Abstract
Context:
Significant reforms are needed to improve healthcare system performance in Quebec. Even though the characteristics of high-performing healthcare systems are well-known, Quebec's reforms have not succeeded in implementing many critical elements. Converging evidence from political science models suggests stakeholders' preferences are central in determining policy content, adoption, and implementation.
Objective:
To analyze whether doctors’, nurses’, pharmacists' and health administrators' preferences could explain the observed inability to implement known characteristics of high-performing healthcare systems.
Design:
A questionnaire on various propositions identified in the scientific literature was sent to 2,491 potential respondents.
Results:
Overall response rate was 37%. There was considerable consensus on identified solutions to improve the healthcare system. Resistance was observed in two major areas: information systems and changes directly affecting doctors' practice. The groups' positions cannot explain the inability to implement important characteristics of high-performing systems. The findings raise new questions on the actual sources of resistance.
Abstract
Contexte:
D'importantes réformes sont nécessaires pour améliorer la performance du système de santé au Québec. Même si on connaît bien les caractéristiques des systèmes de santé performants, les réformes entreprises au Québec n'ont pas permis la mise en place de plusieurs éléments essentiels. Les données provenant des modèles en science politique suggèrent que les préférences des parties prenantes jouent un rôle central dans l'élaboration du contenu, dans l'adoption et dans la mise en œuvre des politiques.
Objectif:
Analyser dans quelle mesure les préférences des médecins, infirmières, pharmaciens et administrateurs des institutions de santé peuvent expliquer l'incapacité à mettre en place les caractéristiques propres aux systèmes de santé performants.
Méthodes:
Un questionnaire portant sur plusieurs propositions identifiées dans la littérature scientifique a été envoyé à 2 491 répondants potentiels.
Résultats:
Le taux de réponse général était de 37 %. Il y a un fort consensus sur les solutions identifiées pour améliorer le système de santé. On observe une résistance dans deux secteurs principaux: les systèmes d'information et les changements qui affectent directement la pratique des médecins. La position des groupes ne peut toutefois expliquer l'incapacité à mettre en place les caractéristiques essentielles aux systèmes performants. Ces résultats soulèvent de nouvelles questions quant aux sources réelles de la résistance.
Introduction
Despite consensus that significant reforms are needed to improve Canadian healthcare systems' performance, important characteristics of high-performing healthcare systems have been implemented slowly or even not at all. One plausible explanation is the potential disagreement between or within stakeholder groups having an influence on health policies. In this article, we analyzed doctors’, nurses’, pharmacists' and health administrators' preferences regarding a set of propositions aiming at improving the healthcare system.
Many characteristics of high-performing healthcare delivery systems are well known and consensual (Baker et al. 2008; Casalino et al. 2003; Contandriopoulos and Brousselle 2010; Feachem et al. 2002; Ham et al. 2003; Katz et al. 2009; McMurchy 2009; Mechanic 2008; Robinson et al. 2004; Russell et al. 2009; Shortell et al. 2005). These include a system-wide focus on primary care implemented through integrated delivery systems (IDSs) responsible for a given population, in which doctors are remunerated in other ways besides pure fee-for-service. Clinical and managerial practices should be based on strong integrated information systems at the individual, clinical, organizational and population levels. IDSs should also be accountable at both individual and population levels.
In Quebec, all publicly appointed commissions since the beginning of Medicare (Castonguay-Nepveu Commission 1967–1970; Clair Commission 2000; Rochon Commission 1988) have identified similar characteristics and recommended policy options consistent with scientific evidence. In Canada, the Romanow Commission (Romanow 2002) also drew on scientific evidence to ensure the healthcare system's sustainability and improve timely access to good-quality care by recommending the development of an accountable, primary care-centred system relying on interprofessional teams and robust information systems. The same recommendations have appeared in other national and provincial commissions' reports (Drummond 2012; Fyke 2001; Health Council of Canada 2008; Ontario HSRC 2000; Romanow 2002).
However, analysis of reforms implemented in Quebec during the past 20 years suggests that, although they led to important structural changes, many critical elements were systematically ignored – such as revising doctors' compensation models, increasing access to primary care, and implementing an integrated information system – and consequently the desired results were not achieved (Contandriopoulos and Brousselle 2010). The convergence of scientific evidence and public commission recommendations shows that the obstacle to implementing reforms is neither lack of evidence nor ignorance about solutions (Lewis 2007). The logical conclusion is that the main challenge lies in translating recommendations into policy and implementing policy in actual delivery system structures and practices. Previous research (Contandriopoulos and Bilodeau 2008; Contandriopoulos and Brousselle 2010; Contandriopoulos et al. 2007) suggests most such obstacles arise from different interest group positions on the desirability of given policy options (Drummond 2012).
In this paper, we report on the positions of four stakeholder groups – doctors, nurses, pharmacists and health administrators – regarding a set of policy propositions supported by scientific writings. The objective was to examine the degree of convergence in those groups' support for various policy solutions and to identify points of resistance that might explain the observed inability to implement evidence-based healthcare system policy changes.
