Abstract
Objective
The aim of the study was to compare the mechanical behavior of interference screw tibial fixation vs. screw-plus-staple tibial fixation in an animal model.
Methods
Thirty-six pieces of swine knee specimens were selected and divided into two groups: Group 1, tibial fixation with interference screw (n = 17), and Group 2, fixation with interference screw and staple (n = 19). The models were submitted to a single cycle of tension testing. The following variables were measured: graft cross-sectional area, failure point on 10 mm (F10), yield load (Fy), and stiffness.
Results
The mean values of graft cross-sectional area, F10, Fy, and stiffness did not present significant differences between the groups.
Conclusion
The addition of a second staple-type ligament fixation device, complementing the interference screw, did not increase the mechanical safety of the system.
Keywords: Anterior cruciate ligament, Tibia, Orthopedic fixation devices, Biomechanical phenomena, Tendons
Resumo
Objetivo
Comparar o comportamento mecânico da fixação tibial com parafuso de interferência versus parafuso de interferência com agrafe, em modelo animal.
Métodos
Foram selecionadas 36 peças de joelho suíno e divididas em dois grupos: Grupo 1, fixação tibial com parafuso de interferência (n = 17) e Grupo 2, fixação com parafuso de interferência e agrafe (n = 19). Os modelos foram submetidos a teste de ciclo único de tração. Foram mensuradas as seguintes variáveis: medida da área de seção transversal do enxerto, ponto de falha nos 10 mm (F10), yield load (Fy) e rigidez.
Resultados
Os valores médios de área de seção transversal do enxerto, F10, Fy, e rigidez não apresentaram diferenças significativas entre os grupos.
Conclusão
A adição de um segundo dispositivo de fixação ligamentar tibial tipo agrafe, complementar ao parafuso de interferência, não aumentou a segurança mecânica do sistema.
Palavras-chave: Ligamento cruzado anterior, Tíbia, Dispositivos de fixação ortopédica, Fenômenos biomecânicos, Tendões
Introduction
The anterior cruciate ligament (ACL) is one of the four most important ligaments of the knee. Together with the posterior cruciate ligament, tibial collateral, and posterolateral ligaments, it helps maintain the knee stable by not allowing abnormal movements between the femur and the tibia. The treatment of ACL injury is often surgical. In the absence of an ACL, the practice of some sports becomes inadvisable, as frequent sprains may occur due to instability and its complications.1 The indication of surgical reconstruction of the ACL is due to the presence of symptoms, especially instability. This method of treatment presents better results for sports practice.2
In the United States, the most commonly used graft for ACL reconstruction is the knee flexor tendons, more specifically the tendons of the gracilis and semitendinosus muscles. This graft is also called quadrupled grafts, because it has four bundles, two from the gracilis and two from the semitendinosus.3 Its main advantages are low morbidity at the donor site, lower rates of quadriceps muscle atrophy, and less painful rehabilitation. As a disadvantage of this technique, some authors question the rigidity of tendon fixation to the bone.4
In most cases of ACL reconstruction, the tibia is secured with interference screws, which was the first device specially designed for this type of surgery.5 This isolated method may not be sufficient for tibial fixation since the tibial cancellous bone has a lower density than its femoral equivalent.6 This finding is more frequently observed in elderly patients or in those with diseases that affect bone density. In these cases, an additional fixation may be required.7 Another possible advantage of a secondary fixation is the fact that the patient is authorized to undergo a more aggressive initial rehabilitation, with less muscle mass and proprioception loss, due to the increase in fixation resistance.
The three frequent options for additional tibial attachment to the screw are staples, a screw post, and a screw with a washer. The use of screw posts or screws with washers is affordable and present good results.8 The disadvantage is that, in some cases, it can generate pain in the region under the screw head. This incidence of pain can reach 48% of the cases.8
The staple is a fixation method that has the advantage of being positioned at the same level as the bone structures, reducing the chances of discomfort for the patient. The staple can be used as a supplement to the interference screw, but only a few studies in the literature have assessed the mechanical behavior of the supplementary fixation with staples in the tibia.7, 9, 10
This study is aimed at comparing, in an animal model, the mechanical behavior of tibial fixation of the flexor tendon grafts with an interference screw vs. an interference screw plus a staple.
