Abstract
Summary
Scientific advances and technical developments in the field of laboratory diagnosis and their practical applications have raised ethical issues linked to religion, beliefs, lifestyle and traditions prevailing in different communities. Some of these are pertinent to genetic screening at various stages of life, prenatal diagnosis and the right of the genetically affected fetus to live—all aspects relevant to inbreeding marriages. Of relevance are medical and ethical principles based on professional responsibility. These ideological and social aspects encounter the challenges of science and its applications in the health field, which are linked, directly or indirectly, to scientific achievements and applications related to human genetics. Analysis of the human genome and identification of its sequence, and chemical components, and theories arising from connection of human genome components in health and disease conditions, have led to global requirements to outline legal aspects and ethical principles in relation to diagnosis, prevention and health care.
This paper presents basic aspects of disseminating genetic information, guiding the individual, the couple, or the concerned family through genetically induced ill health and methods of control and prevention. The paper discusses the elements and manner and presents details of the application of genetic counseling in Islamic communities in light of scientific, religious, social and legal aspects in the Islamic arena.
The knowledge gained from discoveries in human genetics since the advent of the recombinant DNA technology has the potential for making significant improvements in health when applied properly at the individual, family and community levels. If such discoveries and information are integrated into primary health care in an ethically acceptable manner and with respect for cultural and religious beliefs, the increased benefits for diagnosis, treatment and prevention of human genetic conditions will be appreciable. This is because genetics and biomedical technology have opened vast new avenues for research and can provide humankind with much needed therapeutic tools. But, when human life and dignity are at stake, technology cannot be left on its own to govern ethics, nor can health technology, practices and procedures be left to the vagaries of economic forces and personal interests.
The primary focus of genetic counseling coupled to genetic testing is to protect patients and families with genetic conditions and to lay down health policy and principles of dealing with ethical aspects of the field of human genetics. Needless to say, the practice has to observe the acceptable code of conduct and the prevailing traditions and community beliefs.
The purpose of the paper is to assist policy-makers and other officials, practitioners and other health providers, in ensuring that genetic information and genetic services are introduced into the broader medical practice in the community at large in an ethically acceptable manner. Of relevance is the need to allay fears and to reassure the public that adequate controls exist to prevent abuses of genetic information.
Genetic diseases in Islamic/Arab Countries—magnitude of the problem
Several genetic disorders occur at a high frequency in the Islamic/Arab countries and affect individuals and families irrespective of their socio-economic status.1–3 Some genetic diseases, including the haemoglobinopathies, thalassaemias, enzymopathies and some inborn errors of metabolism, occur at s high frequency in several of the Islamic/Arab countries and constitute a major health problem (Table 1). Other disorders, including several inborn errors of metabolism, neurological disorders, muscular disorders and congenital defects, are also of frequent occurrence.4–14
Table 1.
Classes and examples of major genetic diseases.
| Genetic diseases | Description |
|---|---|
| Single gene disorders | Includes sickle cell disease, thalassaemia, cystic fibrosis, hemophilia, neurofibromatosis, phenylketonuria, and others (this group follows a particularly clear manner of inheritance in the family pedigree and is rare) |
| Chromosomal disorders | Examples are Down syndrome, Klanefilter syndrome, Turner syndrome, trisomy of chromosome 13 (these affect the number and structure of the chromosomes) |
| Multifactorial disorders | Examples are congenital malformation, harelip, cleft palate, diabetes mellitus, hypertension, cardiovascular diseases, etc (this group is more common and affects a high percentage of the population, and many of these disorders are inborn defects while others have an onset in later life) |
| Somatic cell mutation | Includes malignancies, aging process changes. Mitochondrial disorders: Examples are hereditary blindness, labor optic atrophy |
Several factors are linked to the occurrence of genetic disorders 15–17 including consanguinity and recessive genetic disorders.18–19 Consanguinity is of frequent occurrence in most of the Islamic/Arab countries and first cousin marriages are most prevalent. Second cousin marriages and other forms of inbreeding also occur. In addition, it is a common practice that individuals belonging to a tribe or a specific area prefer to marry within the same tribe or area. It is well known the frequency of occurrence of rare disorders increases several magnitudes in populations, where inbreeding is frequent and as a consequence several rare congenital defects and inborn errors have been reported in the Islamic/Arab countries. Hence, genetic services must be made a component of “public health policy” in each country with everyone having an equal access to services for diagnosis, treatment and prevention of genetic diseases.