Methods
This article reports on an anonymous survey that was part of a sequential qualitative–quantitative mixed-method study (Creswell and Plano Clark 2011). The survey content was based on analysis of the first-phase, individual interviews with 31 people having influence on Quebec health policy (Brousselle et al. 2014), and on solutions suggested by scientific articles and the above-cited Quebec health commissions. The interviews focused on healthcare system strengths, problems, and solutions and on identifying persons with the most influence on healthcare policies.
We invited a random sample of 750 doctors, 748 nurses and 750 pharmacists to participate in the survey. Inclusion criteria were membership in a professional order and active practice status. Contact information was obtained from Quebec's College of Physicians, Order of Nurses and College of Pharmacists. All senior administrators (n = 243) of healthcare institutions were identified through public service e-mail directories and solicited. Administrators were the CEOs (Directeur général), vice-CEO (Directeur général adjoint) and clinical directors (e.g., directeur des services professionnels, directeur des soins infirmers, etc.) from all hospital structures in Quebec. The questionnaire was sent by e-mail or mail to these 2,491 persons between August 17 and November 24, 2015.
The questionnaire elicited the degree of agreement with a series of propositions supported by the scientific literature and endorsed by leaders in the previous interviews. It included 29 questions on seven themes: (1) healthcare system performance; (2) information systems; (3) patients' roles; (4) primary care team functioning; (5) primary care accessibility; (6) coordination between hospital and primary care; and (7) clinical appropriateness and efficiency. Each theme was introduced by a fictional case study to illustrate the proposed solutions in day-to-day practice. In a last single open question, respondents were invited to make three suggestions to the Health Minister to improve the healthcare system. We also elicited demographic and practice information. The questionnaire was developed in French and English and made available both online and in paper form.
Statements about policy proposals were strongly worded to elicit degree of agreement on a 5-point Likert scale (1 = strongly disagree, 3 = neutral, 5 = strongly agree). A neutral point was included to identify the proportion of stakeholders not polarized on the issues. Within a given theme, the proposed changes were ordered on a gradient from what we believed would be perceived as more benign or consensual measures to more invasive or drastic changes. Results are presented in this order.
The questionnaire and the survey strategy were cognitively tested with 12 respondents from the four stakeholder groups. We adapted Dillman's Total Design Method (Dillman et al. 2009) to optimize response rate; since the survey was anonymous, all potential respondents were sent reminders and a second questionnaire. Administrators and nurses were invited to answer the survey online, as we only had their e-mail addresses. French paper versions were mailed to doctors and pharmacists, with instructions for responding online if preferred, or for obtaining an English paper version. Closed questions were analyzed using SPSS 22.0. Open question responses were independently coded by two persons. The study was approved by the Human Research Ethics Committee of the Université de Sherbrooke Hospital.
Likert scores were analyzed in two ways. In the first, the numbers of respondents in each group supporting or opposing each survey statement were analyzed to assess the distribution of opinions. For each group, each statement was then categorized according to four possibilities. If more than 60% of the respondents in the group agreed or strongly agreed with a statement, we considered it supported. Likewise, if more than 60% of the respondents in the group disagreed or strongly disagreed with a statement, we considered it opposed. If neither the “agree” and “strongly agree” nor the “disagree” and “strongly disagree” proportions showed a clear majority, and the indifferent constituted less than 15% of the total respondents in the group, then the distribution of opinion was likely bimodal. Finally, if none of the above applied, it meant respondents were more or less evenly spread and no clear consensus was apparent. Table 1 (see Table 1) presents this data using a colour code to facilitate reading.
In the second analysis, we computed the Likert score means and standard deviations for each group's answers to each question. Mean scores are usually presented as bar graphs with error bars. However, even though the data are discrete, we added a connecting line between each group's mean score, our rationale being that the order of the questions for each theme in the survey instrument was determined by our expectation of a dwindling level of support. The connecting lines put the emphasis on the similitude or divergence between groups in the variation of the support regarding each question.
Results
In all, 934 persons answered the survey but only 919 completed surveys were included in the analysis due to missing responses. Response rates for the final sample were: pharmacists 45%, doctors 40%, administrators 33%, nurses 26%; overall 37%. The respondent sample was generally representative of the sex, training, and location of each group's population, except that university-trained nurses were significantly over-represented. We weighted nurses' responses to control for this bias. A total of 774 (82%) participants answered the open question, with a mean of 3.2 solutions (range 1–12) provided per respondent.
The overall response rate of 37% is somewhat lower than observed in surveys of professionals and managers (Blais et al. 1999; Gilbert et al. 2006; Haley et al. 2000; Maheux et al. 2006; Makni et al. 2002; National Physician Survey 2007; O'Loughlin et al. 2007; Richard et al. 2005; Sicotte et al. 2002; Tremblay et al. 2009). However, if we exclude nurses, the combined response rate for the other groups falls within the range generally observed. For nurses, our rate was lower than generally observed (Faulkner and Laschinger 2008; Laschinger et al. 2008; Laschinger et al. 2009; Lehoux et al. 2006; Lucas et al. 2008; Tremblay et al. 2009). While we have no definitive explanation for the lower than expected response rate, nurses were the only group for which we had to rely mostly on e-mails as the primary contact modality.
