Abstract
BACKGROUND
High resolution computerized tomography (HRCT) is valuable for detection of early erosive changes suggestive of cholesteatoma. The aim of our study was to determine characteristic CT findings in patients with middle ear cholesteatoma.
METHODS
We conducted a retrospective review of CT scans and surgical and histopathological reports in 64 patients with middle ear cholesteatoma (35 male, 29 female; age range, 7–80 years, median age, 22 years). CT scans were evaluated for the presence of intra-tympanic non-dependent soft tissue density, the extent of middle ear involvement, bone expansion and thinning, and bone erosions involving the ossicles and adjacent structures.
RESULTS
Middle ear cholesteatoma was more common in male patients and in patients aged 20–35 years. All patients had soft tissue density in the middle ear. Fifty-nine (92%) had expansion of the aditus and mastoid antrum, 59 (92%) had erosions of the ossicles, with involvement of the long process of the incus in 48 (75%), 55 (86%) had an eroded scutum, 55 (86%) an eroded facial nerve canal, 57 (89%) an eroded Koerner’s septum, which was totally destroyed in 19 (27%), 48 (75%) had tegmen erosion, and 63 (98%) had erosions of the antral walls. The correlation of pre-operative CT with surgical and histopathological findings was 97%.
CONCLUSION
Middle ear cholesteatoma is a distinct clinical entity with characteristic findings that may be suggested by CT imaging. These findings should alert the clinician to the possibility of cholesteatoma, which will guide in the surgical approach and treatment plan.
Keywords: Temporal bone, cholesteatoma, CT
Middle ear cholesteatoma, which is more often acquired than congenital, has been recognized clinically and radiologically for many years.1,2,3 Acquired cholesteatoma is the main complication of chronic otitis, resulting from ingrowth of the keratinizing squamous epithelium, from the external acoustic meatus to the middle ear through the tympanic membrane.1,3 The hallmarks of cholesteatoma are a soft tissue mass-like opacity in the middle ear cavity and mastoid antrum associated with smooth bony erosion of the ossicles and expansion of adjacent structures.4 The radiographic appearance of the soft tissue itself does not differ, whether it is cholesteatoma or granulation tissue, but the association of bone erosion is highly suggestive of cholesteatoma. The absence of abnormal soft tissue on CT essentially excludes cholesteatoma.5 To minimize the interpretative errors of mild bone erosions, particularly the tegmen, the lateral semicircular canals and horizontal portion of the facial nerve canal, familiarity with the radiographic variations and comparison with the normal side are valuable.5,6 High resolution computerized tomography (HRCT) is most valuable for detection of early erosive changes in the ossicles, particularly in the smaller parts such as the incudostapedial junction, as well as in the detection of non-dependent soft tissue opacification suggestive of cholesteatoma. The purpose of our study was to review the computed tomography (CT) findings in patients with surgically proved middle ear cholesteatoma in an attempt to determine characteristics suggestive of the disease entity.
Methods
We retrospectively reviewed CT scans and compared them with surgical and histopathological results in 64 patients with middle ear cholesteatoma (35 male, 29 female; median age, 22 years; mean age, 36.5 years; age range, 7–80 years). The criteria for diagnosis were chronic intermittent aural discharge associated with either a marginal tympanic membrane perforation or a tympanic membrane inadequately visualized owing to the presence of granulations or squamous debris in the external auditory meatus.5
The radiologic demonstration of the different disease manifestations and anatomical changes necessitated high resolution computed tomography (HRCT) technique. Scans were performed along the axial and direct coronal planes in all cases. Non-contrast CT was adequate. However, intravenous contrast medium was given in some patients when brain extension was suspected. Scans were done using the Siemens Somatom Volume Zoom. Parameters applied included 512 matrix, 200 field of view, 1-mm section thickness (contiguous slices), fast scan mode, beam hardening correction, 120 KV, 150 mA exposure, with approximately 25 slices performed per examination. The operative reports of these patients were compared with the pre-operative CT scans in order to correlate the following features:4 location and extension of cholesteatoma, erosion of the ossicular chain, integrity of the facial nerve, integrity of the semi-circular canals, integrity of the tegmen, and extension of cholesteatoma outside the middle ear. In addition, integrity of mastoid air cells, trabeculae, petrosquamosal (Koerner’s) septum, as well as changes in the tympanic membrane were similarly assessed. The CT studies were correlated with surgical and histo-pathological reports in all patients.
Results
Clinical findings in our series showed that middle ear cholesteatoma was more common in male patients. The disease was bilateral in 25 cases (39.06%), 20 (31.25%) were left-sided, and 19 (26.69%) right-sided. The presenting clinical complaints were non-specific and consisted mainly of chronic otomastoiditis. Ten (15.63%) patients with more advanced disease also presented with vertigo, but only 4 (6.25%) were found to have labyrinthine fistula, owing to the invasion of the disease into the otic capsule. There were 3 (4.68%) who has neurological symptoms due to intra-cranial extension of the disease; all developed brain abscess.
