Abstract
Objectives
This study is aimed at evaluating whether core decompression of the femoral head in the early stages of femoral head osteonecrosis improves patients’ subjective perception of pain and avoids the progression of the disease to a femoral head collapse and a final indication of total hip arthroplasty.
Methods
Eighteen patients (30 hips) in the early stages of the disease (Ficat and Arlet 1 and 2A) were evaluated through clinical, radiological, risk factor maintenance, and by the functional Merle D’Aubigné, and Postel score before and after core decompression of the femoral head.
Results
There was an improvement of symptoms up to the sixth month in 83.3% of the hips evaluated through the Merle D’Aubigné and Postel score. However, 73.3% of the cases evolved with femoral head collapse, and in 50%, total hip arthroplasty was indicated regardless of whether or not the risk factors were maintained.
Conclusions
Core decompression of the femoral head improves patients’ pain early in the initial stages of the pathology. However, it does not alter the prognosis and the ultimate indication of total hip arthroplasty in the final stages of the disease.
Keywords: Core decompression, Femur head necrosis/pathology, Femur head necrosis/physiopathology, Femur head necrosis/diagnosis, Treatment outcome
Resumo
Objetivos
O presente estudo tem como objetivo avaliar se a descompressão simples da cabeça femoral nos estágios iniciais da osteonecrose da cabeça femoral melhora a percepção subjetiva da dor dos pacientes e se evita a progressão da doença para o colapso da cabeça femoral e a indicação final de artroplastia total do quadril.
Métodos
Foram avaliados 18 pacientes (30 quadris) em estágios iniciais da doença (Ficat e Arlet 1 e 2A) por critérios clínicos, radiológicos, manutenção dos fatores de risco e pela escala funcional de Merle D’Aubigné e Postel antes e após a descompressão simples da cabeça femoral.
Resultados
Houve melhoria dos sintomas precocemente (até o sexto mês) em 83,3% dos quadris avaliados pela escala de Merle D’Aubigné e Postel. No entanto, 73,3% dos casos evoluíram com colapso da cabeça femoral e em 50% deles foi indicada artroplastia total do quadril, independentemente da manutenção ou não dos fatores de risco.
Conclusões
A descompressão simples da cabeça femoral melhora a dor dos pacientes precocemente nos estágios iniciais da patologia. Entretanto, não altera o prognóstico da doença e a indicação final de artroplastia total do quadril nos estágios finais da doença.
Palavras-chave: Descompressão da cabeça femoral, Necrose da cabeça do fêmur/patologia, Necrose da cabeça do fêmur/fisiopatologia, Necrose da cabeça do fêmur/diagnóstico, Resultado do tratamento
Introduction
Avascular osteonecrosis of the femoral head is a multifactorial condition whose pathophysiology is not very well defined.1, 2, 3 Numerous studies have been described to try to elucidate the pathology and prognosis of this disease, without much success.
It is a common finding in orthopedic practice, especially among hip specialists. The most affected age group comprises adults between the third and fifth decade of life; this condition has an evolving character, accounting for 5–18% of all total hip arthroplasty (THA) surgeries. Its main known etiologies are corticosteroid and alcohol use, trauma sequelae, and coagulation diseases; it is also commonly observed in patients with human immunodeficiency virus (HIV), systemic lupus erythematosus, and in those who have undergone organ transplantation and are using immunosuppressants.4 All factors lead to the trade of bone remodeling for bone resorption, which culminates in femoral head collapse.
The treatment of this pathology is not yet a consensus in the literature, but the majority of the studies decide treatment based on the presence or absence of collapse of the femoral head. In the early stages of the disease, when collapse has not yet occurred (classification Ficat and Arlet 1 and 2), one of the suggested treatments is the decompression of the necrotized area, with or without graft replacement, which may or may not be vascularized.5, 6, 7, 8, 9, 10, 11, 12, 13, 14, 15 This treatment can improve symptoms in up to 80% of cases, and is an attempt to delay disease progression. In these cases, the presence or absence of edema in magnetic resonance imaging (MRI) is not well correlated to symptom improvement.16 More conservative authors indicate the use of anticoagulants for preventing disease progression and avoiding a surgical procedure, which also presents positive results.17, 18, 19 Other studies assessed the efficacy of bisphosphonates in the prevention of femoral head collapse, with unsatisfactory results.20
The primary objective of the present study is to check whether there was any change in patients’ subjective perception of pain after the procedure.
