Abstract
The increasing incidence of diabetes mellitus worldwide makes traditional approaches to its management inadequate. The involvement of young people in this diabetic “epidemic” provides an opportunity to apply a multidisciplinary approach to its management, to help reduce the huge burden of the disease and its complications. In 1998, we established a diabetic clinic for young adults, located within a privately owned company health center, because they were not receiving adequate attention in the adult clinic. Our purpose was to optimize diabetes control by teaching about diet, exercise, medications, and other practical diabetic management issues. In this special communication, we describe the organization of the clinic and present our experience with 105 patients in the first 4 years. Diabetic control as measured by serial glycosylated haemoglobin levels (HbA1c) and the occurrence and severity of diabetic ketoacidosis improved in our patients over those 4 years. Studies in the West have shown that small reductions in HbA1c have translated into dramatic decreases in microvascular complications. Application of this model to a larger population group is needed. Further study may help determine whether to adopt this pattern of care more widely, with its obvious benefits in reduction of diabetic morbidity, mortality and health care cost. We also identified three groups that may require special attention: females, young adults who develop the disease as children, and adolescents who have no regular adult supervision.
Saudi Aramco Al Hasa Health Center (SA-AHHC), which is part of Saudi Aramco Medical Services Organization, provides care for the company’s healthcare population of about 80 000 in the Al Hasa area of Saudi Arabia. Among these are 5000 adult diabetic patients, looked after in the diabetic clinic. SA-AHHC has a 24-hour daily emergency medical service and offers secondary care in obstetrics and gynaecology, paediatrics and internal medicine.
In recent years, many new adolescents have presented to us with new onset diabetes mellitus, consistent with the increasing occurrence of the disease world-wide.1–5 These patients were a significant group among those treated in our stabilization unit (SU).6 The Young Diabetes Clinic was established in 1998 to follow these patients as they did not receive adequate attention in the diabetes clinic, which was overloaded with older patients, many of whom had diabetic complications. The aim was to optimize their diabetic control by teaching about diet, exercise, medications, and other practical diabetic management issues. It was hoped that ultimately, this would help reduce the burden of the disease in family life and healthcare cost. This report presents our experience with patients aged 14 to 20 years for the first four years (1998–2002) of this clinic.
The Organization of the Young Diabetes Clinic
In the organization of the Young Diabetes Clinic, a multidisciplinary approach was taken from the beginning, in accordance with the recommendations of several expert panels7,8,9 with a team, led by a consultant physician, comprising several health professionals, each knowledgeable and interested in the relevant area. A diabetes nurse educator provided general teaching, insulin injection technique, glucometer and medication use, hypoglycaemia recognition and treatment, and exercise. A social worker assessed family life, schooling, and cultural and socio-economic barriers to good control. A dietitian gave practical diet advice, assessed school and home meal routines, food availability and preferences, and exercise. A diabetes nurse provided patient registration and screening, and assistance in examination, investigation and appointments. A consultant physician gave general direction and guidance and served as overall coordinator.
Teaching emphasis was on the “tripod” backbone of diabetic control: exercise, diet, and medications, linked by education. Additionally, each member outlined a patient’s programme and devised an individual plan, followed subsequently for each patient, after the first visit. Other health staff were co-opted for specific issues when necessary. Patients were referred by primary care and EMS physicians, or senior nurses. Pediatric-diagnosed patients were transferred at the age of 14, the transition age from pediatrics to medicine in our institution.
The Clinic in Practice
The clinic operated on an appointment system with appointments on the same day and time weekly. Appointments were scheduled to minimize school absence whenever possible. At the first clinic attendance, team members were introduced to patients, the clinic routine was explained, together with the diabetic control tripod; demographic data were collected, and a complete physical examination performed. Patients were encouraged to purchase glucose meters; the clinic provided test strips, and the diabetes educator demonstrated their use. The team met briefly before each clinic to discuss problem patients previously identified by the nurse on review of patient records, to ensure the same approach by all. Patients were seen every 6 to 8 weeks or more frequently if necessary.