Material and methods
The test specimens were mounted with swine tibiae and bovine tendons.11, 12 They were divided into two groups: Group (1) control group, in which the graft was secured with interference screws; Group (2) double fixation group, in which the graft was secured with interference screw and staples.
The tendons were harvested in a slaughterhouse, and the peritendinous tissues were removed. As the tendon anatomy is Y-shaped, they were dissected to form two tendon segments. The two ends of the separated tendons were sutured with No. 5 polyester thread.
Tendons were harvested in pairs, for measurement in a perforated ruler, with millimeter holes, in order to create quadrupled grafts. Only grafts with a maximum diameter of 9 mm were included in the study.
To accurately gauge the area, the grafts were immersed in type II Jeltrate alginate (Dentsply, York, PA, United States) in a 20-cm-long, 5-cm-wide box. After a few seconds, the alginate paste becomes gelatinous and creates a cast. This cast was sectioned transversely into 10-mm-thick blocks.13
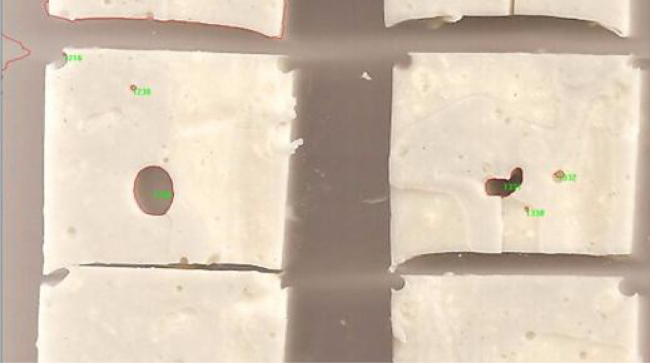
Sections from the resulting template were scanned at 600 dpi resolution using an HP J5780® digitizer; the Image-Pro Plus® software was used to generate cross-sectional area measurements of the templates from the scanned images (Fig. 1).
Fig. 1.
Image acquired by the scanner in Image-Pro Plus software.
The area of each quadrupled graft was obtained by adding the mean area of its four extremities.
Swine tibiae were obtained from animals of Large White breed weighing between 100 and 120 kg. Forty specimens were selected and purchased in a slaughterhouse for human consumption.
The surgical procedure began with a conventional tibial guide to position a Kirschner wire, which served as a guide for drilling the 9-mm tunnel with a cannulated drill. The tunnel was created in its original insertion; its exit was placed between the intercondylar eminences, in the superior articular surface. The drill followed the guidewire on the medial aspect of the tibia, approximately 2 cm medial to the anterior tibial tuberosity.
