Abstract
Backgrounds
Self-efficacy plays an important role in pulmonary rehabilitation, but it is still unknown which factors exert their effects on postsurgical rehabilitation self-efficacy among non-small cell lung cancer (NSCLC) patients. This study aims to assess relationships among physical function, social factors, psychological factors, quality of life (QOL) and self-efficacy, and the effects of these variables on self-efficacy among NSCLC patients.
Methods
A cross-sectional survey was administered to 238 postsurgical NSCLC patients (response rate 95.2%) at five tertiary hospitals in Fuzhou, China. the participants completed a pack of questionnaires. Structural equation modeling (SEM) was conducted to test the hypothetical model.
Results
The SEM results supported the hypothesized structural model (χ2/df = 1.511, p>0.05). The final model showed that confrontation coping, subjective well-being (SWB), social support, psychological growth (PTG) and anxiety and depression can be directly related to self-efficacy (coefficient = 0.335, coefficient = 0.288, coefficient = 0.150, coefficient = 0.024, and coefficient = -0.004, respectively, p<0.01). Confrontation coping also had indirect effect via SWB (coefficient = 0.085, p<0.01), which had indirect connection via PTG (coefficient = 0.005, p<0.01). Social support and anxiety and depression had indirect pathways as well. As expected, self-efficacy directly affected the quality of life.
Conclusions
This study suggests that higher confrontation coping style, SWB, social support, and PTG and lower anxiety and depression levels could effectively enhance their self-efficacy and consequently, improve QOL. These findings may help develop an intervention aimed at enhancing self-efficacy for this patient population.
Introduction
Lung cancer is a leading cause of cancer mortality and morbidity worldwide [1]. In China, the incidence of lung cancer has markedly increased over the last few decades and is predicted to be 1 million per year by 2025 [2,3]. Presently, surgery remains the primary treatment for lung cancer [4]. Pulmonary rehabilitation management was found to effectively reduce the symptom burden and side effects after pneumonectomy, such as pain [5], fatigue [6], anxiety and depression [7], and increase lung function [8,9] and the quality of life (QOL) [10,11].
Self-efficacy plays an important role in pulmonary rehabilitation [12]. Signe et al. demonstrated that self-efficacy was one of the predictors of health status improvement and overall QOL in pulmonary rehabilitation [13]. Previous studies have investigated the relationship between self-efficacy and numerous cancer-related factors, including socio-demographic and clinical characteristics, physical function, psychological distress (e.g., anxiety and depression), psychological growth (i.e. post-traumatic growth, PTG), health behaviors and QOL [4,14–16]. However, the pathway or mechanism associating self-efficacy with physical or psychological health outcomes on cancer patients is not well understood. Furthermore, these previous studies have demonstrated such relationships through the use of self-efficacy as a mediator or independent variable, not as a dependent variable. A structural equation modeling (SEM), which analyzes both direct interrelationships of independent variables and their indirect effects through other variables [17], may help clarify the role of self-efficacy in lung cancer patients.
According to the definition set forth by Bandura, self-efficacy is a belief in one’s ability to organize and execute the course of action required to produce a specific outcome, usually specific to a given task or domain [18]. Self-efficacy for coping and management may change depending on the type of cancer and phases of care from diagnosis, to treatment and survivorship [19]. So far, majority of the studies looked at breast and colorectal cancer and few focused on lung cancer, especially non-small cell (NSCLC) to identify the relationships and interactions between self-efficacy and physical function, social factors, psychological factors and QOL among NSCLC patients during post-op rehabilitation.
Given the high disease burden of lung cancer in China, and the importance of self-efficacy in pulmonary rehabilitation, it is imperative to identify pathways through which factors exert their effects on postsurgical rehabilitation self-efficacy, which can then be applied to design integrated interventions to enhance self-efficacy and QOL. The aim of this study was to use SEM to determine factors that may affect self-efficacy in postsurgical NSCLC patients. The following hypotheses are proposed and tested to generate a behavioral relationship model:
Pain, poor sleep condition, unproductive coping strategies (fear-avoidance and acceptance-resignation), and anxiety and depression will have a direct negative relationship to self-efficacy.
Confrontation coping, social support, SWB, and PTG will be have a direct positively relationship to self-efficacy.
Self-efficacy will have a direct positive relationship with QOL.
