Introduction
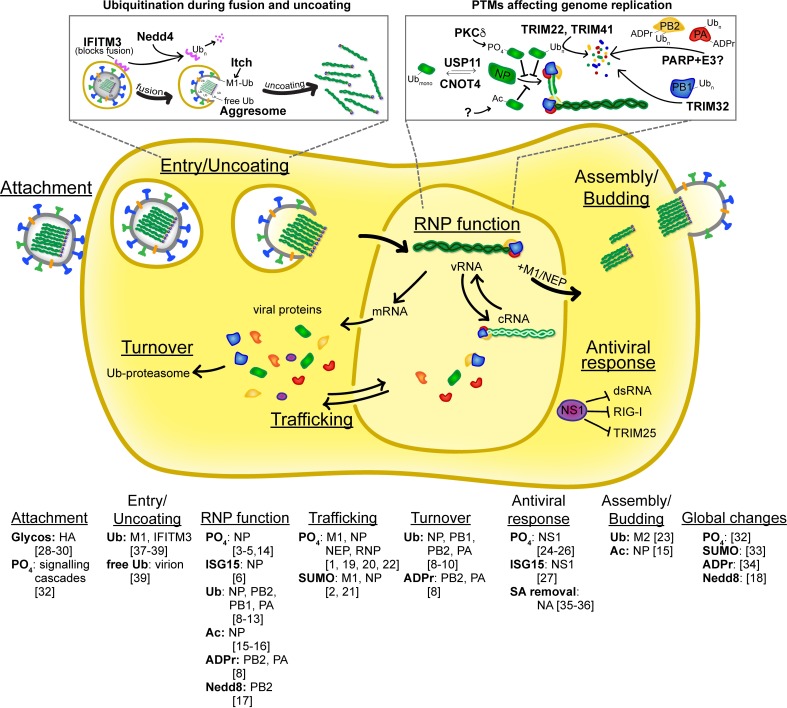
Precise coordination of cellular processes requires prompt specification of protein function in response to various stimuli. This specification includes regulating protein abundance, localization, catalysis, and binding. Post-translational modifications (PTMs) provide cells the plasticity for dynamic and reversible control of protein function. Viral infections provide an exciting lens through which to study PTMs, since PTMs contribute to both cellular responses to infection and viral hijacking of the host. PTMs enhance the already multifunctional nature of viral proteins and offer another level of functional diversity within limited genetic space. Influenza virus protein functions are fine-tuned by diverse types of PTMs, including phosphorylation, ubiquitination, SUMOylation, neddylation, ISGylation, glycosylation, ADP-ribosylation, palmitoylation, and acetylation. All of the major viral proteins are subject to at least one type of PTM. Additionally, as influenza viruses encode no known protein-modifying enzymes, all of these PTMs are mediated by host machinery. Here, we use influenza virus and its proteins as exemplars for how PTMs impact virus replication (Fig 1).
Fig 1. Post-translation control of key steps during the influenza virus replication cycle.
Simplified diagram of key steps during the influenza virus life cycle highlighting events that are regulated by PTMs to viral or host proteins. The specific modifications, target proteins, and references are listed for each step. Two processes are highlighted in depth; these examples were chosen because the PTMs and causative host enzymes are known and the modifications have discrete effects on replication. In addition, a large number of PTMs have been identified on viral proteins, but no discrete function has yet been assigned [14]. Ac, acetylation; ADPr, ADP-ribosylation; cRNA, plus-sense genomic RNA; dsRNA, double-stranded RNA; Glycos., N-linked glycosylation; ISG15, ISGylation; Nedd8, neddylation; NP, nucleoprotein; NS1, nonstructural protein 1; PO4, phosphorylation; PTM, post-translational modification; RNP, ribonucleoprotein complex; SA, sialic acid; SUMO, SUMOylation; Ub, ubiquitin and ubiquitination; vRNA, minus-sense genomic RNA.
Do PTMs regulate the function of the influenza ribonucleoprotein complex?