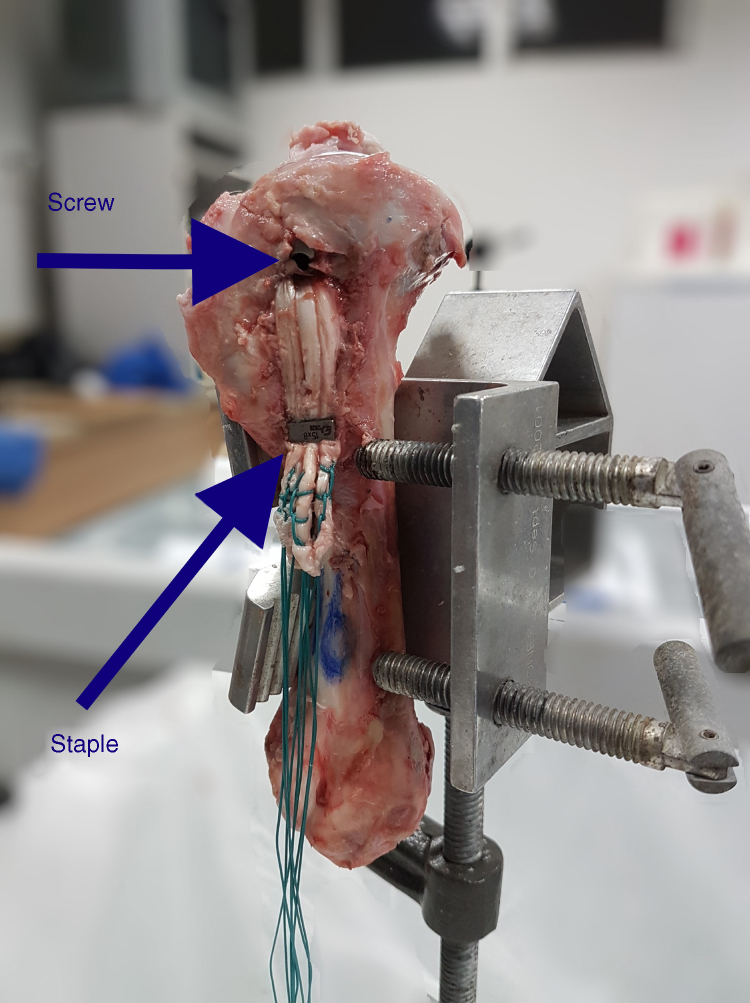
In 17 specimens, the graft was secured only with a 9-mm diameter titanium interference screw (Group 1). In Group 2, a thorny staple was used (Fig. 2) in association to the interference screw to secure the graft (Fig. 3).
Fig. 2.

Thorny staple.
Fig. 3.
Fixation with interference screw and staple.
After the surgical procedure, the specimens were embedded in epoxy resin 134 in rigid PVC molds with the dimensions of 60 mm diameter, 75 mm length, and 3.3 mm thickness. The epoxy resin was manipulated at a ratio of 1:4, i.e., 25% catalyst and 75% resin. The total curing time of 60 min was respected.
In order to maintain the specimens upright during the simultaneous filling of six casts with resin, a support device was constructed with MDF sheets (15-mm thick), a brushed steel bar (12.7 × 500 mm), and wood screws (5 × 30 mm). The height from the base to the support bar was 230 mm; the external length of the graft, 500 mm; and the external width, 180 mm.
After being embedded in resin, the samples were mounted in a fixation and alignment device for the assay. This device consists of an angled precision vise with jaws designed to allow the attachment of cylindrical bodies. The configuration of the vise allowed a good visual alignment between the traction axis and the graft tunnel.
The jaws of the vise were made of AISI 1045 steel, with wedge creases inclined at 20°, which allowed tilting the x-axis from 20° to 65°.
The tendon traction sleeve was made of the same material as the vise and consists of three components: a fixation screw in the load cell, the U-shaped body, and an 8-mm diameter pin on which the tendon was looped.
During all manipulation, storage, and fixation procedures and mechanical testing, the tibiae and tendons were kept moist with an isotonic saline solution to avoid dehydration and alteration of their mechanical characteristics.
The tendons were placed in an EMIC DL 10000 traction machine, equipped with displacement transducers and an S-type load cell (EMIC-CCE5KN), with a maximum nominal load of 500 Kgf and resolution of 0.1 Kgf. The graft was maintained at 50 mm from the tibia, simulating the surgical condition. The fixation of the tendon loops on the sleeve and of the test specimen on the jaws was made through visual alignment of the axis of rotation of the machine and the axis passing through the graft tunnel in the fixation device.
After fixation of the porcine knee to the machine, a constant 80-N traction force was applied for 2 min for pre-tensioning and system accommodation.14 Thereafter, the traction force was returned to 10 N. At that moment, the single traction test was initiated at a speed of 30 mm/min. The test was interrupted after 10 mm of displacement. F10 was defined as the force measurement at the point of 10 mm of displacement.15
The force and displacement data were provided by the EMIC machine's software (TESC) and exported to Microsoft Excel® software.