CT findings
Soft tissue density
Acquired cholesteatomas are characterized on CT by the presence of a non-dependent, homogeneous soft tissue mass with a focal area of bone destruction.7 In the majority of our cases, this soft tissue density had mass-like features (Figures 1–7). The tissue masses were homogeneous in 62 cases (96.87%), polypoidal in 48 (75%), non-dependent in 63 (98.44%), and expansile (smooth bony expansion of the attic and mastoid antrum) in 59 (92.20%). The mass subtotally occupied the middle ear cavity and antrum in 52 cases (81.25%). Only a few (n=7, 11%) of these soft tissue densities had totally filled the whole middle ear cavity, or were focally localized to the attic and mastoid antrum (n=5, 7.81%).
Figure 1.
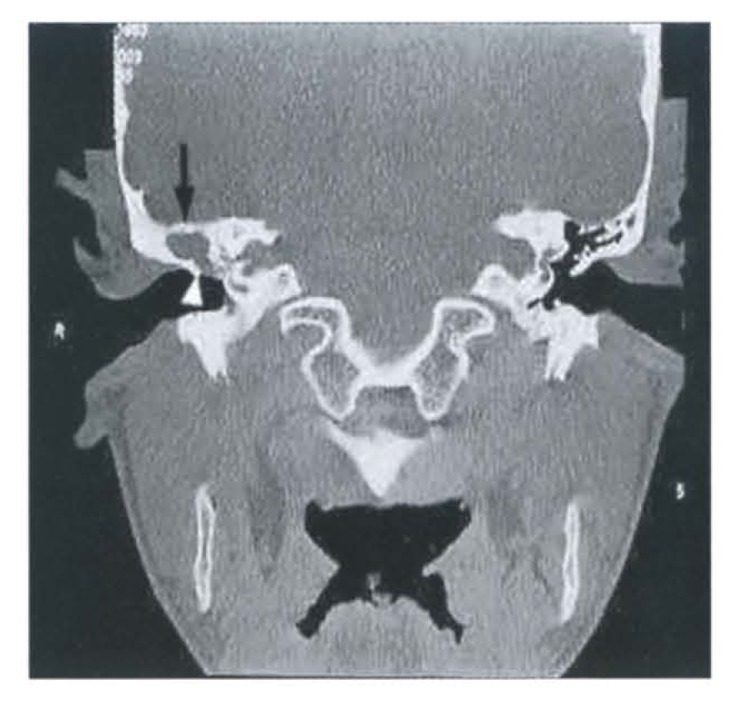
Coronal plane. The right mastoid is acellular and sclerotic. Soft tissue mass is seen in the mastoid antrum, aditus ad antrum and mesotympanum. Scutum (spur) is blunted (white arrowhead), tegmen is intact (arrowed), but Koerner’s septum is eroded. Note the absence of ossicles due to cholesteatoma. The left side is normal.
Figure 2.
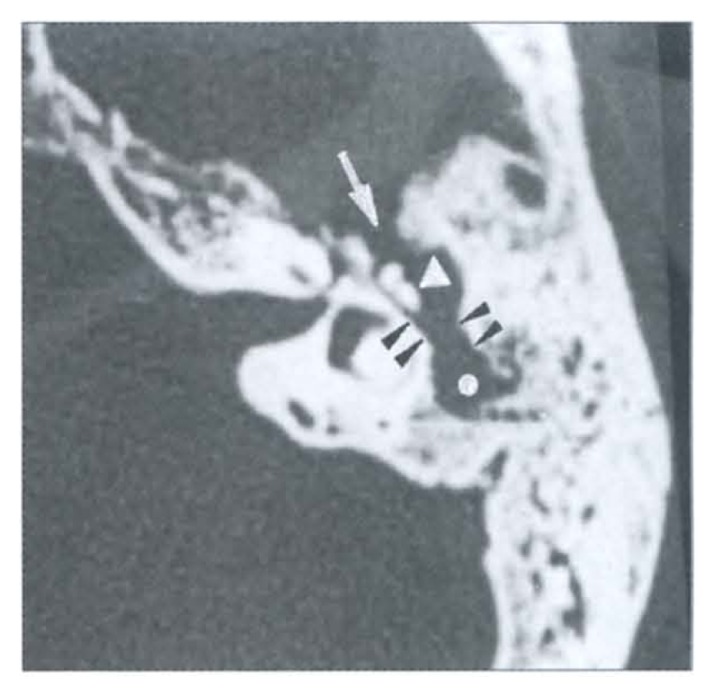
Axial image of left temporal bone demonstrates soft tissue mass (white dot) clearly displacing the malleo-incudal complex medially (white arrowhead). The left mastoid is markedly sclerotic and thickened with very few atrophic air cells. Aditus ad antrum is widened with loss of “figure of 8” (double black arrowheads). A bone defect is seen in the tegmen anteriorly (white arrow). Koerner’s septum is gone.