The secondary objective was to compare symptom improvement or worsening among the osteonecrosis classifications and to verify whether the radiological progression of the disease and the Merle D’Aubigné and Postel functional score21 are associated with the assessed traits, mainly the persistence of risk factors.
Methods
The present study consists of a series of cases that is aimed at reporting the clinical and radiological results of cases of avascular osteonecrosis of the femoral head, regardless of etiology, treated with core decompression of the necrotic area. The present study was approved by the Ethics Committee (No. 2071224), and all patients signed an informed consent form.
All patients with osteonecrosis of the femoral head who had undergone core decompression within the last five years were included in the study. Patients who refused to participate, those with initial femoral head collapse (Ficat and Arlet stages 2 B, 3, and 4), those who did not have an adequate postoperative follow-up, and those who died of causes not related to this condition were excluded.
The protocol for core decompression of the femoral head consisted of placing the patient in a supine position on a radiolucent orthopedic surgical table and inserting a 2.5-mm guidewire into the femoral neck to the necrotic area, as identified on MRI, aided by fluoroscopy, and drilling the necrotic area with a cannulated 10-mm trephine, without graft replacement of any sort (Fig. 1). All patients in the postoperative period underwent the same rehabilitation protocol: no weight-bearing on the operated limb for three weeks, partial for another three weeks; after six weeks, total weight-bearing was permitted; pain was managed with simple analgesic and nonsteroidal anti-inflammatory drugs (NSAIDs) for 7 days, except in cases of contraindications.
Fig. 1.
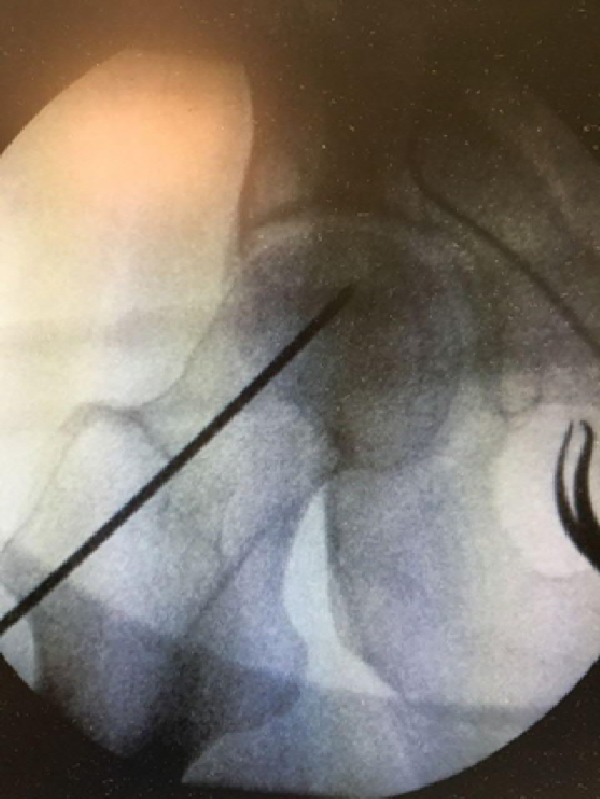
Positioning the guidewire in the femoral neck, toward the necrotic area.
The preoperative criteria were gender, age, osteonecrosis etiology, Ficat and Arlet stage, and Merle D’Aubigné and Postel functional score.
The postoperative criteria assessed in the present study were the subjective response of symptom improvement in the sixth postoperative month; hip joint pain was the main complaint assessed, and satisfaction with the surgery was measured in relation to pain. The mean follow-up time was 2.53 months. Post-maintenance of the etiologic factor, time until symptom improvement, radiological progression of the disease, and indication for THA (endpoint) were also evaluated.
Statistical analysis
After patient selection, 18 patients (30 hips) submitted to core decompression of the osteonecrotic area of the femoral head were evaluated. In 12 of them, simultaneous bilateral lesions were observed, occurring in the early stages of the disease (Ficat and Arlet 1 and 2A); bilateral decompression in a single surgical moment was indicated. In the others, unilateral decompression was indicated. The patients were categorized according to the radiological classification and causes of osteonecrosis (14 patients had a secondary cause – nine used corticosteroids, four had HIV, one had sickle cell anemia, and four patients had an idiopathic etiology).
