The balance between the pulmonary and the systematic blood flows is a critical factor in the overall patho-physiology of congenital cardiac lesions. Simple and isolated cardiac lesions may cause severe symptoms in any particular patient when associated with unbalanced systemic/pulmonary circulations e.g. isolated atrial septal defect may lead to significant symptomatology of congestive heart failure when there is a large shunt and markedly increased pulmonary blood flow. Valvular pulmonic stenosis may lead to severe cyanosis if the valve is critically stenosed with markedly decreased pulmonary blood flow. Complex lesions, on the other hand, may lead to trivial or no symptoms if associated with balanced pulmonary and systemic blood flows. This fact is well illustrated in this rare case where the occurrence of two complex cyanotic anomalies in the same patient failed to cause any significant symptoms.
In this particular patient each lesion canceled the detrimental hemodynamic effect of the other lesion resulting in balanced pulmonary/systemic circulations and no significant symptoms.
Case Report
A 4-year old male was referred for cardiac evaluation because of occasional “blue coloration” of his lips noticed by his mother when he plays. The parents were cousins and had three children; all of them had significant cyanotic nongenital heart disease (two children had transposition of the great arteries and one had tetralogy of Fallot).
His physical examination was significant for mild cyanosis (masked by his relatively dark skin) with oxygen saturation on room air of 85% by pulse oximetry. There was a single loud second heart sound. The rest of his examination was completely normal, including normal growth and development for his age. Pulmonary atresia, ventricular septal defect, and aorto-pulmonary collaterals were suspected despite the absence of any significant heart murmurs.
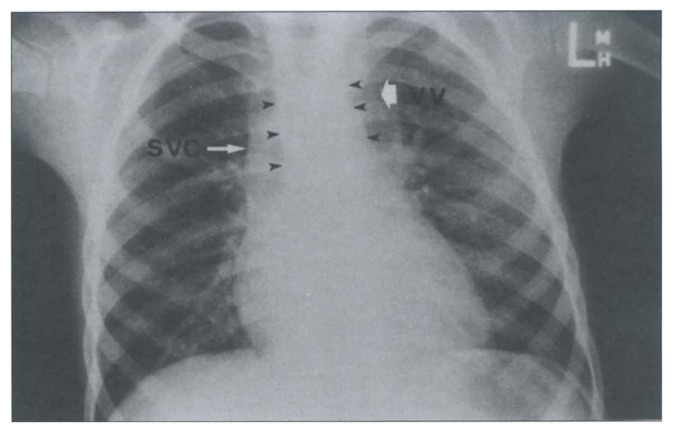
Chest x-ray revealed a normal cardiac silhouette and pulmonary vascular markings. The appearance of the superior mediastinum was unusual in that, while the projection of the great vessels was narrower than normal, the overall width of the superior mediastinum was within normal limits due to the presence of increased opacity on both sides of the great vessels (Figure 1).
Figure 1.
Plain chest x-ray from a 4-year-old child with transposition of the great arteries (D-TGA) and supra-cardiac total anomalous pulmonary venous connection (TAPVC). The supra-cardiac vertical vein (VV) and the enlarged right superior vena cava (SVC) are well delineated. This supra-cardiac shadow masked the narrow mediastinum commonly seen with TGA (black arrow head). Both the cardiac silhouette and the pulmonary vascular markings were normal, which is an unexpected finding in TAPVC (i.e. each anomaly corrects the hemodynamic abnormality caused by the other lesion.
An echocardiogram was performed which revealed complete transposition of the great arteries (D-TGA), a 10-mm atrial septal defect with right-to-left shunt and a total anomalous pulmonary venous connection (TAPVC) via a left ventrical vein to the left innominate vein. Cardiac catheterization and angiography confirmed the echocardiographic diagnosis (Figures 2,3). The Qp:Qs was 1:1.04. The patient was referred for surgical repair, which consisted of pulmonary artery banding followed in 2 weeks by arterial switch and repair of the anomalous pulmonary venous connection.
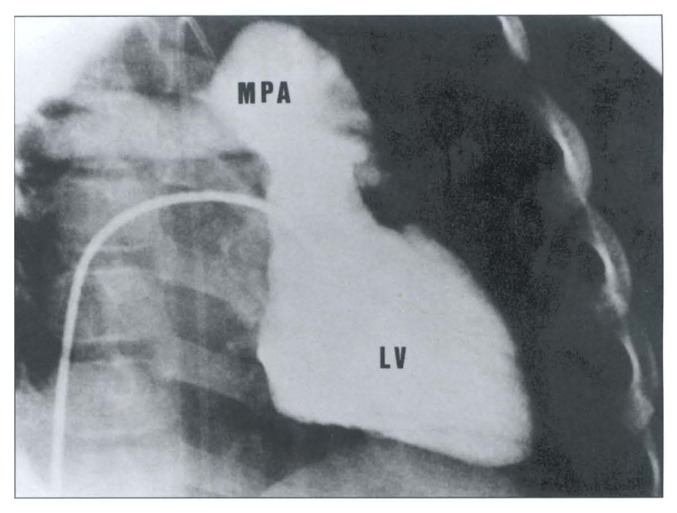
Figure 2.
