To the Editor: Juvenile hypothyroidism is a rare cause of precocious puberty. This unusual presentation occurs in patients with untreated hypothyroidism of long duration. In this article we describe two cases of juvenile hypothyroidism with signs of precocious puberty in two prepubertal girls who developed breast enlargement, vaginal bleeding, and severe growth retardation. Our purpose is to emphasize the importance of hypothyroidism, which is benign and easily treatable, in the differential diagnosis of precocious puberty.
Case 1
An 8-year old girl presented with abdominal pain, anorexia and vaginal bleeding. She had the same symptoms one month previously Physical examination at the time of admission disclosed a body weight of 21 kg (10th to 25th percentile), a height of 106 cm (<5th percentile), and normal vital signs. She had large breasts compatible with Tanner Stage 4, without pubic hair. Her thyroid gland was palpable and clearly visible. On ultrasonographic examination, two cystic lesions in both ovaries were detected. With an initial diagnosis of ovarian tumor the patient was operated on and the lesions were removed (on pathological examination, the lesions were shown to be follicular cysts). Ten days after admission hormonal examination showed a total T4 of 16.77 nmol/L (normal: 58–161 nmol/L), a plasma free T4 of 2.8 pmol/L (normal: 10.3 to 35 pmol/L), T3RU of 24% (normal: 24% to 37%), TSH>100 mu/L(normal:0.3–5), FSH of 3.9 IU/L, LH of 1.8 IU/L, and estradiol of 1178 pmol/L (normal: 18–661pmol/L), which was high in relation to the patient's chronological age . Bone age was estimated at 4 years and 8 months using the Greulich and Pyle method.1 Treatment with thyroid hormone was started. Three months later the breasts had decreased in size, and there was no vaginal bleeding.
Case 2
A 9-year-old girl was referred to the pediatric endocrinology and metabolism ward for evaluation of growth deceleration and periodic vaginal bleeding, which started 6 months previously Physical examination at the time of admission disclosed a body weight of 24 kg (10th to 25th percentile), a height of 108 cm (<5th percentile), and a upper-to-lower segment ratio of 1.2/1. Pubertal development was rated B3P1A1 (Figure 1) with reference to Tanner stage with signs of estrogenisation of the external genitalia.2 There was stage 2 goiter and no history of pain in the neck in the area corresponding to the thyroid. Bone age was estimated at 5 years using the Greuliche and Pyle method 1 and pelvic ultrasonography revealed bilaterally enlarged multicystic ovaries, with a uterus of pubertal dimensions. Hormonal investigation showed a total T4 of 15.48nmol/L (normal: 58–161nmol/L), a plasma free T4 of 3 pmol/L (normal: 10.3 to 35pmol/L), T3RU of 23% (24–37), TSH>100 mμ/L (normal: 0.3 to 5 mμ/L) FSH of 6 IU/L, LH of 1.2 IU/L, and estradiol of 954 pmol/L (normal 18–661). Antithyroperoxidase antibodies were strongly positive. After ten weeks of treatment with sodium levothyroxine she had a 4-cm height velocity, decreased breast size and the ovarian cysts were resolved.
Figure 1.