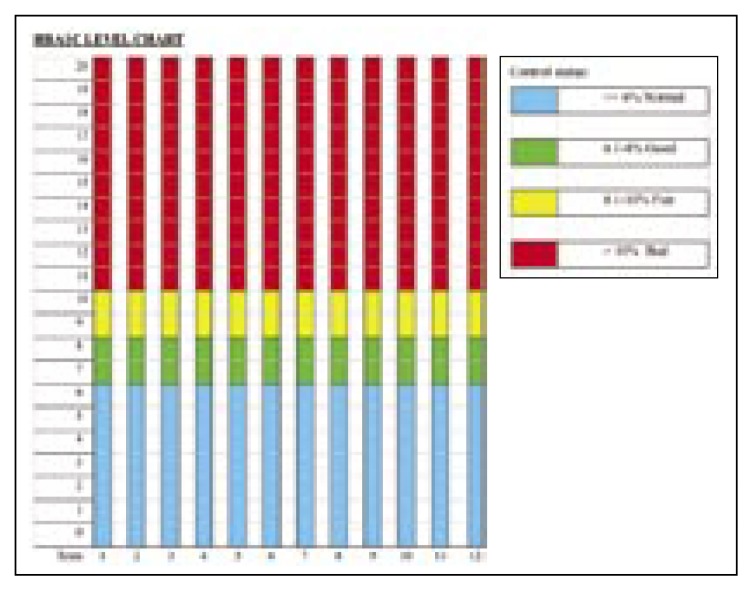
Eye examination, vascular and neurological examinations and monitoring of serum lipids, were performed at least annually, with specialist clinic referrals, as indicated. Those with special problems were sometimes admitted to the SU for prolonged contact. Diabetic ketoacidosis (DKA) occurrences were recorded, but ultimately glycosylated haemoglobin (HbA1c), which was measured quarterly, was our control indicator. Normal non-diabetic levels in our laboratory were 3.8–6.3% (total glycosylated Hb 4.8–7.8%). We divided results into color-coded categories made into wall mounted charts in consulting rooms, to motivate patients by demonstrating HbA1c trends to them (Figure 1). We strived to get the best result from each patient. Other activities like joint team sessions, group teaching and an open day were held every 4 to 6 months for patients and their families to improve overall diabetic control.
Figure 1.
Wall chart for recording changes in glycosylated hemoglobin (HbA1c).
Experience in the First Four Years (1998–2002)
We had over 100 patients by the year 2000, of which 51 were males and 54 females; most were diagnosed at ≥14 years of age (Table 1). The girls were more likely to be obese at diagnosis. Although the mean body mass index (BMI) for boys was not significantly different from that of girls, 57% of the girls compared with 45% of the boys were overweight or obese (P<0.05), based on a BMI of 25–29.9 as overweight and BMI of over 30 as obese;10 27% of boys and 28.6% of girls were obese.
Table 1.
Information on patients enrolled in the clinic by the year 2000.
| Male | Female | Total | |
|---|---|---|---|
| Number of patients | 51 | 54 | 105 |
| Diagnosed at ≥14 years | 64 | ||
| Tranfered from pediatrics | 41 | ||
| Body mass index (kg/m2) | 25.57 | 25.95 | |
| Overweight/obese (%) | 46 | 57 | |
| Obese (%) | 27 | 29 |
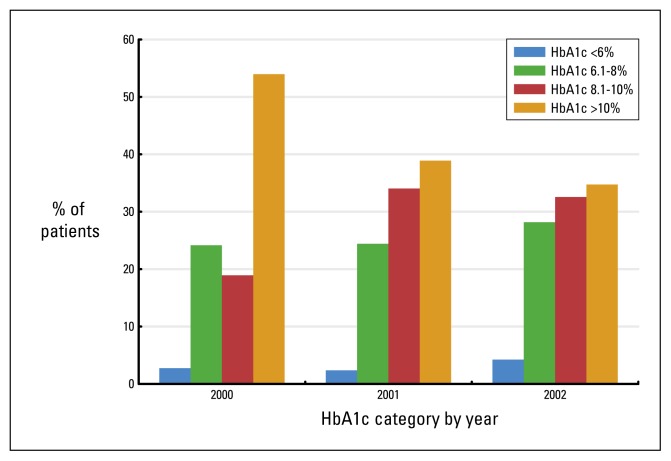
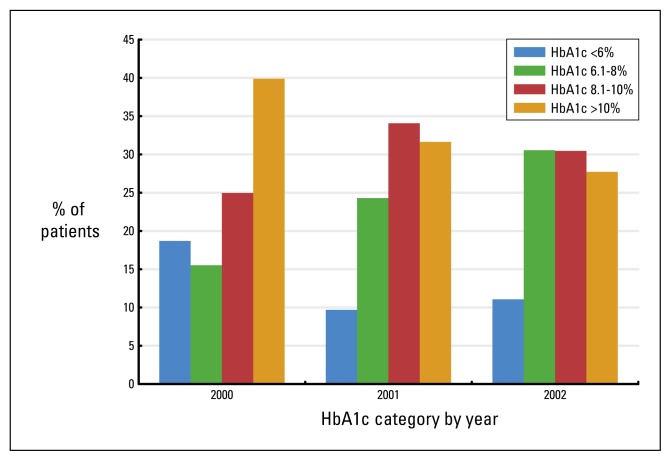
Compliance with clinic attendance (though not always in accord with recommendations) was high from the beginning at about 85% compared with 70% in our general clinics; by the end of 2002, this had risen to over 95%. The proportion of blood glucose meter users rose from 60% in year 2000 to 83% by the end of year 2002. Diabetic control improved over the years as outlined in Figures 2 to 4, which summarize serial HbA1c values. The proportion of patients in the poor control group with mean annual HbA1c >8% decreased during the period, but the change was not statistically significant (Figure 2 and 3). Males had better results than females, as did adult-diagnosed compared with paediatric-diagnosed patients. Patients regularly accompanied by parents or adult relatives also had better results than those who were not. Individual teaching was preferred over group teaching.