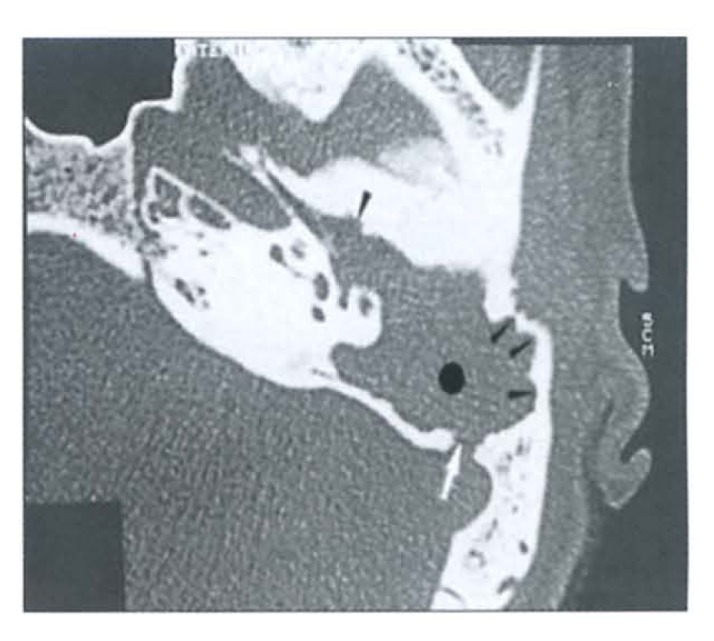
Figure 3.
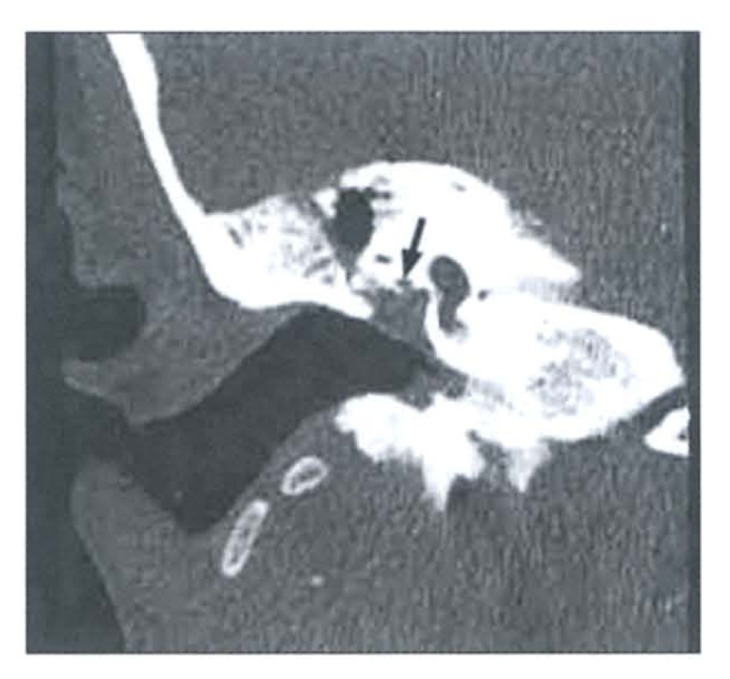
Aggressive acquired cholesteatoma. Coronal image demonstrates mass in direct apposition to tympanic segment of facial nerve canal (arrowed). A small wall defect is noticeable inferiorly. Bone sclerosis and few atrophic mastoid air cells are present. Trabeculations are intact.
Figure 4.
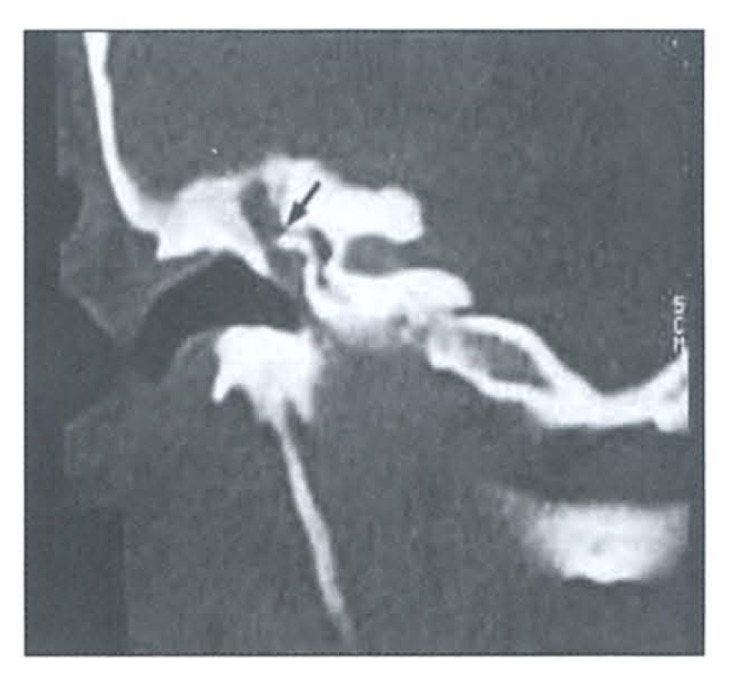
Erosive cholesteatoma. Coronal image demonstrates soft tissue densifications of the middle ear cavity. Ossicles are totally destroyed. There is a labyrinthine fistula (arrowed). Marked sclerosis of an acellular temporal bone is noticeable. Tympanic membrane is thickened and partially obliterated.
Figure 5.