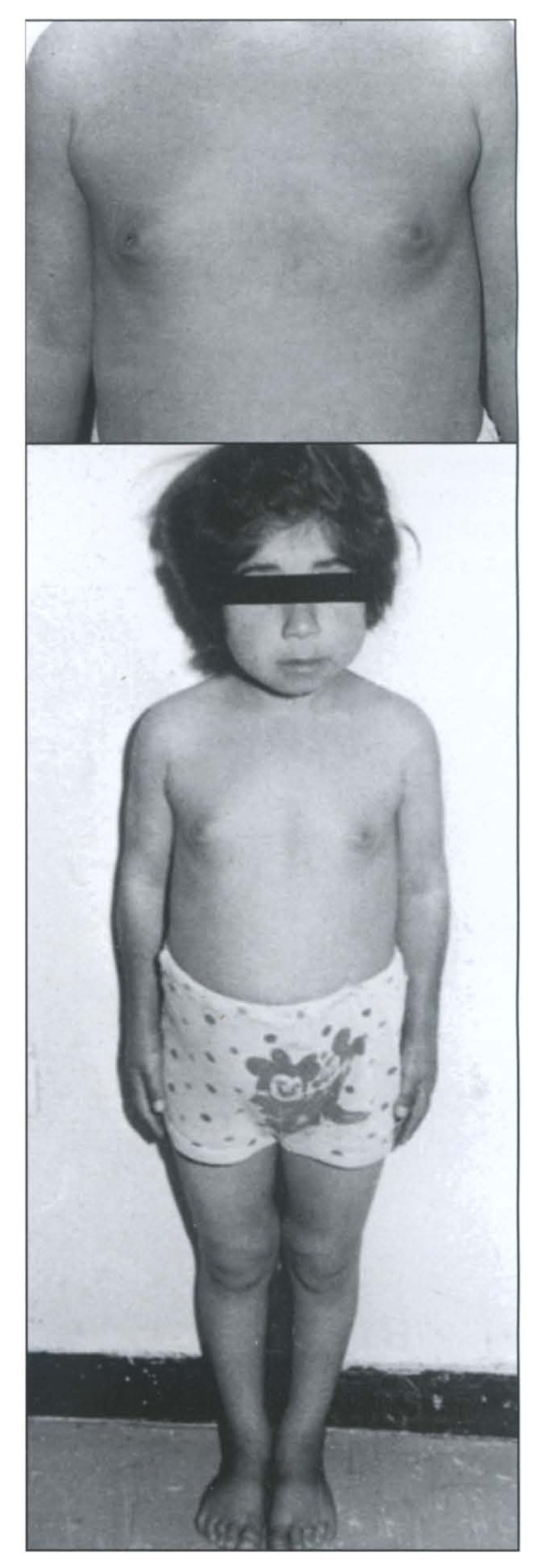
Breast enlargement (top) and disproportional short stature in hypothyroidism.
Discussion
Hypothyroidism during childhood and adolescence is usually mild. Delayed puberty, severe skeletal and growth retardation and delayed eruption of permanent teeth are characteristic findings in patients with severe hypothyroidism.3 Thyroid hormone is essential for growth, sexual development and reproductive function.4 Thyroid hormone plays a permissive role in puberty; its absence may delay the onset or retard the progress of pubertal maturation by interfering with gonadotropin secretion.3,5
Classically, in untreated hypothyroidism, the onset of puberty is usually delayed until epiphyseal maturation has reached 12 to 13 years of age, but a significant minority of patients develop precocious puberty.6 Since the onset of puberty is more closely correlated with osseous maturation than with chronologic age, precocious puberty in a child with untreated hypothyroidism and a prepubertal bone age presents a strikingly nonphysiologic association.7 The signs of sexual maturation are not accompanied by a pubertal growth spurt; rather growth is impaired. Decreased growth velocity and bone age delay, unusual in precocious puberty, is associated with an exaggerated weight increase, which suggest the diagnosis of hypothyroidism.8 Some authors believe that precocious puberty with bone age delay is pathognomonic.1 Girls show breast development, an enlargement of the labia minor, usually without the appearance of pubic hair, and a solitary cyst or multiple cysts may be demonstrable with pelvic ultrasonography or by physical examination.9
Gordon et al described a case of acquired primary hypothyroidism in a prepubertal girl who presented with profound bradycardia, precocious puberty, severe vaginal bleeding, and markedly enlarged ovarian cysts.10 Chemaitilly et al reported a child with Downs syndrome in whom metrorrhagia and precocious puberty revealed primary autoimmune hypothyroidism.8 In most boys with juvenile hypothyroidism, the testes are enlarged because of an increase in size of the seminiferous tubules, but signs of virilization and Leydig cell maturation are absent.11
Van Wyk et al proposed that precocious puberty in hypothyroidism results from the overproduction of gonadotropins due to the loss of negative feedback on the pituitary12 The gonadotropin in the serum of these patients, however, is relatively low for their degree of gonadal stimulation. Anasti et al concluded that cross-reactivity of TSH with the FSH receptor is a potential pathogenic mechanism of precocious puberty in severe juvenile hypothyroidism.13 Niedziela and coworkers concluded that pubertal signs due to central stimulation of gonadotropins are possible in severe hypothyroidism, and that full regression of pubertal signs can be obtained when euthyroid TSH levels are reached.14 Gordon et al concluded that percutaneous cyst aspiration is useful to treat ovarian hyperstimulation caused by hypothyroidism.10 In this report one of the patients had an unnecessary operation before diagnosis was confirmed by hormonal studies. Whatever the mechanism, treatment of hypothyroidism with sodium levothyroxine results in rapid return of the hormonal and clinical manifestations to normal status.