Influenza virus transcribes and replicates its negative single-stranded RNA genome via a virally encoded RNA-dependent RNA polymerase (RdRp). This is performed by the viral ribonucleoprotein complex (RNP), containing genomic RNA encapsidated by the viral nucleoprotein (NP) and bound at both termini by a single heterotrimeric RdRp. While all components of the RNP are post-translationally modified, mechanistic consequences of NP PTMs have been particularly well described. During infection, newly made NP traffics from the cytoplasm into the nucleus and then back to the cytoplasm as either free NP or assembled RNPs. NP trafficking is regulated by both phosphorylation and SUMOylation [1,2]. Phosphorylation of NP at its N-terminal nuclear localization signal inhibits interaction with nuclear import factors, whereas internal NP phosphorylation inhibits interactions with nuclear export factors [1]. SUMOylation appears to be important for nuclear retention, as mutant NPs lacking SUMOylation sites are prematurely exported to the cytoplasm [2]. Viruses encoding NP SUMO-site mutants exhibit profound defects in replication and rapidly revert to wild type.
Nuclear NP oligomerizes along the length of newly synthesized genomic RNA. This process is negatively regulated for both influenza A and B viruses by NP phosphorylation at conserved sites on apposing sides of the homotypic interface [3,4]. Preventing phosphorylation by mutagenesis results in hyperoligomerization of NP, and deleting the responsible host kinase causes severe defects in RNP assembly, function, and viral replication; these data suggest that phosphorylation at these positions is critical for incorporation of NP into nascent RNPs [5]. NP oligomerization during influenza B virus infection is also inhibited by ISGylation, but in this case, the PTM is a possible antiviral response [6].
All RNP components are ubiquitinated, and perturbing global ubiquitination impairs RNP function [7]. In certain contexts, ubiquitination results in protein turnover, especially when polyubiquitin chains are appended [8–11] (Fig 1). However, ubiquitination also plays a regulatory role during infection. NP is dynamically monoubiquitinated and deubiquitinated at lysine 184 (K184) [12,13]. This modification may regulate interaction of NP with genomic RNA to facilitate genome replication. Thus, ubiquitination of RNP proteins plays dual roles, both inhibiting and promoting replication.
Functions of additional RNP PTMs are less well defined. Phosphorylation of the three polymerase subunits—PB1, PB2, and PA—has unknown consequences [14]. PB1, PA, and NP undergo N-terminal acetylation with no specific assigned functions [14]. NP is also acetylated on internal lysine residues [15,16]. Mimicking NP acetylation disrupts the ability of NP to stabilize replication intermediates. Notably, NP is acetylated on K184, the same residue that is monoubiquitinated, suggesting potential cross-talk between different PTMs. The polymerase subunits PB2 and PA are ADP-ribosylated [8]. ADP-ribosylation promotes their ubiquitination and subsequent degradation, providing another example of PTM cross-talk. In an apparent paradox, neddylation of PB2 blocks viral replication [17], yet inhibition of the neddylation pathway also results in poor replication [18]. In sum, RNP PTMs serve both as tunable ways to regulate polymerase function and as antiviral responses that attempt to block replication.
What do PTMs do for other influenza virus proteins?
In addition to regulating RNPs, PTMs impact genome trafficking and evasion of antiviral responses. RNPs assemble in the nucleus and are exported to the cytoplasm, where they traffic to sites of assembly and budding. Export requires the viral matrix protein (M1) and the nuclear export protein (NEP). Current data support a daisy-chain model in which the RNP interacts with M1, M1 interacts with NEP, and NEP interacts with the cellular export machinery. Phosphorylation of M1 enhances import [19]. M1 phosphoablative mutants remain in the cytoplasm, whereas M1 phosphomimetic mutants or a temperature-sensitive phosphorylation hypermorph are retained in the nucleus [19,20]. All of these mutants exhibit replication defects. Formation of the RNP-M1-NEP daisy chain and its export are affected by M1 SUMOylation and possibly phosphorylation on NEP [14,21]. M1 SUMO-site mutants exhibit decreased interaction with RNPs, resulting in vRNA nuclear export defects and reduced viral titers. Phosphorylation of NEP at several conserved residues adjacent to its nuclear export signal may also control export, although functional analyses indicate that these sites are not essential regulators of NEP function [22]. Whether M1 phosphorylation is reversed concomitant with SUMOylation and nuclear export remains to be determined, but it could represent a system for dynamic control of M1 localization throughout infection. Once exported, RNPs are trafficked to the plasma membrane, where ubiquitination of the viral membrane protein M2 plays a key role in particle assembly and release [23].