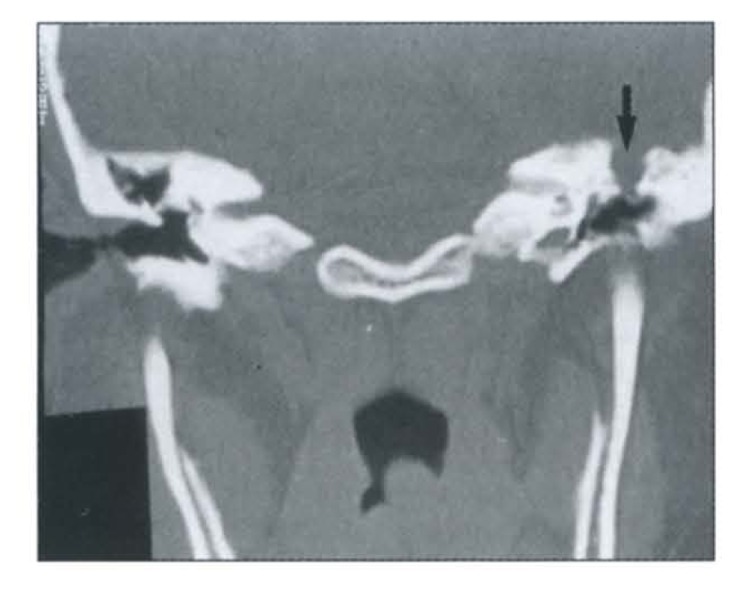
Coronal CT scan of the temporal bones. Cholesteatoma is present in the left side with defective tegmen (arrowed).
Figure 6.
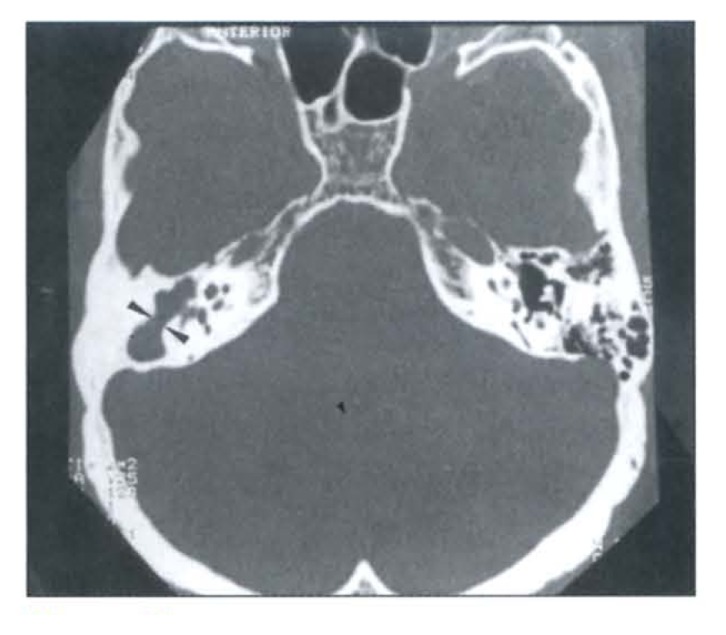
Axial CT image demonstrates an acquired cholesteatoma on the right side. There is a partial loss of “figure of 8” (double arrowheads), absence of ossicles, Koerner’s septum, trabeculae and air cells. The left side is normal. A normal Koerner’s septum is seen as a short linear structure at the middle of the left mastoid antrum.
Figure 7.
Erosive cholesteatoma. Axial image demonstrates expansile soft tissue mass (dotted) with scalloped smooth eroded walls (small arrowheads) of the attic and antrum. There is a posterior defect involving the left sigmoid sinus plate (white arrow). The ossicles are absent and extension of the disease to the protympanum is depicted. Eustachian tube is obstructed.
Ossicular chains
Erosion of the ossicles is commonly seen with cholesteatomas, as they enlarge and come in contact with contiguous structures in the middle ear.8–10 Of the 59 (92.19%) cases with ossicular erosions, the incus was mostly affected (n=48, 75%) (the long process of the incus was the most commonly eroded). The stapes, the second most affected ossicular bone (n=42, 65.62%), was also totally eroded. In the remaining cases (n=28, 43.75%), the stapes was seen but was apparently masked by the surrounding soft tissue density of the cholesteatoma. Although the malleus was the least affected bone by erosion (n=26, 40.64%), its erosions were the most easily observable finding (Figure 1). In our review, 14 cases (21.87%) showed lateral displacement and 9 cases (14.06%) exhibited medial shifting (Figure 2).
Facial nerve canals
HRCT findings are usually straightforward, but in the diseased middle ear the soft tissue densities may about the tympanic part of the facial nerve canal. To clearly visualize this part of the canal, coronal images must be meticulously analyzed. Of the 64 cases we found, 18 (28%) involvement with 15 (23.44%) partially eroded (Figure 3), and 3 (4.69%) were totally destroyed.
Semicircular canals
Due to its anatomically close proximity to the medial wall of the attic, the lateral semicircular canal is the most frequently eroded.1,4,10,11 However, a false impression of the canal fistula may be encountered. Thus, axial CT sections must be reinforced by coronal images for evidence of cortical thinning.4,12
One persistent complication of cholesteatoma is invasion of the labyrinth. The incidence of labyrinthine fistula secondary to cholesteatoma has remained relatively constant over the last 50 years.13,14 A fistula has been defined as invasion of the bony otic capsule.13 By far the most commonly compromised region is the lateral semicircular canal. The diagnosis of fistula can be made when the mass is in direct apposition to the membranous portion of the labyrinth. Careful evaluation on both axial and coronal images for evidence of cortical thinning in all patients with middle ear disease is necessary.12 We have encountered a total of 9 cases (14%) involving the lateral semicircular canals, 4 (6.25%) positive for labyrinthine fistula and 5 (7.81%) partially eroded (Figure 4).