In addition, medical genetic services aim to detect early persons with genetic disorders and those at high risk for these disorders. Presymptomatic diagnosis, followed by appropriate intervention may control the disease. This is true specially in multifactorial disorders with an onset in later life.
Education and awareness programmes
For the successful implementation of any prevention programme, adequate awareness, in amount and depth, in the community, is essential. ‘Genetic services’ touch a wider group than ordinary health services, since genetic information affects an entire family and not just an individual. It may be predictive of future adverse events in an individual or family members health, and the choices made, based on the genetic information, may affect future generations. Thus, careful understanding of the defect, its genetic basis, its inheritance, its clinical consequences, mode of treatment, and ways and means of prevention is necessary. This requires education and awareness as well as adoption of preventive measures, including pre-marital screening and early diagnosis and intervention, including inborn screening. Unless the general population is educated and made aware of the prevalent conditions, steps towards control and prevention will be inefficient.
In Islamic/Arab communities, overall literacy is still lower than in developed countries. However, a sufficient amount of information may be conveyed to affected persons, their families and the overall population by well designed awareness programmes, involving preparation of booklets in Arabic, posters, lectures, videotapes, articles in newspapers, inclusion of biology curricula in secondary schools, and doctor-patient, doctor-family, doctor-doctor and family-family interactions.
Ethical principles in medical genetics
Ethical guidelines applied to medicine are universal and are the same for medical genetics. They concern autonomy, beneficence, justice, non-malfeasance, confidentiality and medical responsibility (Table 2). Respect for the autonomy of others is an essential ethical principle. This involves telling the truth and respecting confidentiality. It also involves protecting those persons who have diminished autonomy such as children and other persons with mental impairment or other disabilities. Physicians from all disciplines are taught to do good, be kind, avoid doing harm or if harm cannot be avoided, to minimize harm to concerned individuals and families. These principles are more strictly followed in genetics. In addition, goals of justice demand that all persons are treated fairly and equally and obtain what they deserve or are entitled to. Thus medical genetics, like any health care field, ought to be governed by ethically justified rules.
Table 2.
Ethical principles of relevance to genetic counselling.
|
In the Islamic/Arab countries these principles have to be firmly engraved in the teaching of health professionals. Islam strongly emphasizes each of these principles with special emphasis on equality of all mankind, goodness and kindness to all and avoidance of harmful, evil and selfish motives that may relate to genetic disorders in the community.27–32
Goals of community services in fields of human genetics
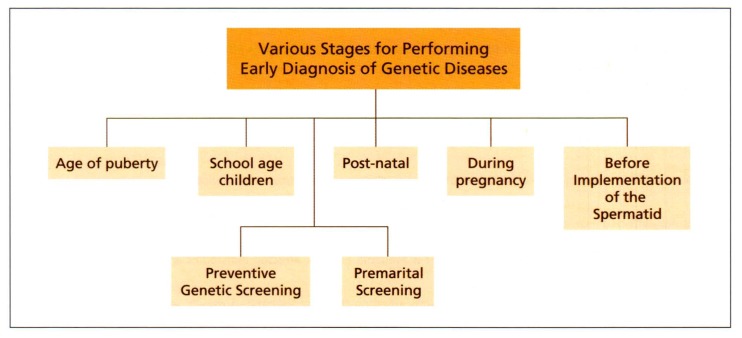
Medical genetics is the field of medicine that is most centrally involved in providing services to persons with genetic diseases, their families, carriers and high-risk groups. Medical genetic services are aimed at identifying the person with the genetic defect or a higher susceptibility to develop defects. Once an accurate diagnosis has been made, the next steps are to provide proper care, therapeutic measures, rehabilitation for those requiring it, and adequate steps towards control and preventive measures, including genetic counseling. Genetic services also involve pre-symptomatic diagnosis in high-risk groups, and early diagnosis and treatment, including gene therapy (Figure 1). The major goals of community services related to medical genetics are:
Figure 1.
