and K588 are the other known positions in GP2 where mutation alters Cat-B dependence (14). Residues 584 and 588 are located in HR1D, an alpha-helix structure at the C-terminal end of HR1 that is part of the internal fold of the prefusion structure of the GP. Residue 574 is positioned in HR1B, the second half of a horizontal alpha-helix that is perpendicular to HR1D, and makes direct contacts with the neighboring fusion loop (Fig. 3C and 6). Wild-type R574 makes a hydrogen bond (∼1.8 Å) with the carboxyl group of alanine at amino acid 530 of the adjacent GP2 fusion loop (Fig. 6, upper panels), tethering the FL and likely aiding its tucked-in prefusion conformation. R574 is fully conserved among all filoviruses (R575 for Reston ebolavirus and Marburg), as shown in Fig. 3B. The R574H mutation would eliminate the H bond to amino acid 530, leading to a less stably tethered FL in the prefusion GP (Fig. 6, lower panels). We propose that this mutation allows easier release of the FL and serves as the basis for the Cat-B-independent phenotype observed in the R574H mutant.
FIG 6.
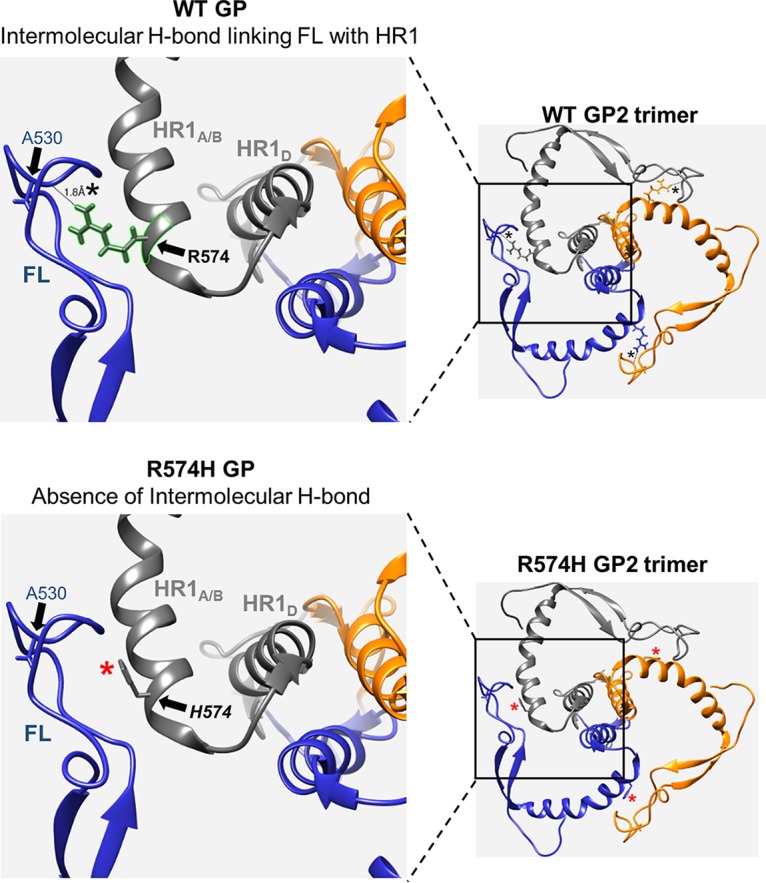
Arginine-to-histidine mutation at amino acid 574 disrupts an intermolecular hydrogen bond that connects the fusion loop and HR1 regions of adjacent GP2 monomers. Ribbon structures of wild-type GP and R574H mutant GP highlighting the absence of the H bond in the mutant GP. For both, the full GP2 trimer is shown in the smaller image on the right, with the boxed area magnified in the image on the left. GP2 monomers are individually indicated in blue, gray, and orange. The 574 residue (wild type in bold and mutant in italics) is shown as a stick structure. The A530 residue in the FL is shown as a blue stick structure. The black asterisks in the wild-type structure denote the presence of the H bond, and the red asterisks in the mutant structure denote the absence of the H bond. Molecular structures are derived from PDB structure 3CSY (13) and portrayed as ribbons generated with the UCSF Chimera package (39).