The first point at which the chart line stopped being straight was also recorded, as it is the point where the tendon deformity has ceased to be elastic (with a capacity to return to the original state) and has become plastic.16 This parameter is called the yield load and is represented in this study as Fy.7
For certain F10 and Fy, the secant mode was used to measure the slope of the line, which translates into stiffness measurements (R10 and Ry).
The F10 and Fy values of each group were divided by the area of the graft tested to measure tension, and are represented as σ10 and σy.
Student's t-test was used to obtain the p-value to assess the statistical significance of the difference between the groups. Values were considered significant when p < 0.05.
Results
The mean area value for Group 1 was 37 ± 10 mm2, and for Group 2, 32 ± 4 mm2; no statistically significant difference was observed between the groups (p > 0.05).
When comparing both groups, no statistically significant difference was observed regarding F10 and Fy failure loads, stiffness measurements (R10 and Ry), and strength and tension; the results are shown in Table 1.
Table 1.
Results of the mean values of the force at the 10 mm displacement point (F10), yield load (Fy), rigidity (R10 and Ry), and tension (σ10 and σy) for Groups 1 and 2, and statistical significance (p).
| Group 1 | Group 2 | p | |
|---|---|---|---|
| F10 (N) | 324.7 ± 12 A | 333.1 ± 78 A | 0.4 |
| Fy (N) | 304.6 ± 13 B | 251 ± 144 B | 0.12 |
| R10 (N/mm) | 31.5 ± 12 C | 32.4 ± 8 C | 0.39 |
| Ry (N/mm) | 38.4 ± 14 D | 40.3 ± 12 D | 0.33 |
| σ10 (MPa) | 9.3 ± 4 E | 10.2 ± 2 E | 0.19 |
| σy (Mpa) | 8.9 ± 5 F | 7.7 ± 4 F | 0.21 |
Note: Different capital letters represent statistically significant differences in the line.
Discussion
The most studied double fixation methods use screw posts, anchors, and staples. A theoretical advantage of the staple over the others is that it acts directly on the tendon. This can lead to a more efficient mechanical action when compared with anchors and screw posts, which are secured through wires. Despite this type of mechanical action, in the present study, no significant differences were found between the group in which the tibial fixation was made only with interference screws and the group with interference screws associated with staples. In the classic study by Kurosaka et al.,5 better results were found in the tensile strength of cadaver grafts secured with interference screws when compared with staples; it can be hypothesized that the interference screw already reaches the mechanical limit of the tendon and that the complementary fixation is no longer able to increase resistance. In turn, in the study by Gerich et al.,17 maximum strength values ranging from 506 to 758 N were observed in the group in which fixation was made with interference screws and 558 N for the group with staples. The rigidity calculated for a 175 N-load was significantly higher in the staple fixation group. An important limitation when comparing the present results with those observed by Kurosaka et al.5 and Gerich et al.17 is that they analyzed single fixations in the patellar tendon; in the present study, one group had combined fixation, and in both groups, the fixation was made over a tendon graft.
For the tests with ACL reconstruction fixation devices, the ideal would be to have musculoskeletal tissue of young human donors, since the ACL reconstruction procedure is indicated in physically active patients.2 The shortage of young cadaver tissue leads to the hunt for similar substitutes, as the main factor in fixation durability is bone quality. One of the most used options is the swine knee, because it has a similar anatomy, despite the fact that its cancellous bone is more resistant.12 The ideal animal model for simulation of human knee flexors is the bovine digital tendon, whose mechanical behavior is very similar to that of the human knee flexor tendon.11 The present study was aimed at comparing the effectiveness of different fixation devices using the animal tissue models best suited for the investigation. However, the absolute data should not be extrapolated to human beings.