PTMs are important for the two main viral proteins that engage the host immune response: the nonstructural protein 1 (NS1) and hemagglutinin (HA). NS1 is the canonical antagonist of innate immune responses. NS1 sequesters dsRNA to avoid detection by host sensors and also antagonizes and directly binds these sensors, including RIG-I and TRIM25. Phosphorylation and ISGylation of NS1 disrupt protein–RNA interactions, while phosphorylation also disrupts protein–protein interactions [24–27]. In this case, the host utilizes PTMs to disarm viral countermeasures. PTMs on the viral glycoprotein HA, however, are exploited by influenza virus to evade immune detection and increase viral spread. The viral glycoprotein HA mediates attachment and entry. HA is the immunodominant viral protein that elicits most of the humoral response from infection. Glycosylation of viral envelope proteins is a well-described mode of immune evasion, and gain or loss of specific N-linked glycosylation sites helps shield influenza HA from antibody recognition and neutralization [28]. HA glycosylation has more recently been shown to increase virulence and fitness after immune escape [29,30]. PTMs of influenza virus proteins vary by host species as well, with potential impacts on replication and pathogenicity. For example, recent data indicate that lower vaccine efficacy results in part from differential HA glycosylation that occurs when viruses are grown in mammalian or avian hosts [31].
Does influenza virus exploit PTMs to modulate host protein function?
Host cell reprograming during infection often focuses on wholesale changes in gene transcription, such as the induction of interferon-stimulated genes. Remodeling of the host cell might be more broadly considered to also include changes in protein degradation, subcellular localization, and differential activation of cell signaling cascades. Cellular proteins and their PTMs regulate reprogramming events, a feature exploited by influenza virus. Influenza infection results in global changes in PTMs of the host proteome, including triggering kinase cascades [32], reprogramming of cellular SUMOylation [33], stimulation of ADP-ribosylation [34], and activation of the neddylation pathway [18]. PTMs themselves can also be modified. The viral neuraminidase (NA) mediates release of new viral particles by cleaving sialic acid from host glycans. Interestingly, NA removes sialic acid moieties from viral and cellular proteins, including the host cytokine TGF-β, leading to its activation as part of a protective response to infection [35,36].
Influenza viruses indirectly utilize PTMs to co-opt cellular machinery. The ubiquitin machinery plays key roles at multiple steps during entry (Fig 1). Infection-triggered cascades promote ubiquitination of M1 to facilitate release of the incoming virion [37]. Influenza virus entry also relies on the cellular E3 ligase NEDD4 to ubiquitinate and reduce levels of the entry inhibitor IFITM3 [38]. Influenza virions contain nonconjugated ubiquitin chains, which upon entry direct incoming viral cores to the cellular aggresome, where they are efficiently uncoated and associated with the microtubule network for nuclear import of released RNPs [39]. Therefore, the host’s PTM machinery modifies both viral and host proteins, creating a cellular milieu conducive for replication.
Given what we know about PTMs and influenza virus, what don’t we yet know?
Studies of PTMs have shed light on our understanding of the influenza replication cycle while also raising exciting new questions. Whereas PTMs have been mapped to all viral proteins—with most being modified at multiple sites by diverse PTMs—the host effectors and functional outcomes of most PTMs remain unknown. While some of the PTMs have clearly defined activities (see above), perhaps the largest question is whether all of the modifications discovered so far have functional impacts during infection. Even if all of the PTMs are functionally important, it is possible that some modifications are required only under discrete circumstances but dispensable at other times, making this a more complicated question to address. We also have little appreciation for how these modifications change temporally during infection. It has been proposed that dynamic PTMs could dictate progression of the replication cycle. Indeed, it is the reversible nature of these PTMs that make them attractive mechanisms for dynamic regulation. Yet, how specific PTMs are orchestrated during influenza virus infection and whether this serves to temporally order viral processes has only begun to be explored.
Viral proteins are notoriously multifunctional, and understanding how the varied tasks are separated remains elusive. An exciting possibility is that PTMs parse these different functions by establishing distinct populations of the same viral protein. For example, the separation of viral transcription from genome replication during influenza virus infection is incompletely understood. Viral proteins, small viral RNAs, and various host proteins have all been implicated in biasing polymerase output. The proteins of the viral RNP are modified by multiple PTMs, and PTMs could provide additional mechanisms to establish discrete populations of transcribing versus replicating RNPs.