Theme 1: Need for system improvement
The first question measured support regarding the need for general improvement in the system's performance. Results showed strong support, with all respondents (100%) agreeing Quebec's healthcare system needs improvement. The only variation was in the relative proportions of “agree” versus “strongly agree”. This result tallies with the Commonwealth Fund survey for Quebec (Commissaire à la santé et au bien-être 2016).
Theme 2: Information systems
There was strong support in all groups for the idea that all professionals should receive feedback on their practice and that information systems should make it possible to monitor healthcare team practices. A majority of respondents also agreed administrative data should be coupled with clinical data to monitor professional practice. It is noteworthy that although 56% of doctors agreed or strongly agreed, 27% disagreed or strongly disagreed. However, while respondents generally agreed feedback on clinical practice would be good at individual or team levels, there was less support for sharing this information with professional orders. The strongest support for this idea was observed among the pharmacists. Support for using clinical information systems to control incentives was even weaker, with only a minority of professionals supporting the idea and a majority of doctors disagreeing or strongly disagreeing. As illustrated in Figure 1, as statements linking clinical information to external control became stronger, support became weaker.
Figure 1.
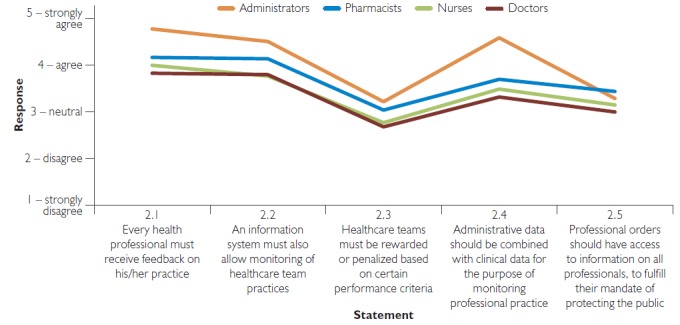
Overall agreement regarding the role and place of information systems with questions ordered in increasing degree of external control
Theme 3: Patients' roles
The first-phase qualitative interviews showed broad support for increasing patients' centrality in decision-making at individual and system levels. This tallied with pressure in this direction from professional groups, such as Choosing Wisely (http://www.choosingwisely.org), and with funding agency initiatives, such as the Canadian Institutes for Health Research (CIHR) Strategy for Patient-Oriented Research (http://www.cihr-irsc.gc.ca/e/41204.html). Our goal was to assess the acceptability of a greater role and more rights for patients. More specifically, we focused the questions on increasing patients' access to their clinical data and their clinicians (Figure 2). The acceptability of such a shift was rather low. More than 60% of doctors disagreed or strongly disagreed with all three proposals. Only administrators, among the four groups, clearly supported the idea that patients should have online access to tests and exams. Nurses, pharmacists and administrators were divided on this idea. When the question suggested giving patients full access to their electronic health record, only administrators supported this idea (with 58% agreeing or strongly agreeing), while other groups showed significant opposition (with 70% of doctors, 51% of nurses and 59% of pharmacists disagreeing or strongly disagreeing with the statement).
Figure 2.
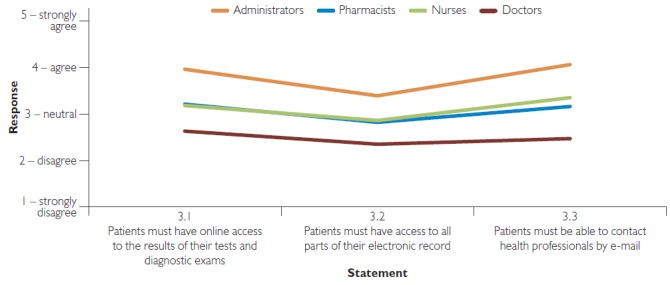
Agreement regarding patients' roles
Theme 4: Primary care teams functioning
The fourth theme focused on implementing strongly interdisciplinary primary care teams that would include doctors, nurse practitioners, clinical nurses, social workers, and other professionals, and in which doctors would be a minority of the workforce. A clear majority of respondents in each group agreed such teams would increase accessibility to services and improve care for patients with multi-morbidities, and that they should not be allowed to refuse patients with mental and drug addiction problems. Likewise, there was consensus that primary care teams should collaborate with pharmacies, implement a broader scope of practice for non-doctor professionals – on which even doctors agreed in majority (59%) – and coordinate diagnostic and specialized care for their patients. When asked whether teams should meet daily to discuss clinical cases, doctors mainly disagreed (56%); several commented that daily meetings would be too frequent. Nurses and pharmacists agreed with the proposition, while administrators were more polarized on this question (Figure 3).
Figure 3.