Methods
Study design
From March 2015 to August 2015, a cross-sectional study was conducted in the departments of cardiothoracic surgery at five tertiary hospitals in Fuzhou, Fujian province, China. Two hundred fifty patients who satisfied the following inclusion criteria were enrolled: a) able to read and understand Chinese, b) age ≥18, c) have undergone lung resection for suspected or confirmed lung cancer, d) Karnofsky performance status score ≥60%. Participants with cognitive deficits, severe postoperative complications, metastasis or other malignancies were excluded. A sample size greater than 200 was required for SEM analysis [20,21]. Clinical data were collected from the medical records and all participants filled out a set of structured questionnaires (see below). Before survey, all eligible participants included in this study were given verbal informed consent. This study was approved by the Institutional Review Board of Central South University (number: 2013017). (S1 Fig and S1 File)
Measurements
Demographic and clinical characteristics
The demographic data collected included age, gender, marital status, place of residence, educational level, religion, family per capita monthly income (Yuan, RMB), employment status, medical insurance, smoking status. Clinical information collected from the chart review included surgical site, cancer stage, histological type, type of surgery, length of hospital stay and comorbidities.
Postoperative rehabilitation self-efficacy
The self-efficacy of postoperative rehabilitation management was measured using the Self-Efficacy Scale for Postoperative Rehabilitation Management of Lung Cancer (SESPRM-LC) [4]. The 27-item SESPRM-LC with six sub-domains was rated on a five-point Likert scale (1 = not at all confident to 5 = completely confident). The total scores of SESPRM-LC ranged from 27 to 135, with higher scores indicating greater self-efficacy. The reliability and validity have demonstrated sound psychometrics in NSCLC postsurgical patients through the classical test theory and item response theory methods [4].
Quality of life (QOL)
QOL was assessed using the Functional Assessment of Cancer Therapy–Lung scale (FACT-L, Version 4) [22], which has been widely used in lung cancer studies with adequate psychometric properties. FACT-L contains 36 items covering the factors of well-being in the physical, functional, emotional, social/family realms, and lung cancer subscale. All FACT-L items are rated on a 5-point Likert-type scale ranging from 0 (not at all) to 4 (very much). Higher scores represent better quality of life or fewer symptoms[22]. In this study, the Cronbach’s α coefficients for the five subscales ranged from 0.543 to 0.932, and for the overall scale 0.896.
Anxiety and depression
Anxiety and depression were measured by the Chinese version of the Hospital Anxiety and Depression scale (HADS)[23]. The HADS contains 14 items for anxiety and depression. Each subscale is scored from 0 to 21, with higher scores indicating greater distress. This score is classified as no anxiety or depression (0–7), borderline (8–10), and severely anxious/depressed (11–21). The Chinese version of HADS has been validated [23]. In this study, the Cronbach’s α coefficients for the five subscales ranged from 0.686to 0.750, and for the overall scale 0.817.
Social support
Social support was measured by the Multidimensional Scale of Perceived Social Support(MSPSS)[24,25]. The 12-item MSPSS contains 3 factors, the perceived social support from family, friends, and significant others. The scale employed a 7-point rating scale ranging from 1 (Very strongly disagree) to 7 (Very strongly agree). In this study, the Cronbach's α coefficient was 0.907 for overall scale.
Subjective well-being (SWB)
SWB was assessed by the Simplified Face Scale. This very brief, pictorial scale of mood uses a sequence of seven faces and does not require reading literacy [26,27]. The seven faces range from happy and smiling to sad and crying. In this study, the Cronbach's α coefficient was 0.891 for overall scale.
Coping
Coping styles were measured with the Medical Coping Modes Questionnaire (MCMQ) [28,29]. A 19-item MCMQ was used to evaluate patients’ cognitive-behavioral and illness-related coping strategies, including confrontation, fear-avoidance and acceptance-resignation. The scale is scored on a four-point Likert scale ranging from 1 (never) to 4 (very much). In this study, the Cronbach's α coefficient of overall scale was 0.762.
Sleep condition
Sleep condition was measured by Athens Insomnia Scale(AIS) [30]. The AIS is a self-assessment psychometric instrument designed for quantifying sleep difficulty. It consists of 8 items measured on numeric scale (0 “no problem” to 3 “did not sleep at all”). The total score is classified as no sleep disorder (<4), suspected sleep disorder (4–6), and insomnia (>6). In this study, the Cronbach's α coefficient was 0.848.
Pain
Pain was measured by the visual analogue scale(VAS). which was considered the most accurate and reproducible scale of measuring the intensity of pain[31]. VAS was a numeric scale based on 11 points (0 “no pain” to 10 “the most intense and unbearable pain”). The psychometric properties were verified by prior studies [32].