Proposed model for Cat-B independence.
The existing model for the steps involved in EBOV entry (7, 14) suggests that, following internalization, GP is cleaved first by Cat-L, which increases the fusion capacity of the 18-kDa GP intermediate but does not make it fusion competent. Following this step, the GP is further cleaved by Cat-B to create a fusion-competent 17-kDa GP. We posit that in the wild-type GP the intermolecular A530-R574 H bond contributes to “holding” the FL in place in the 17-kDa GP after Cat-B cleavage. A schematic of the existing model incorporating our proposed H bond linkage is shown in Fig. 7A. This H bond is disrupted at a step downstream of Cat-B cleavage, possibly before or as a result of fusion triggering. We propose, as illustrated in Fig. 7B, that the absence of the H bond in the R574H mutant induces instability in the FL prefusion conformation. This, in turn, promotes a premature release of the FL from its prefusion conformation in the 18-kDa intermediate after Cat-L cleavage, thus allowing Cat-B independent entry.
FIG 7.
Proposed model of Cat-B independence due to the loss of a stabilizing hydrogen bond in the R574H mutant GP. (A) Cartoon of the predominant model of Cat-B-dependent entry of EBOV GP that includes the proposed stabilizing effect of the intermolecular H bond on the prefusion conformation. The hydrogen (H) bond is shown as a red dotted line. The position of the GP1 beta 13-beta 14 fragment on the outer edge of the FL is an approximation based on GP crystal structures. The H bond is proposed to remain intact after Cat-B cleavage and is broken at a downstream step. (B) Proposed model of the R574H mutant GP that lacks the H bond. Premature release of the FL is proposed to occur after Cat-L cleavage in the 18-kDa GP intermediate due to instability of the FL prefusion conformation.
Not all filovirus GPs require Cat-B cleavage for infectivity, at least in Vero cells. Sudan and Reston ebolaviruses, as well as Marburg viruses, are reported to be Cat-B independent (16, 30). We believe the H bond connecting FL and HR1 exists with the same purpose in these viruses. It may prove insightful to determine if an analogous mutation to histidine in GP of these viruses also results in increased infectivity (assuming that no other TC mutations exist in these GPs). An increase in infectivity would suggest that the FLs of these mutant GPs, regardless of cathepsin requirement differences, are also prone to more rapid triggering and, hence, entry.
Effects of mutations on therapeutics targeting GP.
These mutations could impact screening and characterization studies for therapeutic antibodies and inhibitors targeting EBOV GP1,2. Both FL and HR1 are prime targets for candidate therapeutics. FL, in particular, is a target for a number of important antibodies such as the neutralizing antibody KZ52 (32) and two therapeutics antibodies in the ZMapp cocktail, c2G4 and c4G7 (33). The D552N mutation lies within the epitopes of these three antibodies, and mutation of D552 to alanine severely reduces their activities (34). It is not determined yet if D552N and the nearby H549R mutation alter the efficacy of these antibodies, but this illustrates the uncertainty that TC mutations can create if they appear in surrogate virus or EBOV stocks used in these types of studies.
The possibility of these mutations arising as escape mutations to these therapies should also be considered. The same D522E mutation we observed in our pseudotyped virus and EBOV stock was recently reported to emerge in Bundibugyo ebolavirus GP as an escape mutant to the BDBV317 and BDBV340 antibodies (35). Curiously, the epitopes for these antibodies map to the second heptad repeat region near the membrane-proximal external region. This suggests that FL mutations can influence the efficacy of antibodies that target other regions in GP2.
GP adaptation on Vero E6 and HuH7 cells.
Vero E6 cells are the standard cell line used to grow EBOV stocks and to characterize EBOV growth properties. Previous studies report that upon passage in Vero E6 cells, genetic changes can occur in EBOV GP. This is exemplified by the 7 U-8 U conversion(19), but a mutation in the fusion loop has also been defined. Our findings here further highlight the propensity of EBOV GP to mutate in Vero E6 cells. Specifically, the mutations we identified point to the fusion process and cathepsin-B cleavage as being readily adaptive in Vero E6 cells. The instability of the clinical GP sequence in Vero E6 cells raises the question of whether these cells are ideal for virus stock generation and characterization.