Figure 2.
Glycosylated hemoglobin (HbA1c) in females from 2000 to 2002.
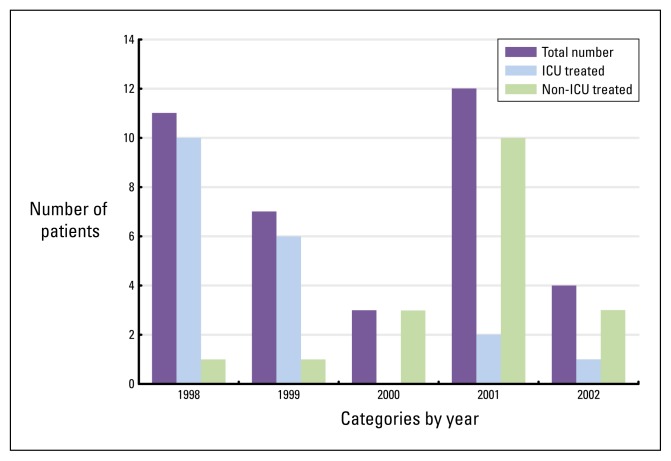
Figure 4.
Occurrence of diabetic ketoacidosis from 1998 to 2002.
Figure 3.
Glycosylated hemoglobin (HbA1c) in males from 2000 to 2002.
The prevalence and severity of DKA decreased from 1999 to 2002. Most cases occurred in previously diagnosed patients and were mild enough to be treated in the SU, rather than in the intensive care unit (ICU) (Figure 4); even in 2001 when their number increased, all but 2 were treated in the SU. There were several hypoglycaemic events in well-controlled patients; none required SU admission. These patients were given more teaching. No patient developed retinopathy or neuropathy.
Discussion
Diabetes mellitus is common in the populations of Saudi Arabia and its neighbours.11,12 Its management is costly, both in monetary terms and in human suffering, once complications develop13,14 For example, in Canada, where the cost has been computed, an acute myocardial infarction costs CAD $19 000, while haemodialysis for one year costs CAD $63 000.15 Saudi Arabian figures are even higher. One haemodialysis session in our system costs SAR 1700 (CAD $660). With most dialysis patients needing thrice weekly sessions, this is equivalent to SAR 265 200 (CAD $102 300) per patient yearly. No monetary value can of course be placed on the human cost of complications resulting in amputations or blindness.
Since many countries are now taking both medical and political action to contain diabetes,16,17,18 it is logical to focus on some preventive action that would decrease its economic burden by targeting young people, in whom the greatest benefits can be realized. This requires only a fraction of the costs currently incurred in the care of the older diabetic population. Thus, there is a strong economic argument for a clinic like ours dedicated to young people who are generally better educated than the older population, and more appreciative of important diabetic control factors. Many older patients assume, wrongly, that absence of symptoms means that all is well with diabetic control.