PTG
PTG was measured by the Posttraumatic Growth Inventory (PTGI) [33]. The Chinese version of PTGI is a 21-item self-reported inventory with five domains, which are relation to others, new possibilities, personal strengths, spiritual change, and appreciation of life. The questionnaire uses a six-point scale (0 “I did not experience this change after the traumatic event” to 5 “I experienced this change to a very great degree after the traumatic event”). Higher scores implied greater posttraumatic growth. The Chinese version of PTGI was verified previously[34].In this study, the Cronbach’s α ranged from 0.701 to 0.850 for the five domains, and 0.926 for the overall score.
Statistical analysis
Data analysis was conduct using SPSS 17.0 (IBM, Chicago, IL,USA) and Mplus 6.1. Missing data were managed by expectation maximization. p<0.05 was considered significant. Descriptive statistics were calculated to estimate the frequencies, means, and standard deviations of the study variables. Correlations among the factors were examined by Pearson’s correlation analysis and stepwise linear regression analysis. In this study, the data meet the assumptions of normality (one-sample kolmogrov-smirnov test was no statistical significance). SEM with a maximum likelihood (ML) estimation method was used to evaluate the fit of the hypothesized theoretical model based on the following criteria [35]: Normed chi-square (χ2/df, 1.0–3.0, p>0.05), Root Mean Squared Error of Approximation (RMSEA<0.08), Comparative Fit Index (CFI,>0.9), Normed Fit Index (NFI, >0.9), and Goodness of Fit Index (GFI, >0.9). Hypotheses regarding the structural relationships of the constructs in the final model were evaluated using the magnitude of path coefficients (standardized coefficient) and their significance. The bootstrap method was applied for the indirect effects in the hypothesized model (repeated 1000 times) using ML estimation.
Results
Characteristics of the participants
Of the 250 eligible patients recruited, 12 were excluded from analysis because of missing data > 30%. Four questionnaires contained missing data to a lesser degree and were included in the analysis. Final sample size was 238 patients (effective response rate 95.2%). Demographic and clinical characteristics of the participants are shown in Table 1. The participants’ age range was 32 to 68 years, and the average age was 58.37±9.94 years. Three-quarters were male. The length of hospital stay was 11.51±8.01 days. Vast majority (96%) of the participants were married.
Table 1. Demographic and clinical characteristics of study participants(N = 238).
| Variable | N(%) | Variable | N(%) |
|---|---|---|---|
| Demographic data | Clinical characteristics | ||
| Age (years) | Cancer stage (%) | ||
| ≤34 | 7(3.0%) | In situ | 12(5.0%) |
| 35~59 | 114(48.0%) | I (Ia+Ib) | 86(36.1%) |
| >60 | 117(49.0%) | Ⅱ(Ⅱa+Ⅱb) | 100(42.1%) |
| Gender (%) | Ⅲ(Ⅲa+Ⅲb) | 40(16.8%) | |
| Male | 178(75.0%) | Histologic type(%) | |
| Female | 60(25.0%) | Squamous | 92(38.6%) |
| Place of residence(%) | Adenocarcinoma | 131(55.0%) | |
| Urban | 94(39.5%) | Adenosquamous | 9(3.8%) |
| Suburban | 32(13.4%) | Bronchoalveolar | 3(1.3%) |
| Rural | 112(47.1%) | Large undifferentiated | 3(1.3%) |
| Religion (%) | Type of surgery (%) | ||
| Yes | 117(49.2%) | Thoracotomy | 86(36.1%) |
| No | 121(50.8%) | VATSa | 152(63.9%) |
| Educational level(%) | Comorbidities | ||
| Less than high school degree | 86(36.2%) | No | 140(58.8%) |
| High school degree (including technical training) | 100(42.0%) | Yes | 98(41.2%) |
| Bachelor’s degree or higher | 52(21.8%) | Surgical site | |
| Family per capita monthly income (Yuan, RMB) | Left | 100(42.0%) | |
| <1000 | 14(5.9%) | Right | 134(56.3%) |
| 1000~2999 | 90(37.8%) | Both | 4(1.7%) |
| 3000~4999 | 70(29.4%) | Re-admission | |
| 5000~ | 64(26.9%) | Yes | 56(23.5%) |
| Employment status | No | 182(76.5%) | |
| Full-time Employment | 37(15.5%) | ||
| Unemployment | 11(4.6%) | ||
| Retired | 82(34.5%) | ||
| Farmer | 92(38.7%) | ||
| Other | 16(6.7%) | ||
| Medical insurance(%) | |||
| New agricultural cooperative medical insurance | 135(56.7%) | ||
| Urban basic medical insurance | 98(41.2%) | ||
| Self-paid(uninsured) | 5(2.1%) | ||
| Smoking status(%) | |||
| Former/current smoker | 115(48.3%) | ||
| Never smoked | 123(51.7%) |
a, VATS,Video-assisted thoracoscopic surgery.