Various stages in the early diagnosis of genetic diseases.
to help people with a genetic disadvantage and their families to live and reproduce as normally as possible and to make informed choices in reproductive and health matters,
to assist people to obtain access to relevant medical services (diagnostic, therapeutic, rehabilitative or preventive) or social support systems.
to help the genetically disadvantaged to adapt to their unique situation.
to help the genetically disadvantaged become relevant persons, informed on relevant new developments and beneficial potentials.
Medical genetic services require specially trained personnel, including physicians, science graduates with a Ph.D. in genetics, nurses, specially trained health care workers, genetic counselors, social workers and laboratory personnel. In the Islamic/Arab countries, steps have to be taken to provide training to appropriate categories of personnel to provide adequate genetic services, at all levels of the health care delivery system, to achieve the set goals.
Genetic counseling—the framework
The following two definitions of genetic counselling are worth consideration. Peter S. Harper20 puts forward a definition used commonly in several books of genetics: Genetic counselling is the process by which patients or relatives at risk of a disorder that may be hereditary, are advised of the consequences of the disorder, the probability of developing or transmitting it and the ways in which this may be prevented, avoided or ameliorated. A second definition given by Kelly in a very valuable book entitled “Clinical Genetics and Genetic Counseling”21 defines genetic counseling as: An educational process that seeks to assist affected or at risk individuals to understand the nature of the genetic disease, its transmission and the options open to them in management and family planning.
Genetic counseling is a component of several medical disciplines, but genetic counseling plays an essential role in control and prevention of genetic disorders and is considered inseparable from genetic diagnosis. Its role in medical genetics is of particular significance as it utilizes the predictive nature of genetic decisions to estimate the risk of recurrence in other members of the family, as well as to help increase the knowledge of the family about the causes, the diagnostic aspects, the available treatment strategies and ways and means of achieving the ultimate goal of prevention. An important aspect of genetic counseling is the provision of the estimated recurrence risk to the families with a genetic disease, patients or other members of the family, or carrier individuals planning to get married or conceive, or individuals who have been exposed to harmful environmental factors.
Genetic counseling deals with three major elements to achieve control and prevention:
diagnostic aspects, where an accurate diagnosis is required for a secure foundation of the advice,
the calculation of recurrence risk, and
a communicative role, providing beneficial information about the disease and available supportive, preventive and ameliorative measures, to ensure that those who are advised will benefit.