Tegmen
Overlying the epitympanum and antrum, the tegmen is a thin bony roof that is clearly visualized on coronal sections. In 46 cases (71.87%), partial erosions were seen and 2 (3.13%) were positive for dehiscence (tegmental bone defect) (Figures 2, 5). In the remaining 16 (25%), the tegmen was intact.
Scutum (spur)
The bony scutum marks the lateral border of the Prussak’s space (between the malleoincudal complex and inferolateral wall of the attic). 12 Involvement of the scutum was present in 55 cases (86%) in our series. Forty cases (62.50%) were blunted (Figure 1) and 15 (23.4%) were destroyed. Few cases (n=9, 14.06%) were intact.
Aditus ad antrum
A superoposterior communication between the attic and the mastoid antrum is called the aditus ad antrum. When cholesteatoma is present, it may erode its wall and widen the “waistline” (aditus) resulting in the loss of the “figure of 8”.4 There were 55 cases (67%) of involvement noted, 25 (39.06%) with loss of “figure of 8” and 18 (28.13%) of these had wall erosions (Figures 2, 6).
Petrosquamosal septum (Koerner’s Septum)
The petrosquamosal septum is a pointed bony projection directed obliquely downward and forward, originating from the antral roof. An antral cholesteatoma usually erodes this thin structure. In our series, there were 57 cases (89%), with 38 (59.38%) partially eroded and 19 (29.68%) completely destroyed (Figures 1, 2, 6). In only 5 cases (7.81%) was the septum preserved.
Mastoid air cells
Chronic otomastoiditis and tympanic membrane perforation are associated with acquired cholesteatoma. In all 64 (100%) cases, the affected mastoids were all sclerotic due to chronic infection. The majority, 43 cases (67.18%), were acellular (Figures 1, 4, 5, 6) and 21 cases (32.81%) had few and atrophic air cells, 20 (31.25%) of which were opaque while in only 1 case (1.56%) were the air cells clear but with thickened walls (Figures 2, 3).
Mastoid Antrum
In our series, the antra were replaced by soft tissue densities in 55 cases (85.94%), while 48 cases (75%) were expanded (Figures 1, 2, 6, 7) and 15 cases (23.43%) showed partial smooth bony erosions.
Extensions
Several spaces may be involved in extensions. In the Eustachian tube, persistence of inflammation in the protympanic mucosa may project downward to the isthmus and lead to eustachian tube dysfunction. This is thought to be a possible pathogenesis of cholesteatoma.15,16,17 In our series, 48 cases (75%) were obstructed (Figure 7). The remaining 16 (25%) remained patent and clear. We also had extensions in the facial recess in 49 cases (77%) (Figure 7), in the tympanic recess (sinus tympani) in 45 cases (70%), in the protympanum in 41 cases (41%) (Figure 7), and in the external auditory canal in 14 cases (22%). The measurement of CT density values was found to be of little use because the CT findings were similar in cholesteatoma, granulation tissues, and mucosal edema or effusion. Therefore, they may be indistinguishable on CT scanning, 7,18,19,20 unless an air-fluid level can be seen in the case of middle ear effusion.
Extension beyond the middle ear
Complications of cholesteatoma, even in the mildest form, will compromise quality of life and if left unrecognized or untreated may result in death.21 Complications are related to osseous destruction, which may lead to serious and potentially fatal intracranial conditions. The mechanism of bone destruction by cholesteatoma is explained by the pressure of the matrix of the cholesteatoma and by enzymatic bone resorption.22,23 Our analysis found 3 cases with brain abscesses. Two of these were found to have destruction of the tegmen and the third occurred as a result of a defect in the sigmoid sinus plate (Figure 7).
Tympanic Membrane
Although otoscopic examination is unquestionably efficient in the assessment of the tympanic membrane, we also found that 48 cases (75%) were thickened and 39 (61%) associated with retraction. The remaining 13 (30.31%) were obliterated by soft tissue densities (Figures 3, 4), 2 (3.13%) showed bulging and 1 case (1.56%) was totally absent.
Automastoidectomy
The contents of an acquired cholesteatoma may drain externally, leaving only the aggressive peripheral microscopic membrane that consists of keratinizing stratified squamous epithelium. No soft tissue mass is seen in the imaging and the CT appearance is reminiscent of mastoidectomy. This is the so-called automastoidectomy (mural cholesteatoma).12 Only 1 case (1.56%) occurred in our series.
Trabeculations
In 29 cases (45.31%) trabeculations were destroyed due to the expansile nature of the cholesteatoma. In 20 cases (31.25%) they were eroded and in 13 (20.31%) obliterated (Figures 2, 4, 5, 6). Obliteration was mainly due to sclerosing mastoiditis. Occasionally trabeculae may remain intact and 2 cases (3.13%) were seen in our analysis (Figure 3).