References
- 1.Greulich WW, Pyle SI. Radiographic atlas of skeletal development of the hand and wrist. 2nd ed. Stanford: Stanford University Press; 1959. [Google Scholar]
- 2.Tanner JM. Growth at adolescence. Oxford: Blackwell; 1978. pp. 28–39. [Google Scholar]
- 3.Foley TP. Acquired hypothyroidism during infancy, childhood, and adolescence. In: Braverman LE, Utiger RD, editors. Werner & Ingbar's The Thyroid. 7th ed. Philadelphia: Lippincott-raven; 1996. pp. 994–997. [Google Scholar]
- 4.Weber G, Vigone MC, Stroppa L, Chiumello G. Thyroid function and puberty. J Pediatr Endocrinol Metab. 2003 Mar;16(Suppl 2):253–257. [PubMed] [Google Scholar]
- 5.Rosen D, Kelch R. Precocious and delayed puberty. In: Becker KL, editor. Principles and practice of endocrinology and metabolism. 2nd ed. Philadelphia: J.B. Lippincott company; 1995. pp. 830–836. [Google Scholar]
- 6.Kelnar CJ. Endocrine gland disorders and disorders of growth and puberty. In: Campbell AGM, McIntosh N, editors. FORFAR and ARNEIL’S Textbook of Pediatrics. 5th ed. London: Churchill livingstone; 1998. pp. 1048–1050. [Google Scholar]
- 7.DiGeorge AM. The Endocrine System. In: Behrman RE, Kliegman RM, Arvin AM, editors. Nelson Textbook of Pediatrics. 15th ed. Philadelphia: W.B. Saunders; 1996. pp. 1567–41594. [Google Scholar]
- 8.Chemaitilly W, Thlassinos C, Emond S, Thibaud E. Metrorrhagia and precocious puberty revealing primary hypothyroidism in a child with down’s syndrome. Arch Dis Child. 2003;88:330–331. doi: 10.1136/adc.88.4.330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Grumbach MM, Styne DM. Puberty. In: Wilson JD, Foster DW, editors. Williams Textbook of endocrinology. 9th ed. Philadelphia: W.B. Saunders; 1998. pp. 1509–1601. [Google Scholar]
- 10.Gordon CM, Austin DJ, Radovick S, Laufer MR. Primary hypothyroidism presenting as severe vaginal bleedings in a prepubertal girl. J Pediatr Adolesc Gyn. 1997 Feb;10(1):35–38. doi: 10.1016/s1083-3188(97)70042-1. [DOI] [PubMed] [Google Scholar]
- 11.Jannini EA, Ulisse S, Arminton M. Macroorcidism in juvenile hypothyroidism. J Clin Endocrinol Metab. 1995;80:2543–2544. doi: 10.1210/jcem.80.8.7629256. [DOI] [PubMed] [Google Scholar]
- 12.Van wyk J, Grumbach M. Syndrom of precocious menstruation and galactorrhea in juvenile hypothyroidism: An example of hormonal overlap in pituitary feedback. J Pediatr. 1960;57:416–423. [Google Scholar]
- 13.Anasti JN, Flack MR, Froehlich J, et al. A potential novel mechanism for precocious puberty in juvenile hypothyroidism. J Clin Endocrinol Metab. 1995;80:276–279. doi: 10.1210/jcem.80.1.7829625. [DOI] [PubMed] [Google Scholar]
- 14.Niedziela M, Korman E. Severe hypothyroidism due to auto immune atrophic thyroiditis — Predicted target height and a plausible mechanism for sexual precocity. J Pediatr Endocrinol Metab. 2001;14:901–7. doi: 10.1515/jpem.2001.14.7.901. [DOI] [PubMed] [Google Scholar]