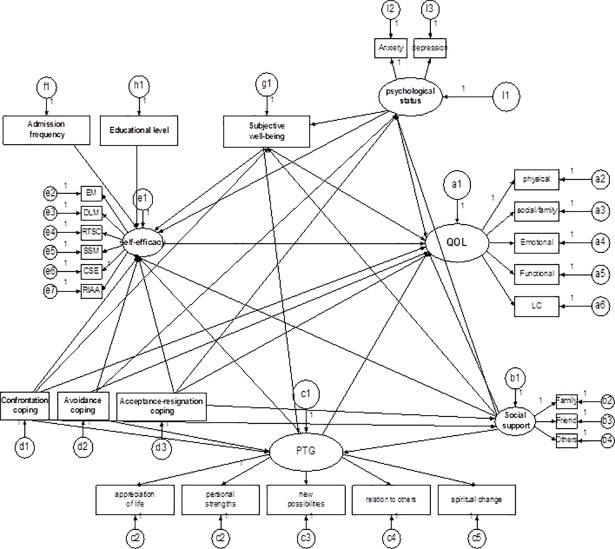
The hypothesis model of postsurgical rehabilitation management self-efficacy
Based on the findings of previous study [36], 12 variables were included in the linear regression model. The results from stepwise linear regression analysis highlighted the six influencing factors: anxiety and depression (Beta = -0.247,adjusted R2 = 0.113, p = 0.004), social support (Beta = 0.768,adjusted R2 = 0.148, p = 0.000), SWB (Beta = 0.375, adjusted R2 = 0.136, p = 0.000), PTG (Beta = 0.300, adjusted R2 = 0.051, p = 0.029), confrontation and acceptance-resignation coping (Beta = 0.442 & -0.158, adjusted R2 = 0.202, p<0.01). Based on our understanding of the literature and these preliminary data, we constructed the hypothesis model for self efficacy during postsurgical pulmonary rehabilitation which was further analyzed with SEM (Fig 1).
Fig 1. The hypothesis model of factors influencing self efficacy during postsurgical rehabilitation management.
PTG, posttraumatic growth; LC, lung cancer subscale; EM, emotional management self-efficacy subscale; DLM, daily life management self-efficacy subscale; RTSC, rehabilitation training and skills cultivating self-efficacy subscale; RIAA, rehabilitation information acquisition and application self-efficacy subscale; CSES, coping with treatment side effects self-efficacy self-efficacy subscale; SSM, symptom self-management self-efficacy subscale. QOL, quality of life.
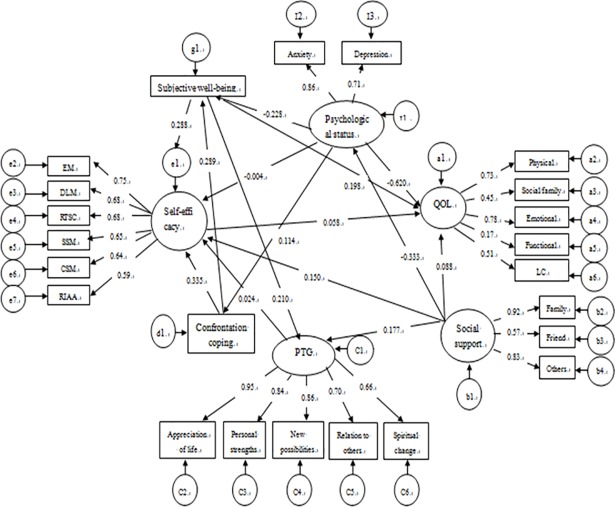
The final model and model estimation of SEM
Paths with no significant statistical effect, and variables with squared multiple correlations of 0 were eliminated from the hypothesis model (p>0.05).The overall fit of final model was found to be acceptable (Fig 2). The final model fit the data adequately and satisfied our preset criteria, χ2/df = 1.511(p>0.05), RMSEA = 0.063, CFI = 0.910, GFI = 0.900, NFI = 0.870. All paths showed significant statistical effect (p<0.05).
Fig 2. Finalized model of factors influencing self-efficacy postsurgical rehabilitation management.
PTG, posttraumatic growth; LC, lung cancer subscale; EM, emotional management; DLM, daily life management; RTSC, rehabilitation training and skills cultivating; RIAA, rehabilitation information acquisition and application; CSES, coping with treatment side effects self-efficacy; SSM, symptom self-management.QOL, quality of life. Oval indicates latent variables. Square indicates observe variables. Circle indicates error. Numbers on the arrows are coefficients of influence, with the signs indicates enhancing or reducing effects.