The multidisciplinary approach to diabetic management is recommended by various authorities on diabetes.7–9,19 Although the scope for its application is limited in developing countries like Saudi Arabia, because of insufficient manpower resources, it should be applied whenever possible as it is cost-effective. For instance, HbA1c reduction has been related to decreased progression of the complications of diabetes,20–25 including in young people.23 Thus the serial HbA1c reduction in our patients, if continued in future years, would represent a marked decrease in the expected rate of development of vascular complications. In the landmark Diabetes Control and Complications Trial, a decrease of 1% in HbA1c value produced a 25% decrease in microvascular endpoints, which was most marked in the need for photocoagulation.24 In the United Kingdom study for type 2 diabetes, a similar reduction decreased laser treatment by 37% and cataract extraction by 10%.25 These benefits also improved quality of life by preserving vision.26 The results can be extrapolated to other body systems, notably the kidneys and nervous system, where microvascular complications wreak havoc. Similarly, a reduction in DKA occurrence and severity is an improvement both in patients’ quality of life and expenditure on the use of hospital and ICU facilities.
Young patients achieve better control of their diabetes when they are led by adults. This may be related to young people’s psychology. Generally they do not have a long-term view of matters, but are interested mostly in the present. Adults may help focus their minds on, and encourage them towards achieving, set goals; even when they remain silent, their mere presence sends a strong message that diabetic control is important.
The greater acceptability and effectiveness of one-on-one teaching vs. group teaching may be cultural. Patients may feel shame or loss of face in sharing what they perceive as personal problems or failures, with others. This contrasts sharply with the mutual encouragement and support that patients and families generally derive in disease-specific associations, like those for cerebral palsy, epilepsy, Down’s syndrome and cystic fibrosis in Europe and North America. Males may have done better than females because they were more likely, for socio-cultural reasons, to have participated in physical activities including regular exercise, an important leg of the diabetic control tripod. Males were also more motivated; some females seemed frustrated by the socio-cultural restrictions on them. They and their families were more likely to hide the diagnosis, fearing that it would affect future marriage prospects. Our results, if confirmed by other studies, suggest three potential target groups among young diabetic patients for special attention, if and when such clinics are planned: females, young adults who develop the disease as children, and adolescents who have no regular adult supervision.
Acknowledgements
We thank all our colleagues at SA-AHHC who have worked with us to develop this service. The authors were employed by Saudi Aramco Medical Services Organisation when the study resulting in this paper was undertaken, and are grateful to the company for all the materials and services which made the study possible.
References
- 1.Fagot-Campagna A, Venkat Narayan KM. Type 2 diabetes in children. BMJ. 2001;322:377–378. doi: 10.1136/bmj.322.7283.377. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Dokheel TM. An epidemic of childhood diabetes in the United States? Evidence from Allegheny County, Pennsylvania. Pittsburgh Diabetes Epidemiology Research Group. Diabetes Care. 1993;16(12):1606–1611. doi: 10.2337/diacare.16.12.1606. [DOI] [PubMed] [Google Scholar]
- 3.Ehtisham S. Prevalence of type 2 diabetes in children in Birmingham. BMJ. 2001;322:1428. [PMC free article] [PubMed] [Google Scholar]
- 4.Rosenbloom AL, Joe JR, Young RS, Winter WE. Emerging epidemic of type 2 diabetes in youth. Diabetes Care. 1999;22(2):345–354. doi: 10.2337/diacare.22.2.345. [DOI] [PubMed] [Google Scholar]
- 5.An American epidemic. Newsweek. 2000 Sep;4:40–46. [PubMed] [Google Scholar]
- 6.Udezue E. A five year experience of a short-stay observation unit in Saudi Arabia. Annals of Saudi Medicine. 2003;23(1–2):72–75. doi: 10.5144/0256-4947.2003.72. [DOI] [PubMed] [Google Scholar]