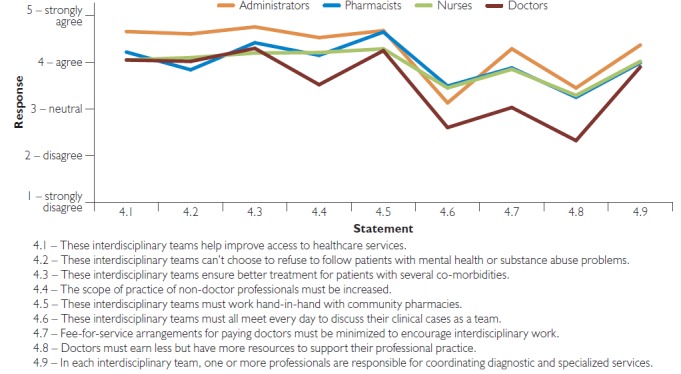
Acceptability of strongly interdisciplinary primary care teams
It is interesting to note that, when it came to modifying fee-for-service – the dominant doctor compensation model in Quebec – we observed similar agreement (40%) and disagreement (38%) proportions among doctors, with 21% being indifferent. Yet maintaining that model is likely to stifle interdisciplinary practice and is commonly seen as a barrier to implementing the primary care model described in the survey instrument (Mason 2016). It is interesting to note, from a policy perspective, that if those doctors declaring indifference to that issue were to change their minds and support the option, it could create the necessary conditions for a change in the way doctors are paid. There was strong support (72% of nurses and pharmacists and 91% of administrators) and almost no opposition from non-doctors to revising the doctor compensation model (only 6% to 9% of non-doctors opposing the idea). The idea of reallocating funds from doctors' compensation into more primary care resources was, on average, modestly supported by all non-doctor groups and clearly opposed by doctors.
Theme 5: Primary care accessibility
The fifth theme was a continuation of the previous one but focused more specifically on primary care accessibility and patient rostering (Figure 4). Rostering patients to a primary care team was widely supported by all groups, as was the idea that patients should be required to consult this team first for non-urgent care. On the supply side, respondents strongly agreed on the desirability of extending opening hours, including evenings and weekends. However, support dropped, especially among doctors and nurses, when rostering was interpreted as a way to measure whether patients actually consulted their assigned team and to penalize teams when they did not. In other words, clinicians accepted rostering patients but were reluctant to be held accountable when patients sought care outside their rostered clinic.
Figure 4.
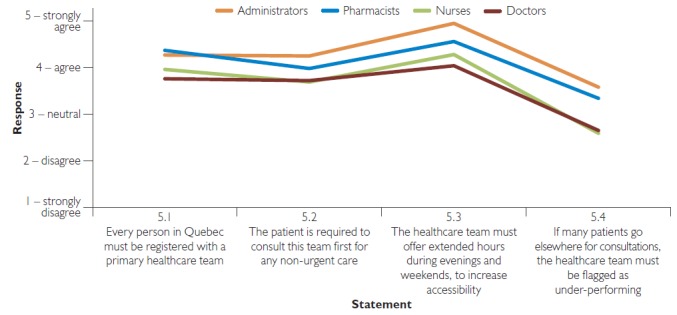
Acceptability of patient rostering and primary care accessibility
Theme 6: Coordination between hospital and primary care
There is much evidence that optimizing patient care pathways could significantly enhance quality and efficiency. In Quebec, this idea dominated policy debates in two large-scale forced-merger laws enacted in 2004 and 2015 (Contandriopoulos et al. 2007; Québec 2003, 2015). In 2004, most hospitals, long-term care institutions (centres d'hébergement et de soins de longue durée [CHSLDs]), and community clinics were merged to create health and social services centres (CSSSs) mandated to develop geographically defined healthcare networks. However, the intended improvements in collaboration with autonomous primary care teams within those territories did not materialize. In 2015, almost all remaining autonomous hospitals and all CSSSs in each region were further merged to create 22 multisite, multi-mission care delivery institutions. Primary care structures were again not included, and no credible care-coordination mechanisms were implemented (Contandriopoulos et al. 2014). We therefore assessed support for propositions regarding sharing of responsibility and coordination of care between hospitals and primary care networks. As long as the question's formulation implied no transfer of resources or activities, all groups unambiguously supported the principle of improving coordination of hospital and primary care (Figure 5). When the question implied a transfer of activities, however, intergroup polarization increased.
Figure 5.
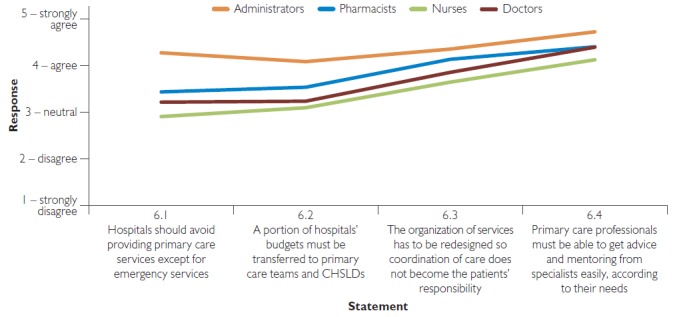
Agreement regarding coordination between hospital and primary care
CHSLDs = centres d'hébergement et de soins de longue durée (residential and long-term care centres).