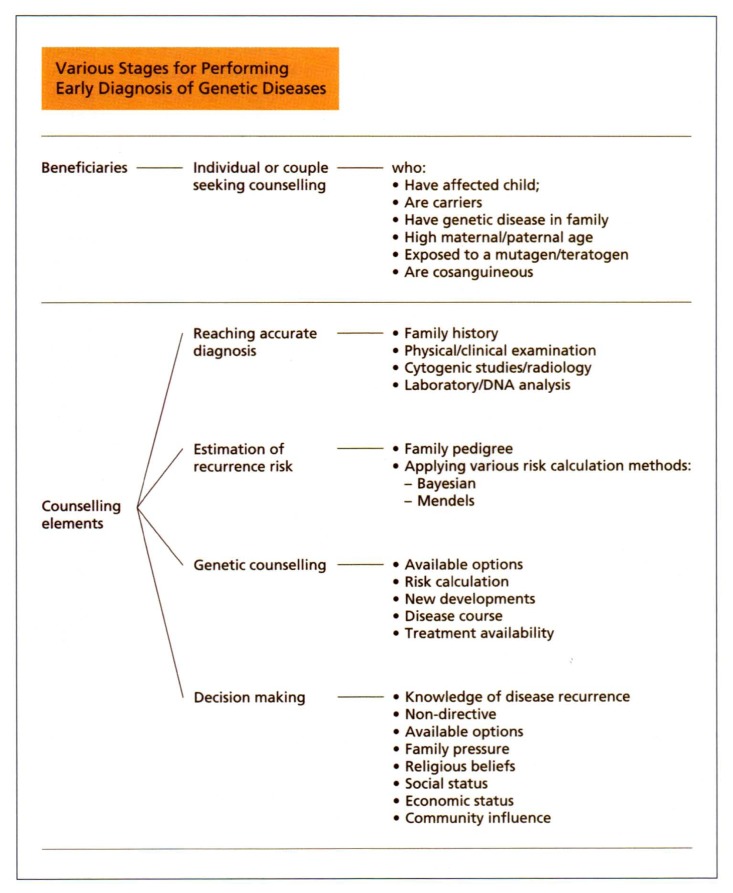
The main stages of genetic counseling process
An informal form of genetic counseling has been carried out for thousand of years. The scientific practices that started at the beginning of the century were developed after Mendel’s Laws of Inheritance. However, in 1979, genetic counseling was first recorded in Index Medicus and has since been given significant importance. In the span of the last two to three decades, there has been remarkable interest in the field of genetic counseling as a preventive measure for genetic disorders. The major components of genetic counseling include reaching an accurate diagnosis, calculation of risk of recurrence, information counseling, decision making processes, and long term follow-up (Figure 2). The counsellor must provide accurate information without any bias, listen to the concerns of the individuals, help them to express and understand their own values and help them to work towards their own decisions, particularly when it comes to reproductive choices. Since counseling should be non-directive, the counselor does not tell the counselee what to do; the decision is that of the individuals and families.
Figure 2.
Beneficiaries and elements of genetic counseling.
Broadly, the two major elements of non-directive counseling include the provision of accurate, complete and unbiased information to the families, and the provision of support, understanding and an empathic relationship that offers guidance to the individuals or families to make their own decision (Figure 2).
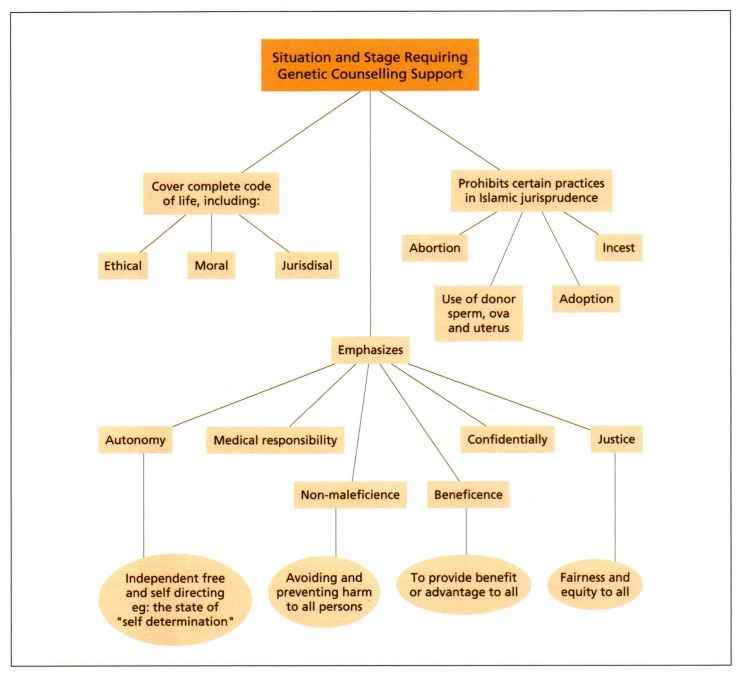
Genetic testing and counseling in the Islamic Concepts
In Islamic/Arab communities, the counselor should have full awareness of the beliefs, traditions and values of the community and take special care in avoiding any confrontation. Some components of genetic counseling are sensitive points and the transfer from one social context to another needs careful consideration. In the Islamic/Arab communities, due to their strong religious beliefs, social reservations and the high significance of customs and traditions, the genetic counseling process should be geared to providing maximum benefit within the appropriate framework (Figure 3).22,24 Considering the major steps listed in Figure 2, it is obvious that (i) for reaching an accurate diagnosis, the same universally acceptable procedures listed earlier are applicable and Islamic/Arabic communities and considerations are by no means disturbed or offended by these; (ii) calculation of the risk or probability of recurrence is also made using the same universal procedures and is not altered by variations in religious or social context, (iii) providing detailed and accurate information to the counselee is also a universally acceptable process and should clarify all aspects of the genetic condition in question, (iv) when coming to the decision making process, several points have to be dealt with carefully. Though the decision is that of the counselee or the family, certain important points must be borne in mind by the genetic counselor to avoid any conflicts after the decision has been made.