Comparative analysis
The analysis of pre-operative HRCT scans correlated with the surgical findings and histopathologic reports with a high degree of accuracy (96.88%) (Table 1). Of 64 cases, evaluation of the malleus was in agreement with the postoperative results in 60 cases (94%). In 4 cases, no erosions were seen in HRCT but erosions were found in surgery, but this was due to the long interval between the pre-operative HRCT and the day of actual surgical intervention. In the assessment of the incus, 61 cases (96%) matched with the operative findings. Subtle erosions in 3 cases seen in CT images were found to be negative in surgery. The stapes showed agreement in 59 cases (92%) in both pre-operative scans and surgical results. Of the 28 cases (43.75%) with an unclear degree of erosion in HRCT scans (due to being masked by the surrounding soft tissue density), the surgical reports indicated total destruction of the stapes in 26 cases (40.63%) while 2 (3.13%) were severely eroded. The remaining 5 cases (7.81%) showed subtle erosions as analyzed in HRCT, but were found normal in surgery. The HRCT-surgical evaluation of the lateral semicircular canal revealed 63 cases (94.44%) in agreement. In both, partial erosions were seen in 5 cases (7.81%). There were 4 cases (6.25%) that had labyrinthine fistula in HRCT but only 3 (4.69%) were in agreement with the surgical findings. However, the post-operative report stated that the remaining case (1.56%) had marked erosion with dehiscence.
Table 1.
Pre-operative CT, surgical and histopathological correlation.
| Diagnosis | Pre-op ct | Surgery | Histopath |
|---|---|---|---|
| Cholesteatoma | 62 | 61 | 60 |
| Cholesteatoma and/or polyp | 1 | ||
| Cholesteatoma and tympanosclerosis | 1 | ||
| Tympanosclerosis with inflammatory polyp | 1 | 1 | |
| Granulation tissues (pure) | 1 | ||
| Aural polyp | 2 | 2 | |
| TOTAL | 64 | 64 | 64 |
Pre-operative demonstration of facial nerve canal involvement was often difficult not only because of its small size but due to its oblique orientation (tympanic portion) and the presence of developmental dehiscence, particularly when abutted by the soft tissues. The usefulness of the coronal planes are very important in doubtful cases. In our series, 55 cases (86%) had CT-surgical agreement. In partially eroded canals, 15 (23.44%) positive cases were shown by CT. Only 7 cases (10.94%) were noted in surgery, 2 (3.13%) of which had dehiscence. The other 8 cases with very subtle marginal irregularities in HRCT were negative in surgery. In 3 cases (4.69%) with facial nerve canal destruction, 2 (3.13%) had similar changes in surgery while in 1 (1.56%) more than 50% dehiscence was reported in surgery.
Complete agreement was noted in the three patients with brain abscess and in one case of automastoidectomy. In two cases with brain abscess the points of otogenic extension were through the defect in the tegmen tympani and the other one was via a defect in the eroded sigmoid sinus plate.
Discussion
The diagnosis of cholesteatoma is usually made on otologic examination.2,4,24–26 In cases in which the diagnosis is not obvious, computerized tomography may demonstrate a soft tissue mass with characteristic ossicular displacement and erosion of bone. Cholesteatoma in hidden areas, such as the posterior tympanic recess, may be revealed by a CT scan even if it is not detected by otologic examination. A CT scan also provides information about congenital anatomic variations that may be encountered during surgery, as well as the complications of cholesteatoma.4 Years of experience with HRCT have clearly demonstrated its superiority for the evaluation of the temporal bone, particularly utilizing the thin-section, high-resolution techniques. HRCT provides a more precise definition of the anatomic extent of the disease of the middle ear and the relationship of these cholesteatoma masses to the contiguous structures. Comparison with the normal is useful in doubtful cases.
The hallmarks of cholesteatoma are the presence of soft tissue density in the middle ear cavity, ossicular erosions, smooth erosions of the middle ear borders and adjacent structures. These changes, when associated with bony expansion of the middle ear cavity, are highly suggestive of cholesteatoma. However, they are not specific as other mass lesions like ectopic meningioma may simulate this finding and cannot be differentiated from cholesteatoma.4,7
Our investigation demonstrates that the CT findings that may suggest a diagnosis of middle ear cholesteatoma consist of non-dependent polypoidal soft tissue densification of the middle ear cavity and antrum (focal, partial or total), with associated expansion and smooth erosion of the walls, ossicular displacement and erosions. These features are similar to those described in the literature.4, 7 Because they are commonly a complication of chronic mastoiditis, there is almost always co-existing inflammatory disease with adjacent mastoid air cells.7 Our study demonstrates this in all patients.
When the air cells appear “cloudy” but maintain their irregular trabecular pattern, or whenever there is obliteration of mastoid antrum and periantral cells by increased reactive bone formation, chronic mastoiditis without cholesteatoma is indicated.4 Complete opacification of the middle ear with no bony destruction makes radiologic differentiation of cholesteatoma from middle ear effusions and granulation tissue difficult, if not impossible.7,27 The presence of an air-fluid level or a soft tissue (fluid) mass in the dependent portion of the middle ear would render support to a diagnosis of effusion.7 In cases where the antrum was enlarged with an air-fluid level, this finding was suggestive of infected cholesteatoma.4
In our series, non-dependent, homogeneous and polypoidal soft tissue densities were present in the mastoid antrum and middle ear cavity. In the majority of cases, soft tissues occupied all spaces at the time of CT study. Many of the patients had both granulation tissue and cholesteatoma, which could not be radiographically distinguished.4
Cholesteatoma in the antrum is characterized by a smooth cavity that is usually larger than normal owing to bone erosion. Because considerable anatomic variations exist in the normal side, it is important to compare the diseased ear with the uninvolved side. Another sign of antral cholesteatoma is erosion or absence of the bony partition known as the Koerner’s septum.4 Out of 64 cases, 57 (89%) in our series demonstrated such involvement.