The statements that specialist doctors should support primary care teams as needed and that patients should not be left to assume the burden of coordinating their own care were both widely supported by all groups. The idea that hospitals should stop offering non-urgent primary care was still supported by a majority but with much more polarization: administrators 88%, pharmacists 61%, doctors 54% and nurses 51%.
Theme 7: Clinical appropriateness and efficiency
There was strong support from all groups for greater use of scientific evidence in clinical practice (administrators 99%, doctors 92%, nurses 90%, pharmacists 96%) and institutional management. All groups agreed institutions should be allowed to eliminate diagnostic tests or clinical practices not deemed relevant, with stronger support among administrators (89%) than pharmacists (67%), nurses (62%) or doctors (53%) (see Figure 6). Again, support fell when the statement implied any coercion or limitation of professional autonomy.
Figure 6.
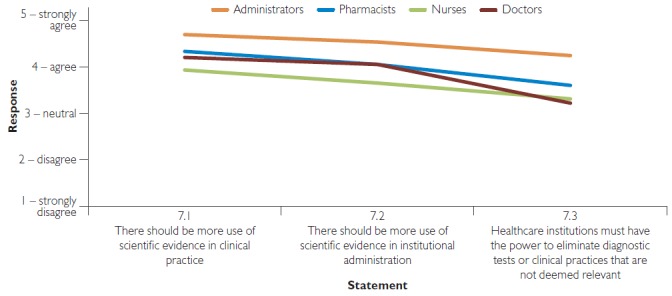
Agreement regarding clinical appropriateness and efficiency
Open question: Respondents' suggestions to the Health Minister
There was significant convergence in solutions proposed. All groups supported increasing interdisciplinary teams and redefining roles of non-doctor professionals. Likewise, all professionals saw improving access to primary care as a priority. Administrators proposed different action priorities, which included revising professionals' compensation models and improving care appropriateness (Table 2).
Table 2.
Most salient solutions put forward by each professional group
| Ranking | Solutions | |||
|---|---|---|---|---|
| Administrators | Doctors | Nurses | Pharmacists | |
| 1 | Revise professional modes of payment | Increase interdisciplinarity and redefine roles on non-doctor professionals | Increase interdisciplinarity and redefine roles on non-doctor professionals | Increase interdisciplinarity and redefine roles on non-doctor professionals |
| 2 | Increase interdisciplinarity and redefine roles on non-doctor professionals | Improve access to technical platform and specialists | Enhance access to primary care services | Enhance access to primary care services |
| 3 | Increase care pertinence | Enhance access to primary care services | Improve working conditions and appreciate professionals' work | Implement a systemic patient file |
Discussion
This study offers new insights into how stakeholders compare in their support for specific implementable solutions. It revealed broad consensus among the four groups on solutions for improving healthcare performance. Furthermore, the impressive convergence in responses to the closed question suggest this consensus is not an artefact of closed question surveying.
In general, we did not observe major differences in the groups' support for the various propositions. General levels of agreement went in a similar direction for all groups, with only levels of support somewhat differing. Hence, our results do not suggest polarization or clear disagreement between administrators, pharmacists, nurses and doctors on most questions, but rather that some groups are more (or less) enthusiastic in their support.
Overall, administrators were more supportive of system reform than were other groups, often closely followed by pharmacists. While doctors' pattern of support for various statements was almost always the same as for the other groups, they were consistently below the others in their mean score for almost all statements tested.
Based on levels of support expressed, we would anticipate resistance to change in two major areas. The first relates to information systems and includes both patients having access to their clinical data and information being used for monitoring and team accountability. Although the majority in each group supported the statements related to information systems, clearly there was resistance, which may relate to the scope of intrusion into clinical practice and to fear of undesirable effects. This suggests the pace of information systems implementation should be kept in line with professional capacity for adoption and that experimental sites might be good starting points to learn from experiences and adjust systems according to what may be acceptable.
The second area where resistance was observed among doctors was on topics directly affecting medical practice: patients' right to access professionals by e-mail, doctor compensation models, and the proposition that doctors be paid less and, in exchange, receive more resources for their practice. These points all relate to compensation; at this time, e-mail contacts are not compensated, and the other two points directly affect income. Medical practice organization and doctor compensation are clearly elements that were side-stepped in reforms of the past 20 years in Quebec. One important observation from this survey is that the balance of power lies in the hands of those doctors declaring indifference on the topic.
However, in our view, the real contribution of this paper lies elsewhere. As indicated, our results showed there is a margin of action for substantial improvement in healthcare system performance, such as removing barriers to interdisciplinary team work, using information systems to inform professionals on their practice and monitor performance, and applying scientific evidence more substantially to clinical and administrative practice. Yet even though our results show strong consensual support for many policy options, those solutions are not currently at the forefront of the transformations in Quebec's healthcare system.
Furthermore, our finding that there was strong consensus and broad support among professionals and administrators around many policy options contradicts the political allegation that failure in implementing those solutions is due to stakeholder resistance. This raises further research questions about why some evidence-supported policy avenues are consistently not implemented in Quebec and why reforms have repeatedly failed to implement important and scientifically sound solutions to improve performance. An intriguing avenue of investigation might be the influence of medical unions. In interviews, key spokespersons cited these unions as the actors with the most influence on health policies (Brousselle et al. 2014), far more influential than pharmaceutical companies, public opinion or even the government itself. Could they be so powerful that they prevent implementation of recommended changes even if their members support those changes? To what extent do medical unions represent doctors' opinions? These questions warrant closer examination.