The roles of PTMs have generally been characterized in isolation, raising the question of how these modifications work in concert. Moreover, since certain amino acid residues can be subject to many different PTMs, a single residue may be competitively or differentially modified over time. Several examples of PTM cross-talk on influenza virus proteins have already been identified [8,12,16], suggesting additional levels of regulatory complexity. Additionally, continuing advances in detection and characterization of PTMs will undoubtedly uncover new facets of influenza virus biology [40]. In summary, influenza viruses utilize PTMs to modulate multiple steps throughout the viral replication cycle. Infection induces global changes in PTMs as well as targeted modifications on specific viral proteins. While many PTMs support viral infection, others are part of antiviral responses. How PTMs change across infection for both host and viral proteins, how PTMs work in concert during replication, and how they impact pathogenicity and host range are exciting and open questions.
Acknowledgments
We thank members of the Mehle lab for critical reading of the manuscript and V. Tran for graphical assistance. We apologize to our colleagues whose work could not be cited because of space restraints.
Funding Statement
ARD is funded by T32AI078985. AM is funded by R01AI125271 and a Shaw scientist award from the Greater Milwaukee Foundation. AM holds an Investigators in the Pathogenesis of Infectious Disease Award from the Burroughs Wellcome Fund. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
References
- 1.Zheng W, Li J, Wang S, Cao S, Jiang J, Chen C, et al. Phosphorylation controls the nuclear-cytoplasmic shuttling of influenza A virus nucleoprotein. J Virol. 2015;89(11): 5822–5834. 10.1128/JVI.00015-15 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Han Q, Chang C, Li L, Klenk C, Cheng J, Chen Y, et al. Sumoylation of influenza A virus nucleoprotein is essential for intracellular trafficking and virus growth. J Virol. 2014;88: 9379–90. 10.1128/JVI.00509-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Turrell L, Hutchinson EC, Vreede FT, Fodor E. Regulation of influenza A virus nucleoprotein oligomerization by phosphorylation. J Virol. 2015;89: 1452–5. 10.1128/JVI.02332-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Mondal A, Potts GK, Dawson AR, Coon JJ, Mehle A. Phosphorylation at the homotypic interface regulates nucleoprotein oligomerization and assembly of the influenza virus replication machinery. PLoS Pathog. 2015;11: e1004826 10.1371/journal.ppat.1004826 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Mondal A, Dawson AR, Potts GK, Freiberger EC, Baker SF, Moser LA, et al. Influenza virus recruits host protein kinase C to control assembly and activity of its replication machinery. Elife. 2017;6: e26910 10.7554/eLife.26910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhao C, Sridharan H, Chen R, Baker DP, Wang S, Krug RM. Influenza B virus non-structural protein 1 counteracts ISG15 antiviral activity by sequestering ISGylated viral proteins. Nat Commun. 2016;7: 12754 10.1038/ncomms12754 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Kirui J, Mondal A, Mehle A. Ubiquitination up-regulates influenza virus polymerase function. J Virol. 2016;90: 10906–10914. 10.1128/JVI.01829-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Liu C-H, Zhou L, Chen G, Krug RM. Battle between influenza A virus and a newly identified antiviral activity of the PARP-containing ZAPL protein. Proc Natl Acad Sci U S A. 2015;112: 14048–53. 10.1073/pnas.1509745112 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Fu B, Wang L, Ding H, Schwamborn JC, Li S, Dorf ME. TRIM32 Senses and Restricts Influenza A Virus by Ubiquitination of PB1 Polymerase. PLoS Pathog. 2015/06/10. 2015;11: e1004960 10.1371/journal.ppat.1004960 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Di Pietro A, Kajaste-Rudnitski A, Oteiza A, Nicora L, Towers GJ, Mechti N, et al. TRIM22 Inhibits Influenza A Virus Infection by Targeting the Viral Nucleoprotein for Degradation. J Virol. 