The quantitative characteristics of the groups were described with summary measures (mean, standard deviation, median, and minimum and maximum), and the qualitative variables were described using absolute and relative frequencies.22 The pain score was described according to the osteonecrosis classification and the moment of evaluation; it was compared with the classifications and moments using generalized estimation with an interchangeable correlation matrix between the moments of evaluation, with Poisson marginal distribution and the identity link function.23 Femoral head collapses were described according to the characteristics of interest and the association with bivariate logistic regressions was studied.24 The change in the pain score between the assessment periods (final–initial) was recorded; the changes were described according to the persistence of risk factors. The alterations in the Merle D’Aubigné and Postel scores were compared between cases with and without persistence of risk factors using the Mann–Whitney test.22
A 5% significance level was adopted.
Results
The results are presented in tables that describe the characteristics of the patients, the Merle D’Aubigné and Postel scores, and the presence or absence of femoral head collapse and the indication for THA (Table 1, Table 2).
Table 1.
Description of the characteristics of the patients and the evaluated cases.
| Variable | Description |
|---|---|
| Age (years), mean ± SD | 43.6 ± 11.8 |
| Gender – n (%) | |
| Female | 7 (38.9) |
| Male | 11 (61.1) |
| Side, n (%) | |
| Right | 14 (46.7) |
| Left | 16 (53.3) |
| Ficat and Arlet, n (%) | |
| 1 | 11 (36.7) |
| 2A | 19 (63.3) |
| Early symptomatic improvement, n (%) | |
| No | 5 (16.7) |
| Yes | 25 (83.3) |
| THA indication, n (%) | |
| No | 15 (50) |
| Yes | 15 (50) |
| Persistence of risk factor, n (%) | |
| No | 12 (40) |
| Yes | 18 (60) |
| Head collapse, n (%) | |
| No | 8 (26.7) |
| Yes | 22 (73.3) |
| Merle d’Aubigne and Postel (pre) | |
| Mean ± SD | 10.4 ± 2.4 |
| Median (min; max) | 10 (7; 16) |
| Merle d’Aubigne and Postel (6 months) | |
| Mean ± SD | 13.9 ± 2.2 |
| Median (min; max) | 14 (10; 18) |
Table 2.
Description of the Merle D’Aubigné and Postel scores in each moment and according to the osteonecrosis classification, and comparative test results.
| Merle d’Aubigne and Postel | Ficat and Arlet |
P Classification | P Moment | P Hospitalization | |
|---|---|---|---|---|---|
| 1 (n = 11) | 2A (n = 19) | ||||
| Pre | 0.157 | <0.001 | 0.497 | ||
| Mean ± SD | 11.7 ± 2.9 | 9.7 ± 1.7 | |||
| Median (min; max) | 12 (8; 16) | 10 (7; 13) | |||
| 6 months | |||||
| Mean ± SD | 14.5 ± 2.3 | 13.6 ± 2.1 | |||
| Median (min; max) | 14 (11; 18) | 14 (10; 18) | |||
Generalized estimating equations with Poisson distribution.
Table 2 shows that there was a difference in the Merle D’Aubigné and Postel functional score only between the moments of evaluation (p < 0.001), regardless of the osteonecrosis classification; i.e., in general, in the sixth postoperative month, patients presented functional improvement compared to the preoperative period, but no difference was observed regarding the preoperative Ficat and Arlet score. The mean evolution of the Merle D’Aubigné and Postel functional score during the moments was statistically similar between the classifications (p = 0.497), and no difference between was observed the classifications (p = 0.157).
Table 3 showed an early improvement of the symptoms; it was observed that femoral head collapse directly influenced the indication of THA (p = 0.030). This result was observed after bivariate logistic regression. The persistence of risk factors (use of corticosteroids and other pathologies) was not statistically significant as a predisposing factor to functional score deterioration (Table 4) or radiological progression.
Table 3.
Description of femoral head collapse according to the characteristics of interest and result of association analyses.
