To the Editor: Isolated adrenal metastasis from hepatocellular carcinoma (HCC) is reportedly of low incidence compared to metastasis to lung, bone or brain.1 We describe a case of hepatocellular carcinoma in a 53-year-old man who underwent left adrenalectomy for adrenal metastasis of hepatocellular carcinoma. Twenty-four months after curative radical hepatectomy for primary HCC and liver transplantation, a metastatic lesion of the left adrenal gland was detected during a routine radiological evaluation. A left adrenal resection was performed. Close follow up with imaging studies and monitoring of alpha-fetoprotein levels were clinically useful for early detection of isolated adrenal metastasis. Metastasis to the adrenal gland from HCC should be effectively managed and the appropriate surgical treatment selected if intrahepatic recurrence and/or other extrahepatic metastasis are controlled.
Our patient was a 53-year-old man who acquired hepatitis C virus in 1980 following blood transfusion during surgery for total hip replacement. By the late nineties, he had developed the symptoms and signs of liver cirrhosis with portal hypertension associated with ascites and recurrent episodes of upper gastrointestinal bleeding.
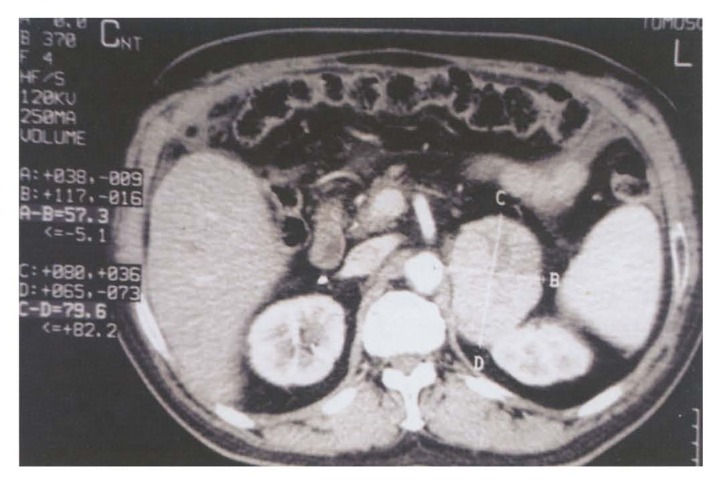
In February 1999, an ultrasound examination revealed a 3×3-cm mass in the right hepatic lobe. Laboratory studies showed normal liver function tests with an elevated alpha-fetoprotein (AFP) serum level of 756 ng/mL (normal value, <10 ng/mL). Computer tomography (CT) of the abdomen and pelvis revealed a 3.3×3-cm mass in the right hepatic lobe. In light of these findings and the history of hepatitis C virus infection, HCC was strongly suspected. A radical hepatectomy and liver transplantation was performed in 1999. Pathologic examination of the liver showed a single 3.3×3×2.7-cm nodule comprised of well-differentiated HCC, in association with cirrhosis. Post-operative AFP was in the normal range. The patient was followed up every 6 months with physical exam, AFP levels and CT-scan of the abdomen and pelvis. In February 2002, he presented for routine follow up. The AFP level had risen to 143 ng/mL. CT scan of the abdomen and pelvis revealed large 6×8-cm heterogeneous lesion in the left adrenal gland (Figure 1) that was not present on the previous examination six months earlier. This mass did not show any calcifications or enhancement after IV contrast administration. The above findings raised the possibility of metastasis versus primary adrenal malignancy.
Figure 1.
CT-scan of the abdomen showing a 6×8-cm heterogeneous mass in the left adrenal gland (AB × CD).
Pheochromocytoma was excluded based on laboratory tests. Fine needle aspiration under CT-guidance from the left adrenal gland was positive for metastatic HCC. After a complete metastatic work up including bone scan, the patient underwent left adrenal resection. Pathology revealed a well-differentiated metastatic HCC.
HCC is the most common solid organ tumor worldwide and the eighth most common malignancy.2 The incidence has increased over the past ten years. This increase is likely related to HCV infection.3 Total hepatectomy and liver transplantation is the most attractive treatment for resectable HCC. It entails removal of all the liver parenchyma that may potentially contain micrometastases. HCC tends to metastasize hematogenously to multiple foci. Distant metastases are usually detected at a mean of 7 months after radical resection of the primary tumor.4 Treatment of extrahepatic recurrences is important in prolonging survival in some patients. The most common sites of metastasis include lung, peritoneum, adrenal gland and bone. The adrenal gland is the second most common site of HCC metastasis in autopsied cases with the left adrenal gland being more commonly involved than the right and bilateral metastasis being less common than unilateral.1,5 In a series of 225 consecutive cases autopsied in 10 years, Nakashima et al found adrenal metastasis in 19 patients (8.4%).1 Aramaki et al followed 155 patients with HCC for extrahepatic recurrence after hepatectomy. Recurrences were found in 15 patients. Four patients had no intrahepatic recurrence and 11 patients had simultaneous intrahepatic recurrence. Location of metastases included lung, bone and adrenal glands.6
Clinical symptoms of adrenal metastasis are discovered late in the course either because of compressive symptoms, flank pain or adrenal insufficiency7–9 Detection of such metastasis in the early stage is difficult, resulting in delayed diagnosis and poor outcome. Close follow up by evaluation of tumor markers and diagnostic imaging is essential for the early detection of metastatic lesions. In our patient, detection was primarily due to a strict follow-up protocol with AFP repeated every 3 months and diagnostic imaging every 6 months. However, the tumor that was detected by a CT-scan 6 months later was a large 6×8-cm tumor. Therefore a combination of diagnostic imaging every three months and a tumor marker assay every month (not only AFP, but also des-gamma carboxy prothrombin (DCP) and AFP-L3% (lectin-reactive – fetoprotein) is necessary for early diagnosis of recurrence.