Table 2 illustrate the relationship between the structural parameters. The confrontation coping (coefficient = 0.335), SWB (coefficient = 0.288), social support (coefficient = 0.150), PTG (coefficient = 0.024) and anxiety and depression (coefficient = -0.004) can be seen to be directly related to self-efficacy (p<0.01 for model) (S1 Data).
Table 2. Effect coefficients of model-standardized estimates.
| Dependent variables | Independent variables | Direct effect | Indirect effect | Total effect |
|---|---|---|---|---|
| Confrontation coping | Self-efficacy | 0.335* | 0.085* | 0.419* |
| Social support | Self-efficacy | 0.150* | 0.006* | 0.162* |
| Subjective well-being | Self-efficacy | 0.288* | 0.005* | 0.293* |
| PTG a | Self-efficacy | 0.024* | 0.000 | 0.024* |
| Anxiety and depression | Self-efficacy | -0.004* | -0.027* | -0.031* |
| Self-efficacy | QOL b | 0.058* | 0.000 | 0.000 |
a, PTG, Posttraumatic growth
b, QOL, quality of life
*p<0.01
Confrontation was indirectly related to self-efficacy, mediated by SWB (indirect coefficient = 0.085, p<0.01). SWB was also indirectly related self-efficacy, mediated by PTG (indirect coefficient = 0.005, p<0.01). Social support had two indirect relationship pathways on self-efficacy, which were mediated by anxiety and depression and PTG (indirect coefficient for indirect effect = 0.006, p<0.01). Similar to social support, anxiety and depression also in turn had two indirect pathways to self-efficacy, via confrontation coping and SWB (indirect coefficient = -0.027, p<0.01).
Discussion
This study has two unique contributions. First, we provided a comprehensive model that illustrates the relationships between diverse variables and self-efficacy for postsurgical rehabilitation management in NSCLC patients. Second, we examined the potential effect mechanisms and interactions among these factors by SEM. We found that confrontation, social support, and PTG predicted higher levels of self-efficacy, whereas anxiety and depression predicted lower levels. Therefore, the study opens new doors of enhancing self-efficacy among postsurgical NSCLC patients that emphasizes the role of confrontation coping styles, social support, SWB, PTG and anxiety and depression. We also illustrated the close relationship between self-efficacy and QOL.
Compared with avoidance and acceptance-resignation coping strategies, confrontation coping facilitated self-efficacy, and had the largest effect coefficient. Our model suggest that confrontation not only directly enhances postoperative rehabilitation self-efficacy, but also exerts indirect effects through improving the patients’ SWB. It is worthwhile to assess NSCLC populations' coping strategies as rehabilitation progresses. Healthcare providers can encourage NSCLC patients to take on corrective confrontation coping strategy in order to have a better sense of well-being and feel self efficient.
SWB was both a direct influencer and mediating factor for self-efficacy. We observed that in postsurgical NSCLC patients, SWB may further improve their cognitive function (e.g., susceptibility, comprehension, and acceptability), cognitive and problem solving initiatives, effectively strengthening the postsurgical rehabilitation self-efficacy. Some of these cognitive changes were important contents of PTG [37].
Consistent with Bandura's social cognitive theory, we noted social support as a direct facilitator of self-efficacy and indirectly enhances it through psychological states and PTG. Social support provides a feeling of psychological wellbeing, positive perceptions and growth in cancer patients [38]. Social support was viewed as a protective factor against negative psychological states (e.g., anxiety and depression) and PTG [39]. Thus, postsurgical NSCLC populations with higher level of perceived social support and PTG, and less anxiety and depression, may feel more confident to conduct postsurgical rehabilitation management activities.
Social support and self-efficacy as important facilitators of PTG have been mentioned previously [40,41], and confirmed here. We also show an indirect pathway between social support and self-efficacy via PTG. The help and support from spouse, family, and friends are a critical part of lung cancer patients' response to their illness and treatments and should be exploited to enhance self-efficacy during post-surgical rehabilitation. Construction of a support network for the NSCLC population, a platform for communication with each other, experience sharing and family encouragement may help reduce cancer patients’ postoperative anxiety and depression, and provide them a sense of hope and confidence, resulting in a greater sense of personal strength and growth.
Our study verified the direct relationship between PTG and self-efficacy, as reported previously [42]. PTG may help assist the development of self-efficacy. Postsurgical NSCLC patients with higher level of PTG tend to use social resources and personal abilities (e.g., rehabilitation coping techniques), and adapt positive coping strategies with various of physical and psychological distress.