Left ventriculogram (LV) showing the origin of the main pulmonary artery (MPA) from the LV with intact ventricular septum (not profiled in this view).
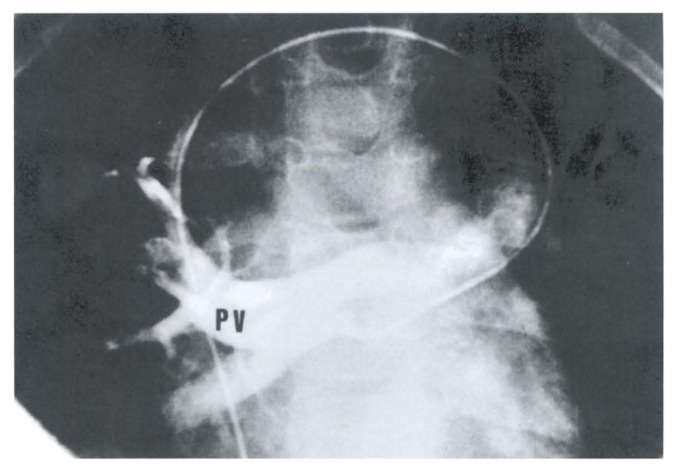
Figure 3.
Selective injection into the right pulmonary veins (PV) which connected anomalously to a vertical vein, to the innominate vein, then to the right superior vena cava. A similar injection was obtained from the left pulmonary veins. Catheter course: Inferior vena cava - to the right atrium - to superior vena cava - to left innominate vein - to vertical vein - to common pulmonary vein behind the left atrium - to the right pulmonary veins.
Discussion
The combination of complete transposition of the great arteries (D-TGA) and total anomalous pulmonary venous connection (TAPVC) is very rare.1–4
Unlike the few previous reports of this combination, which mainly addressed the surgical technique, this report illustrates the pathophysiology of the two major lesions together. The basic hemodynamic abnormality in complete transposition of the great arteries is the presence of two parallel circulations which, in the absence of adequate mixing of the pulmonary and systemic venous returns, results in severe cyanosis immediately after birth and is incompatible with long term survival. In total anomalous pulmonary venous connection, on the other hand, there is torrential pulmonary blood flow resulting in severe congestive heart failure and cyanosis in the newborn infant.
In the presence of a small atrial septal defect (in this patient it was 10 mm by echocardiography), each anomaly “corrects” the basic hemodynamic abnormality of the other anomaly—TAPVC will provide total mixing of both pulmonary and systemic venous returns in the right atrium and in D-TGA the main pulmonary artery arises from the left ventricle and is not subjected to the torrential blood flow which, in this case, was well controlled by the small atrial septal defect. This patient, therefore, had balanced pulmonary/systemic blood flow (evidenced by Qp:Qs of 1 during the cardiac atheterization) and was completely asymptomatic apart from his cyanosis.
Cyanosis, in his case, was due to complete admixture of the systemic and pulmonary blood flows in the right atrium before being distributed equally between 213 the systemic and the pulmonary circulations.
References
- 1.Whitaker W, Watson DA, Keates PG. Total anomalous pulmonary venous drainage into the left innominate vein associated with transposition of the great vessels. Circulation. 1964;30:918–922. doi: 10.1161/01.cir.30.6.918. [DOI] [PubMed] [Google Scholar]
- 2.Amodeo A, Corno A, Marino B, Carta MC, Marcelletti Combined repair of transposed great arteries and total anomalous pulmonary venous connection. Ann Thorac Surg. 1990;50:820–821. doi: 10.1016/0003-4975(90)90697-5. [DOI] [PubMed] [Google Scholar]
- 3.Gontijo B, Fantini F, Baybosa M, Gomes MV, Gutierrez C, Vrandecic M. Surgical repair of transposition of great arteries and total anomalous pulmonary venous return to the coronary sinus. European J of Cardio-Thorac Surg. 1994;8:391–392. doi: 10.1016/1010-7940(94)90035-3. [DOI] [PubMed] [Google Scholar]
- 4.Ueda Y, Miki S, Okita Y, Tahata T, Sakai T, Matsuyama K, Matsumura M, Tamura T. Transposition of the great arteries associated with total anomalous pulmonary venous return. Ann Thorac Surg. 1994;57:470–472. doi: 10.1016/0003-4975(94)91021-9. [DOI] [PubMed] [Google Scholar]