Treatment of extrahepatic recurrence of HCC is important in prolonging survival in some patients. For patients who present with extrahepatic metastasis coexisting with intrahepatic recurrence, intrahepatic recurrence should be controlled by locoregional therapy, and extrahepatic metastasis should be controlled by systemic chemotherapy and/or irradiation.6 Patients presenting with an isolated metastasis to the adrenal gland with no evidence of intrahepatic recurrence should be actively managed and the appropriate surgical treatment selected. Morimoto et al reported a case of HCC where asynchronous bilateral adrenalectomy was performed 15 and 25 months after curative resection of right hepatic lobe HCC. They recommended bilateral total adrenalectomy for such patients accompanied by postoperative hormonal supplementation.10
In conclusion, strict close follow-up examinations including tumor markers and diagnostic imaging are recommended in all patients treated for HCC for the early detection of intrahepatic recurrence and/or extrahepatic metastasis. Patients presenting with isolated adrenal metastasis with no intrahepatic recurrence should be treated by surgical resection. Long-term follow-up of a large number of cases is needed to clarify the clinical significance of this strategy and assess whether systemic chemotherapy is needed to eradicate micrometastases.
References
- 1.Nakashima T, Okuda K, Kojiro M, Jimi A, Yamagushi R, Sakamoto K, Ikari T. Pathology of hepatocellular carcinoma in Japan. Cancer. 1983;51:863–867. doi: 10.1002/1097-0142(19830301)51:5<863::aid-cncr2820510520>3.0.co;2-d. [DOI] [PubMed] [Google Scholar]
- 2.Chen CJ, Yu MW, Liaw YF. Epidemiological characteristics and risk factors of hepatocellular carcinoma. J Gastroenterol Hepatol. 1997;12 S:294–308. doi: 10.1111/j.1440-1746.1997.tb00513.x. [DOI] [PubMed] [Google Scholar]
- 3.El-Seraj HB, Mason AC. Rising incidence of hepatocellular carcinoma in the United States. N Engl J Med. 1999;340:745–750. doi: 10.1056/NEJM199903113401001. [DOI] [PubMed] [Google Scholar]
- 4.Lisker-Milman M, Martin P, Hoofnagle GH. Conditions associated with hepatocellular carcinoma. Med Clin North Am. 1989;73:999–1009. doi: 10.1016/s0025-7125(16)30650-2. [DOI] [PubMed] [Google Scholar]
- 5.Iwamoto S, Okuda K, Takeda N, Sonoda K, Sanefuji H. Case report: right-sided periadrenal metastasis supplied by the hepatic artery. Clues to the genesis of pedunculated hepatocellular carcinoma. J Gastroenterol Hepatol. 1997;19:62–66. doi: 10.1111/j.1440-1746.1997.tb00449.x. [DOI] [PubMed] [Google Scholar]
- 6.Aramaki M, Kawano K, Kai T, Yokoyama H, Morii Y, Sasaki A, Yoshida T, Kitano S. Treatment for extrahepatic metastasis of hepatocellular carcinoma following successful hepatic resection. Hepatogastroenterology. 1999;46:2931–2934. [PubMed] [Google Scholar]
- 7.Kuromatsu R, Hirai k, Majima Y, Fujimoto T, Shimauchi Y, Tsukiyama Y, Aoki E, Saitsu H, Nakashima O, Kojiro M. A patient with hepatocellular carcinoma who underwent resection of the primary lesion 10 years ago and resection of a giant adrenal metastasis 8 and half years later. Gastroenterol Jpn. 1993;28:312–6. doi: 10.1007/BF02779236. [DOI] [PubMed] [Google Scholar]
- 8.Otabe S, Muto S, Asano Y, Sato K, Ohtani N, Kawamoto C, Ido K, Kimura K. Hyperreninemic hypoaldosteronism due to hepatocellular carcinoma metastatic to the adrenal gland. Clin Nephrol. 1991;35:66–71. [PubMed] [Google Scholar]
- 9.Takamura T, Nagai U, Yamashita H, Nohara E, Ando H, Kagaya M, Urabe T, Kaneko S, Kobayashi K. Adrenal insufficiency due to metastatic hepatocellular carcinoma. Endocr J. 1999;46:591–6. doi: 10.1507/endocrj.46.591. [DOI] [PubMed] [Google Scholar]
- 10.Morimoto T, Honda G, Oh Y, Ozaki N, limura Y, Yamamoto Y, Sakai Y, Yamamoto M, Yamauchi A, Ikai I, Shimahara Y, Yamaoka Y. Management of adrenal metastasis of hepatocellular carcinoma by asynchronous resection of bilateral adrenal glands. J Gastroenterol. 1999;34:132–7. doi: 10.1007/s005350050229. [DOI] [PubMed] [Google Scholar]