Figure 3.
Islamic teachings in the field of genetics.
In the Islamic and Arabic communities, testing at various stages and beneficial interventions are viewed together (Table 3). Various stages of testing are to be governed by the possible benefit that can be gained and the subsequent dealing within the framework of the Islamic Shareah. Premarital and newborn testing are generally viewed as acceptable procedures. On the other hand, prenatal testing is faced with some limitations, where the available reproductive choices and options require several ethical principles that must be considered. The relevant aspects include:
Table 3.
Available options for individuals at different stages of testing.
Population screening including newborn screening and screening of school children
Premarital screening
|
Prenatal diagnosis as a procedure, is allowed in Islam, as long as it does not unnecessarily increase risk for the mother and the fetus, and leads to abortion that is not in line with Islamic Shareah.
-
Abortion is generally unacceptable in Islam 40 days after conception. However, the Islamic Jurisprudence Council of Makkah Al-Mukaramah (The Islamic World League) passed a Fatwa No. 4 (Legal Resolution) in its 12th Session held from 15–22 Rajab 1410H (10–17 February 1990),25 which state that “If the fetus reached 120 days counted from conception date, abortion is not allowed even if the medical diagnosis proved that the fetus is malformed, except only if it is proved by report from a committee formed of competent trustworthy physicians that continuance of the pregnancy has a confirmed risk to the mother’s life. If this is the case it is allowed to abort, whether the fetus is malformed or no to drive away larger harm (hurt, damage, or detriment).
“Before 120 days of pregnancy counted from date of conception, if this is proved and confirmed by a report from a Committee formed of competent trustworthy physicians and on the basis of laboratory means that the fetus is grossly malformed with untreatable severe condition and if he stays and born on his time, his life will be vicious and painful for him and for his family, then it is allowed to abort it on the basis of the parents requisition.”
Thus, by extending the time of permissible abortion to 120 days (134 days from LMP), there is an ample opportunity to ascertain the diagnosis of severely affected embryos and fetuses, particularly with the application of the recombinant DNA techniques.
Regarding assisted reproduction, Islamic teaching does not prohibit in vitro fertilization (IVF), provided that the ova, sperm and uterus are from husband and wife during the existence of the matrimonial bond. If divorce or death of a spouse occurs then no procreation is allowed. Hence all forms of artificial insemination by a donor or egg donation are completely outlawed in Islam.
Adoption of children in a way that the lineage of child is not kept with his/her biological parents is not allowed in Islam, though Islam strongly encourages caring for orphans or children of unknown parents, and this is regarded as a charity and a great act of worship.