All of the mutant viruses we identified here showed similar increases in growth kinetics over levels in the wild-type virus on HuH7 cells, but only one mutation, R574H, appeared in passage on HuH7 cells (Fig. 1). We are uncertain why the evolutionary trajectory in the different cell types appears to be different, but this may be due to the general mutability in the different cell types. Tsuda et al. reported that the genetic mutation accumulation of GP in HuH7 cells is lower than that in Vero and other monkey kidney cell lines (29). This lower genetic plasticity could be one reason why most of the mutations we identified in Vero cells did not emerge in HuH7 cells. It is also possible that the R574H mutation has a growth advantage in HuH7 cells that enabled it to outcompete the other mutations. If so, understanding the basis for such an advantage in HuH7 cells could be insightful. Our findings here show that clinical EBOV GP, independent of the 7 U-8 U conversion, is prone to adaptation in HuH7 cells.
MATERIALS AND METHODS
Cell culture and viruses.
Vero E6 and HuH7 cells were grown in Dulbecco's modified Eagle's medium (DMEM) supplemented with 10% fetal bovine serum (FBS). Recovery and initial passage (P1) of the recombinant VSV-MAK-GP virus was described previously (25). Mutant viruses encoding amino acid changes in GP were isolated by aspirating individual plaques derived from the recovered virus P1 stock and inoculation into 0.5 ml of DMEM to serve as clone master stocks. Aliquots of each clone master stock were sequenced prior to growth amplification, as described previously (25). Working stocks for each mutant virus were generated by adding 0.2 ml of the clone master stock onto Vero E6 cells in T-75 flasks (with 12 ml of DMEM) and harvesting supernatants upon complete infection of the monolayer (∼72 h). Supernatants were clarified by low-speed centrifugation (900 × g), and aliquots were frozen at −80°C. Working stocks were sequenced to confirm the presence of the expected GP mutation. Mutant virus working stocks used in these studies had no detectable wild-type residue at the expected position or any other nucleotide changes in the GP gene. Working stock titers were determined by standard plaque assay on Vero E6 cells.
Immunofluorescent staining of viral proteins.
Vero E6 cells in 12-well plates were fixed with 4% paraformaldehyde and permeabilized with 0.1% Triton X-100 at 16 hpi. Cells were blocked with 1% bovine serum albumin (BSA) for 1 h prior to the addition of antibodies. EBOV GP1,2 was probed with c4G7 and c2G4 primary antibodies (Mapp Biopharmaceutical) and anti-human Alexa Fluor 568 secondary antibody (Thermo Fisher Scientific). VSV M protein was probed with mouse 23H12 primary antibody and anti-mouse Alexa Fluor 488 secondary antibody (Thermo Fisher Scientific). Fluorescent images were captured on a Zeiss 200M epifluorescence microscope using identical exposure settings for wild-type and mutant analysis.
VLP cell entry assay.
EBOV VLPs incorporating the β-lactamase (BlaM)-VP40 fusion protein were pseudotyped with wild-type or mutant GP1,2. The EBOV Makona wild-type GP sequence (GenBank accession number AHX24658.2) was cloned into a pcDNA3 plasmid. Mutant GP-encoding plasmids were generated by using primer-designed site-directed mutagenesis (QuickChange PCR; Stratagene) with a pcDNA3 wild-type GP plasmid serving as a template. HEK-293T cells were transfected with plasmids encoding EBOV NP, VP40-BlaM, and wild-type or mutant GP-encoding plasmids for 65 h at 37°C and 5% CO2. Supernatants were harvested and clarified, and VLPs were purified by ultracentrifugation through a 20% sucrose cushion (25,000 rpm at 4°C for 1.5 h). VLP pellets were resuspended in phosphate-buffered saline (PBS), aliquoted, and stored at −80°C. Incorporation of GP and VP40-BlaM in VLPs was confirmed by Western blotting. VP40-BlaM content was measured by comparison with known input amounts of recombinant VP40-glutathione S-transferase (GST) protein (30-1837; Fitzgerald), and all VLPs were normalized by their VP40-BlaM content. Vero E6 cells in 12-well plates were infected with VLPs (VP40-BlaM input of 8 ng) by spinoculation (1 h at 1,200 × g), followed by incubation at 37°C for an additional hour. Cells were washed to remove unbound particles, trypsinized, and transferred to 96-well U-bottom plates and incubated with CCF2-AM fluorescent reporter overnight at 18°C. Cells were fixed with 4% paraformaldehyde, and the percentage of BlaM-positive cells was measured by flow cytometry.