Limitations
This study has a few limitations worth mentioning. While we committed significant time and energy to survey data collection, the response rates were still far from perfect. Data collection also took place during a massive structural reform in Quebec that probably impacted respondent perceptions. Finally, the analysis presented here is mostly descriptive and exploratory. For those reasons, the precise level of support for each policy option should be interpreted with caution. However, we believe that the overall portrait of a large consensus for evidence-based solution isn't affected by those limitations.
Conclusion
Quebec's healthcare system reforms over the past 20 years have mostly focused on transforming the structure of care (decentralization and recentralization, shift to healthcare networks, increased role for family medicine groups). However, little has changed with regard to medical practice, which remains largely centred around medical responsibility and is resistant to shifting to interdisciplinary teams and compensation models that support group work rather than individual productivity. However, this study suggests there is broad consensus among professionals for implementing important changes in the healthcare system and medical practice. Polarization among professionals is not the core issue. Could better evidence, communication, and open political debates be part of the solution?
Contributor Information
Astrid Brousselle, Professor, School of Public Administration, University of Victoria, Victoria BC; Researcher, Charles LeMoyne Hospital Research Center, Longueuil, QC.
Damien Contandriopoulos, Professor, School of Nursing, University of Victoria, Victoria, BC.
Jeannie Haggerty, Professor, Department of Family Medicine, McGill University; Researcher, St. Mary's Hospital Research Center, Montreal, QC.
Mylaine Breton, Professor, Department of Community Health Sciences, Université de Sherbrooke; Researcher, Charles LeMoyne Hospital Research Center, Longueuil, QC.
Michèle Rivard, Professor, University of Montreal School of Public Health; Researcher, University of Montreal Public Health Research Institute (IRSPUM), Montreal, QC.
Marie-Dominique Beaulieu, Professor, Department of Family and Emergency Medicine, University of Montreal; Researcher, University of Montreal Hospital Research Center (CRCHUM), Montreal, QC.
Geneviève Champagne, Coordinator, Charles LeMoyne Hospital Research Center, Longueuil, QC.
Mélanie Perroux, Coordinator, University of Montreal Public Health Research Institute (IRSPUM), Montreal, QC.
References
- Baker G.R., MacIntosh-Murray A., Porcellato C., Dionne L., Stelmacovich K., Born K. 2008. High Performing Healthcare Systems: Delivering Quality by Design. Toronto, ON: Longwoods Publishing Corporation. [Google Scholar]
- Blais R., Lambert J., Maheux B. 1999. “What Accounts for Physician Opinions about Midwifery in Canada?” Journal of Nurse-Midwifery 44(4): 399–407. 10.1016/S0091-2182(99)00061-0. [DOI] [PubMed] [Google Scholar]
- Brousselle A., Contandriopoulos D., Breton M., Rivard M., Haggerty J., Beaulieu M.-D., Perroux M. 2014. “Comment réformer le système de santé ? Perceptions des acteurs-clés des forces du système de santé au Québec, des problèmes et des solutions pour améliorer la performance et garantir sa pérennité.” Université de Sherbrooke, Longueuil, QC: Retrieved January 13, 2018. <http://ipspl.info/Comment_Reformer_Systeme_Sante.pdf>. [Google Scholar]
- Casalino L., Gillies R.R., Shortell S.M., Schmittdiel J.A., Bodenheimer T., Robinson J.C. et al. 2003. “External Incentives, Information Technology, and Organized Processes to Improve Health Care Quality for Patients with Chronic Diseases.” Journal of the American Medical Association 289(4): 434–41. 10.1001/jama.289.4.434. [DOI] [PubMed] [Google Scholar]
- Castonguay-Nepveu Commission. 1967–1970. Rapport de la Commission d'enquête sur la santé et le bien-être social. Québec, QC: Éditeur officiel du Québec. [Google Scholar]
- Clair Commission. 2000. Rapport et recommandations de la commission d'étude sur les services de santé et les services sociaux: Les solutions émergentes. Québec, QC: Gouvernement du Québec. [Google Scholar]
- Commissaire à la santé et au bien-être. 2016. Perceptions et expériences des médecins de première ligne: le Québec comparé. Retrieved January 18, 2018. <http://www.csbe.gouv.qc.ca/fileadmin/www/2015/CWF/CSBE_Rapport_CWF_2015.pdf>.