Negative psychological states such as anxiety or depression both directly and indirectly reduced postsurgical NSCLC patients’ self-efficacy. Cancer patients with lower level of anxiety and depression tend to take positive confrontation coping strategies [43,44], and have higher SWB [45]. Healthcare providers can help postsurgical NSCLC patients increase positive emotional experiences, reduce anxiety and depression, increase their SWB and encourage them to apply more confrontation coping strategies, in order to enhance their self-efficacy.
This study is not free from limitations. First, given the cross-sectional and self-reported study design, we cannot infer causality among the factors examined. Second, the current sample was recruited from five tertiary hospitals in Fujian province and may have limited generalizability. Third, the participants have to answer roughly 150 questions in ten questionnaires that were used in this study, possibly causing survey fatigue. Finally, although the sample size met with the criterion of SEM, the same data was used to identifying the hypothesized model and evaluating the model. Future study should be designed to replicate the current study using a large sample drawn from different regional hospitals to further verify our results.
Conclusions
This study model suggested that higher confrontation coping style, SWB, social support, and PTG and lower anxiety and depression levels could effectively enhance their self-efficacy and consequently, improve QOL. The findings could inspire the development of an effective and operative intervention aimed at enhancing self-efficacy of postsurgical NSCLC patients. To achieve this, clinical nurses should consider the following factors, such as coping skills, SWB, social support, PTG and anxiety and depression to enhance postsurgical rehabilitation self-efficacy and ultimately improve QOL.
Supporting information
(JPG)
(DOCX)
(SAV)
Acknowledgments
We sincerely thank all the participants and their family supporters without whom this study would have not been possible, and the healthcare providers of those hospitals, who assist in the data collection of the study.
Data Availability
All relevant data are within the paper and its Supporting Information files.
Funding Statement
This study was supported by Grant from the Natural Science Foundation of Hunan Province, China (Grant number. 12J6095) and Startup Fund for scientific research, Fujian Medical University (Grant number: 2016QH017).
References
- 1.Li XH, Zhu JL, Hong C, Zeng L, Deng LM, Jin LY. Effects of systematic rehabilitation programs on quality of life in patients undergoing lung resection. Mol Clin Oncol. 2013; 1:200–208. 10.3892/mco.2012.31 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.WHO[cited 1 June 2015]. Available from: http://www.cancer.org/research/cancerfactsstatistics/cancerfactsfigures2015/index.
- 3.She J. Lung cancer in China: challenges and interventions. Chest. 2013; 143: 1117–1126. 10.1378/chest.11-2948 [DOI] [PubMed] [Google Scholar]
- 4.Huang FF, Yang Q, Han XY, Zhang JP, Lin T. Development and validation of a self‐efficacy scale for postoperative rehabilitation management of lung cancer patients. Psycho‐Oncology.2017; 26:1172–1180. 10.1002/pon.4296 [DOI] [PubMed] [Google Scholar]
- 5.Wildgaard K, Ravn J, Nikolajsen L, Jakobsen E, Jensen TS, Kehlet H. Consequences of persistent pain after lung cancer surgery: a nationwide questionnaire study. Acta Anaesthesiol Scand. 2011;55:60–68. 10.1111/j.1399-6576.2010.02357.x [DOI] [PubMed] [Google Scholar]
- 6.Hoffman AJ, Brintnall RA, von Eye A, Jones LW, Alderink G, Patzelt LH, et al. Home-based exercise: promising rehabilitation for symptom relief, improved functional status and quality of life for post-surgical lung cancer patients. J Thorac Dis. 2014;6:632–640. 10.3978/j.issn.2072-1439.2014.06.08 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Shi Y, Gu F, Hou LL, Hu YQ. Self-reported depression among patients with non-small cell lung cancer. Thorac Cancer. 2015; 6:334–337. 10.1111/1759-7714.12179 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Kaneda H, Saito Y, Okamoto M, Maniwa T, Minami K, Imamura H. Early postoperative mobilization with walking at 4 hours after lobectomy in lung cancer patients. Gen Thorac Cardiovasc Surg. 2007;55:493–498. 10.1007/s11748-007-0169-8 [DOI] [PubMed] [Google Scholar]