Deep-sequencing analysis of EBOV Makona isolate viruses.
Clinical isolate Ebola virus/Homo sapiens-WT/SLE/2014/Makona-G3817 (GenBank accession number KM233091) was passaged on Vero E6 cells for 16 days. Virus was harvested, and this P1 stock was designated R4467. The EBOV Makona virus stocks were sequenced at the U.S. Army Medical Research Institute of Infectious Diseases using an unbiased amplification protocol. RNA was isolated from TRIzol-treated material using a Zymo Direct-Zol kit (Zymo Research, Irvine, CA, USA). Sequence-independent single-primer amplification (SISPA) was performed as previously described (36). Amplified material was prepared for Illumina-based next-generation sequencing by shearing DNA to 400 bp using an M220 focused ultrasonicator (Covaris, Woburn, MA). Sequencing libraries were prepared using an Apollo 324 PrepX ILM 32I (Wafergen, Fremont, CA) with in-house dual indexes. The quality of the libraries was assessed for correct size on a DNA 1000 chip (Agilent Technologies, Santa Clara, CA) and quantified using a quantitative PCR (qPCR) library quantification kit for Illumina sequencing platforms (Kapa Biosystems, Wilmington, MA). Sequencing was performed on a MiSeq benchtop sequencer (Illumina, San Diego, CA) with either a MiSeq version 2 or kit producing 2-by-151 paired-end reads.
For virus stock R4467, we estimated the frequency of the T-to-G mutation at nucleotide 7568 resulting in the D522E amino acid change using the in-house pipeline VSALIGN (37). VSALIGN is a Perl pipeline that uses open-source programs cutadapt and prinseq-lite (38) for preprocessing of samples, including adapter removal, PCR duplicate removal, and quality filtering. Additional preprocessing steps are provided using in-house tools to remove chimeric sequences, sequences with bad or no mate, and sequences that do not have significant matches to the reference. Reference-based alignment to isolate Ebola virus/H. sapiens-WT/SLE/2014/Makona-G3817 (GenBank accession number KM233091) was performed on the remaining sequence with SeqMan NGen (SeqMan NGen, version 14.0.0.87; DNASTAR, Madison, WI) to determine consensus and determine frequency of small nucleotide polymorphisms (SNPs).
Cysteine protease inhibitor treatments.
Cysteine protease inhibitors CA-074 [(l-3-trans-(propylcarbamyl)oxirane-2-carbonyl)-l-isoleucyl-l-proline] (Sigma-Aldrich, St. Louis, MO) and E64D [2S,3S-trans-(ethoxycarbonyloxirane-2-carbonyl)-l-leucine-(3-methylbutyl) amide] (Enzo Life Sciences, Farmingdale, NY) were dissolved in dimethyl sulfoxide (DMSO) at 100× concentrations and added to cells at a final concentration of 1× inhibitor in 1% (vol/vol) DMSO. Cells were pretreated with inhibitors for 4 h prior to infection. Inhibitors were maintained in medium throughout the duration of virus adsorption and incubation.
Western blotting.