One of the parameters of the study was the failure of the system at 10 mm of displacement (F10) since it is recognized that 10 mm of anterior tibial translation indicates clinical instability and therapeutic failure.15 The values of F10 were similar to the yield load (Fy), which is the most commonly used parameter in current studies.18
The use of the F10 failure point, i.e., an increase of the graft length by 10 mm, could be an additional variable to be collected in biomechanical studies. Although this occurs below the 445 N threshold, defined as a minimum acceptable for rehabilitation of ACL reconstruction surgery, it is believed that ligament insufficiency is already defined at this point.19 Thus, even if there is a linear force vs. displacement behavior, a force measurement of less than 445 N at the point of 10 mm would mean a probable failure, even if the curve does not demonstrate yield load. This hypothesis motivated the adoption of this parameter.19
Studies evaluating additional tibial fixation with staples had force values at the point of failure similar to those observed in the present study. One study showed a failure force of 254 N for screw fixation and 197 N for screw and staple (p = 0.24).7 Other studies evaluating tibial fixation also found similar values, using other methods of additional fixation.20, 21
Both rigidity parameters (R10 and Ry) showed no significant difference between the groups. A possible explanation for this lack of significance is that the values observed may represent the plastic limit of the graft. Therefore, the addition of another fixation device did not increase system resistance. This hypothesis is strengthened by the fact that the F10 and Fy values were similar. Another factor is the high density of porcine cancellous bone, which may have increased screw effectiveness. Therefore, the screw as an isolated fixation device may have been sufficient to bring the tendon to its plastic deformation, making additional attachments irrelevant from the mechanical standpoint.10, 12 However, another study observed a greater clinical stability in the group with additional fixation with staples two years after surgery.9
In the two studies in which fixation stiffness was compared, the absolute values were substantially higher than those found in this study, although not statistically significant.7, 9 A possible explanation is that such differences may have occurred due to prior cyclical testing. In both studies, a cyclic test was performed prior to traction, which could have led to accommodation of the fixation system, providing a more immediate response to the tensioning of the system, which would be translated as greater stiffness. These data may suggest a cyclic pretensioning prior to graft fixation, which may increase stiffness; the literature present divergent opinions of poor scientific quality, being unable to prove this behavior.22, 23, 24
In Group 1, the influence of the cross-sectional area was suppressed by the stress calculation (σ10 and σy). An accurate measurement of the graft area is critical in correcting this bias. Studies that measure graft area only through a perforated ruler, which has a sharp increase at each test hole, can impact the reliability of the values. Alginate cast measurement meets the precision requirements, in addition to being of low cost.
The present study has some limitations, such as the small sample size, the fact that no cyclic tests were performed, that animal models were used, and that the models had no femur. The study was aimed at performing an isolated evaluation of the tibial fixation, and the presence of a femur could generate a bias. Graft traction was made in the same line as the tibial tunnel, simulating the worst possible scenario.5, 25, 26, 27 Future studies, which consider the above limitations, are necessary to determine the mechanical efficacy of the extra-tunnel staple associated with an interference screw in the tibial fixation of quadrupled flexor tendon grafts.
Conclusion
The present study failed to demonstrate a greater efficacy of the double fixation of quadrupled flexor tendons using interference screw and staple when compared with fixation made with an interference screw alone.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Study conducted at Universidade Federal do Paraná (UFPR), Curitiba, PR, Brazil.