The cloning of humans is not allowed in Islam, as this process does not follow the “Fitrah of Allah” i.e. sexual reproduction.
Genetic counseling may be sought for different situations as presented schematically in Figure 4 and Table 3. In almost every situation psychological counseling is required, specially when a child is born with a genetic or birth defect, or prenatal diagnosis results show an abnormality. Learning of the situation may generate severe emotional upheaval and the genetic counselors have an important role to play in providing psychosocial support.
Ethical Issues relevant to specific conditions
Of special interest is the therapy of genetic diseases, pre-symptomatic susceptibility and carrier testing, and confidentiality and disclosure.
Therapy of genetic diseases
Several genetic diseases can be treated and cured or the consequences may be prevented or delayed by appropriate care strategies applied at the appropriate stage. Thus congenital defects, such as congenital heart disease, have been treated by surgical intervention in utero; congenital dislocation of the hip can be corrected by proper care during the neonatal stage; mental retardation associated with phenylketonuria can be prevented by reducing the amount of phenylalanine in diet; consequences of congenital hypothyroidism can be avoided by treatment with thyroid hormone; and infections in sickle cell disease may be avoided by pneumococcal vaccination and penicillin prophylaxis. No serious ethical issues are raised against these therapeutic strategies since they all encourage beneficence and non-malfeasance. Early diagnosis and early intervention are essential to avoid the consequences of these genetic conditions. However, gene therapy and the feasibility of stem cell generated organ replacements need to be judged in time, when these methods become practically available.
Pre-symptomatic, susceptibility and carrier testing
Presymptomatic and susceptibility testing for late onset diseases is being introduced more and more in genetic testing. Some individuals appear clinically healthy but carry the genes or genetic susceptibility to develop the disease later in life. In some cases (i.e., multifactorial disorders i.e. CHD, hypertension, colorectal cancer) environmental factors play a role in predisposing to disease development. Such cases, if diagnosed early and followed by appropriate intervention may not develop the disease or may have a delayed onset or minimal complications, by avoiding the environmental factor. Similarly, if the individuals have an abnormal gene for a late-onset-disease such as Huntington’s disease, the individual may be prepared to deal with its clinical consequences. Pre-symptomatic and susceptibility testing is encouraged, particularly if therapeutic measures are available. If intervention is currently not available, it is suggested that presymptomatic susceptibility testing should be available, provided that the testing is voluntary; that informed consent is obtained and the person is mentally capable of giving consent; the person is fully informed of the limitations of the test or uninformative results, or of the inability to predict exact age of onset or severity of symptoms; the person is ready to accept the status of carrier or later the affected status; the information provided by the test will prevent harm to the person tested, spouse, family, prospective children or others; and genetic counselling, both pre-test, and post-test is available for an appropriate length and intensity.
An important issue regarding testing children for adult-onset diseases is that if a medical benefit through prevention or treatment is available then testing of children should be encouraged. However, if it is not currently available, then the testing of children for adult-onset diseases should be postponed until adulthood in order for him/her to make his/her own decision. Counseling sessions must explain benefits and risks in the testing of children.26–27
Confidentiality and disclosure
Confidentiality of all genetic information related to an individual, in order to protect him from harm caused by disclosure to institutional third parties, is of utmost importance. Lack of confidentiality or disclosure is considered as one of the most frequent ethical problems in medical genetics.
If a genetic condition exists which increases risk to his/her relatives, then it is not only important to encourage the person to disclose the condition to those involved, but also to have genetic counseling for his/her self and for family members, particularly if there is affordable treatment or preventive measures are available. In all other situations, all concerned must follow a strict confidentiality code with the patient, including the physician, nurses, laboratory workers, other health care personnel and genetic counselors.