2013/02/15. 2013;87: 4523–4533. 10.1128/JVI.02548-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Patil G, Zhao M, Song K, Hao W, Bouchereau D, Wang L, et al. TRIM41-Mediated Ubiquitination of Nucleoprotein Limits Influenza A Virus Infection. J Virol. 2018; e00905–18. 10.1128/JVI.00905-18 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Liao T-L, Wu C-Y, Su W-C, Jeng K-S, Lai MMC. Ubiquitination and deubiquitination of NP protein regulates influenza A virus RNA replication. EMBO J. 2010;29: 3879–3890. 10.1038/emboj.2010.250 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Lin Y-C, Jeng K-S, Lai MMC. CNOT4-Mediated Ubiquitination of Influenza A Virus Nucleoprotein Promotes Viral RNA Replication. MBio. 2017;8: e00597–17. 10.1128/mBio.00597-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Hutchinson EC, Denham EM, Thomas B, Trudgian DC, Hester SS, Ridlova G, et al. Mapping the Phosphoproteome of Influenza A and B Viruses by Mass Spectrometry. PLoS Pathog. 2012;8(11): e1002993 10.1371/journal.ppat.1002993 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Giese S, Ciminski K, Bolte H, Moreira ÉA, Lakdawala S, Hu Z, et al. Role of influenza A virus NP acetylation on viral growth and replication. Nat Commun. 2017;8: 1259 10.1038/s41467-017-01112-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Hatakeyama D, Shoji M, Yamayoshi S, Yoh R, Ohmi N, Takenaka S, et al. Influenza A virus nucleoprotein is acetylated by histone acetyltransferases PCAF and GCN5. J Biol Chem. 2018;293: 7126–7138. 10.1074/jbc.RA117.001683 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Zhang T, Ye Z, Yang X, Qin Y, Hu Y, Tong X, et al. NEDDylation of PB2 Reduces Its Stability and Blocks the Replication of Influenza A Virus. Sci Rep. 2017;7: 43691 10.1038/srep43691 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Sun H, Yao W, Wang K, Qian Y, Chen H, Jung Y-S. Inhibition of neddylation pathway represses influenza virus replication and pro-inflammatory responses. Virology. 2018;514: 230–239. 10.1016/j.virol.2017.11.004 [DOI] [PubMed] [Google Scholar]
- 19.Wang S, Zhao Z, Bi Y, Sun L, Liu X, Liu W. Tyrosine 132 phosphorylation of influenza A virus M1 protein is crucial for virus replication by controlling the nuclear import of M1. J Virol. 2013;87: 6182–91. 10.1128/JVI.03024-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Whittaker G, Kemler I, Helenius A. Hyperphosphorylation of mutant influenza virus matrix protein, M1, causes its retention in the nucleus. J Virol. 1995;69: 439–45. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Wu C-Y, Jeng K-S, Lai MM-C. The SUMOylation of matrix protein M1 modulates the assembly and morphogenesis of influenza A virus. J Virol. 2011;85: 6618–28. 10.1128/JVI.02401-10 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Reuther P, Giese S, Gotz V, Riegger D, Schwemmle M. Phosphorylation of Highly Conserved Serine Residues in the Influenza A Virus Nuclear Export Protein NEP Plays a Minor Role in Viral Growth in Human Cells and Mice. J Virol. 2014;88: 7668–7673. 10.1128/JVI.00854-14 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Su W-C, Yu W-Y, Huang S-H, Lai MMC. Ubiquitination of the Cytoplasmic Domain of Influenza A Virus M2 Protein Is Crucial for Production of Infectious Virus Particles. J Virol. 2018;92: e01972–17. 10.1128/JVI.01972-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Zheng W, Cao S, Chen C, Li J, Zhang S, Jiang J, et al. Threonine 80 phosphorylation of non-structural protein 1 regulates the replication of influenza A virus by reducing the binding affinity with RIG-I. Cell Microbiol. 2017;19: e12643 10.1111/cmi.12643 [DOI] [PubMed] [Google Scholar]