Cell lysates were harvested by washing cell monolayers twice with PBS followed by lysis with 1% NP-40 buffer containing a protease inhibitor cocktail (A32955; Thermo Scientific). Cytoplasmic fractions were processed by SDS-PAGE on 4 to 20% gradient Tris-HCl gels (Bio-Rad) and electroblotted onto polyvinylidene difluoride (PVDF) membranes. Membranes were blocked with Odyssey blocking buffer (927-40000; Li-Cor Biosciences) for 1 h before the addition of primary antibodies. VSV matrix (M) protein was probed with mouse anti-M antibody 23H12 (1:2,000). The Ebola glycoprotein (GP) was probed with human-mouse chimeric anti-GP antibody c6D8 (Mapp Biopharmaceutical), and the VP40 protein was probed with rabbit anti-VP40 antibody (IBT), both at 1:2,000 dilutions. Hsp90 protein was probed with mouse anti-Hsp90 α/β antibody (Santa Cruz Biotechnologies) at a 1:2,000 dilution. IRDye secondary antibodies (Li-Cor Biosciences) were utilized at 1:10,000 dilutions for imaging on an Odyssey CLx scanner (Li-Cor Biosciences). Goat anti-human IRDye secondary antibody was used for the human-mouse chimeric anti-GP antibody. Protein bands were quantified with Image Studio software (Li-Cor Biosciences).
Accession number(s).
The sequences determined in this study have been deposited in the GenBank database under BioProject number PRJNA470889.
ACKNOWLEDGMENTS
We thank Judith M. White at the University of Virginia School of Medicine and Erica Ollmann Saphire at The Scripps Research Institute, La Jolla, CA, for helpful discussions. We also thank the members of the Connor laboratory at Boston University School of Medicine for their critical readings of the manuscript. We thank Karla Prieto for performing the sequencing of the SL-3817 isolate at USAMRIID.
This work was funded by R21AI135517 and AI1096159 to J.H.C. Work at the U.S. Army Medical Research Institute of Infectious Diseases was funded by the Defense Threat Reduction Agency, project CB10246 (to G.P.). Molecular graphics and analyses were performed with the UCSF Chimera package. Chimera was developed by the Resource for Biocomputing, Visualization, and Informatics at the University of California, San Francisco (supported by NIGMS P41-GM103311) (39).
The content of this publication does not necessarily reflect the views or policies of the U.S. Army.
REFERENCES
- 1.World Health Organization. 2018. Ebola virus disease, 12 February 2018 World Health Organization, Geneva, Switzerland: http://www.who.int/news-room/fact-sheets/detail/ebola-virus-disease. [Google Scholar]
- 2.Qiu X, Wong G, Audet J, Bello A, Fernando L, Alimonti JB, Fausther-Bovendo H, Wei H, Aviles J, Hiatt E, Johnson A, Morton J, Swope K, Bohorov O, Bohorova N, Goodman C, Kim D, Pauly MH, Velasco J, Pettitt J, Olinger GG, Whaley K, Xu B, Strong JE, Zeitlin L, Kobinger GP. 2014. Reversion of advanced Ebola virus disease in nonhuman primates with ZMapp. Nature 514:47–53. doi: 10.1038/nature13777. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Corti D, Misasi J, Mulangu S, Stanley DA, Kanekiyo M, Wollen S, Ploquin A, Doria-Rose NA, Staupe RP, Bailey M, Shi W, Choe M, Marcus H, Thompson EA, Cagigi A, Silacci C, Fernandez-Rodriguez B, Perez L, Sallusto F, Vanzetta F, Agatic G, Cameroni E, Kisalu N, Gordon I, Ledgerwood JE, Mascola JR, Graham BS, Muyembe-Tamfun J-J, Trefry JC, Lanzavecchia A, Sullivan NJ. 2016. Protective monotherapy against lethal Ebola virus infection by a potently neutralizing antibody. Science 351:1339–1342. doi: 10.1126/science.aad5224. [DOI] [PubMed] [Google Scholar]