- Contandriopoulos D., Bilodeau H. 2008. “The Political Use of Poll Results about Public Support for a Privatized Healthcare System in Canada.” Health Policy 90(1): 104–12. 10.1016/j.healthpol.2008.08.001. [DOI] [PubMed] [Google Scholar]
- Contandriopoulos D., Brousselle A. 2010. “Reliable in Their Failure: An Analysis of Healthcare Reform Policies in Public Systems.” Health Policy 95(2–3): 144–52. 10.1016/j.healthpol.2009.11.018. [DOI] [PubMed] [Google Scholar]
- Contandriopoulos D., Hudon R., Martin E., Thompson D. 2007. “Tensions entre rationalité technique et intérêts politiques: l'exemple de la mise en œuvre de la Loi sur les agences de développement de réseaux locaux de services de santé et de services sociaux au Québec.” Canadian Public Administration 50(2): 193–217. 10.1111/j.1754-7121.2007.tb02011.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Contandriopoulos D., Perroux M., Brousselle A., Breton M. 2014. Analyse logique des effets prévisibles du projet de loi n°10 et des avenues d'intervention souhaitables. Retrieved January 18, 2018. <www.cssante.com/sites/www.cssante.com/files/memoirecontandriopoulosetal.pdf>.
- Creswell J.W., Plano Clark V.L. 2011. Designing and Conducting Mixed Methods Research (2nd ed.). Thousand Oaks, CA: Sage Publications. [Google Scholar]
- Dillman D.A., Smyth J.D., Christian L.M. 2009. Internet, Mail, and Mixed-Mode Surveys: The Tailored Design Method (3rd ed.). Hoboken, NJ: John Wiley & Sons Inc. [Google Scholar]
- Drummond D. 2012. Commission on the Reform of Ontario's Public Services: Public Services for Ontarians, a Path to Sustainability and Excellence. Toronto, ON: Ontario Ministry of Finance. [Google Scholar]
- Faulkner J., Laschinger H. 2008. “The Effects of Structural and Psychological Empowerment on Perceived Respect in Acute Care Nurses.” Journal of Nursing Management 16(2): 214–21. 10.1111/j.1365-2834.2007.00781.x. [DOI] [PubMed] [Google Scholar]
- Feachem R.G.A., Sekhri N.K., White K.L., Dixon J., Berwick D.M., Enthoven A.C. 2002. “Getting More for Their Dollar: A Comparison of the NHS with California's Kaiser Permanente.” BMJ 324(7330): 135–43. 10.1136/bmj.324.7330.13. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fyke K.J. 2001. Caring for Medicare: Sustaining a Quality System. Regina, SK: Saskatchewan Commission on Medicare. [Google Scholar]
- Gilbert A., Maheux B., Frappier J., Haley N. 2006. “Adolescent Care. Part 1: Are Family Physicians Caring for Adolescents' Mental Health?” Canadian Family Physician 52(11): 1440–41. [PMC free article] [PubMed] [Google Scholar]
- Haley N., Maheux B., Rivard M., Gervais A. 2000. “Lifestyle Health Risk Assessment. Do Recently Trained Family Physicians Do It Better?” Canadian Family Physician 46(8): 1609–16. [PMC free article] [PubMed] [Google Scholar]
- Ham C., York N., Sutch S., Shaw R. 2003. “Hospital Bed Utilisation in the NHS, Kaiser Permanente, and the US Medicare Programme: Analysis of Routine Data.” BMJ 327(7426): 1257. 10.1136/bmj.327.7426.1257. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Health Council of Canada. 2008. Strategic Plan 2008/2009–2012/2013: Taking the Pulse Toward Improved Health and Health Care in Canada. Toronto, ON: Health Council of Canada. [Google Scholar]
- Katz A., Glazier R.H., Vijayaraghavan J. 2009. The Health and Economic Consequences of Achieving a High-Quality Primary Healthcare System in Canada “Applying What Works in Canada: Closing the Gap”. Ottawa, ON: Canadian Health Services Research Foundation. [Google Scholar]
- Laschinger H.K.S., Wong C.A., Ritchie J., D'Amour D., Vincent L., Wilk P. et al. 2008. “A Profile of the Structure and Impact of Nursing Management in Canadian Hospitals.” Healthcare Quarterly 11(2): 85–94. 10.12927/hcq.2008.1959. [DOI] [PubMed] [Google Scholar]
- Laschinger S., Heather K., Finegan J., Wilk P. 2009. “Context Matters: The Impact of Unit Leadership and Empowerment on Nurses' Organizational Commitment.” Journal of Nursing Administration 39(5): 228–35. 10.1097/NNA.0b013e3181a23d2b. [DOI] [PubMed] [Google Scholar]
- Lehoux P., Richard L., Pineault R., Saint-Arnaud J. 2006. “Delivery of High-Tech Home Care by Hospital-Based Nursing Units in Quebec: Clinical and Technical Challenges.” Nursing Leadership 19(1): 44–55. [DOI] [PubMed] [Google Scholar]
- Lewis S. 2007. “Can a Learning-Disabled Nation Learn Healthcare Lessons from Abroad?” Healthcare Policy 3(2): 19–28. 10.12927/hcpol.2007.19388. [PMC free article] [PubMed] [Google Scholar]