| Variable | Head collapse |
OR | CI (95%) |
p | ||
|---|---|---|---|---|---|---|
| No (n = 8) | Yes (n = 22) | Inferior | Superior | |||
| Ficat and Arlet, n (%) | 0.088 | |||||
| 1 | 5 (45.5) | 6 (54.5) | 1.00 | |||
| 2A | 3 (15.8) | 16 (84.2) | 4.44 | 0.80 | 24.61 | |
| Early improvement of symptoms, n (%) | 0.466 | |||||
| No | 2 (40) | 3 (60) | 1.00 | |||
| Yes | 6 (24) | 19 (76) | 2.11 | 0.28 | 15.77 | |
| Indication of THA, n (%) | 0.030 | |||||
| No | 7 (46.7) | 8 (53.3) | 1.00 | |||
| Yes | 1 (6.7) | 14 (93.3) | 12.25 | 1.27 | 118.36 | |
| Persistence of risk factor, n (%) | 0.866 | |||||
| No | 3 (25) | 9 (75) | 1.00 | |||
| Yes | 5 (27.8) | 13 (72.2) | 0.87 | |||
| Alteration in the Merle d’Aubigne and Postel | 1.20 | 0.90 | 1.59 | 0.210 | ||
| Mean ± SD | 2.4 ± 3.2 | 3.9 ± 2.7 | ||||
| Median (min; max) | 3 (−4; 5) | 4 (−2; 7) | ||||
Multivariate logistic regression.
Table 4.
Description of changes in pain scores (Merle D’Aubigné and Postel) according to persistence of the risk factors and result of the comparative test.
| Persistence of risk factor |
p | ||
|---|---|---|---|
| No (n = 12) | Yes (n = 18) | ||
| Alteration in the Merle d’Aubigne and Postel | 0.325 | ||
| Mean ± SD | 4 ± 2.6 | 3.1 ± 3 | |
| Median (min; max) | 5 (−1; 7) | 4 (−4; 6) | |
Mann–Whitney test.
Table 4 indicates that there was no difference in the Merle D’Aubigné and Postel alterations between cases with and without persistence of risk factors (p = 0.325).
Discussion
Osteonecrosis is a condition of multifactorial and extensive etiology, which hinders the definition of a single and standardized treatment. The number of factors that impact this condition and its progressive characteristic have fostered the use of several techniques aiming at improving early symptoms and the progression of the bone pathology. These multifactorial aspects make it difficult to conduct an unbiased study with statistically significant results. This condition continues to be underdiagnosed in its initial phase; if an early diagnosis is made, decompression is a possible treatment option. If the diagnosis is made in advanced stages, with established femoral head collapse, the indicated treatment is THA.
This study was aimed at analyzing the characteristics of patients who underwent decompression in the last two years; all procedures were performed in the same way (guidewire placement in the femoral neck with fluoroscopic aid and drilling with a cannulated burr in the necrotic area). The authors believe that the symptoms may be related to the presence of bone edema, which was observed in all cases submitted to the procedure.25 A significant improvement of the patients’ early symptoms was observed in 83.3% of decompressed hips.
The score used for the evaluation of preoperative and postoperative pain did not present statistically significant alterations after six months, which indicates that the decompression treatment improves the early pain symptomatology, but does not alter the disease prognosis. This has been a challenge for hip surgeons, who have used new techniques associated with core decompression, such as the use of vascularized or non vascularized grafts,26, 27, 28 stem cell injection,29 shock waves, and anticoagulant drugs.30 Moreover, various techniques have been described using different types of drills and number of drillings. The results have been similar, with initial symptom improvement that does not influence disease progression.
The present study has some limitations that should be highlighted: the ideal would be to isolate a single risk factor and perform a long-term follow-up, in order to determine whether a specific treatment is effective, both for symptoms and for altering the natural course of the disease. Although all lesions were observed in the femoral head loading area, it was not possible to quantify the extent of the necrotic area and to correlate that finding with the prognosis. Furthermore, the presence of a conservative treatment control group would have contributed to clarifying the actual efficacy of core decompression of the femoral head.
As this was a retrospective study, with a survey of medical records of previously operated cases, both the creation of a control group and the analysis of a single risk factor were not possible.
The normal course of the disease, which leads to femoral head collapse, was observed in 73.3% of the cases; 50% of the cases presented THA indication due to pain complaints, with a mean time until THA indication of 1.13 years after femoral head core decompression. Similarly to studies conducted in other centers, even with decompression, the observed outcome was the natural progression of the disease in most cases.
Conclusion
Core decompression of the femoral head aids in the painful symptomatology in the short-term but does not appear to alter the progression of the bone lesion.
More studies are needed to determine the best type of treatment in the early stages of the disease, always with the ultimate goal of avoiding arthroplasty in young patients.
Conflicts of interest
The authors declare no conflicts of interest.
Footnotes
Study conducted at Grupo de Quadril, Instituto de Ortopedia e Traumatologia, Hospital das Clínicas, Faculdade de Medicina, Universidade de São Paulo, São Paulo, SP, Brazil.