- 4.Zhao Y, Ren J, Harlos K, Jones DM, Zeltina A, Bowden TA, Padilla-Parra S, Fry EE, Stuart DI. 2016. Toremifene interacts with and destabilizes the Ebola virus glycoprotein. Nature 535:169–172. doi: 10.1038/nature18615. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Jeffers SA, Sanders DA, Sanchez A. 2002. Covalent modifications of the Ebola virus glycoprotein. J Virol 76:12463–12472. doi: 10.1128/JVI.76.24.12463-12472.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Volchkov VE, Feldmann H, Volchkova VA, Klenk HD. 1998. Processing of the Ebola virus glycoprotein by the proprotein convertase furin. Proc Natl Acad Sci U S A 95:5762–5767. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Lee JE, Saphire EO. 2009. Ebolavirus glycoprotein structure and mechanism of entry. Future Virol 4:621–635. doi: 10.2217/fvl.09.56. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Saeed MF, Kolokoltsov AA, Albrecht T, Davey RA. 2010. Cellular entry of Ebola virus involves uptake by a macropinocytosis-like mechanism and subsequent trafficking through early and late endosomes. PLoS Pathog 6:e1001110. doi: 10.1371/journal.ppat.1001110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Nanbo A, Imai M, Watanabe S, Noda T, Takahashi K, Neumann G, Halfmann P, Kawaoka Y. 2010. Ebolavirus is internalized into host cells via macropinocytosis in a viral glycoprotein-dependent manner. PLoS Pathog 6:e1001121. doi: 10.1371/journal.ppat.1001121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Côté M, Misasi J, Ren T, Bruchez A, Lee K, Filone CM, Hensley L, Li Q, Ory D, Chandran K, Cunningham J. 2011. Small molecule inhibitors reveal Niemann-Pick C1 is essential for Ebola virus infection. Nature 477:344–348. doi: 10.1038/nature10380. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Miller EH, Obernosterer G, Raaben M, Herbert AS, Deffieu MS, Krishnan A, Ndungo E, Sandesara RG, Carette JE, Kuehne AI, Ruthel G, Pfeffer SR, Dye JM, Whelan SP, Brummelkamp TR, Chandran K. 2012. Ebola virus entry requires the host-programmed recognition of an intracellular receptor. EMBO J 31:1947–1960. doi: 10.1038/emboj.2012.53. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Carette JE, Raaben M, Wong AC, Herbert AS, Obernosterer G, Mulherkar N, Kuehne AI, Kranzusch PJ, Griffin AM, Ruthel G, Cin PD, Dye JM, Whelan SP, Chandran K, Brummelkamp TR. 2011. Ebola virus entry requires the cholesterol transporter Niemann-Pick C1. Nature 477:340–343. doi: 10.1038/nature10348. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lee JE, Fusco ML, Hessell AJ, Oswald WB, Burton DR, Saphire EO. 2008. Structure of the Ebola virus glycoprotein bound to an antibody from a human survivor. Nature 454:177–182. doi: 10.1038/nature07082. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Wong AC, Sandesara RG, Mulherkar N, Whelan SP, Chandran K. 2010. A forward genetic strategy reveals destabilizing mutations in the Ebolavirus glycoprotein that alter its protease dependence during cell entry. J Virol 84:163–175. doi: 10.1128/JVI.01832-09. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Chandran K, Sullivan NJ, Felbor U, Whelan SP, Cunningham JM. 2005. Endosomal proteolysis of the Ebola virus glycoprotein is necessary for infection. Science 308:1643–1645. doi: 10.1126/science.1110656. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marzi A, Reinheckel T, Feldmann H. 2012. Cathepsin B & L are not required for Ebola virus replication. PLoS Negl Trop Dis 6:e1923. doi: 10.1371/journal.pntd.0001923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Gregory SM, Harada E, Liang B, Delos SE, White JM, Tamm LK. 2011. Structure and function of the complete internal fusion loop from Ebolavirus glycoprotein 2. Proc Natl Acad Sci U S A 108:11211–11216. doi: 10.1073/pnas.1104760108. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Gregory SM, Larsson P, Nelson EA, Kasson PM, White JM, Tamm LK. 2014. Ebolavirus entry requires a compact hydrophobic fist at the tip of the fusion loop. J Virol 88:6636–6649. doi: 10.1128/JVI.00396-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Volchkova VA, Dolnik O, Martinez MJ, Reynard O, Volchkov VE. 2011. Genomic RNA editing and its impact on Ebola virus adaptation during serial passages in cell culture and infection of guinea pigs. J Infect Dis 204(Suppl):S941–S946. doi: 10.1093/infdis/jir321. [DOI] [PubMed] [Google Scholar]
- 20.Maruyama T, Parren PW, Sanchez A, Rensink I, Rodriguez LL, Khan AS, Peters CJ, Burton DR. 1999. Recombinant human monoclonal antibodies to Ebola virus. J Infect Dis 179:S235–S239. doi: 10.1086/514280. [DOI] [PubMed] [Google Scholar]
- 21.Ito H, Watanabe S, Takada A, Kawaoka Y. 2001. Ebola virus glycoprotein: proteolytic processing, acylation, cell tropism, and detection of neutralizing antibodies. J Virol 75:1576–1580. doi: 10.1128/JVI.75.3.1576-1580.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Wilson JA, Hevey M, Bakken R, Guest S, Bray M, Schmaljohn AL, Hart MK. 2000. Epitopes involved in antibody-mediated protection from Ebola virus. Science 287:1664–1666. doi: 10.1126/science.287.5458.1664. [DOI] [PubMed] [Google Scholar]
- 23.Alazard-Dany N, Volchkova V, Reynard O, Carbonnelle C, Dolnik O, Ottmann M, Khromykh A, Volchkov VE. 2006. Ebola virus glycoprotein GP is not cytotoxic when expressed constitutively at a moderate level. J Gen Virol 87:1247–1257. doi: 10.1099/vir.0.81361-0. [DOI] [PubMed] [Google Scholar]
- 24.Hoffmann M, Crone L, Dietzel E, Paijo J, González-Hernández M, Nehlmeier I, Kalinke U, Becker S, Pöhlmann S. 2017. A polymorphism within the internal fusion loop of the Ebola virus glycoprotein modulates host cell entry. J Virol 91:e00177-17. doi: 10.1128/JVI.00177-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Ruedas JB, Ladner JT, Ettinger CR, Gummuluru S, Palacios G, Connor JH. 2017. Spontaneous mutation at amino acid 544 of the Ebola virus glycoprotein potentiates virus entry and selection in tissue culture. J Virol 91:e00392-17. doi: 10.1128/JVI.00392-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hoenen T, Groseth A, Feldmann F, Marzi A, Ebihara H, Kobinger G, Feldmann H. 2014. Complete genome sequences of three Ebola virus isolates from the 2014 outbreak in West Africa. Genome Announc 2:e01331-14. doi: 10.1128/genomeA.01331-14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Baize S, Pannetier D, Oestereich L, Rieger T, Koivogui L, Magassouba N, Soropogui B, Sow MS, Keïta S, De Clerck H, Tiffany A, Dominguez G, Loua M, Traoré A, Kolié M, Malano ER, Heleze E, Bocquin A, Mély S, Raoul H, Caro V, Cadar D, Gabriel M, Pahlmann M, Tappe D, Schmidt-Chanasit J, Impouma B, Diallo AK, Formenty P, Van Herp M, Günther S. 2014. Emergence of Zaire Ebola virus disease in Guinea. N Engl J Med 371:1418–1425. doi: 10.1056/NEJMoa1404505. [DOI] [PubMed] [Google Scholar]