References
- 1.Bollen S. Ligament injuries of the knee – limping forward? Br J Sports Med. 1998;32(1):82–84. doi: 10.1136/bjsm.32.1.82. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cohen M., Abdalla R.J., Ejnisman B., Filardi M.S., Amaro J.T. Estudo comparativo no tratamento das lesöes do ligamento cruzado anterior no esporte. Rev Bras Ortop. 1997;32(5):337–341. [Google Scholar]
- 3.Scannell B.P., Loeffer B.J., Hoeing M., Peindl R.D., D’Alessandro D.F., Connor P.M. Biomechanical comparison of hamstring tendon fixation devices for anterior cruciate ligament reconstruction: Part 2, four tibial devices. Am J Orthop (Belle Mead NJ) 2015;44(2):82–85. [PubMed] [Google Scholar]
- 4.Brand J., Jr., Weiler A., Carbon D.N., Brrown C.H., Jr., Johnson D.L. Graft fixation in cruciate ligament reconstruction. Am J Sports Med. 2000;28(5):761–774. doi: 10.1177/03635465000280052501. [DOI] [PubMed] [Google Scholar]
- 5.Kurosaka M., Yoshiya S., Andrish J.T. A biomechanical comparison of different surgical techniques of graft fixation in anterior cruciate ligament reconstruction. Am J Sports Med. 1987;15(3):225–229. doi: 10.1177/036354658701500306. [DOI] [PubMed] [Google Scholar]
- 6.Scheffler S.U., Sudkamp N.P., Gockenjan A., Hoffmann R.F., Weller A. Biomechanical comparison of hamstring and patellar tendon graft anterior cruciate ligament reconstruction techniques: the impact of fixation level and fixation method under cyclic loading. Arthroscopy. 2002;18(3):304–315. doi: 10.1053/jars.2002.30609. [DOI] [PubMed] [Google Scholar]
- 7.Lee J.J., Otarodifard K., Jun B.J., McGarry M.H., Hatch G.F., 3rd, Lee T.Q. Is supplementary fixation necessary in anterior cruciate ligament reconstructions? Am J Sports Med. 2011;39(2):360–365. doi: 10.1177/0363546510390434. [DOI] [PubMed] [Google Scholar]
- 8.Camanho G.L., Camanho L.F., Viegas A.C. Reconstrução do ligamento cruzado anterior com tendões dos músculos flexores do joelho fixos com Endobutton. Rev Bras Ortop. 2003;38(6):329–336. [Google Scholar]
- 9.Fabbriciani C., Mulas P.D., Ziranu F., Deriu L., Zarelli D., Millano G. Mechanical analysis of fixation methods for anterior cruciate ligament reconstruction with hamstring tendon graft. An experimental study in sheep knees. Knee. 2005;12(2):135–138. doi: 10.1016/j.knee.2004.05.001. [DOI] [PubMed] [Google Scholar]
- 10.Prado M., Martín-Castilla B., Espejo Reina A., Serrano-Fernández J.M., Pérez-Blanca A., Ezquerro F. Close-looped graft suturing improves mechanical properties of interference screw fixation in ACL reconstruction. Knee Surg Sports Traumatol Arthrosc. 2013;21(2):476–484. doi: 10.1007/s00167-012-1975-9. [DOI] [PubMed] [Google Scholar]
- 11.Donahue T.L., Gregersen C., Hull M.L., Howell S.M. Comparison of viscoelastic, structural, and material properties of double-looped anterior cruciate ligament grafts made from bovine digital extensor and human hamstring tendons. J Biomech Eng. 2001;123(2):162–169. doi: 10.1115/1.1351889. [DOI] [PubMed] [Google Scholar]
- 12.Nurmi J.T., Sievanen H., Kannus P., Jarvinen M., Jarvinen T.L. Porcine tibia is a poor substitute for human cadaver tibia for evaluating interference screw fixation. Am J Sports Med. 2004;32(3):765–771. doi: 10.1177/0363546503261732. [DOI] [PubMed] [Google Scholar]
- 13.Stieven Filho E., Malafaia O., Ribas-Filho J.R., Diniz O.E.S., Borges P.C., Albano M. Biomechanic analysis of the sewed tendons for the reconstruction of the anterior cruciate ligament. Rev Col Bras Cir. 2010;37(1):52–57. doi: 10.1590/s0100-69912010000100011. [DOI] [PubMed] [Google Scholar]
- 14.Yamanaka M., Yasuda K., Tohyama H., Nakano H., Wada T. The effect of cyclic displacement on the biomechanical characteristics of anterior cruciate ligament reconstructions. Am J Sports Med. 1999;27(6):772–777. doi: 10.1177/03635465990270061401. [DOI] [PubMed] [Google Scholar]