- 25.Kathum OA, Schräder T, Anhlan D, Nordhoff C, Liedmann S, Pande A, et al. Phosphorylation of influenza A virus NS1 protein at threonine 49 suppresses its interferon antagonistic activity. Cell Microbiol. 2016;18: 784–791. 10.1111/cmi.12559 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Hsiang T-Y, Zhou L, Krug RM. Roles of the Phosphorylation of Specific Serines and Threonines in the NS1 Protein of Human Influenza A Viruses. J Virol. 2012;86: 10370–10376. 10.1128/JVI.00732-12 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Zhao C, Hsiang T-Y, Kuo R-L, Krug RM. ISG15 conjugation system targets the viral NS1 protein in influenza A virus-infected cells. Proc Natl Acad Sci. 2010;107: 2253–2258. 10.1073/pnas.0909144107 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Skehel JJ, Stevens DJ, Daniels RS, Douglas AR, Knossow M, Wilson IA, et al. A carbohydrate side chain on hemagglutinins of Hong Kong influenza viruses inhibits recognition by a monoclonal antibody. Proc Natl Acad Sci U S A. 1984;81: 1779–1783. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Zhao D, Liang L, Wang S, Nakao T, Li Y, Liu L, et al. Glycosylation of the Hemagglutinin Protein of H5N1 Influenza Virus Increases Its Virulence in Mice by Exacerbating the Host Immune Response. J Virol. 2017;91: e02215–16. 10.1128/JVI.02215-16 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Kosik I, Ince WL, Gentles LE, Oler AJ, Kosikova M, Angel M, et al. Influenza A virus hemagglutinin glycosylation compensates for antibody escape fitness costs. PLoS Pathog. 2018;14: e1006796 10.1371/journal.ppat.1006796 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Zost SJ, Parkhouse K, Gumina ME, Kim K, Diaz Perez S, Wilson PC, et al. Contemporary H3N2 influenza viruses have a glycosylation site that alters binding of antibodies elicited by egg-adapted vaccine strains. Proc Natl Acad Sci. 2017;114: 12578–12583. 10.1073/pnas.1712377114 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Planz O. Development of cellular signaling pathway inhibitors as new antivirals against influenza. Antiviral Res. 2013;98: 457–68. 10.1016/j.antiviral.2013.04.008 [DOI] [PubMed] [Google Scholar]
- 33.Domingues P, Golebiowski F, Tatham MH, Lopes AM, Taggart A, Hay RT, et al. Global Reprogramming of Host SUMOylation during Influenza Virus Infection. Cell Rep. 2015;13: 1467–1480. 10.1016/j.celrep.2015.10.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Seo GJ, Kincaid RP, Phanaksri T, Burke JM, Pare JM, Cox JE, et al. Reciprocal inhibition between intracellular antiviral signaling and the RNAi machinery in mammalian cells. Cell Host Microbe. 2013/10/01. 2013;14: 435–445. 10.1016/j.chom.2013.09.002 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Carlson CM, Turpin EA, Moser LA, O’Brien KB, Cline TD, Jones JC, et al. Transforming Growth Factor-β: Activation by Neuraminidase and Role in Highly Pathogenic H5N1 Influenza Pathogenesis. Fouchier RAM, editor. PLoS Pathog. 2010;6: e1001136 10.1371/journal.ppat.1001136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Schultz-Cherry S, Hinshaw VS. Influenza virus neuraminidase activates latent transforming growth factor beta. J Virol. 1996;70: 8624–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Su W-C, Chen Y-C, Tseng C-H, Hsu PW-C, Tung K-F, Jeng K-S, et al. Pooled RNAi screen identifies ubiquitin ligase Itch as crucial for influenza A virus release from the endosome during virus entry. Proc Natl Acad Sci. 2013;110: 17516–17521. 10.1073/pnas.1312374110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Chesarino NM, McMichael TM, Yount JS. E3 Ubiquitin Ligase NEDD4 Promotes Influenza Virus Infection by Decreasing Levels of the Antiviral Protein IFITM3. PLoS Pathog. 2015;11: e1005095 10.1371/journal.ppat.1005095 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Banerjee I, Miyake Y, Nobs SP, Schneider C, Horvath P, Kopf M, et al. Influenza A virus uses the aggresome processing machinery for host cell entry. Science (80-). 2014;346: 473–477. 10.1126/science.1257037 [DOI] [PubMed] [Google Scholar]
- 40.Ke M, Shen H, Wang L, Luo S, Lin L, Yang J, et al. Identification, Quantification, and Site Localization of Protein Posttranslational Modifications via Mass Spectrometry-Based Proteomics. Advances in experimental medicine and biology. 2016. pp. 345–382. 10.1007/978-3-319-41448-5_17 [DOI] [PubMed] [Google Scholar]