- 28.Tong Y-G, Shi W-F, Liu D, Qian J, Liang L, Bo X-C, Liu J, Ren H-G, Fan H, Ni M, Sun Y, Jin Y, Teng Y, Li Z, Kargbo D, Dafae F, Kanu A, Chen C-C, Lan Z-H, Jiang H, Luo Y, Lu H-J, Zhang X-G, Yang F, Hu Y, Cao Y-X, Deng Y-Q, Su H-X, Sun Y, Liu W-S, Wang Z, Wang C-Y, Bu Z-Y, Guo Z-D, Zhang L-B, Nie W-M, Bai C-Q, Sun C-H, An X-P, Xu P-S, Zhang X-L-L, Huang Y, Mi Z-Q, Yu D, Yao H-W, Feng Y, Xia Z-P, Zheng X-X, Yang S-T, Lu B, et al. 2015. Genetic diversity and evolutionary dynamics of Ebola virus in Sierra Leone. Nature 524:93–96. doi: 10.1038/nature14490. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Tsuda Y, Hoenen T, Banadyga L, Weisend C, Ricklefs SM, Porcella SF, Ebihara H. 2015. An improved reverse genetics system to overcome cell-type-dependent Ebola virus genome plasticity. J Infect Dis 212:S129–S137. doi: 10.1093/infdis/jiu681. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Misasi J, Chandran K, Yang J-Y, Considine B, Filone CM, Côté M, Sullivan N, Fabozzi G, Hensley L, Cunningham J. 2012. Filoviruses require endosomal cysteine proteases for entry but exhibit distinct protease preferences. J Virol 86:3284–3292. doi: 10.1128/JVI.06346-11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Albariño CG, Shoemaker T, Khristova ML, Wamala JF, Muyembe JJ, Balinandi S, Tumusiime A, Campbell S, Cannon D, Gibbons A, Bergeron E, Bird B, Dodd K, Spiropoulou C, Erickson BR, Guerrero L, Knust B, Nichol ST, Rollin PE, Ströher U. 2013. Genomic analysis of filoviruses associated with four viral hemorrhagic fever outbreaks in Uganda and the Democratic Republic of the Congo in 2012. Virology 442:97–100. doi: 10.1016/j.virol.2013.04.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Maruyama T, Rodriguez LL, Jahrling PB, Sanchez A, Khan AS, Nichol ST, Peters CJ, Parren PW, Burton DR. 1999. Ebola virus can be effectively neutralized by antibody produced in natural human infection. J Virol 73:6024–6030. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Audet J, Wong G, Wang H, Lu G, Gao GF, Kobinger G, Qiu X. 2014. Molecular characterization of the monoclonal antibodies composing ZMAb: a protective cocktail against Ebola virus. Sci Rep 4:6881. doi: 10.1038/srep06881. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Davidson E, Bryan C, Fong RH, Barnes T, Pfaff JM, Mabila M, Rucker JB, Doranz BJ. 2015. Mechanism of binding to Ebola virus glycoprotein by the ZMapp, ZMAb, and MB-003 cocktail antibodies. J Virol 89:10982–10992. doi: 10.1128/JVI.01490-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Flyak AI, Kuzmina N, Murin CD, Bryan C, Davidson E, Gilchuk P, Gulka CP, Ilinykh PA, Shen X, Huang K, Ramanathan P, Turner H, Fusco ML, Lampley R, Kose N, King H, Sapparapu G, Doranz BJ, Ksiazek TG, Wright DW, Ollmann Saphire E, Ward AB, Bukreyev A, Crowe JE Jr. 2018. Broadly neutralizing antibodies from human survivors target a conserved site in the Ebola virus glycoprotein HR2-MPER region. Nat Microbiol 3:670–677. doi: 10.1038/s41564-018-0157-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Djikeng A, Halpin R, Kuzmickas R, DePasse J, Feldblyum J, Sengamalay N, Afonso C, Zhang X, Anderson NG, Ghedin E, Spiro DJ. 2008. Viral genome sequencing by random priming methods. BMC Genomics 9:5. doi: 10.1186/1471-2164-9-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Kugelman JR, Wiley MR, Nagle ER, Reyes D, Pfeffer BP, Kuhn JH, Sanchez-Lockhart M, Palacios GF. 2017. Error baseline rates of five sample preparation methods used to characterize RNA virus populations. PLoS One 12:e0171333. doi: 10.1371/journal.pone.0171333. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Schmieder R, Edwards R. 2011. Quality control and preprocessing of metagenomic datasets. Bioinformatics 27:863–864. doi: 10.1093/bioinformatics/btr026. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Pettersen EF, Goddard TD, Huang CC, Couch GS, Greenblatt DM, Meng EC, Ferrin TE. 2004. UCSF Chimera—a visualization system for exploratory research and analysis. J Comput Chem 25:1605–1612. doi: 10.1002/jcc.20084. [DOI] [PubMed] [Google Scholar]