References
- 1.Ficat R.P. Treatment of avascular necrosis of the femoral head. Hip. 1983:279–295. [PubMed] [Google Scholar]
- 2.Gou W.L., Lu Q., Wang X., Wang Y., Peng J., Lu S.B. Key pathway to prevent the collapse of femoral head in osteonecrosis. Eur Rev Med Pharmacol Sci. 2015;19(15):2766–2774. [PubMed] [Google Scholar]
- 3.Pouya F., Kerachian M.A. Avascular necrosis of the femoral head: are any genes involved? Arch Bone Jt Surg. 2015;3(3):149–155. [PMC free article] [PubMed] [Google Scholar]
- 4.Shah K.N., Racine J., Jones L.C., Aaron R.K. Pathophysiology and risk factors for osteonecrosis. Curr Rev Musculoskelet Med. 2015;8(3):201–209. doi: 10.1007/s12178-015-9277-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Hungerford D.S. Response: the role of core descompression in the treatment of ischemic necrosis of the femoral head. Arthritis Rheum. 1989;32(6):801–806. doi: 10.1002/anr.1780320623. [DOI] [PubMed] [Google Scholar]
- 6.Specchiulli F., Capocasale N., Laforgia R., Solarino G.B. The surgical treatment of idiopathic osteonecrosis of the femoral head. Ital J Orthop Traumatol. 1987;13(3):345–351. [PubMed] [Google Scholar]
- 7.Tooke S.M., Nugent P.J., Bassett L.W., Nottingham P., Mirra J., Jinnah R. Results of core decompression for femoral head osteonecrosis. Clin Orthop Relat Res. 1988;(228):99–104. [PubMed] [Google Scholar]
- 8.Warner J.J., Philip J.H., Brodsky G.L., Thornhill T.S. Studies of nontraumatic osteonecrosis. The role of core decompression in the treatment of nontraumatic osteonecrosis of the femoral head. Clin Orthop Relat Res. 1987;(225):104–127. [PubMed] [Google Scholar]
- 9.Chotivichit A., Korwutthikulrangsri E., Pornrattanamaneewong C., Achawakulthep C. Core decompression with bone marrow injection for the treatment of femoral head osteonecrosis. J Med Assoc Thai. 2014;97(Suppl 9):S139–S143. [PubMed] [Google Scholar]
- 10.Saito S., Ohzono K., Ono K. Joint-preserving operations for idiopathic avascular necrosis of the femoral head. Results of core decompression, grafting and osteotomy. J Bone Jt Surg Br. 1988;70(1):78–84. doi: 10.1302/0301-620X.70B1.3276703. [DOI] [PubMed] [Google Scholar]
- 11.Chotivichit A., Korwutthikulrangsri E., Auewarakul C., Sarirasririd S. Core decompression and concentrated autologous bone marrow injection for treatment of osteonecrosis of the femoral head. J Med Assoc Thai. 2012;95(Suppl 9):S14–S20. [PubMed] [Google Scholar]
- 12.Joint Surgery Group of the Orthopaedic Branch of the Chinese Medical Association Guideline for Diagnostic and Treatment of Osteonecrosis of the Femoral Head. Orthop Surg. 2015;7(3):200–207. doi: 10.1111/os.12193. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Wei M., Wang Z.G., Liu Y.J., Li Z.L. Drilling decompression for femoral head necrosis at collapse stage. Zhongguo Gu Shang. 2015;28(6):562–566. [PubMed] [Google Scholar]
- 14.Beckmann J., Roth A., Niethard C., Mauch F., Best R., Maus U. Bone marrow edema and atraumatic necrosis of the femoral head: therapy. Orthopade. 2015;44(9):662–671. doi: 10.1007/s00132-015-3146-4. [DOI] [PubMed] [Google Scholar]
- 15.Shah S.N., Kapoor C.S., Jhaveri M.R., Golwala P.P., Patel S. Analysis of outcome of avascular necrosis of femoral head treated by core decompression and bone grafting. J Clin Orthop Trauma. 2015;6(3):160–166. doi: 10.1016/j.jcot.2015.03.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kerimaa P., Väänänen M., Ojala R., Hyvönen P., Lehenkari P., Tervonen O. MRI-guidance in percutaneous core decompression of osteonecrosis of the femoral head. Eur Radiol. 2016;26(4):1180–1185. doi: 10.1007/s00330-015-3905-y. [DOI] [PubMed] [Google Scholar]