Signs indicating cholesteatoma in the attic include Erosion or destruction of scutum or spur (the lateral wall of the attic) (Figure 1), widening of the aditus ad antrum (loss of figure of “8” appearance) (Figure 2, 6), antral wall erosions and widening (Figures 2, 6), ossicular erosions and destruction (Figures 4, 6), medial attic wall erosion which may lead to facial nerve canal involvement, which may cause paresis or paralysis (Figure 3), erosion of the lateral semicircular canal which may result into fistula formation (Figure 4), dehiscence of tegmen tympani (Figures 2, 5), dehiscence of sigmoid sinus plate (Figure 7), erosion of the external auditory canal (EAC), and automastoidectomy. CT will reliably detect but not always characterize disease. Unfortunately, cholesteatoma sac, associated granulation tissue, mucosal edema and effusion may be indistinguishable on CT scanning.4,18 Although cholesteatoma is said to show a lower attenuation than granulation tissue, the difference is subtle and only magnetic resonance imaging can differentiate the two. After clinical examination, otoscopy and a diagnosis of cholesteatoma, CT can determine its extent by revealing a soft tissue mass and bone erosion, with 80% specificity.18 Although otoscopic recognition of cholesteatoma is often reliable, imaging modalities should be used on all patients suspected of harboring a cholesteatoma to determine the presence of gross or subtle changes and the presence of complications, which are mostly due to bone erosions. The specific issues that must be assessed on imaging studies and that will affect the surgical treatment are bone erosion and the degree of extension. CT is sensitive for the detection of early bone erosions and detailed imaging of the soft tissue extent of middle ear cholesteatoma provides information that may affect their surgical resection.
In summary, in our cases HRCT enabled the pre-operative delineation of the cholesteatoma and the recognition of its manifestations and complications. The proximity of these soft tissue masses to the neighboring structures and facial nerve is best appreciated when the area is viewed in axial and coronal sections using 1×1 mm (HRCT). Excellent contrast between bone, air and soft tissues can be demonstrated. On imaging of the cholesteatoma, the presences of a soft tissue densification with bone erosions and an expansile effect on the adjacent bony borders of part or all of the middle ear cavity or air cells is considered diagnostic. In addition, the demonstration of the characteristic appearance of the cavity may be pathognomonic. Our study showed excellent correlation between the preoperative HRCT scans, the surgical and the histopathological findings in cholesteatoma cases. HRCT is confirmed to be valuable in the diagnosis and in guiding the surgical management of cholesteatoma. Also, the role of HRCT early in the course of the disease can potentially reduce the risks of late complications associated with underdiagnosed cholesteatoma. CT imaging has proven to be an accurate method of depicting the characteristic findings of middle ear cholesteatoma, including the extent and complications. Therefore, HRCT is the method of choice for the examination of the middle ear structures and pathology such as cholesteatoma. Our results are consistent with those of previously recognized series and suggest that the diagnosis of middle ear cholesteatoma may be indicated by certain characteristic findings in CT.
Acknowledgment
We thank Beltran Bacsid and Fikri Hassan for their meticulous computed tomographic technique and Ma. Corazon Braza for her valuable secretarial assistance.
References
- 1.Robert Y, Dubrule F, Carcasset S, et al. Petrous bone extension of middle ear acquired cholesteatoma. Acta Radiologica. 1996;37:166–170. doi: 10.1177/02841851960371P134. [DOI] [PubMed] [Google Scholar]
- 2.Phelps PD, Lloyd GAS. The radiology of cholesteatoma. Clin Radiol. 1980;31:501–512. doi: 10.1016/s0009-9260(80)80034-1. [DOI] [PubMed] [Google Scholar]
- 3.Swartz JD. Cholesteatoma of the middle ear, diagnosis, etiology and complications. Radiol Clin North Am. 1984;22:15. [PubMed] [Google Scholar]
- 4.Mafee MF, Levin BC, Applebaum EL, Campos CF. Cholesteatoma of the middle ear and mastoid. Otolaryngol Clin North Am. 1988;21:265–268. [PubMed] [Google Scholar]
- 5.Leighton SEJ, Robson AK, Anslow P, Milford CA. The role of CT imaging in the management of chronic suppurative otitis media. Clin Otolaryngol. 1993;18:23–29. doi: 10.1111/j.1365-2273.1993.tb00804.x. [DOI] [PubMed] [Google Scholar]