Conclusion
The rapid progress and accumulation of data on the human genome and enrichment in our understanding of inheritance in health and disease conditions has reached a stage where necessary social adjustments have to be made to minimize the number of affected individuals, and to benefit those who are susceptible and carriers. The resultant improvement in human well being can be brought about only if basic human values are taken into consideration and the conceived programmes are sensitive to issues of human dignity.
The incidence of genetic diseases in the Islamic world is high because of social and other factors that promote consanguinity. In view of this, we suggest that genetic services should be made a component of public health policy by offering diagnosis, care and prevention possibilities. The prevention programme should include dissemination of information through various media and direct genetic counseling. While at the diagnostic and risk evaluation levels, the universally acceptable procedures encounter no conflicting views, genetic counseling has to be receptive to the teachings of Islam, long held beliefs and prevailing tradition. In this regard, Islam stresses a regard for individual autonomy, confidentiality, intent of beneficence and preservation of familial integrity. Islam also has its injunctions on abortion, adoption and cloning, which need to be taken into consideration while implementing policies and procedures in genetic services and practices.
References
- 1.El-Hazmi MAS, Warsy AS. Genetic Disorders among Arab Populations. Saudi Med J. 1996;17(2):108–123. [Google Scholar]
- 2.Warsy AS. Genetic and Congenital Disorders—Magnitude and Spectrum of the Problem; WHO/KSU Workshop on Ethical and Genetic Counselling Issues in the Region (Guidelines); Riyadh. 15–16 November, 1999. [Google Scholar]
- 3.Hamida BM. Magnitude and spectrum of the problem. WHO/KSU Workshop on Ethical and Genetic Counselling Issues in the Region (Guidelines); Riyadh. 15–16 November, 1999. [Google Scholar]
- 4.Mathew PM, Hamdan JA, Nazar H. Cystic fibrosis presenting with recurrent vomiting and metabolic alkalosis. Eur J Pediatr. 1991;150:264–266. doi: 10.1007/BF01955527. [DOI] [PubMed] [Google Scholar]
- 5.Nazer H. Early diagnosis of cystic fibrosis in Jordanian children. J Trop. 1992;38:113–115. doi: 10.1093/tropej/38.3.113. [DOI] [PubMed] [Google Scholar]
- 6.Kagalwalla YA, Beg MR. Alkaptonuria: A case report. Saudi Med J. 1991;12:438–439. [Google Scholar]
- 7.Hardy MJ, O Connel JP. Maple syrup urine disease in two siblings in Saudi Arabia. Saudi Med J. 1987;8:250–252. [Google Scholar]
- 8.Al-Jurayyan NAM, Al-Nuaim A, El-Desouki M. Congenital hypothyroidism: Clinical laboratory characteristics in infants detected by neonatal screening. Ann Saudi Med. 1992;12:135–139. doi: 10.5144/0256-4947.1992.135. [DOI] [PubMed] [Google Scholar]
- 9.Teebi A. Mendelizing inborn errors of morphogenesis among the Arabs. An overview from Kuwait. Med Assoc. 1990;24:122–124. [Google Scholar]
- 10.Rubello Pento M, Buhl L. Prevalence of spinal muscular atrophy in Oman: a six month study. Emirates Med J. 1992;10:131–136. [Google Scholar]
- 11.Al-Arrayed SS, Mohammed AM. Fragile X-syndrome in a Bahraini family. Bahrain Med Bull. 1990:84–90. [Google Scholar]
- 12.Al-Tahan AR. The pattern of peripheral neuropathy in Saudi Arabia: The experience at King Khalid University Hospital 1983–1990. Saudi Med J. 1994;15:127–132. [Google Scholar]