- 17.Papakostidis C., Tosounidis T.H., Jones E., Giannoudis P.V. The role of “cell therapy” in osteonecrosis of the femoral head. A systematic review of the literature and meta-analysis of 7 studies. Acta Orthop. 2016;87(1):72–78. doi: 10.3109/17453674.2015.1077418. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Wang C.J., Cheng J.H., Huang C.C., Yip H.K., Russo S. Extracorporeal shockwave therapy for avascular necrosis of femoral head. Int J Surg. 2015;24(Pt B):184–187. doi: 10.1016/j.ijsu.2015.06.080. [DOI] [PubMed] [Google Scholar]
- 19.Hong Y.C., Zhong H.M., Lin T., Shi J.B. Comparison of core decompression and conservative treatment for avascular necrosis of femoral head at early stage: a meta-analysis. Int J Clin Exp Med. 2015;8(4):5207–5216. [PMC free article] [PubMed] [Google Scholar]
- 20.Lee Y.K., Ha Y.C., Cho Y.J., Suh K.T., Kim S.Y., Won Y.Y. Does zoledronate prevent femoral head collapse from osteonecrosis? A prospective, randomized, open-label multicenter study. J Bone Jt Surg Am. 2015;97(14):1142–1148. doi: 10.2106/JBJS.N.01157. [DOI] [PubMed] [Google Scholar]
- 21.Ugino F.K., Righetti C.M., Alves D.P.L., Guimarães R.P., Honda E.K., Ono N.K. Evaluation of the reliability of the modified Merle d’Aubigné and Postel Method. Acta Ortop Bras. 2012;20(4):213–217. doi: 10.1590/S1413-78522012000400004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Kirkwood B.R., Sterne J.A.C. 2nd ed. Blackwell Science; Malden, MA: 2006. Essential medical statistics. [Google Scholar]
- 23.McCullagh P., Nelder J.A. 2nd ed. Chapman and Hall/CRC; Boca Raton, Fl: 1989. Generalized linear models. [Google Scholar]
- 24.Neter J., Kutner M.H., Nachtsheim C.J., Wasserman W. 4th ed. Irwin; Chicago: 1996. Applied linear statistical models. [Google Scholar]
- 25.Kubo Y., Yamamoto T., Motomura G., Tsukamoto N., Karasuyama K., Sonoda K. MRI-detected bone marrow changes within 3 weeks after initiation of high-dose corticosteroid therapy: a possible change preceding the subsequent appearance of low-intensity band in femoral head osteonecrosis. Rheumatol Int. 2015;35(11):1909–1912. doi: 10.1007/s00296-015-3346-6. [DOI] [PubMed] [Google Scholar]
- 26.Fontecha C.G., Roca I., Barber I., Menendez M.E., Collado D., Mascarenhas V.V. Femoral head bone viability after free vascularized fibular grafting for osteonecrosis: SPECT/CT study. Microsurgery. 2016;36(7):573–577. doi: 10.1002/micr.22452. [DOI] [PubMed] [Google Scholar]
- 27.Chen X.T., Tan X.Y., Liu Y.W., Zhang X.D., Liu L.Y., Jia Y.D. Application of minimally invasive, decompression bone graft implantation combined with metal trabecular bone reconstruction system for early stage osteonecrosis of femoral head. Zhongguo Gu Shang. 2015;28(5):422–425. [PubMed] [Google Scholar]
- 28.Chen X., Tan X., Gao S., Zhang X., Li J., Liu Y. Sartorius muscle-pedicle bone graft for osteonecrosis of the femoral head. Int Orthop. 2016;40(7):1417–1425. doi: 10.1007/s00264-015-2921-5. [DOI] [PubMed] [Google Scholar]
- 29.Tabatabaee R.M., Saberi S., Parvizi J., Mortazavi S.M., Farzan M. Combining concentrated autologous bone marrow stem cells injection with core decompression improves outcome for patients with early-stage osteonecrosis of the femoral head: a comparative study. J Arthroplasty. 2015;30(9 Suppl):11–15. doi: 10.1016/j.arth.2015.06.022. [DOI] [PubMed] [Google Scholar]
- 30.Albers A., Carli A., Routy B., Harvey E.J., Séguin C. Treatment with acetylsalicylic acid prevents short to mid-term radiographic progression of nontraumatic osteonecrosis of the femoral head: a pilot study. Can J Surg. 2015;58(3):198–205. doi: 10.1503/cjs.016814. [DOI] [PMC free article] [PubMed] [Google Scholar]