- 6.Jackler RK, Dillon WP, Schindler RA. Computed tomography in suppurative ear disease: a correlation of surgical and radiographic findings. Laryngoscope. 1984;94:746–752. doi: 10.1288/00005537-198406000-00004. [DOI] [PubMed] [Google Scholar]
- 7.Liu DPC, Bergeron RT. Contemporary radiologic imaging in the evaluation of middle ear-attic-antral complex cholesteatomas. Otolaryngol Clin North Am. 1989;22:897–909. [PubMed] [Google Scholar]
- 8.Ishii K, Takahashi S, Matsumoto K, Kabayashi T, et al. Middle ear cholesteatoma extending into the petrous apex: evaluation by CT and MR imaging. Am J Neuroradiol. 1991;12:719–724. [PMC free article] [PubMed] [Google Scholar]
- 9.Valvassori GE, Buckingham RA. Radiology of the temporal bone. In: Valvassori GE, Buckingham RA, Carter BL, et al., editors. Head and Neck Imaging. Stuttgart: Thieme; 1988. pp. 1–172. [Google Scholar]
- 10.Silver AJ, Janecka I, Wazen J, et al. Complicated cholesteatomas: CT findings in inner ear complications of middle ear cholesteatomas. Radiology. 1987;164:47–51. doi: 10.1148/radiology.164.1.3588926. [DOI] [PubMed] [Google Scholar]
- 11.Johnson DW, Voorhess RL, Lufkin RB, Hanafee W, Canalis RF. Cholesteatomas of temporal bone: role of computed tomography. Radiology. 1983;148:733. doi: 10.1148/radiology.148.3.6878694. [DOI] [PubMed] [Google Scholar]
- 12.Swartz JD. Inflammatory disease of the temporal bone. In: Som PM, Bergeron RT, editors. Head and Neck Imaging. St. Louis: Mosby; 1991. pp. 993–1027. [Google Scholar]
- 13.Herzog JA, Smith PG, Kletzker GR, Maxwell KS. Management of labyrinthine fistulae secondary to cholesteatoma. Am J Otology. 1996;17:410–415. [PubMed] [Google Scholar]
- 14.McCabe BF. Labyrinthine fistula in chronic mastoiditis. Ann Otol Rhinol Laryngol. 1984;93(suppl 112):138–141. doi: 10.1177/00034894840930s424. [DOI] [PubMed] [Google Scholar]
- 15.Chao WY, Chang SJ. Ultrastructure of eustachian tube mucosa in chronic otitis media with cholestetaoma. Am J Otolaryngol. 1996;17:161–166. doi: 10.1016/s0196-0709(96)90054-x. [DOI] [PubMed] [Google Scholar]
- 16.Bluestone CD, Casselbrant ML, Cantekin EI. Funtional obstruction of the eustachian tube in the pathogenesis of aural cholesteatoma in children. In: Spade J, editor. Cholesteatoma and mastoid surgery. Amsterdam: Kugler Publications; 1982. pp. 211–224. [Google Scholar]
- 17.Chao WY. Eustachian tube dysfunction in the pathogenesis of middle ear cholesteatoma: clinical considerations. In: Hsien T, editor. Proceedings of the second sino-Japanese Otolaryngology-Head and Neck Surgery Academic Conference; Taipei, Taiwan. 1993. pp. 42–43. [Google Scholar]
- 18.Watts S, Flood LM, Clifford KA. Systematic approach to interpretation of computed tomography scans prior to surgery of middle ear cholesteatoma. J Laryngol Otology. 2000;114:248–253. doi: 10.1258/0022215001905454. [DOI] [PubMed] [Google Scholar]
- 19.Phelps PD, Wright A. Imaging cholesteatoma. Clin Radiol. 1990;41:156–162. doi: 10.1016/s0009-9260(05)80958-4. [DOI] [PubMed] [Google Scholar]
- 20.Jackler RK, Dillon WP, Schindler RA. Computerised tomography in suppurative ear disease: a correlation of surgical and radiographic findings. Laryngoscope. 1984;94:746–752. doi: 10.1288/00005537-198406000-00004. [DOI] [PubMed] [Google Scholar]
- 21.Harris JP, Darrow DH. Complications of chronic otitis media. In: Nado JB Jr, Shuknet HF, editors. Surgery of the ear and temporal bone. New York: Raven Press Ltd; 1993. pp. 171–190. [Google Scholar]
- 22.Chao YH, Yun SH, Shin JO, Yoon JY, Lee DM. Cochlear fistula in chronic otitis media with cholesteatoma. The Am J Otology. 1996;17:15–18. [PubMed] [Google Scholar]
- 23.Abramson M, Harke LA, McCabe BF. Labyrinthine fistula complicating chronic suppurative otitis media. Arch Otolaryngol. 1974;100:141–142. doi: 10.1001/archotol.1974.00780040147012. [DOI] [PubMed] [Google Scholar]
- 24.Buckingham RA, Valvassori GE. Tomographic evaluation of cholesteatoma of the middle ear and mastoid. Otolaryngol Clin North Am. 1973;6:363–377. [PubMed] [Google Scholar]
- 25.Buckingham RA, Valvassori GE. Tomographic and surgical pathology of cholesteatoma. Arch Otolaryngol. 1970;91:464–496. doi: 10.1001/archotol.1970.00770040658014. [DOI] [PubMed] [Google Scholar]
- 26.Mafee MF, Kumar A, Yannias D, et al. Computed tomography of the middle ear in the evaluation of cholesteatoma and other soft tissue masses: comparison with pleuri-direction tomography. Radiology. 1983;148:465–472. doi: 10.1148/radiology.148.2.6867344. [DOI] [PubMed] [Google Scholar]
- 27.Swartz JD, Goodman RS, Russel KB. High resolution computed tomography of the middle ear and mastoid. Part II: Tubotympanic disease. Radiology. 1983;148:455–459. doi: 10.1148/radiology.148.2.6867342. [DOI] [PubMed] [Google Scholar]