- Lucas V., Laschinger H.K.S., Wong C.A. 2008. “The Impact of Emotional Intelligent Leadership on Staff Nurse Empowerment: The Moderating Effect of Span of Control.” Journal of Nursing Management 16(8): 964–73. 10.1111/j.1365-2834.2008.00856.x. [DOI] [PubMed] [Google Scholar]
- Maheux B., Gilbert A., Haley N., Frappier J. 2006. “Adolescent Care. Part 2: Communication and Referral Practices of Family Physicians Caring for Adolescents with Mental Health Problems.” Canadian Family Physician 52(11): 1442–43. [PMC free article] [PubMed] [Google Scholar]
- Makni H., O'Loughlin J.L., Tremblay M., Gervais A., Lacroix C., Dery V., Paradis G. 2002. “Smoking Prevention Counseling Practices of Montreal General Practitioners.” Archives of Pediatrics & Adolescent Medicine 156(12): 1263–67. 10.1001/archpedi.156.12.1263. [DOI] [PubMed] [Google Scholar]
- Mason D. 2016. “JAMA Forum: Partnering with Nurses to Transform Primary Care.” Retrieved January 16, 2018. <https://newsatjama.jama.com/2016/11/01/jama-forum-partnering-with-nurses-to-transform-primary-care/>. [DOI] [PubMed]
- McMurchy D. 2009. What Are the Critical Attributes and Benefits of a High-Quality Primary Healthcare System? Ottawa, ON: Canadian Health Services Research Foundation. [Google Scholar]
- Mechanic D. 2008. The Truth About Health Care: Why Reform Is Not Working in America (Critical Issues in Health and Medicine). Camden, UK: Rutgers University Press. [Google Scholar]
- National Physician Survey. 2007. Retrieved January 18, 2018. <http://www.nationalphysiciansurvey.ca/nps/home-e.asp>. College of Family Physicians of Canada (CFPC), Canadian Medical Association (CMA), Royal College of Physicians and Surgeons of Canada (RCPSC), Canadian Institute for Health Information (CIHI) and Health Canada.
- O'Loughlin J., Makni H., Tremblay M., Karp I. 2007. “Gender Differences among General Practitioners in Smoking Cessation Counseling Practices.” Preventive Medicine 45(2–3): 208–14. 10.1016/j.ypmed.2007.06.005. [DOI] [PubMed] [Google Scholar]
- Ontario HSRC. 2000. Looking Back, Looking Forward, Seven Points for Action. Retrieved July 17, 2018. <http://www.ontla.on.ca/library/repository/mon/1000/10286349.pdf>.
- Richard L., Pineault R., D'Amour D., Brodeur J.-M., Séguin L., Latour R., Labadie J.-F. 2005. “The Diversity of Prevention and Health Promotion Services Offered by Québec Community Health Centres: A Study of Infant and Toddler Programmes.” Health and Social Care in the Community 13(5): 399–408. 10.1111/j.1365-2524.2005.00576.x. [DOI] [PubMed] [Google Scholar]
- Robinson J.C., Shortell S.M., Li R., Casalino L.P., Rundall T. 2004. The Alignment and Blending of Payment Incentives within Physician Organizations Health Services Research 35(5): 1589–606. 10.1111/j.1475-6773.2004.00305.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rochon Commission. 1988. Rapport de la commission d'enquête sur les services de santé et les services sociaux. Québec, QC: Publications du Québec. [Google Scholar]
- Romanow R.J. 2002. Building on Values: The Future of Health Care in Canada – Final Report. Ottawa, ON: Commission on the Future of Health Care in Canada. [Google Scholar]
- Russell G., Johnston S., Thille P., Geneau R., Conklin J., Hogg W., Ikezawa Y. 2009. A Structure for Co-ordinating Canadian Primary Healthcare Research. Ottawa, ON: Canadian Health Services Research Foundation. [Google Scholar]
- Shortell S.M., Schmittdiel J., Wang M.C., Li R., Gillies R.R., Casalino L.P. 2005. “An Empirical Assessment of High-Performing Medical Groups: Results from a National Study.” Medical Care Research and Review 62(4): 407–34. 10.1177/1077558705277389. [DOI] [PubMed] [Google Scholar]
- Sicotte C., D'Amour D., Moreault M.-P. 2002. “Interdisciplinary Collaboration within Quebec Community Health Care Centres.” Social Science and Medicine 55(6): 991–1003. 10.1016/S0277-9536(01)00232-5. [DOI] [PubMed] [Google Scholar]
- Tremblay M., Cournoyer D., O'Loughlin J. 2009. “Do the Correlates of Smoking Cessation Counseling Differ across Health Professional Groups?” Nicotine & Tobacco Research 11(11): 1330–38. 10.1093/ntr/ntp142. [DOI] [PubMed] [Google Scholar]
- Québec. 2003. Act Respecting Local Health and Social Services Network Development Agencies. Chapter A-81. Retrieved July 13, 2018. <http://legisquebec.gouv.qc.ca/en/showdoc/cs/S-4.2>.
- Québec. 2015. Act to Modify the Organization and Governance of the Health and Social Services Network, in Particular by Abolishing the Regional Agencies. Chapter O-7.2. Retrieved July 13, 2018. <http://legisquebec.gouv.qc.ca/en/ShowDoc/cs/O-7.2>