- 13.Ahmed MA. Marfan’s syndrome. Saudi Med J. 1984;5:319–322. [Google Scholar]
- 14.Warsy AS, El-Hazmi MAF, Hammoda H. Alpha-1-antitrypsin: Frequencies of PiM subtypes in a Saudi population. Saudi Med J. 1991;12:376–379. [Google Scholar]
- 15.Emery AEH, Mueller RF. Elements of Medical Genetics. 8th Ed. London: Churchill Livingston; 1991. [Google Scholar]
- 16.Thompson MW, McInnes RR, Willard HF. Genetics in Medicine. 5th Ed. Philadelphia: W.B. Saunders and Co; 1991. [Google Scholar]
- 17.WHO. Prevention of avoidable mutational disease. Bull World Health Organ. 1986;64:205–216. [PMC free article] [PubMed] [Google Scholar]
- 18.Nader S. Congenital abnormalities in newborn of consanguineous and non-consanguineous parents. Obstet and Gynecol. 1979;53:195–199. [PubMed] [Google Scholar]
- 19.Al-Awadi SA, Moussa MA, Naguib KK. Consanguinity among the Kuwaiti population. Clin Genet. 1985;26:243–246. doi: 10.1111/j.1399-0004.1985.tb00236.x. [DOI] [PubMed] [Google Scholar]
- 20.Harper PS. Practical Genetic Counselling. 5th Ed. Oxford: Butterworth and Heinemann; 1998. [Google Scholar]
- 21.Kelly TE. Clinical Genetics and Genetic Counselling. Chicago: Year Book; 1986. [Google Scholar]
- 22.El Hazmi MAF. Ethics of genetic counselling in the Arab/Islamic communities. Riyadh: Al-Obeikan Press; 2003. [Google Scholar]
- 23.Albar MA. Counselling about genetic diseases: an Islamic perspective. East Mediterranean Health J. 1999;5(6):1129–1133. [PubMed] [Google Scholar]
- 24.Albar MA. Ethical considerations in the prevention and management of genetic disorders with special emphasis on religions considerations. Saudi Med J. 2002;23(6):627–632. [PubMed] [Google Scholar]
- 25.Albar MA. AlJanin Al-Mushawan wa Al-Almradh Alwirathiyia. Paper presented at: Fatwa 4. 12th Session of Islamic Jurisprudence Council of Islamic World League, Makkah Al-Mukaramah; February 10–17, 1990; Jeddah, Saudi Arabia. [Google Scholar]
- 26.International Ethical Guidelines for Biomedical Research involving Human Subjects. Geneva: CIOMS/WHO; 1993. [PubMed] [Google Scholar]
- 27.Watson MS. Report of the Joint DOE-NIH EISI Task Force on Genetic Testing. Baltimore: Johns Hopkins University Press; 1998. Promoting safe and effective genetic testing in the United States. [Google Scholar]
- 28.Joshi S, Al-Essa MA, Archibald A, Ozand PT. Biotinidase deficiency: a treatable genetic disorder in Saudi population. East Mediterr Health J. 1999;5(6):1213–1217. [PubMed] [Google Scholar]
- 29.Subramanyam SB. Saudi aminoacidemias: a six year study. Indian J Pediatr. 1996;63(5):641–644. doi: 10.1007/BF02730809. [DOI] [PubMed] [Google Scholar]
- 30.Al-Nuaim L, Talib ZA, El-Hazmi MA, Warsy AS. Sickle cell and G-6-PD deficiency gene in cord blood samples: experience at King Khalid University Hospital, Riyadh. J Trop Pediatr. 1997;43(2):71–74. doi: 10.1093/tropej/43.2.71. [DOI] [PubMed] [Google Scholar]
- 31.Simonaro CM, Desnick RJ, McGovern MM, Wasserstein MP, Schuchman EH. The demographics and distribution of type B Niemann-Pick disease: novel mutations lead to new genotype/phenotype correlations. Am J Hum Genet. 2002;71(6):1413–1419. doi: 10.1086/345074. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Al-Essa MA, Sakati NA, Bakheet SM, et al. X-linked adrenoleukodystrophy. The Saudi experience. Saudi Med J. 2000 Jan;21(1):61–71. [PubMed] [Google Scholar]