- 15.Aga C., Rasmussen M.T., Smith S.D., Jansson K.S., LaPrade R.F., Engebretsen L. Biomechanical comparison of interference screws and combination screw and sheath devices for soft tissues anterior cruciate ligament reconstruction on the tibial side. Am J Sports Med. 2013;41(4):841–848. doi: 10.1177/0363546512474968. [DOI] [PubMed] [Google Scholar]
- 16.Figueiredo Filho D.B., Silva Júnior J.A.D. Desvendando os mistérios do coeficiente de correlação de Pearson (r) Rev Política Hoje. 2009;18(1):115–146. [Google Scholar]
- 17.Gerich T.G., Cassim A., Lattermann C., Lobenhoffer H.P. Pullout strength of tibial graft fixation in anterior cruciate ligament replacement with a patellar tendon graft: interference screw versus stapple fixation in human knees. Knee Surg Sports Traumatol Arthrosc. 1997;5(2):84–88. doi: 10.1007/s001670050032. [DOI] [PubMed] [Google Scholar]
- 18.Stieven Filho E., Mendes M.H.D., Claudino S., Baracho F., Borges P.C., Cunha L.A.M. Biomechanical analysis on transverse tibial fixation in anterior cruciate ligament reconstructions. Rev Bras Ortop. 2015;50(2):174–179. doi: 10.1016/j.rboe.2015.02.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Morrison J.B. Function of the knee joint in various activities. Biomed Eng. 1969;4(12):573–580. [PubMed] [Google Scholar]
- 20.Higano M., Tashibana Y., Sahagushi K., Goto T., Oda H. Effects of tunnel dilation and interference screw position on the biomechanical properties of tendon graft fixation for anterior cruciate ligament reconstruction. Arthroscopy. 2014;29(11):1804–1810. doi: 10.1016/j.arthro.2013.07.263. [DOI] [PubMed] [Google Scholar]
- 21.Yang D.-L., Cheon S.-H., Oh C.-W., Kyung H.-S. A comparison of the fixation strengths provided by different intraosseous tendon lengths during anterior cruciate ligament reconstruction: a biomechanical study in a porcine tibial model. Clin Orthop Surg. 2014;6(2):173–179. doi: 10.4055/cios.2014.6.2.173. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Boylan D., Greis P.E., West J.R., Bachus K.N., Burks R.T. Effects of initial graft tension on knee stability after anterior cruciate ligament reconstruction using hamstring tendons: a cadaver study. Arthroscopy. 2003;19(7):700–705. doi: 10.1016/s0749-8063(03)00400-6. [DOI] [PubMed] [Google Scholar]
- 23.Burks R.T., Leland R. Determination of graft tension before fixation in anterior cruciate ligament reconstruction. Arthroscopy. 1988;4(4):260–266. doi: 10.1016/s0749-8063(88)80041-0. [DOI] [PubMed] [Google Scholar]
- 24.Nurmi J.T., Kannus P., Sievanen H., Jarvela T., Jarvinen M., Jarvinen T.L. Interference screw fixation of soft tissue grafts in anterior cruciate ligament reconstruction: part 2: effect of preconditioning on graft tension during and after screw insertion. Am J Sports Med. 2004;32(2):418–424. doi: 10.1177/0363546503261703. [DOI] [PubMed] [Google Scholar]
- 25.Euguchi A., Ochi M., Adachi N., Deie M., Nakamae A., Usman M.A. Mechanical properties of suspensory fixation devices for anterior cruciate ligament reconstruction: comparison of the fixed-lengh loop device versus the adjustable-length loop device. Knee. 2014;21(3):743–748. doi: 10.1016/j.knee.2014.02.009. [DOI] [PubMed] [Google Scholar]
- 26.Rylander L., Brunelli J., Taylor M., Baldini T., Ellis B., Hawkins M. A biomechanical comparison of anterior cruciate ligament suspensory fixation devices in a porcine cadaver model. Clin Biomech. 2014;29(2):230–234. doi: 10.1016/j.clinbiomech.2013.11.001. [DOI] [PubMed] [Google Scholar]
- 27.Mayr R., Heinrichs C.H., Eichinger M., Coppola C., Schmoelz W., Attal R. Biomechanical comparison of 2 anterior cruciate ligament graft preparation techniques for tibial fixation: adjustable-length loop cortical button or interference screw. Am J Sports Med. 2015;43(6):1380–1385. doi: 10.1177/0363546515574062. [DOI] [PubMed] [Google Scholar]