- 9.Brunelli A, Xiumé F, Refai M, Salati M, Marasco R, Sciarra V, et al. Evaluation of expiratory volume, diffusion capacity and exercise tolerance following major lung resection: a prospective follow-up analysis. Chest. 2007;131:141–147. 10.1378/chest.06-1345 [DOI] [PubMed] [Google Scholar]
- 10.Novoa N, Varela G, Jiménez MF, Aranda JL. Influence of major pulmonary resection on postoperative daily ambulatory activity of the patients. Interact Cardiovasc Thorac Surg. 2009; 9: 934–938. 10.1510/icvts.2009.212332 [DOI] [PubMed] [Google Scholar]
- 11.Chang NW, Lin KC, Lee SC, Chan JY, Lee YH, Wang KY. Effects of an early postoperative walking exercise programme on health status in lung cancer patients recovering from lung lobectomy. J Clin Nurs. 2014; 23:3391–3402. 10.1111/jocn.12584 [DOI] [PubMed] [Google Scholar]
- 12.Vogiatzis I, Rochester CL, Spruit MA, Troosters T, Clini EM; American Thoracic Society/European Respiratory Society Task Force on Policy in Pulmonary Rehabilitation. Increasing implementation and delivery of pulmonary rehabilitation: key messages from the new ATS/ERS policy statement. Eur Respir J. 2016; 47:1336–1341. 10.1183/13993003.02151-2015 [DOI] [PubMed] [Google Scholar]
- 13.Signe BB, Tore WL, Anne HH, Rokne B, Wahl AK. Self-efficacy as a predictor of improvement in health status and overall quality of life in pulmonary rehabilitation-An exploratory study. Patient Educ Couns. 2010;81: 5–13. 10.1016/j.pec.2009.11.019 [DOI] [PubMed] [Google Scholar]
- 14.Heitzmann CA, Merluzzi TV, Jean-Pierre P, Roscoe JA, Kirsh KL, Passik SD. Assessing self-efficacy for coping with cancer: development and psychometric analysis of the brief version of the Cancer Behavior Inventory (CBI-B). Psycho-oncol. 2010; 20:302–312. [DOI] [PubMed] [Google Scholar]
- 15.Lev EL, Eller LS, Kolassa J, Gejerman G, Colella J, Lane P, et al. Exploratory factor analysis: strategies used by patients to promote health. World J Urol. 2007; 25:87–93. 10.1007/s00345-006-0126-7 [DOI] [PubMed] [Google Scholar]
- 16.Chirico A, Lucidi F, Merluzzi T, Alivernini F, Laurentiis M, Botti G, et al. A meta-analytic review of the relationship of cancer coping self-efficacy with distress and quality of life. Oncotarget. 2017;8:36800–36811. doi: 10.18632/oncotarget.15758 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lee JW, Lee KE, Park DJ, Kim SH, Nah SS, Lee JH, et al. Determinants of quality of life in patients with fibromyalgia: A structural equation modeling approach. Plos one. 2017;12:1–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Bandura A. Social Foundations of Thought and Action: A Social Cognitive Theory. Prentice-Hall, Englewood Cliffs, NJ; 1986.
- 19.Manne SL, Ostroff JS, Norton TR, Fox K, Grana G, Goldstein L. Cancer-specific self-efficacy and psychosocial and functional adaptation to early stage breast cancer. Ann Behav Med. 2006;31:145–154. 10.1207/s15324796abm3102_6 [DOI] [PubMed] [Google Scholar]
- 20.Wu ML. Structural equation modeling—the operation and application of AMOS Chongqing, China: Chong qing University Press; 2009. [Google Scholar]
- 21.Kline RB. Principles and Practice of Structural Equation Modeling 2nd ed. New York, NY: Guilford Press;2004. [Google Scholar]
- 22.Cella DF, Bonomi AE, Lloyd SR, Tulsky DS, Kaplan E, Bonomi P. Reliability and validity of the Functional Assessment of Cancer Therapy-Lung (FACT-L) quality of life instrument. Lung Cancer. 1995; 12:199–220. [DOI] [PubMed] [Google Scholar]
- 23.Ye WF, Xu JM. Application and evaluation of the hospital anxiety and depression Scale in patients of general hospital. Chin J of Behaviorial Med Sci. 1993a; 3:17–19. [Google Scholar]
- 24.Pedersen SS, Spinder H, Erdman RA, Denollet J. Poor perceived social support in implantable cardioverter defibrillator (ICD) patients and their partners: cross-validation of the multidimensional scale of perceived social support. Psychosomatics. 2009; 50:461–467. 10.1176/appi.psy.50.5.461 [DOI] [PubMed] [Google Scholar]
- 25.Jiang QJ. Perceived Social Support Scale. Chin J of Behaviorial Med Sci. 2001;10:41–43 [Google Scholar]