- 7.Department of Health. National Service Framework (NSF) for Diabetes: Standards. London UK: 2001. [Google Scholar]
- 8.American Diabetes Association. Standards of medical care for patients with diabetes mellitus. Diabetes Care. 2003;26:33–50. doi: 10.2337/diacare.17.6.616. [DOI] [PubMed] [Google Scholar]
- 9.Canadian Medical Association. 1998 Clinical Practice Guidelines for the management of diabetes in Canada. CMAJ. 1998;159(8 Suppl):S1–S29. [PMC free article] [PubMed] [Google Scholar]
- 10.Millar WJ, Stephens T. The prevalence of overweight and obesity in Britain, Canada, and United States. Amer J Pub Health. 1987;77(1):38–41. doi: 10.2105/ajph.77.1.38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Alwan, King H. Diabetes in the Eastern Mediterranean (Middle East) Region. The World Health Organisation responds to a major public health challenge. Diabetic Medicine. 1995;12:1057–58. doi: 10.1111/j.1464-5491.1995.tb00421.x. [DOI] [PubMed] [Google Scholar]
- 12.Gill G. Diabetes an increasing problem in the Middle East. International Diabetes Digest. 1996;7(1):1. [Google Scholar]
- 13.King H, Aubert RE, Herman WH. Global burden of diabetes, 1995–2025. Prevalence, numerical estimates, and projections. Diabetes Care. 1998;1:1414–1431. doi: 10.2337/diacare.21.9.1414. [DOI] [PubMed] [Google Scholar]
- 14.Bagust A, Hopkinson P, Maslove I, et al. The projected health care burden of type 2 diabetes in the UK from 2000 to 2060. Diabetic Medicine. 2002;19(suppl 4):1–5. doi: 10.1046/j.1464-5491.19.s4.2.x. [DOI] [PubMed] [Google Scholar]
- 15.O’Brien JA, Patrick AR, Caro JJ. Cost of managing complications resulting from type 2 diabetes in Canada. BMC Health Sciences Research. 2003;3:7–12. doi: 10.1186/1472-6963-3-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Mayor S. Government publishes strategy to improve diabetes care. BMJ. 2003;326(7381):121–123. doi: 10.1136/bmj.326.7381.121. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Mudur G. Task force proposes changing body mass indicators for diabetes (India) BMJ. 2003;326(7381):126–7. [Google Scholar]
- 18.Clark CM. How should we respond to the worldwide diabetes epidemic? Diabetes Care. 1998;21:475–6. doi: 10.2337/diacare.21.4.475. [DOI] [PubMed] [Google Scholar]
- 19.American Diabetic Association. Type 2 diabetes in children and adolescents (A Consensus statement) Diabetes Care. 2000:1563–80. [Google Scholar]
- 20.LiYing Zhang, Krzentowski G, Albert A, Lefebvre PJ. Risk of developing retinopathy in Diabetes Control and Complications Trial Type 1 diabetic patients with good or poor metabolic control. Diabetes Care. 2001;24:1275–1279. doi: 10.2337/diacare.24.7.1275. [DOI] [PubMed] [Google Scholar]
- 21.Saum SL, Thomas E, Martyn Lewis A, Croft PR. The effect of diabetic control on the incidence of, and changes in, retinopathy in type 2 non-insulin dependent diabetic patients. Brit Journ Gen Pract. 2002;52:212–21. [PMC free article] [PubMed] [Google Scholar]
- 22.Van Leiden HA, Dekker JM, Moll AC, Nijpels G, Heine RJ, Bouter CD, Stehouwer CDA, Polak BCP. Risk factors for incident retinopathy in a diabetic and non-diabetic population: The Hoorn study. Arch Ophthalmol. 2003;121(2):245–251. doi: 10.1001/archopht.121.2.245. [DOI] [PubMed] [Google Scholar]
- 23.Henricsson M, Nystrom L, Blohme G, Ostman J, Kullberg C, Svensson M, et al. the incidence of retinopathy 10 years after diagnosis in young adult people with diabetes. Diabetes Care. 2003;26:349–354. doi: 10.2337/diacare.26.2.349. [DOI] [PubMed] [Google Scholar]
- 24.Diabetes Control and Complications Trial Research Group. The effect of intensive treatment of diabetes on the development and progression of long-term complications in insulin-dependent diabetes mellitus. New Engl J Med. 1993;329:977–986. doi: 10.1056/NEJM199309303291401. [DOI] [PubMed] [Google Scholar]
- 25.Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvasular complications of Type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000;321:405–412. doi: 10.1136/bmj.321.7258.405. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Kohner E. Comment: treatment of diabetic retinopathy. BMJ. 2003;326(7397):1023–1025. doi: 10.1136/bmj.326.7397.999. [DOI] [PubMed] [Google Scholar]