- 26.Zhang ZJ. Behavioral medical instrument manual. Chin J of Behaviorial Med Sci. 2010;10:110. [Google Scholar]
- 27.Lorish CD, Maisiak R. The Face Scale: a brief, nonverbal method for assessing patient mood. Arthritis Rheum. 1986; 29:906–909.PMID:. [DOI] [PubMed] [Google Scholar]
- 28.Wang XD, Wang XL, Ma H. Rating scales for mental health. Chin Mental Health J. 1999;250–256. [Google Scholar]
- 29.Feifel H, Strack S, Nagy VT. Coping strategies and associated features of medically ill patients. Psychosom Med. 1987;49:616–625.PMID:. [DOI] [PubMed] [Google Scholar]
- 30.Kan KK. Validation of the Insomnia Severity Index, Athens Insomnia Scale and Sleep Quality Index in Adolescent Population in Hong Kong. 2008. [Last accessed on 2015 Nov 23]. Available from: http://www.hdl.handle.net/10722/52015
- 31.Bernabei R, Gambassi G, Lapane K, Landi F, Gatsonis C, Dunlop R, et al. Management of pain in elderly patients with cancer. JAMA. 1998;279:1877–1882. [DOI] [PubMed] [Google Scholar]
- 32.Imperatori A, Grande A, Castiglioni M, Gasperini L, Faini A, Spampatti S,et al. Chest pain control with kinesiology taping after lobectomy for lung cancer: initial results of a randomized placebo-controlled study. Interact Cardiovasc Thorac Surg. 2016;23:223–230. 10.1093/icvts/ivw110 [DOI] [PubMed] [Google Scholar]
- 33.Tedeschi RG, Calhoun LG. The posttraumatic growth inventory: measuring the positive legacy of trauma. J Trauma Stress. 1996;9:455–471. [DOI] [PubMed] [Google Scholar]
- 34.Wang J, Chen Y, Wang YB, Liu XH. Revision of the Posttraumatic Growth Inventory and testing its reliability and validity. J Nurs Sci. 2011;26:26–28. [Google Scholar]
- 35.Zhao QL. Development and Application of Assessment Instruments in Nursing Field Beijing: People's Medical Publishing House; 2014. [Google Scholar]
- 36.Huang FF, Zhang J, Xie L, Zhang JP. A survey on postoperative rehabilitation self-efficacy and its influencing factors of patients with lung cancer. Chin J Nurs Educ.2017;14:619–624. [Google Scholar]
- 37.Li N, Wang L, Cao X, Cao CQ. Posttraumatic Growth and Related Factors in Hospitalized Patients with Advanced Cancer. Chin J Clin Psychology. 2014; 22:623–626. [Google Scholar]
- 38.Schwarzer R, Luszczynska A,Boehmer S, Taubert S, Knoll N. Changes in finding benefit after cancer surgery and the prediction of well-being one year later. Soc Sci Med. 2006; 63: 161–1624. [DOI] [PubMed] [Google Scholar]
- 39.Dinenberg RE, McCaslin SE, Bates MN, Cohen BE. Social support may protect against development of posttraumatic stress disorder: Findings from the heart and soul study. Am J Health Promot. 2014;28:294–297. 10.4278/ajhp.121023-QUAN-511 [DOI] [PubMed] [Google Scholar]
- 40.Lotfi-Kashani F, Vaziri S, Akbari ME, Kazemi-Zanjani N, Shamkoeyan L. Predicting Post Traumatic Growth Based upon Self-Efficacy and Perceived Social Support in Cancer Patients. Iran J Cancer Prev. 2014; 7:115–123. [PMC free article] [PubMed] [Google Scholar]
- 41.McDonough MH, Sabiston CM, Wrosch C. Predicting changes in posttraumatic growth and subjective well-being among breast cancer survivors: the role of social support and stress. Psychooncology. 2014; 23:114–120. 10.1002/pon.3380 [DOI] [PubMed] [Google Scholar]
- 42.Yu Y, Peng L, Tang T, Chen L, Li M, Wang T. Effects of emotion regulation and general self-efficacy on posttraumatic growth in Chinese cancer survivors: assessing the mediating effect of positive affect. Psycho-oncology. 2014; 23:473–478. 10.1002/pon.3434 [DOI] [PubMed] [Google Scholar]
- 43.Zhang TY, Liu RZ, An B. Effects of Coping Styles on Depression and Quality of Life of Cancer Patients. Chin J Rehabil Theory Pract. 2014;5:477–480 [Google Scholar]
- 44.Zhang X, Zhang JP, Wang A et al. Effect of progressive muscle relaxation training on coping style and emotion of patients with lung cancer. J Chongqing Med University. 2015;40:1457–1460 [Google Scholar]
- 45.Xia LX. The effect of SFA psychological interventions on negative affection and SWB of cancer patients undergoing chemotherapy The master’s dissertation. Fourth Military Medical University; 2013. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
(JPG)
(DOCX)
(SAV)
Data Availability Statement
All relevant data are within the paper and its Supporting Information files.